Abstract
Background. This paper reports a series of patients with Mirizzi's syndrome (MS) who were managed at our institution over an 11-year (1994–2005) period. Methods. Retrospective case note study of patients with a definitive or possible diagnosis of MS stated in radiology reports were identified using the hospital's radiology computer coding system. Results. 33 patients were identified with a median age of diagnosis of 70 (35–90) years and male to female ratio of 15:18. Liver function tests were deranged in all patients. Pre-operative radiological diagnosis was achieved in 28 patients: ultrasound scan (n = 4), computer tomography (n = 3), magnetic resonance cholangiopancreatography (n = 10) and endoscopic retrograde cholangiopancreatography (n = 11). Five patients were diagnosed intra-operatively. Type I MS was reported in 27 patients. Laparoscopic cholecystectomy was attempted in 18 patients with 6 being converted to open cholecystectomy. Six patients had biliary stent insertion only and 3 were conservatively managed. Six patients had type II MS, 4 were treated with open cholecystectomy and Roux-en-Y hepaticojejunostomy, 1 underwent an open subtotal cholecystectomy with fistula closure and 1 had percutaneous biliary stent insertion only. The median follow-up period was 2 (1–7) months (n = 18). 10 patients are currently under follow-up. Overall morbidity was 27% (n = 8) and mortality was 7% (n = 2). Conclusion. Pre-operative diagnosis of MS can be achieved using MRCP. Laparoscopic cholecystectomy for type I MS is a safe option and type II MS can be treated with Roux-en-Y hepaticojejunostomy or subtotal cholecystectomy with fistula closure.
Keywords: Mirizzi's syndrome, Biliary fistula, Cholecystocholedochal fistula
Introduction
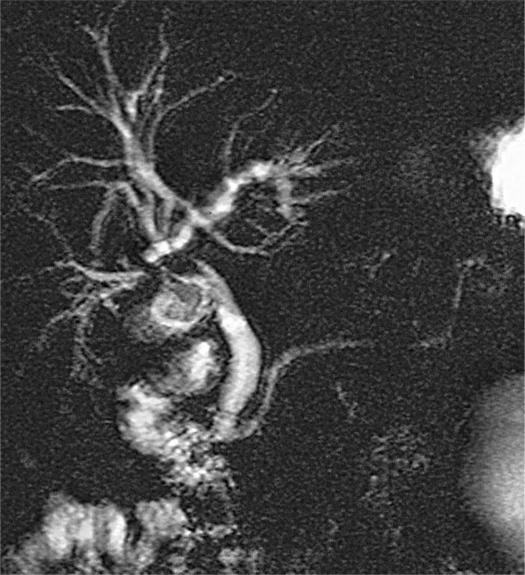
Mirizzi's syndrome (MS) was first described in 1948 as an extrinsic compression of the extrahepatic biliary system by an impacted stone in the gallbladder neck or the cystic duct leading to obstructive jaundice 1. McSherry et al. subsequently classified this syndrome into two distinct types 2; type I MS when there is extrinsic compression of the common hepatic duct by the gallbladder (Figure 1), and type II MS where the gallstone erodes from the gallbladder or cystic duct into the common hepatic duct resulting in a cholecystcholedochal fistula 2. However, this syndrome is rare and occurs in only 0.7–1.4% of patients with gallstone disease 3,4,5. Despite the rarity of this condition, a pre-operative diagnosis is crucial to determine the appropriate surgical management. Since its description there have been changes in management strategies that include diagnostic modalities, endoscopic therapy, and the emergence of minimally invasive surgical techniques. This study presents a retrospective review of the diagnostic work-up and outcome of MS treated within a single institution over the past decade.
Figure 1. .
Magnetic resonance cholangiopancreatography demonstrating type I Mirizzi's syndrome.
Methods
Patients diagnosed with MS at the Leeds Teaching Hospitals NHS Trust during the 11-year period, from August 1994 to August 2005, were identified using the hospital's radiology computer coding system (Radiology Management System). This search identifies patients with a definite diagnosis or suspicion of MS stated in radiology reports, which included ultrasound scan of the abdomen (USS), abdominal computer tomography (CT), magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP) reports. MRCP was introduced in 1997. Case notes of patients were reviewed for demography, clinical presentation, diagnostic work-up (liver function tests and endoscopic/radiological investigations) and clinical outcome (treatment, morbidity and mortality).
USS diagnosis of MS was confirmed with the presence of dilated intrahepatic ducts and common hepatic duct up to the point of external compression by the calculus where the bile duct can be seen to narrow 6. Criteria used to diagnose MS with other radiological modalities (CT, MRCP and ERCP) was cholangiographic evidence of compression of the bile duct by a stone impacted in the gallbladder neck or cystic duct, or the presence of a cholecystcholedochal fistula in keeping with McSherry et al. 2. Criteria for surgical diagnosis of MS in this study was based on surgical dissection and delineation of structures in the subhepatic space as described in McSherry et al. classification 2.
Results
During the study period, 33 patients with MS were identified of the 3,300 total cholecystectomies performed. The median age at diagnosis was 70 (range: 35–90) years and a male to female ratio of 15:18. Type I MS was diagnosed in 27 patients and six had type II MS. Acute surgical admissions were the principal mode of referral in 21 patients, six of whom were tertiary referrals from district general hospitals. The remaining 12 patients were in-hospital referrals from non-surgical specialties.
The most common symptom at presentation was abdominal pain (n = 24), and jaundice (n = 15). In cases of type II MS, five of the six patients presented with jaundice. The classical triad of symptoms of cholangitis was present in only seven patients, of which two patients had type II MS. An abnormality in one or all liver function tests (alkaline phosphatase, alanine aminotransferase and bilirubin) was present in all patients.
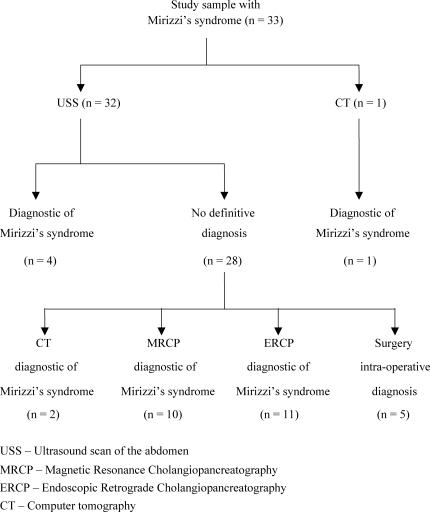
USS was used as a primary radiological investigation in 32 of the 33 patients, and the remaining patient underwent a CT scan. MS was diagnosed in four patients based on USS findings alone. One patient had synchronous common bile duct stones and three patients with type I MS had an empyema of the gallbladder managed with percutaneous cholecystostomy. These three patients underwent a cholecystectomy following recovery.
Second line investigations following no definitive diagnosis on USS (n = 28) were contrast enhanced CT (n = 9), MRCP (n = 14) and ERCP (n = 11) (Figure 2). CT was indicative of MS in three patients and demonstrated a cholecystocholedochal fistula in two patients. Diagnosis was achieved using MRCP in 10 patients and ERCP in 11 patients. ERCP demonstrated co-incidental common bile duct calculi in four patients. In the remaining five patients, diagnosis was made intra-operatively.
Figure 2. .
Imaging performed on patients in our study.
18 of 27 patients with type I MS underwent laparoscopic cholecystectomy, of which six were converted to open cholecystectomy due to unclear anatomy (n = 5) and intra-operative bleeding (n = 1). Two patients had endoscopic biliary drainage for cholangitis prior to surgery. Four patients had an on-table cholangiography. One patient had a laparoscopic cholecystoduodenal fistula repair and one with a synchronous distal common bile duct stricture underwent a laparoscopic choledochoduodenostomy. Six patients deemed unfit for surgery due to co-morbidity underwent endoscopic biliary stent insertion. Two patients declined surgery and one patient with significant co-morbidities was managed with antibiotic prophylaxis.
Four of six patients with type II MS were managed surgically with cholecystectomy and Roux-en-Y hepaticojejunostomy, two of whom had pre-operative biliary drainage for cholangitis. Open subtotal cholecystectomy with fistula repair using the gallbladder remnant was performed in one patient. The remaining patient was treated conservatively with percutaneous biliary stent insertion due to a cerebrovascular event following admission (Figure 3).
Figure 3. .
Management of patients with Mirizzi's syndrome based on the McSherry et al. classification in this study.
There were two (7%) in hospital, non-operative deaths; one patient died following perforation of the duodenum due to biliary stent migration, and the other as a result of cholangitis following percutaneous biliary stent insertion. Overall morbidity was 27% (n = 8) (Table I). Histological examination of the gallbladders demonstrated cholecystitis and no evidence of malignancy in all cases.
Table I. Morbidity data on surgical, endoscopic and radiological treatment of Mirizzi's syndrome in this study.
| Mirizzi's syndrome type | No. of cases (n = 30) | Management of patients | Morbidity (n = 8, 27%) |
|---|---|---|---|
| Type I | 24 | Surgery (n = 18) | Subphrenic collection (n = 2) Cholangitis (n = 1) |
| Endoscopic stenting (n = 6) | Pancreatitis (n = 1) Duodenal perforation secondary to biliary stent migration (n = 1) | ||
| Type II | 6 | Surgery (n = 5) | Biliary leak (n = 2) |
| Percutaneous stenting (n = 1) | Multi-organ failure (n = 1) |
ERCP – Endoscopic Retrograde Cholangiopancreatography
PTC – Percutaneous Transhepatic Cholangiography
The median follow-up period in 18 patients following discharge was 2 (range: 1–7) months. 10 patients are still under follow-up. Two patients were lost to follow-up and one patient was discharged immediately back to the nursing home without further follow-up.
Discussion
Despite advances in radiological modalities, diagnosis of MS is still difficult and is often made intra-operatively 6. USS often demonstrates a gallstone impacted at the neck of the gallbladder or cystic duct, and an associated dilatation of the biliary tract 6. Further imaging is usually required due to difficulty in differentiating MS from biliary tract or gallbladder malignancy. In the present series, USS achieved the diagnosis of type I MS in four patients which is in keeping with previous reports on the sensitivity of USS in this disease (4%) 8. ERCP may assist in differentiating benign from malignant strictures with a smooth outline of the stricture and delineation of a cholecystcholedochal fistula being indicators of type II MS 9. ERCP also has a therapeutic role and improved outcomes have been reported following pre-operative biliary drainage for cholangitis or jaundice 5,10,11. Four patients in the present study underwent biliary drainage endo-scopically for cholangitis prior to definitive surgical treatment. The introduction of MRCP has altered our management practice as it provides equivalent information to ERCP, without the inherent risk of complications 12,13. The diagnostic predictive value of ERCP was similar to MRCP in this study. Studies from other centers have reported similar findings, making MRCP the preferred choice of investigation 12,13. There is no study to date assessing CT scan as a diagnostic modality for MS, although we found that it identified a chole-cystcholedochal fistula in two of the three patients with type II MS.
USS is usually the first-line investigation for patients with abdominal pain and jaundice. Further imaging in cases with equivocal findings depends on the patient's co-morbidities and synchronous biliary tract pathology. We suggest MRCP as the next investigation and ERCP should be reserved for patients where therapeutic intervention is required. CT examination may assist in determining the presence of a cholecyst-choledochal fistula and in cases of suspected malignancy. However, its exact role is uncertain.
The surgical management of MS presents a demanding technical challenge to clinicians. Some authors consider this syndrome a contraindication for laparoscopic intervention due to the anatomical variability present in this syndrome 14,15,16 whereas others have reported successful laparoscopic surgery for type I MS albeit technically challenging 14,17,18,19. Interventions to enhance laparoscopic success include intra-operative cholangiography 4 or intra-operative ultrasound to delineate biliary tract anatomy prior to dissection 18. Previous studies have reported technical difficulties during the dissection phase around Calot's triangle, and removal of the entire gallbladder increased the risk of inadvertently damaging the common bile duct 19,20. Karademir et al. suggested laparoscopic partial cholecystectomy to be a safe and definitive surgical treatment for type I MS 21. It is thought that bile duct narrowing caused by external compression of the offending gallstone with its associated inflammatory tissue generally resolves following decompression with partial cholecystectomy 20. Nevertheless, failure of the laparoscopic approach and high conversion rates (17% 22, 100% 23) have been reported and these are often due to extensive dense adhesions, uncontrollable haemorrhage and failure of completely retrieving all gallstones impacted in the cholecystcholedochal fistula 22,23. In this series, the majority of patients with type I MS were treated successfully by laparoscopic cholecystectomy. In this series, the majority of patients with type I MS were treated successfully by laparoscopic cholecystectomy, suggesting that laparoscopic surgery is a safe surgical option when applied in the appropriate settings with a low threshold for conversion to the open technique. It is crucial to limit dissection away from the area of inflammation adjacent to the common bile duct to avoid possible injury.
The surgical management of type II MS is largely dependent on the size of the cholecystocholedochal fistula and the experience of the surgeon. A recent study reported the successful laparoscopic treatment of type II MS following pre-operative endoscopic biliary stenting which enabled intra-operative identification of the common bile duct 14. Other studies favour open techniques, 4,5,10,11,20,21,24 which include partial chole-cystectomy with primary closure, Roux-en-Y hepaticojejunostomy, cholecysto-duodenostomy and choledochoplasty with gallbladder flap 4,5,10,11,20,21,24. Partial chole-cystectomy with primary closure using the gallbladder remnant and T-tube placement through the fistula opening is considered an appropriate surgical option by some authors 21,25. Baer et al. suggest the use of bilio-enteric bypass of the cholecystocholedochal fistula rather than direct repair of the fistula after observing poor results in one instance 20. Although the direct closure configuration is thought to be prone to bile leakage and stricture formation, 20 Sharma et al. observed good long term results in patients who underwent primary closure of the cholecystocholedochal fistula using a cuff of the gallbladder 11. T-tube insertion into the common bile duct rather than the fistula opening following this procedure is thought to reduce the risk of stenosis by decompressing the common bile duct 11,26. In cases with a wider defect in the bile duct, Roux-en-Y hepaticojejunostomy is recommended to avoid complications such as biliary leakage, cholangitis and stricture formation 4,11,20,21. Although the majority of the patients with type II MS in this study underwent a cholecystectomy and Roux-en-Y hepatico-jejunostomy, subtotal cholecystectomy with fistula repair using gallbladder remnant is also an option.
There are a number of published reports on percutaneous 27,28 and endoscopic 8,29 biliary drainage as a treatment option in MS cases. England et al. found endoscopic therapy an effective temporizing measure prior to definitive surgical intervention in almost half their patients 8 and recommended an endoscopic approach for unsuitable surgical candidates with type II MS 8. Our study reported similar findings with endoscopic biliary stenting being used as a definitive treatment option in patients with significant co-morbidities.
None of the patients in this study had unsuspected gallbladder carcinoma. The incidence of gallbladder cancer in patients with MS is significantly higher than the incidence in longstanding gallstone disease which have been noted to be 27% and 2% respectively 30.
Conclusion
Pre-operative diagnosis of MS can be achieved using MRCP. In cases of type I MS, laparoscopic cholecystectomy is a safe option albeit with a low threshold for conversion to an open procedure. The surgical management of type II MS largely depends on the size of the fistula and a cholecystectomy and Roux-en-Y hepaticojejunostomy or subtotal cholecystectomy with closure of fistula using gallbladder remnant are both treatment options. Endoscopic biliary stent insertion is suitable for patients requiring pre-operative biliary drainage or those with significant co-morbidity.
References
- 1.Mirizzi PL. Syndrome del conducto hepatico. Journal International du Chirurgie. 1948;8:731–77. [Google Scholar]
- 2.McSherry CK, Ferstenberg H, Virshup M. The Mirizzi's syndrome: Suggested classification and surgical therapy. Surg Gastroenterol. 1982;1:219–25. [Google Scholar]
- 3.Bower TC, Nagorney DM. Mirizzi syndrome. HPB Surg. 1988;1:67–76. doi: 10.1155/1988/54294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Csendes A, Carlos Diaz , Burdiles P, Maluenda F, Nava O. Mirizzi's syndrome and cysto-biliary fistula: a unifying classification. Br J Surg. 1989;76:1139–43. doi: 10.1002/bjs.1800761110. [DOI] [PubMed] [Google Scholar]
- 5.Mishra MC, Vashishtha S, Tandon R. Bilio-biliary fistula: pre-operative diagnosis and management implications. Surgery. 1990;108:835–9. [PubMed] [Google Scholar]
- 6.Dewbury KC. The features of the Mirizzi's syndrome on USS examination. Br J Radiol. 1979;52:990. doi: 10.1259/0007-1285-52-624-990. [DOI] [PubMed] [Google Scholar]
- 7.Starling JR, Matallana RH. Benign mechanical obstruction of the common hepatic duct (Mirizzi's syndrome) Surgery. 1980;88:737–40. [PubMed] [Google Scholar]
- 8.England RE, Martin DF. Endoscopic management of Mirizzi's syndrome. Gut. 1997;40:272–6. doi: 10.1136/gut.40.2.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tulassay Z. Endoscopic retrograde cholangiopancreaticography in Mirizzi's syndrome. Am J Gastroenterol. 1987;82:391–2. [PubMed] [Google Scholar]
- 10.Dewar G, Chung SCS, Li AKC. Operative strategy in Mirizzi's syndrome. Surg Gynaecol Obstet. 1990;171:157–9. [PubMed] [Google Scholar]
- 11.Sharma AK, Rangan HK, Choubey RP, Thakur SK, Kumar A. Pitfalls in the management of Mirizzi's syndrome. Trop Gastroenterol. 1998;19:72–4. [PubMed] [Google Scholar]
- 12.Becker CD, Grossholz M, Mentha G, de Payer R, Terrier F. MR cholangio-pancreaticography: technique, potential indications and diagnostic features of benign and malignant conditions. Eur Radiol. 1997;7:865–74. doi: 10.1007/s003300050220. [DOI] [PubMed] [Google Scholar]
- 13.Hintaze RE, Adler A, Veltzke W, AbouRebyeh H, Hammerstingl R, Volg T, Felix R. Clinical significance of magnetic resonance cholangiopancreaticography (MRCP) compared to endoscopic retrograde cholangiopancreaticography (ERCP) Endoscopy. 1997;29:182–7. doi: 10.1055/s-2007-1004160. [DOI] [PubMed] [Google Scholar]
- 14.Binnie NR, Nixon SJ, Palmar KR. Mirizzi's syndrome managed by endoscopic stenting and laparoscopic cholecystectomy. Br J Surg. 1992;79:647. doi: 10.1002/bjs.1800790717. [DOI] [PubMed] [Google Scholar]
- 15.Posta ZG. Unexpected Mirizzi's anatomy: a major hazard to the common bile duct during laparoscopic cholecystectomy. Surg Endosc. 1995;5:412–4. [PubMed] [Google Scholar]
- 16.Rust KR, Clancy TV, Warren G, Meriesdorf J, Maxwell JG. Mirizzi's syndrome: a contraindication to coelioscopic cholecystectomy. J Laparoendosc Surg. 1991;1:133–7. doi: 10.1089/lps.1991.1.133. [DOI] [PubMed] [Google Scholar]
- 17.Paul MG, Burris DG, McGuire AM, Thorsinnson HD, Schonekas H. Laparoscopic surgery in the treatment of Mirizzi's syndrome. J Laparoendosc Surg. 1992;2:157–63. doi: 10.1089/lps.1992.2.157. [DOI] [PubMed] [Google Scholar]
- 18.Meng WC, Kwok SP, Kelly SP, Lau WY, Lij AK. Management of Mirizzi's syndrome by laparoscopic surgery and laparoscopic ultrasonography. Br J Surg. 1995;82:396. doi: 10.1002/bjs.1800820338. [DOI] [PubMed] [Google Scholar]
- 19.Lygidakis N. Spontaneous internal biliary fistulae: early surgery for prevention, radical surgery for cure. A report of 75 cases. Med Chir Dig. 1981;10:695–9. [PubMed] [Google Scholar]
- 20.Baer HU, Matthews JB, Schweizer WP, Gertsch P, Blumgart LH. Management of the Mirizzi's syndrome and the surgical implications of the cholecystocholedochal fistula. Br J Surg. 1990;77:743–5. doi: 10.1002/bjs.1800770708. [DOI] [PubMed] [Google Scholar]
- 21.Karademir S, Astarcioglu H, Sokmen S, Atila K, Tankurt E, Akpinar H, Coker A, Astarcioglu I. Mirizzi's syndrome: Diagnostic and surgical considerations in 25 patients. J Hepatobiliary Pancreat Surg. 2000;7:72–7. doi: 10.1007/s005340050157. [DOI] [PubMed] [Google Scholar]
- 22.Kok KYY, Goh PYM, Ngoi SS. Management of Mirizzi's syndrome in the laparoscopic era. Surg Endosc. 1998;12:1242–4. doi: 10.1007/s004649900828. [DOI] [PubMed] [Google Scholar]
- 23.Targarona EM, Andrade E, Balague C, Ardid J, Trias M. Mirizzi's syndrome: diagnostic and therapeutic controversies in the laparoscopic era. Surg Endosc. 1997;11:842–5. doi: 10.1007/s004649900467. [DOI] [PubMed] [Google Scholar]
- 24.Yip AWC, Chow WC, Chan J, Lam KH. Mirizzi's syndrome with cholecysto-choledochal fistula: preoperative diagnosis and management. Surgery. 1992;111:335–8. [PubMed] [Google Scholar]
- 25.Corlette MB, Bismuth H. Biliobiliary fistula: A trap in the surgery of cholelithiasis. Arch Surg. 1975;110:377–83. doi: 10.1001/archsurg.1975.01360100019004. [DOI] [PubMed] [Google Scholar]
- 26.Balthazar E. The Mirizzi's syndrome: inflammatory stricture of the common hepatic duct. Am J Gastroenterol. 1975;81:144–8. [PubMed] [Google Scholar]
- 27.Cairns SR, Watson GN, Lees WR, Salmon PR. Percutaneous lithotripsy and endo-prosthesis: a new treatment for obstructive jaundice in Mirizzi's syndrome. BMJ. 1987;295:1448. doi: 10.1136/bmj.295.6611.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oxtoby JW, Yeong CC, West DJ. Mirizzi's syndrome treated by percutaneous stone removal. Cardiovasc Intervent Radiol. 1994;40:207–9. doi: 10.1007/BF00571536. [DOI] [PubMed] [Google Scholar]
- 29.Adam A, Roddie ME, Benjamin IS. Case report: Mirizzi's syndrome – treatment with metallic endoprosthesis. Clin Radiol. 1993;48:198–201. doi: 10.1016/s0009-9260(05)80283-1. [DOI] [PubMed] [Google Scholar]
- 30.Redaelli CA, Buchler MW, Schilling MK, Krahenbuhl L, Ruchti C, Blumgart LH, Baer HU. High coincidence of Mirizzi's syndrome and gallbladder carcinoma. Surgery. 1997;121:58–63. doi: 10.1016/s0039-6060(97)90183-5. [DOI] [PubMed] [Google Scholar]