Abstract
Introduction: Normoglycemic patients undergoing pancreaticoduodenectomy (Whipple procedure) often inquire whether they will be diabetic postoperatively. There is limited information on this issue. We therefore looked at a more subtle measurement of long-term glycemic control, hemoglobin A1c (HgbA1c), as a prognostic tool in predicting progression to diabetes post Whipple. Patients and methods: A retrospective review over a 6-year period of all patients undergoing Whipple procedures at a single institution was conducted. In all, 27 patients had no prior history of diabetes, complete follow-up, and measured preoperative HgbA1c values. Postoperative diabetes was defined as the need for oral hypoglycemic agents or insulin. These charts were analyzed for progression to diabetes after Whipple. Results: Of the 27 patients, 10 were considered to have postoperative diabetes. The average preoperative HgbA1c value for these patients was 6.3±0.66. This was statistically different from the 17 patients without postoperative diabetes (average HgbA1c 5.2±0.39, p<0.001). The positive predictive value, negative predictive value, sensitivity, and specificity were 82%, 94%, 90%, and 88%, respectively. Conclusion: This study demonstrates that progression to diabetes is very unlikely after Whipple operation if the preoperative HgbA1c value is in the normal range. The apparent utility of HgbA1c in predicting postoperative diabetes in this small study suggests that this laboratory test may be very helpful in counseling patients for Whipple operation.
Keywords: diabetes, Whipple procedure, hemoglobin A1c
Introduction
Pancreaticoduodenectomy (Whipple procedure) has been viewed as one of the most aggressive surgical procedures in the abdomen. However, with improvement in instrumentation, antibiotics, and operative technique, this operation in now routinely performed with little morbidity at many tertiary care centers. The mortality rate of this operation is now 1–3% in experienced hands. Therefore, patients undergoing Whipple procedure are now concerned about their quality of life after the surgery. One important question asked by normoglycemic patients is whether they will become diabetic after Whipple operation.
In order to answer this question in a simple manner, we examined the utility of hemoglobin A1c (HgbA1c) in predicting progression to diabetes after Whipple surgery. Our hypothesis was that the HgbA1c would be a better indicator of long-term glycemic control and therefore a more sensitive marker of subtle glycemic control issues that would be uncovered after pancreatic surgery.
Patients and methods
All patients undergoing elective pancreatic surgery at a single institution between December 1998 and December 2004 were identified using the institution's case logging database. A total of 82 patients were identified in this time period; patients who did not have preoperative HgbA1c laboratory values available and those who carried a preoperative diagnosis of diabetes were excluded. A subgroup analysis of the 27 eligible patients was conducted through review of both the electronic and paper medical records. Approval for this study was obtained from the Institutional Review Board and met all compliance regulations of the Health Insurance Portability and Accountability Act of 1996.
Upon further evaluation of patient symptoms, surgical treatment, complications, preoperative lab values, and discharge medications, the 27 patients were divided into two groups: those with postoperative diabetes (requiring insulin or oral hypoglycemic agent on discharge) and those patients without postoperative diabetes.
A Student's t test was performed on the two sets of lab values to evaluate statistical differences in preoperative HgbA1c lab values between the two groups. Positive predictive value, negative predictive value, sensitivity, and specificity were calculated.
Results
Over the 6-year period of review, 27 patients met the inclusion criteria. Ten of the 27 patients had postoperative diabetes. The average age of the diabetic patients identified postoperatively was 67.1 years (range 50–81) and the average age for the 17 nondiabetic patients was 56.7 years (range 22–82) (Table I). There were seven female and three male patients in the diabetic group and nine female and eight male patients in the nondiabetic group.
Table I. Demographics, pathology, and surgical complications of the two groups.
| Parameter | Diabetic (n=10) | Nondiabetic (n=17) |
|---|---|---|
| Gender, F:M | 7:3 | 9:8 |
| Mean age (years) (range) | 66.6±10.2 (50–81) | 56.4±16.8 (22–82) |
| Pathology | ||
| Benign | ||
| Adenoma | 2 | 2 |
| Pancreatitis | 1 | 0 |
| Atypia | 1 | 0 |
| Pancreatic cancers | ||
| Adenocarcinoma | 6 | 10 |
| Endocrine | 0 | 2 |
| Intraepithelial | 0 | 2 |
| Nonpancreatic cancer | ||
| Renal cell carcinoma | 0 | 1 |
| Complications | ||
| Leak | ||
| Bile | 1 | 0 |
| Pancreatic | 0 | 2 |
| Infection | 1 | 2 |
| Bleeding | 2 | 3 |
| Death | 1 | 0 |
The demographic differences between the two groups are not statistically significant (p>0.05 by Student's t test).
Pathology was grouped into three categories: benign, pancreatic carcinomas, and nonpancreatic carcinomas (Table I). The diabetic group had four patients with benign pathology (two adenomas, one pancreatitis, one atypia) and six patients with pancreatic adenocarcinomas. The nondiabetic group had 2 patients with benign pathology (2 adenomas), 14 pancreatic cancers (10 adenocarcinomas, 2 endocrine neoplasms, and 2 intraepithelial neoplasms), and 1 patient with nonpancreatic cancer (renal cell carcinoma invading the duodenum).
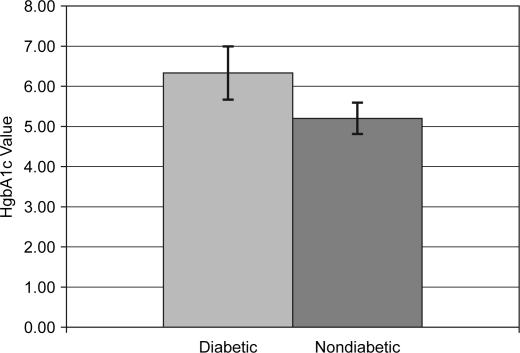
The average preoperative HgbA1c value for the diabetic patients was 6.33±0.66 mg/dl (Figure 1). The 17 nondiabetic patients had an average preoperative HgbA1c of 5.20±0.39 (p<0.001, by Student's t test). Positive predictive value of a high HgbA1c was 82% and negative predictive value of a normal HgbA1c was 94%. Sensitivity and specificity were 90% and 88%, respectively.
Figure 1. .
Average HgbA1c preoperative lab values for diabetic and nondiabetic patients. The difference in preoperative HgbA1c between the diabetic and nondiabetic group was statistically significant (p<0.001). The nondiabetic patients were mainly in the normal range for HgbA1c lab values (normal range 3.2–5.6), while most diabetic patients had predominantly abnormal values.
Discussion
HgbA1c is an excellent test that can help to predict which normoglycemic patients will become diabetic after Whipple operation. The negative predictive value of this test is high (94%), suggesting that if the HgbA1c is normal, the likelihood of diabetes after Whipple operation is low.
HgbA1c has been used in diabetic patients as a good indicator of long-term glycemic control 1,2. Endocrinologists will follow this value along with blood sugar measurements in patients with diabetes. Normal HgbA1c values are associated with lower risk of end organ complications from diabetes 3,4. Therefore, tight diabetic control, as reflected by a normal HgbA1c, is the aim of most endocrinologists.
Literature on the progression to diabetes after pancreatic surgery is very sparse. Studies examining risk factors for diabetes progression after Whipple operation have not been done. While this study represents a small, retrospective review in a single center, the results are powerful and clinically relevant. These results suggest that mild abnormalities in glycemic control can be detected by the HgbA1c value and this translates into a high likelihood of progression to frank diabetes with loss of islet cell mass with pancreatic surgery.
Other confounding factors, such as presence of excess body fat and elevated body mass index, which can result in insulin resistance 5, have not been examined in this study. This will be the target of future work. Our group aims to examine the correlation of islet cell volume in the resected specimen with glycemic control, in order to investigate the balance of insulin production and insulin resistance.
In summary, our results suggest that the clinician can use HgbA1c to counsel normoglycemic patients before Whipple surgery: if the HgbA1c is in the normal range, the likelihood of diabetes postoperatively is very low. Clearly, this is a retrospective study with many limitations and further studies with a larger sample size will be required to further this finding.
Footnotes
Presented at the American Hepato-Pancreatico-Biliary Association meeting in Miami Florida, March 2006.
References
- 1.The Diabetes Control and Complications Trial (DCCT) Research Group. The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the Diabetes Control and Complications Trial. Diabetes 1995;44:968–83. [PubMed] [Google Scholar]
- 2.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care 2004;27:S15–S35. [DOI] [PubMed] [Google Scholar]
- 3.Wei M, Gaskill SP, Haffner SM, Stern MP. Effects of diabetes and level of glycemia on all-cause and cardiovascular mortality. The San Antonio heart study. Diabetes Care. 1998;21:1167–72. doi: 10.2337/diacare.21.7.1167. [DOI] [PubMed] [Google Scholar]
- 4.Andersson DK, Svardsudd K. Long-term glycemic control relates to mortality in type II diabetes. Diabetes Care. 1995;18:1534–43. doi: 10.2337/diacare.18.12.1534. [DOI] [PubMed] [Google Scholar]
- 5.Kahn SE, Prigeon RL, Schwartz RS, Fujimoto WY, Knopp RH, Brunzell JD, et al. Obesity, body fat distribution, insulin sensitivity and islet beta-cell function as explanations for metabolic diversity. J Nutr. 2001;131:354S–60S. doi: 10.1093/jn/131.2.354S. [DOI] [PubMed] [Google Scholar]