Abstract
Objectives:
To describe the Boston Area Community Health (BACH) survey, a National Institutes of Health[en]supported epidemiological study of symptoms suggestive of the following urologic conditions: urinary incontinence, benign prostatic hyperplasia, interstitial cystitis, chronic pelvic pain of bladder origin, prostatitis, hypogonadism, erectile dysfunction, and female sexual dysfunction.
Methods:
BACH used a two-stage stratified cluster design to recruit a community-based random sample of 5506, divided between males (2301) and females (3205), three racial/ethnic groups (black, Hispanic, and white), and four age groups (30[en]39, 40[en]49, 50[en]59, 60[en]79 yr). Validated questionnaires were used to collect information on urologic symptoms, comorbidities, prescribed and over-the-counter medications, reproductive history, quality of life, health care utilization, physical activity, depressive symptoms, interpersonal stress, smoking, alcohol use, fluid intake, nutrition, menopausal status, sexual activity, abuse, anthropometrics (measured height, weight, hip and waist circumference, pulse rate, blood pressure), and sociodemographics including country of origin, marital status, employment status, and income. Blood samples were collected from 68% of all subjects.
Results:
A large representative community-based sample was successfully recruited to provide both cross-sectional and eventually longitudinal data to address important urologic questions.
Conclusions:
BACH has features distinguishing it from most other epidemiological studies in urology. It uses a random community-based sample of people who are racially/ethnically diverse and includes a broad age range (30[en]79 yr). It includes both males and females The study focuses on symptoms rather than variably defined disease conditions, it is multidisciplinary, and it is designed to become longitudinal.
Keywords: Epidemiology, Survey sampling, Symptom research, Urology
1. The concept of a urologic iceberg
In 1963 epidemiologist John Last introduced the concept of “the illness iceberg” to describe how diseases are distributed in the community [1]. Some problems are never presented to a doctor and never receive a diagnosis, and others are presented but not accurately diagnosed: these represent the “submerged portion of the iceberg.” A smaller proportion may be presented, receive an accurate diagnosis, and be recorded as a case: these constitute only the “tip of the iceberg.” This epidemiological metaphor appears useful in understanding urologic symptoms in the general population (Fig. 1).
Fig. 1.
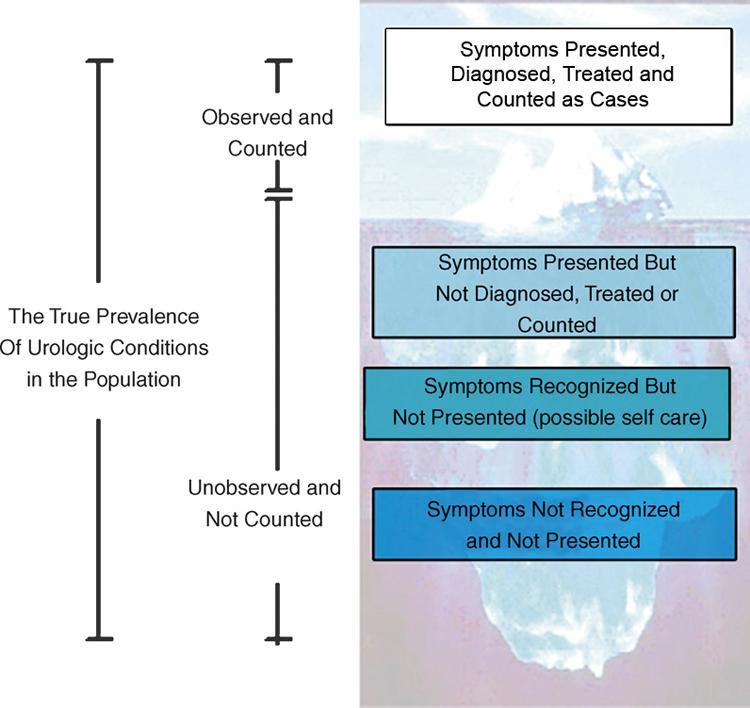
The urologic iceberg: differentiating the true and observed prevalence of urologic symptoms
Only limited population-based information is presently available on the epidemiology of major urologic diseases. Current understanding relies heavily on studies of convenience samples of patients who access medical care and receive a diagnosis (those at the tip of the iceberg). Although few community-based random-sample studies of urologic conditions have been conducted in the United States to date, several factors are contributing to interest in urologic conditions. The U.S. population is rapidly aging, in particular the minority population; between 2000 and 2025, non-Hispanic whites aged 65+ yr will increase 62.4%, non-Hispanic blacks will increase 121.7%, and Hispanics will increase 215% [2]. Americans are increasingly health conscious, with health advice books and web-based information readily available concerning the management of urologic diseases and symptoms. In addition, new treatments are available for urologic conditions, and traditional approaches are being supplanted by patient-friendly, minimally invasive procedures and pharmacologic therapies. Direct-to-consumer advertising in the United States exhorts the public to request treatments for urologic symptoms. Finally, there is increasing interest in quality of life and social functioning, which appear to be affected by urologic diseases. Additional epidemiological data are needed to inform clinical practice and health services research and policy.
2. Gaps in urologic epidemiology
The paucity of epidemiological data on urologic problems is surprising, given their magnitude and costs to the U.S. economy. Some of the most basic information remains unavailable. For example, population-based age-specific prevalence and incidence rates for many major urologic diseases are not available. Disparities in urologic conditions by race/ethnicity remain poorly understood. Changes in urologic symptoms across the life span are not well described (changes may occur because of aging or they may result from other factors, such as weight gain and comorbidities). Major risk factors or correlates for many urologic conditions are not yet clearly identified. Operational definitions for major urologic conditions have not been agreed upon, and the clinical validity and reliability of several instruments in widespread use are questionable. Overlap between symptoms of different urologic conditions (eg, interstitial cystitis and chronic pelvic pain syndrome or chronic pelvic pain and prostatitis) has not been adequately assessed. The magnitude of unmet urologic need in the general community, especially among the unemployed and uninsured, remains unexplored. Racial/ethnic differences in symptom recognition and the use of health care for urologic symptoms has not been well described. The reasons for apparent gender differences in some major urologic symptoms remain uncertain. The effect of psychosocial influences and the use of prescribed and over-the-counter (OTC) medications on urologic symptoms has received little attention. There have been few attempts to examine the impact of urologic problems/symptoms on quality of life and functioning, how these may vary across races, ethnicities, genders, and age groups, and how these may change over time (natural progression and remission). In the absence of reliable data on these issues, especially the major risk factors and early precursors of urologic symptoms among specific racial/ethnic, gender, and age groups, it is difficult to design interventions to improve the urologic status of large populations.
3. The Boston Area Community Health survey
The Boston Area Community Health (BACH) Survey was a response to a National Institutes of Health consensus panel recommendation that research on urologic and gynaecologic conditions in minorities be given the highest priority [3]. The goal of the baseline BACH study was to recruit a random, community-based sample of males and females and obtain cross-sectional data to fill major gaps in epidemiological understanding of several urologic disorders. With the recruitment of 5506 subjects at the end of June 2005, this goal has been achieved.
The BACH study is poised to contribute to our understanding of the epidemiology of a range of urologic symptoms/conditions and is providing population-based prevalence estimates (by race/ethnicity, age, gender, and socioeconomic status) of urologic syndromes, associated risk factors, health care use, and implications for quality of life [4,5].
4. Design specifications
The BACH study was designed to fulfil an ambitious range of methodological requirements. It should employ a randomly selected community-based sample, in contrast to small convenience samples of urologic patients with access to the health care system. The study should include major U.S. racial/ethnic minorities (black, Hispanic, and white subjects). Sufficient numbers of both males and females should be included. The study should cover a broad age range (from 30 to 79 yr), and the age distribution of the sample should be balanced to permit examination of rare conditions across the life span. It should be based on symptoms of disease rather than on variably diagnosed urologic conditions. Wherever possible, the study should use clinically validated research questionnaires to permit comparison of results with other studies. It should be multidisciplinary and permit examination of anthropometric, lifestyle, and psychosocial contributions to urologic problems, along with their quality-of-life implications. Results should be representative of the Boston community and hopefully (with appropriate adjustments) generalizable to the U.S. population. Finally, while initially a cross-sectional survey, it should be able to transition to a prospective cohort study so that the population can be followed over time to estimate incidence rates, examine early precursors of subsequent disease, and observe the natural course (progression and remission) of urologic symptoms.
5. BACH research model and major aims
Figure 2 depicts the research model informing the direction and content of the BACH study. The existence of social disparities (by age, race/ethnicity, and gender) in the prevalence and medical management of urologic symptoms is a major focus of the BACH project, and these three independent variables shape the overall design of the study. The range of urologic signs and symptoms studied are also a distinguishing feature of BACH and comprise the dependent variables. Some symptoms are obviously specific to males (e.g., those concerning erectile dysfunction, hypogonadism, prostatitis, and benign prostatic hyperplasia), whereas others affect both genders (e.g., those suggestive of interstitial cystitis/painful bladder syndrome, chronic pelvic pain, urinary incontinence, sexual dysfunction).
Fig. 2.
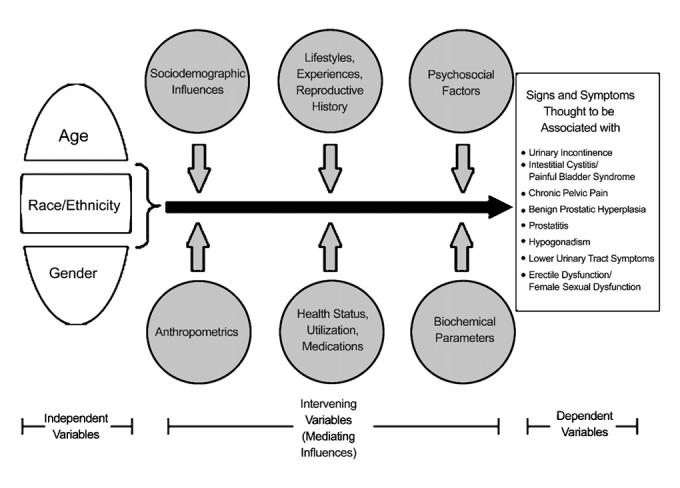
Research model for the Boston Area Community Health epidemiological survey of urologic symptoms
Factors thought to contribute to the aetiology of urologic problems or mediate the relationship between the independent and dependent variables are included in Figure 2. These intervening variables (effect modifiers) are organized into six groups: (1) sociodemographic influences (household composition, occupation and employment status, marital status, education, level of acculturation); (2) lifestyles (physical activity, tobacco usage, alcohol use, diet, sexual activity) and life experiences (history of abuse, reproductive history, menopausal status); (3) psychosocial factors (depression, interpersonal stress, quality of life); (4) anthropometrics (height, weight, hip and waist circumferences, pulse rate, blood pressure); (5) health status (self-reported, diagnosed medical conditions), medical care utilization (health insurance status, access to and use of medical care, perceived severity of symptoms, unmet urologic need), and medications consumed (a complete inventory of prescribed and OTC preparations); and (6) biochemical parameters (including major hormones and an extensive lipid metabolism profile).
The BACH questionnaires and project correspondence were translated and then back-translated in Spanish to ensure cross-cultural equivalence of meaning; 26% of the BACH interviews were conducted in Spanish. All questionnaires and forms used in the BACH survey were annually reviewed and approved by the New England Research Institutes' Institutional Review Board.
6. Steps required to obtain the BACH multiple-stage cluster sample
6.1. Sampling design
To ensure representation of the Boston population in all batches, we employed a stratified, two-stage cluster sampling design, with census blocks as the primary sampling units (PSUs) and households as the secondary sampling units (SSUs). The intent, at least for the first batch, was to invite all eligible adults in selected households to participate. This rule was subsequently modified to include some sampling within selected households to reach the target cell numbers of 250 (Table 1). For results from this sampling design to be representative of the Boston population, it is usual practice to weight observations inversely proportional to their probability of selection into the BACH study [6,7]. These weights are then further post-stratified to the composition of the Boston population according to the 2000 U.S. Census. Analyses are being conducted in version 9.1 of SAS (SAS Institute, Cary, NC, USA) and version 9.0.1 of SUDAAN (Research Triangle Institute, Research Triangle Park, NC, USA). Further details on sampling and weighting procedures are available at www.neriscience.com.
Table 1.
Study design (age, gender, and race/ethnic composition of the BACH sample)
| Gender | Race/Ethnicity | 30[en]39 yr | 40[en]49 yr | 50[en]59 yr | 60[en]79 yr | Total |
|---|---|---|---|---|---|---|
| Males | black | 164 (250) | 224 (250) | 156 (250) | 156 (250) | 700 (1000) |
| white | 201 (250) | 208 (250) | 197 (250) | 229 (250) | 835 (1000) | |
| Hispanic | 250 (250) | 227 (250) | 157 (250) | 132 (250) | 766 (1000) | |
| Females | black | 258 (250) | 287 (250) | 252 (250) | 273 (250) | 1070 (1000) |
| white | 196 (250) | 234 (250) | 271 (250) | 323 (250) | 1024 (1000) | |
| Hispanic | 337 (250) | 320 (250) | 257 (250) | 197 (250) | 1111 (1000) | |
| Total | 1406 (1500) | 1500 (1500) | 1290 (1500) | 1310 (1500) | 5506 (6000) | |
Values are the actual number enrolled; those in parentheses are the desired number.
Bold numbers indicate cells where target enrolment has been reached.
6.2. Stratification of census blocks
Boston consists of 17 residential planning districts. For logistical reasons, we did not sample from the Harbor Island planning district (2000 U.S. Census population 638). The remaining 16 residential planning districts were grouped into four geographic areas, so that the resulting areas were more racially/ethnically homogeneous. The resulting areas (and the planning districts in each area) were: North (Allston/Brighton, Back Bay/Beacon, Central, Charlestown, East Boston, Fenway, South Boston); West/South (Hyde Park, Jamaica Plain, Roslindale, West Roxbury); Roxbury/Mattapan (Mattapan, Roxbury, South End); and Dorchester (North Dorchester, South Dorchester).
Using information from the 2000 U.S. Census, we stratified the 4266 residential blocks in Boston by minority density. We classified a block as “low minority density” if less than 25% of the residents were black and less than 30% were Hispanic, “high-density black” if at least 25% of the resident were black, and “high-density Hispanic” if at least 30% of the residents were Hispanic. This resulted in 12 strata (4 geographic areas × 3 minority densities).
6.3. Sampling census blocks
Based on available data, we sampled 10% of the low-density strata, 15% of the high-density black strata, and 75% of the high-density Hispanic strata (the actual number of blocks selected varied by batch to attain the study goals). All census blocks were randomly ordered within each stratum, and blocks were selected sequentially for each batch.
6.4. Sampling households
All New England towns and cities have contiguous boundaries, so that counties are aggregates of towns and cities, with no unincorporated county land. In Massachusetts, every town and city completes an annual household census (known as “street lists”) of all residents aged 17 yr and older (the voter-eligible population). While gender and date of birth are given for the majority of residents, race/ethnicity is not. These lists are computerized in many cities. In order to use the Boston street lists for BACH, two additional items were mapped onto the existing street list: geocoding (using the Maptitude Geographic Information System for Windows by Caliper, Newton, MA, USA) assigned census tract and block numbers to each address and telephone numbers were identified (by a tele-matching service) for about 50% of the individuals on the street list.
Households were identified by grouping individuals with the same address. For multiple-family dwellings and apartment complexes, the separate apartments were sampled. These were identified through telephone screening, Boston Planning Department information, and field verification as needed. A primary contact person was identified for each household, with preference given to an individual with a telephone number. At the beginning of each batch, a sampling code was randomly assigned to each household. The sampling codes used in BACH included, for example, any age-eligible subject or any minority male subject. These sampling codes were used to subsample households to reach our target goals of equal sample sizes in the 24 design cells.
6.5. Resulting sample and completion rates
The final sample, by design cell, is provided in Table 1. A total of 5506 subjects were recruited (2301 males, 3205 females). The sample balance across the three race/ethnic groups is excellent (1770 black, 1859 Hispanic, 1877 white).
Venous blood samples (20 ml) have been obtained from 3753 BACH subjects (1897 males, 1856 females), comprising 68% of subjects who completed interviews. These samples are frozen at −57°C at Children's Hospital Medical Center Research Laboratories in Boston (Dr. Nader Rifai, Director).
Completion rates are measured at both the household and individual level. An interview at the household level indicates that the household screening was successfully completed. An interview at the individual level indicates that a BACH interview was successfully completed. The contact rate indicates the percent of households/individuals that we were successfully able to contact. The cooperation rate is the percent of those contacted who completed the screening/interview. The response rate is the percent of those we attempted to contact that completed the screening/interview. The refusal rate is the percent of those we attempted to contact who refused to complete the screening/interview. Table 2 summarizes completion rates for the BACH survey after up to 16 diligent attempts to reach subjects.
Table 2.
Various rates of completion for the BACH survey, all batches
| Disposition | Household level | Individual level | ||
|---|---|---|---|---|
| N | N | |||
| Total sampled (S) | 32,937 | 10,009 | ||
| Contacted (C) | 24,063 | 9066 | ||
| Eligible (E) | 22,029 | 8702 | ||
| Interviewed (I) | 12,020 | 5506 | ||
| Contact ratea | 66.0% | 90.6% | ||
| Cooperation ratea | 54.6% | 63.3% | ||
| Response ratea | 36.0% | 57.3% | ||
| Refusal ratea | 30.0% | 33.3% | ||
Rates were calculated as follows: contact rate = C/S; response rate = I/(E + E*); cooperation rate = I/E; refusal rate = (E − I)/(E + E*), where E* = [(S − C)E]/C (AAPOR, 2005: Standard Definition: Final Dispositions of Case Codes and Outcome Rates for Surveys).
Epidemiological studies, especially those focusing on urologic issues, have multiple challenges that affect the completion rates that can be achieved, and these may be of interest to colleagues planning future studies. There is a historical decline in response rates on U.S. epidemiological surveys. Cell phones are replacing conventional landlines, and increasingly U.S. households have unlisted numbers and message machines. Urologic health is a “hard sell,” especially among young adults with few apparent urologic symptoms. Inner-city populations, especially minorities, are suspicious of “outside” researchers (despite employing a multiracial/ethnic field staff). The protocol was time-consuming (2+ h), often conducted early in the morning for males (to control diurnal hormone variation), and required a venous blood draw. “Do-not-call” legislation was widely discussed and introduced in the United States at the height of the fieldwork, and field screening calls are often confused with telemarketing. Many inner-city residents have two or even three jobs and are seldom at home for a field visit. Older subjects are often advised to “Never let strangers into your home” and “Never sign anything,” and BACH required an in-home interview and signed informed consent. Finally, BACH asked very personal questions (eg, bladder control and testicular pain), which some subjects found embarrassing, especially older Hispanic males.
The BACH team appreciates the scientific importance of response rates in epidemiological field studies, and diligent efforts were made to obtain the best yield possible. The BACH baseline completion rate (63.4% of successfully contacted and eligible subjects) is consistent with the rates achieved on comparable epidemiological field studies (eg, the Massachusetts Male Aging Study) with a similar field protocol (lengthy in-home interview, early morning blood draw, anthropometric measurements, sensitive questioning, and, often, bilingual interviewing). Whether the BACH sample is representative of the Boston population and results can be generalized to the U.S. population is discussed below.
6.6. Field logistics
Every attempt was made to establish a close relationship with the inner-city Boston community. BACH staff participated in community and neighbourhood events and health fairs. We established a community advisory board, comprised of local community leaders and representatives of local churches and community health centres, which convened regularly at community sites to review progress and recommend changes designed to improve recruitment and increase the impact of study findings. A local minority-owned small business was contracted to prepare culturally appropriate publicity: BACH posters were displayed on public transportation and brochures were distributed throughout the community (eg, at convenience stores, beauty parlours, and barber shops). The complex recruitment process for eligible BACH subjects involved an introductory letter to each selected household (up to three letters are sent to households without working telephone numbers to request a contact number); telephone screening with a member of the household (at least 10 attempts at different times of the day from 09:00 to 21:00, on different days of the week, including weekends and secondary holidays); and in-person screening by New England Research Institute staff of each age-eligible member of the household (up to three attempts are made through visits to the home). These multiple attempts to contact potential subjects result in one of four outcomes, the household or individual: (1) could not be contacted for screening; (2) is found to be ineligible; (3) is eligible but refuses to participate (reasonable attempts are made to convert initial refusals); (4) is eligible and enrolled and scheduled for an in-person 2-h interview (usually conducted in the subject's home). In summary, up to 16 separate attempts, using different modes (mail, telephone, in-person), are made to reach potential BACH subjects.
To be eligible for BACH, a person must be a member of the randomly selected household; be of a race/ethnicity and gender compatible with the household's sampling code; be between the ages of 30[en]79 yr; be competent to provide signed informed consent; and speak English or Spanish well enough to complete the study. As is common in many studies, participants received $100 as a token of appreciation for their willingness to participate in the study and to partially compensate for their 2+ h contribution. Individuals found to have worrisome health problems (eg, seriously elevated blood pressure, prolactin, cholesterol values, or depression) received a personalized letter and/or telephone call recommending they contact their primary care provider. Those lacking health insurance (approximately 16%) were eligible for care at Boston Medical Center (through the city's free pool).
7. Representativeness and generalizability
We compared the BACH sample with another survey of Boston residents (the Behavioral Risk Factor Surveillance System, sponsored by Centers for Disease Control and Prevention) to check whether BACH is representative of Boston. The only difference is that BACH males were less likely to be employed. To determine whether BACH results can be generalized to the U.S. population as a whole, we compared our sample with three different government-sponsored national surveys (the National Health and Nutrition Examination Survey, the National Health Interview Survey, and the National Behavioral Risk Factor Surveillance System) on many different sociodemographic and health-related variables. The only difference in health-related variables is that there is more asthma in Boston than nationwide, suggesting that with appropriate adjustments BACH results are potentially generalizable to the U.S. population as a whole (detailed comparative data are available at www.neriscience.com).
8. Towards the future: a prospective cohort study
There are plans to transition the BACH study from a cross-sectional to a prospective cohort design, the BACH Cohort Study. In anticipation of this activity, measures have already been taken to ensure continuing high rates of cooperation from the BACH subjects, as described above. Subjects report participation as a positive experience, and considerable goodwill and even commitment to BACH has been established. Results of an effort in 2006 to again contact and interview the first 500 subjects (first interviewed in 2002) reveal that over 84% of baseline subjects can be interviewed again. Only 19 (4%) of these initial 500 subjects have refused future participation.
A shift from a cross-sectional to a prospective cohort design permits an evolution in focus: from a static cross-sectional survey of urologic symptoms to a dynamic longitudinal study of the trajectory of these symptoms [8]. The BACH cohort study will examine the trajectory of urologic symptoms: their incidence (and risk factors), health care seeking and utilization, direct and indirect costs, and consequences for quality of life/functioning. A prospective (longitudinal) study also provides an opportunity to check the robustness of baseline findings (associations) and facilitates understanding of physiologic pathways (disease processes).
The BACH sampling scheme dictated that members of smaller demographic subpopulations would be enrolled in numbers roughly equal to those from larger subpopulations. This design feature provides enhanced statistical power to demonstrate population trends in urologic conditions/symptoms within and across ages and races/ethnicities. A consequence of this approach, however, is that the statistical power achieved in estimating overall population parameters is somewhat less than would be suggested by the total number of subjects [9], due to the fact that, in analyses adjusted to be representative of the underlying population, BACH subsamples contribute information in rough proportion to the size of the subpopulations from which they are drawn.
For a smaller study this could prove to be a fatal limitation, particularly given the loss to follow-up that is an unavoidable feature of large-scale, community-based prospective studies. By contrast, the BACH study's generous baseline sample size[em]coupled with the attention the BACH team is devoting to subject retention, as described above[em]will permit longitudinal analyses to overcome this difficulty. Assuming an 80% follow-up rate among living subjects and overall mortality of 5% between BACH baseline and follow-up, we project that the BACH Cohort Study will obtain data on approximately 4130 subjects. This insures that the BACH Cohort Study will provide stable estimates of incidence rates for urologic conditions/symptoms, while achieving adequate power to address the other questions described above. For instance, given a urologic symptom/condition with a BACH baseline prevalence of 15% and true (but currently unknown) overall population incidence of 1% per year, a 5-yr follow-up would provide data on approximately 170 incident cases over nearly 17,000 person-yr of risk (and a greater number of cases of conditions/symptoms for which older or minority subjects are at elevated risk). Even given the anticipated reductions in statistical power due to unequal sampling probabilities [9], these data would be adequate to estimate, with 95% confidence, the population incidence of the relevant symptom/condition to within ± 4 cases per 1000 person-yr.
9. Conclusion
BACH is an epidemiological survey of urologic symptoms, not a study of urologic diseases. This feature is a departure from many other studies that use self-reports of diagnosed disease states, presuming that most of those experiencing symptoms have access to the health care system and obtain an appropriate diagnosis. That people suffer from urologic symptoms (eg, “the presence of burning, pain, discomfort, or pressure in the pubic or bladder area”) rather than from a diagnostic label is not an arcane point. Disease labels such as “urinary incontinence,” “benign prostatic hyperplasia,” and “interstitial cystitis/painful bladder syndrome” are variably applied by providers to some constellation of symptoms often experienced by individuals and sometimes presented for treatment. Every publication and presentation from BACH is required to emphasize that it is “a survey of symptoms suggestive of urologic disease,” and in no way an attempt to use symptom questionnaires to diagnose urologic conditions[em]which requires physical examination, history taking, and often cystoscopic testing and urodynamic studies.
The BACH study is improving our understanding of the epidemiology of a range of urologic symptoms/conditions. Planned longitudinal follow-up of the BACH subjects will provide needed incidence data, identify predictors/precursors of subsequent urologic symptoms, and facilitate understanding of the natural progression (and remission) of urologic symptomatology. Such understanding is required before effective screening, primary prevention, and treatment strategies for urologic disease can be developed. This is becoming particularly relevant as the U.S. population ages, greatly increasing the number of Americans affected by urologic disorders.
Acknowledgements
Many individuals made valuable contributions to the success of the BACH study: program officials at the NIDDK (National Institutes of Health), Paul Eggers, John Kusek, and Leroy Nyberg; members of a scientific advisory board, Richard Alexander (University of Maryland), Michael Barry (Massachusetts General Hospital, Harvard University), Jeanette Brown (University of California, San Francisco), Elizabeth Calhoun (Northwestern University Medical School), Quentin Clemens (Northwestern University, Feinberg School of Medicine), Geoffrey Cundiff (Johns Hopkins University), Gary Curhan (Channing Laboratory, Harvard University), Steve Jacobsen (Mayo Medical School, Minnesota), Kathleen Propert (University of Pennsylvania Medical Center), and Chris Robertson (Strathclyde University, Glasgow, Scotland); scientific staff at the New England Research Institutes, Varant Kupelian, Heather Litman, Thomas Travison, Andre Araujo, Sharon Tennstedt, Karen Lutfey, and Amy O'Donnell. Finally, we thank the BACH subjects: we are deeply indebted to the 5506 people who kindly agreed to participate and who remain dedicated to the continued success of the BACH study.
Funding sources: This work was supported by a grant from the National Institute of Diabetes and Digestive and Kidney Disorders (DK56842)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Take Home Message
The Boston Area Community Health Study, a random sample (n = 5506) of females and males, aged 30[en]79 years, equally divided across race/ethnic groups, is estimating the true prevalence, correlates, and impact of symptoms suggestive of eight urologic conditions.
References
- 1.Last J. The clinical iceberg. Lancet. 1963;2:28–30. [Google Scholar]
- 2.U.S. Census Bureau Population Division Population Projections Branch http://www.census.gov/population/www/projections/natsum-T3.html. Accessed 1 March 2004.
- 3.National Institutes of Health . National Institute of Diabetes and Digestive and Kidney Diseases workshop on chronic prostatitis: summary statement. U.S. Department of Health and Human Services; Bethesda, MD: 1995. [Google Scholar]
- 4.Kupelian V, Wei JT, O'Leary MP, et al. Prevalence of lower urinary tract symptoms (LUTS) and effect on quality of life in a racially and ethnically diverse random sample: the Boston Area Community Health (BACH) survey. Arch Int Med. 2006;166:2381–7. doi: 10.1001/archinte.166.21.2381. [DOI] [PubMed] [Google Scholar]
- 5.Clemens JQ, Link CL, Kusek J, Nyberg LM, McKinlay JB. The effect of varying definitions on the prevalence of interstitial cystitis (IC)/painful bladder syndrome (PBS) in a racially and ethnically diverse sample. J Urol. 2007;177(4) [Google Scholar]
- 6.Cochran WG. Sampling techniques. 3rd ed. John Wiley & Sons; New York: 1977. [Google Scholar]
- 7.Kish L. Survey sampling. John Wiley & Sons; New York: 1965. [Google Scholar]
- 8.Emberton M. Definition of at-risk patients: dynamic variables. BJU Int. 2006;97(Suppl 2):12–15. doi: 10.1111/j.1464-410X.2006.06099.x. [DOI] [PubMed] [Google Scholar]
- 9.Kish L. Sampling organizations and groups of unequal sizes. Amer Sociol Rev. 1965;30:364–72. [PubMed] [Google Scholar]


