Abstract
Objective
Phosphorus containing additives are increasingly added to food products. We sought to determine the potential impact of these additives. We focused on chicken products as an example.
Methods
We purchased a variety of chicken products, prepared them according to package directions, and performed laboratory analyses to determine their actual phosphorus content. We used ESHA Food Processor SQL Software to determine the expected phosphorus content of each product.
Results
Of 38 chicken products, 35 (92%) had phosphorus containing additives listed among their ingredients. For every category of chicken products containing additives, the actual phosphorus content was greater than the content expected from nutrient database. For example, actual phosphorus content exceeded expected phosphorus content by an average of 84 mg/100g for breaded breast strips. There was also a great deal of variation within each category. For example, the difference between actual and expected phosphorus content ranged from 59 to 165 mg/100g for breast patties. Two 100 g servings of additive containing products contain an average of 440 mg of phosphorus, or about half the total daily recommended intake for dialysis patients.
Conclusion
Phosphorus containing additives significantly increase the amount of phosphorus in chicken products. Available nutrient databases do not reflect this higher phosphorus content, and the variation between similar products makes it impossible for patients and dietitians to accurately estimate phosphorus content. We recommend that dialysis patients limit their intake of additive containing products and that the phosphorus content of food products be included on nutrition facts labels.
Keywords: phosphorus containing additives, dialysis, nutrient databases, nutrition facts labels
INTRODUCTION
Hyperphosphatemia is a major contributor to poor outcomes among dialysis patients and results in increases in both all-cause and cardiovascular mortality rates.[1, 2] Excess phosphorus combines with calcium and deposits in arteries and other soft tissues and leads to the development of atherosclerotic heart disease.[3] Elevated serum phosphorus also stimulates parathyroid hormone and contributes to secondary hyperparathyroidism and renal bone disease.[1, 4, 5]
The amount of phosphorus in the American diet has increased considerably, primarily from phosphorus containing additives in convenience and fast foods.[6] It is estimated that, depending on individual food choices, such additives add as much 1000 mg/day of phosphorus to the diet.[7] Moreover, phosphorus in additives is almost entirely absorbed while only 60% of naturally occurring phosphorus is absorbed.[8] Education regarding high phosphorus foods is a key component of hyperphosphatemia management,[9, 10] but the use of phosphorus containing additives may make it difficult for patients and dietitians to accurately estimate the phosphorus content of foods.
We therefore sought to determine the actual phosphorus content of a number of chicken products and to compare the actual content with that estimated from a reference source that dietitians might consult in advising patients. We focused on chicken products because chicken is a good source of high quality protein for dialysis patients.
METHODS
We surveyed grocery stores in greater Cleveland to determine the types of stores in the area (e.g. grocery chains, discount stores, warehouse stores), the categories of chicken products available (e.g. raw chicken, breaded patties, breaded nuggets), and the specific brands available. We then purchased 38 chicken samples across a variety of store types, products, and brands. We cooked raw chicken products at 350 degrees Fahrenheit until they reached an internal temperature of 165 degrees Fahrenheit and prepared precooked chicken products according to package directions. The samples were allowed to cool and then shipped in cool pack boxes to Medallion Laboratories (Minneapolis, Minnesota). Medallion Laboratories ashed the samples at high temperature, digested them in acid, and used inductively coupled plasma to determine their actual phosphorus content. One sample was analyzed for each product.
We used ESHA Food Processor SQL Software (version 9.8, ESHA Research. Salem OR), to determine the expected phosphorus content of each chicken product. ESHA data is obtained from the United States Department of Agriculture National Nutrient Database for Standard Reference,[11] manufacturers’ analyses, and other reference sources.
The actual and expected phosphorus content were calculated per 100 grams of product. Serving size was determined from nutrition facts labels on each product. The presence of phosphorus containing additives was determined from the ingredient lists of products. In presenting the results, we grouped chicken products based on amount of processing, size, and content (i.e. breast vs. mixed chicken).
RESULTS
Of the 38 chicken products, 35 (92%) had phosphorus containing additives listed among their ingredients (Table 1). Among the 8 boneless breast products, 5 (63%) had phosphorus containing additives. Among the 30 breaded breast strips, breast nuggets, mixed nuggets, breast patties, and mixed patties, 100% had phosphorus containing additives. Additives present included sodium phosphate (present in 71% of products), sodium aluminum phosphate (32%), sodium acid pyrophosphate (26%), monocalcium phosphate (26%), and sodium tripolyphosphate (16%). Ten products contained two additives and another ten products contained three additives.
Table 1.
Actual and expected phosphorus content of a variety of chicken products (n=38).
| Category | Product | Phosphorus containing additives* | Serving size (g) | Actual Phosphorus (mg/100g) | Expected phosphorus (mg/100g) | Difference (mg/100g) |
|---|---|---|---|---|---|---|
| Boneless breast | Giant Eagle fresh chicken breast | None | 112 | 205 | 228 | −23 |
| Dave’s fresh chicken breast | None | Not specified | 184 | 228 | −44 | |
| Kirkland quick frozen chicken breast | None | 112 | 182 | 228 | −46 | |
| Kirkwood quick frozen chicken breast | 1 | 182 | 255 | 228 | 27 | |
| Townsend quick frozen chicken breast | 1 | 113 | 250 | 228 | 22 | |
| Tyson quick frozen chicken breast | 1 | 112 | 317 | 228 | 89 | |
| Giant Eagle quick frozen chicken breast | 1 | 196 | 240 | 228 | 12 | |
| Great Value quick frozen chicken breast | 1 | 196 | 246 | 228 | 18 | |
| Breaded breast strips | Tyson crispy chicken strips | 1 | 92 | 235 | 147 | 88 |
| Barber chicken breast finger filets | 1,3 | 112 | 235 | 147 | 88 | |
| Tyson chicken breast tenderloins | 1,3 | 68 | 253 | 147 | 106 | |
| Kirkwood chicken breast strip fritters | 1 | 92 | 236 | 147 | 89 | |
| Kirkwood chicken breast tenderloins | 1,2,4 | 68 | 242 | 147 | 95 | |
| Banquet chicken breast strips | 2,4,5 | 85 | 183 | 147 | 36 | |
| Breast nuggets | Banquet chicken breast tenders | 2,4,5 | 85 | 186 | 147 | 39 |
| Kirkwood chicken breast tenders | 1,3 | 85 | 229 | 147 | 82 | |
| Weaver breast tenders | 1,3 | 85 | 208 | 147 | 61 | |
| Tyson breast tenders | 1,3 | 85 | 238 | 147 | 91 | |
| Banquet chicken breast nugget | 2,4,5 | 85 | 184 | 147 | 37 | |
| Tyson breast nuggets | 1,3 | 90 | 213 | 147 | 66 | |
| Fast Fixin breast nuggets | 1,2,4 | 85 | 226 | 147 | 79 | |
| Mixed nuggets | Banquet chicken nuggets | 2,4,5 | 85 | 219 | 147 | 72 |
| Blossom Creek chicken nuggets | 3 | 114 | 128 | 147 | −19 | |
| Weaver chicken nuggets | 1 | 75 | 174 | 147 | 27 | |
| Redi serve chicken nibblers | 1 | 77 | 200 | 147 | 53 | |
| Giant Eagle chicken nuggets | 1,3 | 91 | 197 | 147 | 50 | |
| Tyson chicken nuggets | 1,3 | 92 | 221 | 147 | 74 | |
| Breast patties | Tyson breast patties | 1,3 | 73 | 185 | 126 | 59 |
| Weaver breast patties | 1 | 74 | 229 | 126 | 103 | |
| Banquet chicken breast patties | 2,4,5 | 76 | 291 | 126 | 165 | |
| Giant Eagle breast patties | 1,3 | 74 | 202 | 126 | 76 | |
| Kirkwood chicken breast filets | 1,2,4 | 106 | 236 | 126 | 110 | |
| Tyson chicken breast filets | 1 | 129 | 238 | 126 | 112 | |
| Mixed patties | Weaver chicken patties | 1 | 74 | 253 | 126 | 127 |
| Banquet chicken patties | 2,4,5 | 76 | 189 | 126 | 63 | |
| Blossom chicken patties | 3 | 79 | 150 | 126 | 24 | |
| Tyson southern style patties | 1,2,4 | 73 | 221 | 126 | 95 | |
| Redi Serve chicken patties | 1 | 71 | 188 | 126 | 62 |
1 = sodium phosphate, 2 = sodium acid pyrophosphate, 3 = sodium aluminum phosphate, 4 = monocalcium phosphate, 5 = sodium tripolyphosphate
For boneless breasts without phosphorus containing additives, the actual phosphorus content was somewhat less than the content expected from the nutrient database (Figure 1). For every other category of chicken products, the actual phosphorus content was greater than the content expected from the nutrient database. For example, actual phosphorus content exceeded expected phosphorus content by an average of 84 mg/100g for breaded breast strips. There was also a great deal of variation within each category. For example, the difference between actual and expected phosphorus content ranged from 59 to 165 mg/100g for breast patties.
Figure 1.
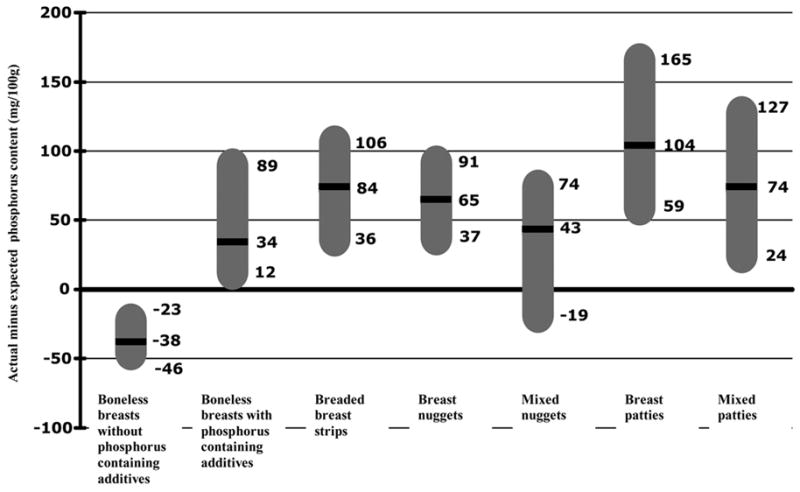
Actual minus expected content of 38 chicken products. For each category of chicken products, the black line represents the mean value while the top and bottom of the gray bar represent the maximum and minimum values.
The difference between actual and expected phosphorus content was significantly higher for products containing phosphorus additives compared to products without additives (−38 vs. +68, p= <.0001). Two 100 g servings of additive containing products would provide an average of 440 mg of phosphorus (range 256 – 634 mg), or about half the total daily recommended intake for dialysis patients.
DISCUSSION
We found that phosphorus containing additives are present in the vast majority of chicken products and significantly increase the phosphorus content of such products. Available reference sources do not reflect this higher phosphorus content, and the variation between similar products makes it impossible for patients and dietitians to accurately estimate phosphorus content.
Our findings have important implications for patients, providers, policy makers, and food manufacturers. Dialysis patients and their providers struggle not only with dietary restrictions but also with nutritional barriers such as poor appetite and needing help with cooking.[12] Convenience and fast foods tend to be palatable and require little or no preparation but often contain phosphorus additives. Instructing dialysis patients to limit their intake of additive containing products would seem to be a reasonable recommendation. However, following such a recommendation will be challenging for several reasons. First, as our analysis of chicken products demonstrates, the availability of additive-free products in grocery stores may be limited. Second, ingredient lists are generally not present on fast food items, making it difficult to identify the presence of phosphorus containing additives. Third, simply knowing that a product contains a phosphorus additive doesn’t allow an accurate estimate of its phosphorus content. Fourth, additive-free products, such as raw chicken breast, may require more effort to prepare. This may not be possible for dialysis patients with physical or social limitations.[12]
Phosphorus containing additives may also have an impact on patients with earlier stages of chronic kidney disease and on the general population. Hyperphosphatemia may contribute to cardiovascular and bone disease among the 10 million Americans with moderate kidney disease.[13–15] In the general population, dietary intakes of phosphorus have been increasing while intakes of calcium have been decreasing.[6] There is evidence to suggest that these intake patterns interfere with the normal process of calcium regulation and affect peak bone mass and rate of bone loss even among individuals with normal renal function. [6, 16–20]
We recommend that manufacturers analyze their products for phosphorus content and make these data available for incorporation into nutrient databases. Food manufacturers should also create lower phosphorus versions of popular products. We also recommend that policymakers mandate that phosphorus content of foods be included on the nutrition facts label. These actions by manufacturers and policymakers will help patients limit their phosphorus intake, will help providers to better instruct patients, and will help researchers to accurately assess dietary intake.
Several limitations must be considered in interpreting our results. We focused only on chicken products obtained in a single geographic region and analyzed one sample per product. However, many of the products we analyzed are national brands and phosphorus containing additives are known to be present in numerous other products. Nonetheless, we recommend that other investigators perform similar analyses with a variety of products in other geographic regions.
In conclusion, phosphorus containing additives significantly increase the amount of phosphorus in chicken products. Available nutrient databases do not reflect this higher phosphorus content, and the variation between similar products makes it impossible for patients and providers to accurately estimate phosphorus content. Despite the development and widespread use of new vitamin D analogues and phosphorus binders, one-third to one-half of dialysis patients continue to have elevated phosphorus levels[14, 21–24]. We speculate that the use of phosphorus containing additives limits the effectiveness of these new therapies. We recommend that dialysis patients limit their intake of additive containing products, that manufacturers develop lower phosphorus versions of their products, and that policymakers require phosphorus content of food products to be included on nutrition facts labels.
Acknowledgments
Supported by grant DK51472 and GCRC M01RR00080 from the National Institutes of Health, Bethesda, Maryland.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Block GA, Hulbert-Shearon TE, Levin NW, et al. Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: a national study. Am J Kidney Dis. 1998;31:607–617. doi: 10.1053/ajkd.1998.v31.pm9531176. [DOI] [PubMed] [Google Scholar]
- 2.Rodriguez-Benot A, Martin-Malo A, Alvarez-Lara MA, et al. Mild hyperphosphatemia and mortality in hemodialysis patients. Am J Kidney Dis. 2005;46:68–77. doi: 10.1053/j.ajkd.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 3.Ribeiro S, Ramos A, Brandao A, et al. Cardiac valve calcification in haemodialysis patients: role of calcium-phosphate metabolism. Nephrol Dial Transplant. 1998;13:2037–2040. doi: 10.1093/ndt/13.8.2037. [DOI] [PubMed] [Google Scholar]
- 4.Goodman WG. The consequences of uncontrolled secondary hyperparathyroidism and its treatment in chronic kidney disease. Semin Dial. 2004;17:209–216. doi: 10.1111/j.0894-0959.2004.17308.x. [DOI] [PubMed] [Google Scholar]
- 5.Malluche HH, Mawad H. Management of hyperphosphataemia of chronic kidney disease: lessons from the past and future directions. Nephrol Dial Transplant. 2002;17:1170–1175. doi: 10.1093/ndt/17.7.1170. [DOI] [PubMed] [Google Scholar]
- 6.Calvo MS, Park YK. Changing phosphorus content of the U.S. diet: potential for adverse effects on bone. J Nutr. 1996;126:1168S–1180S. doi: 10.1093/jn/126.suppl_4.1168S. [DOI] [PubMed] [Google Scholar]
- 7.Bell RR, Draper HH, Tzeng DY, et al. Physiological responses of human adults to foods containing phosphate additives. J Nutr. 1977;107:42–50. doi: 10.1093/jn/107.1.42. [DOI] [PubMed] [Google Scholar]
- 8.Uribarri J, Calvo MS. Hidden sources of phosphorus in the typical American diet: does it matter in nephrology? Semin Dial. 2003;16:186–188. doi: 10.1046/j.1525-139x.2003.16037.x. [DOI] [PubMed] [Google Scholar]
- 9.Ford JC, Pope JF, Hunt AE, et al. The effect of diet education on the laboratory values and knowledge of hemodialysis patients with hyperphosphatemia. J Ren Nutr. 2004;14:36–44. doi: 10.1053/j.jrn.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 10.Cupisti A, D’Alessandro C, Baldi R, et al. Dietary habits and counseling focused on phosphate intake in hemodialysis patients with hyperphosphatemia. J Ren Nutr. 2004;14:220–225. [PubMed] [Google Scholar]
- 11.ARS U.S. Department of Agriculture. USDA Nutrient Database for Standard Reference, Release19. Nutrient Data Laboratory Home page. http://www.ars.usda.gov/nutrientdata Note: Release numbers change as new versions are released, in, 2006.
- 12.Leon JB, Albert JM, Gilchrist G, et al. Improving albumin levels among hemodialysis patients: a community-based randomized controlled trial. Am J Kidney Dis. 2006;48:28–36. doi: 10.1053/j.ajkd.2006.03.046. [DOI] [PubMed] [Google Scholar]
- 13.Clinical practice guidelines for nutrition in chronic renal failure. K/DOQI, National Kidney Foundation. Am J Kidney Dis. 2000;35:S1–140. doi: 10.1053/ajkd.2000.v35.aajkd03517. [DOI] [PubMed] [Google Scholar]
- 14.K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003;42:S1–201. [PubMed] [Google Scholar]
- 15.Mehrotra R. Disordered mineral metabolism and vascular calcification in nondialyzed chronic kidney disease patients. J Ren Nutr. 2006;16:100–118. doi: 10.1053/j.jrn.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 16.Calvo MS. Dietary phosphorus, calcium metabolism and bone. J Nutr. 1993;123:1627–1633. doi: 10.1093/jn/123.9.1627. [DOI] [PubMed] [Google Scholar]
- 17.Calvo MS, Kumar R, Heath H. Persistently elevated parathyroid hormone secretion and action in young women after four weeks of ingesting high phosphorus, low calcium diets. J Clin Endocrinol Metab. 1990;70:1334–1340. doi: 10.1210/jcem-70-5-1334. [DOI] [PubMed] [Google Scholar]
- 18.Metz JA, Anderson JJ, Gallagher PN., Jr Intakes of calcium, phosphorus, and protein, and physical-activity level are related to radial bone mass in young adult women. Am J Clin Nutr. 1993;58:537–542. doi: 10.1093/ajcn/58.4.537. [DOI] [PubMed] [Google Scholar]
- 19.Kemi VE, Karkkainen MU, Lamberg-Allardt CJ. High phosphorus intakes acutely and negatively affect Ca and bone metabolism in a dose-dependent manner in healthy young females. Br J Nutr. 2006;96:545–552. [PubMed] [Google Scholar]
- 20.Teegarden D, Lyle RM, McCabe GP, et al. Dietary calcium, protein, and phosphorus are related to bone mineral density and content in young women. Am J Clin Nutr. 1998;68:749–754. doi: 10.1093/ajcn/68.3.749. [DOI] [PubMed] [Google Scholar]
- 21.Block GA, Klassen PS, Lazarus JM, et al. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004;15:2208–2218. doi: 10.1097/01.ASN.0000133041.27682.A2. [DOI] [PubMed] [Google Scholar]
- 22.Al Aly Z, Gonzalez EA, Martin KJ, et al. Achieving K/DOQI laboratory target values for bone and mineral metabolism: an uphill battle. Am J Nephrol. 2004;24:422–426. doi: 10.1159/000080087. [DOI] [PubMed] [Google Scholar]
- 23.Kimata N, Akiba T, Pisoni RL, et al. Mineral metabolism and haemoglobin concentration among haemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS) Nephrol Dial Transplant. 2005;20:927–935. doi: 10.1093/ndt/gfh732. [DOI] [PubMed] [Google Scholar]
- 24.Lorenzo V, Martin-Malo A, Perez-Garcia R, et al. Prevalence, clinical correlates and therapy cost of mineral abnormalities among haemodialysis patients: a cross-sectional multicentre study. Nephrol Dial Transplant. 2006;21:459–465. doi: 10.1093/ndt/gfi213. [DOI] [PubMed] [Google Scholar]


