Abstract
Obesity has become epidemic in the United States, in Europe, and in many urban areas in the developing world. The globalization of certain ‘fast foods’ and ‘soft drinks’ may, in part, be contributing to this epidemic. Diets high in saturated fatty acids and trans fats as well as drinks that have high fructose corn syrup levels may be particularly harmful. Recent research suggests that fat is a dynamic endocrine organ and that visceral fat is associated with the metabolic syndrome. Central obesity leads to organ steatosis and altered serum adipokines including reduced adiponectin and markedly elevated leptin. This abnormal adipokine milieu results in increased tissue infiltration of monocytes and macrophages which produce proinflammatory cytokines that alter organ function. Over many years, the combination of steatosis and local inflammation leads to fibrosis and eventually to cancer. Nonalcoholic fatty liver disease (NAFLD) is a precursor for nonalcoholic steatohepatitis (NASH). NAFLD and NASH (1) lead to cirrhosis and hepatocellular carcinoma, (2) increase the risk of liver resection, and (3) compromise the outcome of liver transplantation. Similarly, in the pancreas nonalcoholic fatty pancreas disease (NAFPD) may lead to nonalcoholic steatopancreatitis (NASP). NAFPD and NASP may (1) promote the development of chronic pancreatitis and pancreatic cancer, (2) exacerbate the severity of acute pancreatitis, and (3) increase the risk of pancreatic surgery. In the gallbladder nonalcoholic fatty gallbladder disease (NAFGBD, cholecystosteatosis) may lead to steatocholecystitis. Cholecystosteatosis may be an explanation for (1) the increased incidence of chronic acalculous cholecystitis and (2) the increased number of cholecystectomies.
Keywords: adipokines, cholecystosteatosis, obesity, steatohepatitis, steatopancreatitis
Acknowledgements
The opportunity to serve as the President of the International Hepato-Pancreato-Biliary Association (IHPBA) for the past 2 years has been a great honor. The IHPBA has made great strides in recent years, and many people need to be acknowledged for the IHPBA's success. For me personally, the support and understanding of my family have been key. My wife, Betty, and my children, Laura, David, and Susan, have always been by my side and have supported my efforts to enhance the IHPBA. Similarly, my hepato-pancreato-biliary (HPB) surgical colleagues at Indiana University, under the leadership of Keith Lillemoe, have allowed me to devote significant time to the IHPBA and have collaborated on recent studies to document steatopancreatitis and steatocholecystitis. In addition, my research collaborators at Indiana University, in particular Deborah Swartz-Basile, Attila Nakeeb, Abhishek Mathur, and Nicholas Zyromski, have been key in the documentation of these concepts in our animal studies.
The success of the IHPBA is also the result of the hard work of the Executive Secretariat, Medconnect, which is led by Bridget Barbieri. The three people who have made this 7th World Congress in Edinburgh so memorable are O. James Gardner, the Congress Chairman, Rowan Parks, the Local Organizing Chairman, and Camilla O'Brien from Concorde Services. The IHPBA Executive Committee also has to be acknowledged for their multiple contributions to the advancement of the association. Joseph Lau, the immediate Past President, Markus Büchler, the President-Elect, and James Toouli, the Editor of HPB as well as a Past President, all have worked very hard to make the IHPBA the premier international hepato-pancreato-biliary organization. C. Wright Pinson, Treasurer, Dirk J. Gouma, Secretary General, and Jacques Belghiti, Scientific Committee Chairman, also have played key roles in the association's recent success. Finally, let me acknowledge Clint Eastwood, Lee VanCleef, and Eli Wallach who played ‘The Good, The Bad, and The Ugly’, respectively, in the motion picture which provides the subtitle for this Presidential Address.
The obesity epidemic
In the USA obesity has become epidemic over the past 15 years. Obesity is currently defined as a body mass index (BMI) of >30. In 1990 only 10–12% of the US population had a BMI >30. However, by 1995, 14–16% of Americans met this definition of obesity. In 2000, 18–20% of the US population were obese, and in 2005 nearly 25% of Americans had a BMI >30. The obesity problem is not confined to the USA but is truly a global epidemic. In the Americas outside of the USA obesity is increasing in developing countries. In Europe, the percentage of people who are obese varies among the many countries from 10% to 40%. In Africa and Asia the problem of obesity is greater in urban than in rural areas because of the relative increased availability of food and decreased level of activity. As in the USA and in Europe, the problem of obesity is growing rapidly in several countries in south-east Asia.
Diet and obesity
A key factor in the obesity epidemic is diet. Both dietary fats and carbohydrates are likely to be playing a role. For some time, the importance of dietary cholesterol has been appreciated in the pathogenesis of cardiovascular disease. As a result, the concept of ‘good’ and ‘bad’ cholesterol has emerged. Consequently, high density lipoprotein (HDL) cholesterol has been termed ‘good’ whereas low density lipoprotein (LDL) cholesterol has been termed ‘bad’. However, very low density lipoproteins (VLDL) also are not good. Therefore, to fit the terminology of this talk, cholesterol carriers can be termed ‘good’ (HDL), ‘bad’ (VLDL), and ‘ugly’ (LDL).
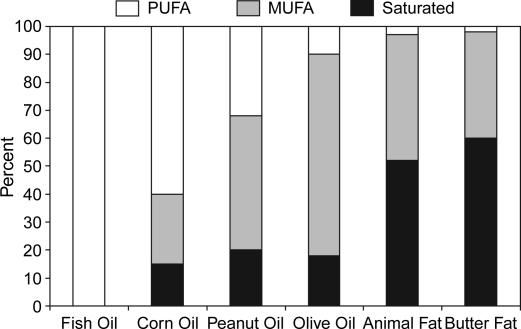
Similarly, fatty acids may be grouped into three categories based on their relative value for health (Table I). In general, polyunsaturated fatty acids (PUFA) and omega-3 fatty acids are ‘good’. In comparison, monounsaturated and saturated as well as omega-6 fatty acids are ‘bad’. Even worse, trans fatty acids, sphingolipids, and ceramides are the most ‘ugly’. Among the various oils and fats that we eat, the relative proportion of PUFA, monounsaturated fatty acids (MUFA), and saturated fatty acids are represented in Figure 1. At one end of the spectrum, fish oils, which are entirely PUFA and omega-3 fatty acids, fall in the ‘good’ category. At the other end of the spectrum, butter fat and animal fats have the highest percentage of saturated fatty acids and other toxic fats which make them the most ‘ugly’.
Table I. Good, bad, and ugly fatty acids.
| Good | Bad | Ugly |
|---|---|---|
| Polyunsaturated | Monounsaturated Saturated | Trans fatty acids |
| Omega-3 | Omega-6 | Sphingolipids Ceramides |
| Fish oil | Peanut oil | Animal fat |
| Corn oil | Olive Oil | Butter fat |
Figure 1. .
Fatty acids in various dietary oils and fats. PUFA, polyunsaturated fatty acids; MUFA, monounsaturated fatty acids.
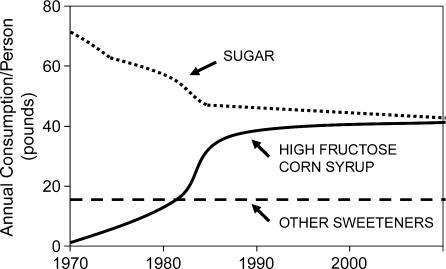
Coincident with the obesity epidemic in the United States and around the world has been the proliferation of ‘fast food’ restaurants. These establishments have been serving diets high in saturated and trans fatty acids, ‘ugly’ fats. At the same time the per capita consumption of ‘soft drinks’ has more than doubled in many parts of the world. These drinks are rich in high fructose corn syrup. Interestingly, the rise in consumption of high fructose corn syrup has paralleled the obesity epidemic (Figure 2). Unfortunately, an unproven theory suggests that drinks with high fructose corn syrup as the primary carbohydrate may be another factor leading to the increased incidence of obesity. Unfortunately, the typical fast food diet has more than double the number of calories (3800 versus 1800) of a ‘balanced’ diet. Moreover, a fast food diet has twice as many carbohydrate (1900 vs 850) and fat (1500 vs 750) calories with a dramatic increase in saturated fats. Thus, the globalization of certain fast foods and soft drinks may, in part, be contributing to the obesity epidemic.
Figure 2. .
Annual consumption of sugar, high fructose corn syrup, and other sweeteners in the United States.
Adipokines
In recent years the importance of visceral fat as an endocrine organ which produces multiple adipokines has been appreciated. The first adipokine to be discovered in 1994 was leptin (Table II). A year later adiponectin was discovered, although the importance of this molecule as a ‘good’ factor has only been appreciated in recent years. Resistin was first discovered in 2000, and the complete role of this ‘bad’ adipokine is still being elucidated. Adiponectin is produced by mature adipocytes, and leptin is expressed most fully by white adipocytes. In comparison, in humans, resistin is produced in the bone marrow and in monocytes. Serum levels of both adiponectin and leptin are higher in women than in men, whereas the reverse is true for resistin. Serum adiponectin levels are not affected by fasting and eating. In comparison, both resistin and leptin levels are lower with fasting and increased after a meal. Perhaps most importantly, adiponectin is anti-inflammatory whereas both resistin and leptin are proinflammatory.
Table II. Good, bad, and ugly adipokines: adiponectin, resistin, and leptin.
| Characteristic | Adiponectin | Resistin | Leptin |
|---|---|---|---|
| Discovered | 1995 | 2000 | 1994 |
| Amino acids | 247 | 114 | 167 |
| Expression | Mature adipocytes | Bone marrow Monocytes | White adipocytes |
| Females | ↑ | ↓ | ↑ |
| Fasting | – | ↓ | ↓ |
| Eating | – | ↑ | ↑ |
| Inflammation | ↓↓ | ↑↑ | ↑↑ |
Adiponectin has direct effects on both the vascular endothelium and monocytes. Adiponectin down-regulates vascular adhesion molecules and, thereby, prevents monocytes from invading tissues. In addition, adiponectin reduces the monocyte production of the proinflammatory cytokines, tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6), and increases the anti-inflammatory cytokines IL-10 and IL-1 receptor antagonist. In comparison, leptin up-regulates vascular adhesion molecules, which leads to monocyte and macrophage transmigration. The macrophages produce TNF-α, IL-6, and monocyte chemotactic protein-1 (MCP-1). In addition, TNF-α further down-regulates adiponectin, which exacerbates the proinflammatory state.
The adipokines clearly play a role in the metabolic syndrome (Table III). Patients with obesity, diabetes, hyperlipidemia, hypertension, and cardiovascular disease all have been shown to have reduced serum adiponectin and markedly increased leptin levels. Similarly, resistin levels are increased in patients who are obese, hyperlipidemic, and hypertensive, although the data are less clear for adult onset diabetes. Both adiponectin and leptin also have been implicated in the pathogenesis of cancer (Table IV). Good human data have shown that patients with breast, endometrial, prostate, and colon cancer have reduced adiponectin and elevated serum leptin levels. Moreover, adiponectin decreases cell growth and angiogenesis whereas leptin promotes these pathogenetic factors. In addition, leptin has been shown to reduce immune function.
Table III. Adipokines and the metabolic syndrome.
| Parameter | Adiponectin | Resistin | Leptin |
|---|---|---|---|
| Obesity | ↓ | ↑ | ↑↑ |
| Diabetes | ↓ | ?↑ | ↑↑ |
| Hyperlipidemia | ↓ | ↑ | ↑↑ |
| Cardiovascular disease | ↓ | ↑ | ↑↑ |
Table IV. Adiponectin, leptin and cancer.
| Parameter | Adiponectin | Leptin |
|---|---|---|
| Cancer types | ||
| Breast | ↓ | ↑ |
| Endometrial | ↓ | ↑ |
| Prostate | ↓ | ↑ |
| Colon | ↓ | ↑ |
| Pathogenesis | ||
| Cell growth | ↓ | ↑ |
| Angiogenesis | ↓ | ↑ |
| Immune function | ? | ↓ |
Hepatic fat
In the United States 15% of adults have nonalcoholic fatty liver disease (NAFLD). Hepatic steatosis is found in half of adults with diabetes, and the same is true for patients with hyperlipidemia. In comparison, 75% of patients coming to gastric bypass surgery have NAFLD. Current thinking suggests that the conversion from NAFLD to nonalcoholic steatohepatitis (NASH) requires a ‘two hit’ theory (Table V). The first ‘hit’ is thought to be the hepatic accumulation of triglycerides and increased hepatic diacylglycerol. Controversy persists regarding the exact etiology of the second ‘hit’. Multiple theories related to altered free fatty acid metabolism, insulin resistance, oxidative stress, lipid peroxidation, ceramide accumulation, reduced adiponectin, and increased proinflammatory cytokines have been suggested.
Table V. The ‘two hit’ theory of steatohepatitis.
| First hit = ↑ hepatic triglycerides |
| ↑ hepatic diacylglycerol |
| Second hit = Free fatty acid metabolism |
| Insulin resistance |
| Oxidative stress |
| Lipid peroxidation |
| Ceramide |
| ↓ Adiponectin |
| ↑ Cytokines |
Nevertheless, NASH has been clearly associated with decreased serum adiponectin (odds ratio [OR] = 6.1), increased serum TNF-α (OR = 5.6), increased waist-to-hip ratio (OR = 2.7), and increased insulin resistance (OR = 1.4). In addition, 30% of patients with NASH will develop hepatic cirrhosis over 5–10 years. Moreover, 10% of patients with NASH-induced cirrhosis will go on to develop hepatocellular carcinoma (HCC).
The incidence of HCC has increased in western countries in recent years. Presently, one-third of these western patients with HCC have no evidence of viral hepatitis. In addition, obesity and diabetes have been clearly demonstrated to be risk factors for HCC with the OR for diabetes being 3.8. Thus, the combination of hepatic steatosis and diabetes may lead to NASH and eventually HCC. Another recently described problem involving hepatic fat is chemotherapy-associated steatohepatitis (CASH). Current data suggest that irinotecan causes hepatic steatosis and that oxaliplatin results in hepatic venous occlusion. Hepatic surgery in patients with CASH is associated with increased bleeding and infectious complications. Moreover, a direct correlation exists between the number of chemotherapeutic cycles and the incidence of postoperative complications.
Presently, 20% of patients undergoing hepatic surgery in the United States have hepatic steatosis. These patients clearly have increased operative morbidity (approximately 50%) and mortality (>10%). Patients with NAFLD undergoing hepatic resection have increased blood loss, an increased transfusion requirement and decreased hepatic regeneration. Patients with NAFLD undergoing liver resection also have been shown to have reduced hepatic omega-3 fatty acids, reduced macro- and microcirculation, and increasing necrotic cell death. Experimental data also suggest that preoperative consumption of fish oils as well as ischemic preconditioning, which preserves adenosine triphosphate, are protective.
NAFLD has similarly been found in 25–35% of liver donors in the United States and Europe. These livers have diminished tolerance to both cold and warm ischemia because of a combination of necrotic and apoptotic cell death, nerapotosis. Livers with >30% macrosteatosis have been shown to have poor graft function. As a result, several investigators have suggested that BMI, a computed tomography (CT) fat index, or donor liver biopsies should be used to assess hepatic steatosis. In addition, experimental data suggest that administration of IL-6 may protect the donor liver with steatosis.
Pancreatic fat
Similar to hepatocellular carcinoma, the association between pancreatic cancer and obesity is robust. Patients with pancreatic cancer are more likely to have an elevated BMI (OR = 1.8) and diabetes (OR = 2.0) and are less likely to be active (OR = 0.5) In addition, epidemiologic data suggest that patients with pancreatic cancer are more likely to eat a high fat and a saturated fat diet. Moreover, pancreatic cancer has been associated with decreased consumption of PUFAs and with the intake of metformin for adult onset diabetes. Experimental data also suggest that PUFAs reduce and that IL-6 promotes tumor growth.
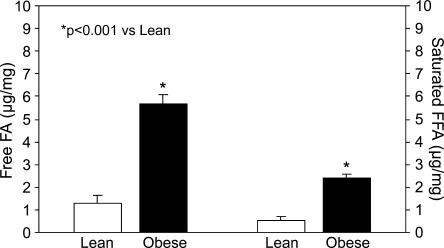
Patients who are obese have been documented to have more severe pancreatitis than lean individuals. Recent experiments from our laboratory also suggest that compared with lean mice, obese leptin-deficient mice have more intra- and interlobular pancreatic fat measured histologically. In addition, obese mice had increased total fat, triglycerides, cholesterol, free fatty acids, and saturated free fatty acids compared with lean mice (Figure 3). In addition, obese mice had significantly more TNF-α and IL-1β in their pancreas. In a follow-up study lean (C57BL/6J, leptin normal), obese (ob/ob, leptin-deficient), and obese (db/db, leptin-resistant) mice underwent either intraperitoneal saline or caerulin injections to produce edematous pancreatitis. The obese mice had more severe pancreatitis histologically than the lean mice, and the hyperleptinemic obese (db/db) mice had the most severe pancreatitis. These studies suggest that nonalcoholic fatty pancreas disease (NAFPD) may lead to nonalcoholic steatopancreatitis (NASP). In addition, serum adiponectin levels correlated inversely with the severity of pancreatitis, suggesting that low adiponectin may be more important than high leptin levels.
Figure 3. .
Pancreas concentrations of free fatty acids (FFA) (left) and saturated FFA (right) in lean and obese mice.
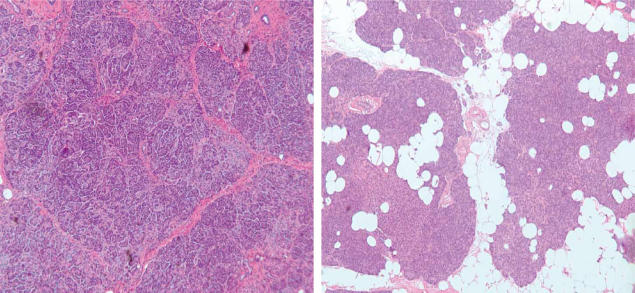
Analogous to the situation with NAFLD and liver surgery, we recently performed a clinical analysis of NAFPD and pancreatic surgery. Forty patients who developed a pancreatic fistula following pancreatoduodenectomy were matched for age, gender, pancreatic pathology, surgeon, and type of operation with 40 control patients who did not develop a pancreatic fistula. Patients with a pancreatic fistula had significantly more intralobular, interlobular, and total pancreatic fat (Figure 4). This analysis suggests that fatty pancreas is a risk factor for postoperative pancreatic fistula.
Figure 4. .
Typical histologic specimen from the neck of the pancreas from a control patient (left, 5×) depicting minimal pancreatic fat and slight fibrosis and from a fistula patient (right 5×) depicting significant intra- and interlobular pancreatic fat and minimal fibrosis.
Biliary fat
Similar to both hepatocellular and pancreatic cancer, the association between gallbladder cancer and obesity is well established. Both obesity and diabetes as well as gallstones are known risk factors for gallbladder cancer. In addition, gallbladder cancer is significantly more common in Pima Indians, native Chileans, and inhabitants of northern India. All of these populations consume high fat diets and are prone to obesity. Obesity, diabetes, and hypertriglyceridemia also are well established risk factors for gallstones. In addition, diets high in fat, saturated fats, cholesterol, and carbohydrates have been associated with gallstone formation in both animals and humans. In addition, diets high in fish oil and olive oil have been shown to decrease the incidence of gallstones. Moreover, statins and ezetimibe, which lower serum and tissue cholesterol, have been shown to prevent gallstone formation.
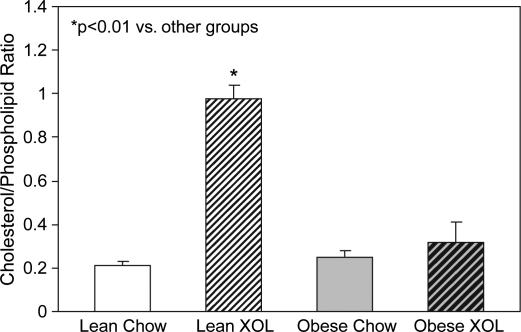
Recent animal data from our laboratory have demonstrated that obese leptin-deficient (ob/ob) and obese leptin-resistant (db/db) mice have enlarged gallbladders that do not respond normally to neurotransmitters. In addition, administration of leptin to obese ob/ob mice and ciliary neurotrophic factor to obese db/db mice has been shown to reverse these phenomena. Moreover, lean mice fed a high fat/high cholesterol diet develop abnormal gallbladders that do not empty normally, in part because of increased cholesterol in the gallbladder wall (Figure 5). Finally, administration of ezetimibe, which blocks fat absorption in the small intestines, lowers serum and gallbladder wall cholesterol, normalizes gallbladder function, and prevents cholesterol crystal and gallstone formation.
Figure 5. .
Cholesterol/phospholipid ratio in the gallbladder wall of lean (C57BL/6J) and obese (ob/ob) mice on a chow (low cholesterol) and high fat/high cholesterol (XOL) diet.
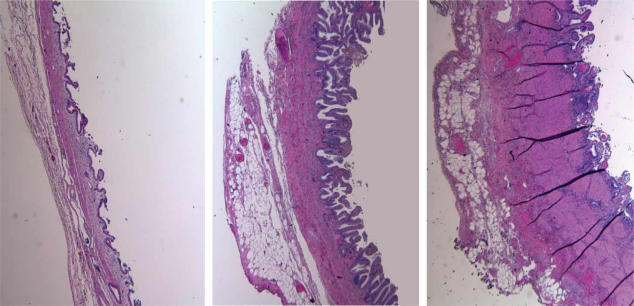
A recent human study from Indiana University confirms these murine observations. Sixteen nondiseased controls, 16 patients with chronic acalculous cholecystitis, and 16 patients with calculous cholecystitis were matched for gender, BMI, and other metabolic syndrome parameters. The acalculous cholecystitis patients were significantly younger. However, both the acalculous and calculous cholecystitis patients had more fat in the gallbladder wall, cholecystosteatosis, than nondiseased controls (Figure 6). A recent murine study comparing lean (C57BL/6J) and obese (ob/ob) mice fed a low (45%) and high (75%) carbohydrate diet confirmed that the obese mice have more fat in the gallbladder and that the high carbohydrate diet exacerbates this phenomenon. In addition, the obese mice and those fed a high carbohydrate diet had increased gallbladder tissue levels of TNF-α, IL-6, and IL-1β. These cytokines have been associated with decreased smooth muscle function and diminished gallbladder absorption. Thus, the presence of increased toxic fats and proinflammatory cytokines, steatocholecystitis, may result in increased gallbladder pressure and pain. As a result, steatocholecystitis may explain the increased incidence of acalculous cholecystitis and the increased rate of cholecystectomy that has paralleled the obesity epidemic in the United States.
Figure 6. .
Histologic section from a nondiseased control (left), an acalculous cholecystitis patient (middle), and a calculous cholecystitis patient (right). The cholecystitis patients had more fat in the gallbladder wall, cholecystosteatosis (alcalculous) or steatocholecystitis (calculous).
Conclusions
The obesity epidemic has led to increased obesity research. Visceral fat is now considered to be an endocrine organ which produces multiple adipokines. The combination of high leptin and low adiponectin is associated with the metabolic syndrome, an insulin-resistant state in which steatosis and proinflammatory cytokines cause organ dysfunction. Over time and probably with a ‘second hit’, inflammation leads to fibrosis and, eventually, to cancer. This sequence of events has been most clearly elucidated in the liver where NAFLD → NASP → cirrhosis → HCC. However, a similar process most likely occurs in the pancreas where NAFPD → NASP → chronic pancreatitis → pancreatic cancer. Likewise, in the gallbladder NAFGBD (cholecystosteatosis) → steatocholecystitis → gallstones → gallbladder cancer. For the HPB surgeon, organ steatosis is significant because it increases the risk of liver resection, alters the function of the donor liver, increases the risk of pancreatic fistula following pancreatic resection, and increases the incidence of chronic acalculous cholecystitis and the need for cholecystectomy.
Footnotes
Presented as the Presidential Address, 7th World Congress of the International Hepato-Pancreato-Biliary Association, Edinburgh, UK, September 2006.