Abstract
Background
There is uncertainty regarding the frequency of adverse events while on a surgical waiting list. We assess the relationship between the duration of wait for cholecystectomy and the risk of emergency admission.
Methods
We analyzed time to emergency admission in a group of 761 patients who underwent cholecystectomy after being seen in clinic for biliary colic and placed on waiting lists at 2 acute care centres in Ontario, from 1997 to 2000.
Results
Emergency admissions due to worsening symptoms occurred in 51 patients (6.7%) waiting for elective cholecystectomy. The weekly rate of emergency admission was low during the first 19 weeks on the list, but increased almost by a factor of 3 after 20 weeks (rate ratio 2.7; 95% confidence interval 2.0–3.7). Relative to the first 4 weeks on the list, the rate was 1.6 times higher after 20 weeks, 2 times higher after 28 weeks and 7 times higher after 40 weeks.
Interpretation
The probability that a patient on a waiting list will be admitted for emergency cholecystectomy consistently increases with the duration of wait, particularly after 20 weeks.
Waiting lists are a common tool for managing access to elective surgery.1 However, little evidence is available on the health impact of delaying surgery for various conditions.2,3,4 Other than mortality, adverse events experienced by patients while on a waiting list have not been systematically examined.5 Without these data, appropriate access time for surgery must be determined on the basis of expert opinion.6
When treatment is delayed, the condition of a patient on a surgical waiting list may deteriorate and require urgent medical attention. In this case, emergency admission for the awaited procedure may be regarded as an adverse effect of waiting. Also, routine operating room activity may be seriously disrupted by unexpected nonelective admissions of patients on waiting lists.7
In patients with biliary colic caused by cholelithiasis, extended treatment delays may increase the probability that the patient will be admitted for delayed cholecystectomy as an emergency case. Emergency admission may be associated with more frequent or more severe attacks of biliary colic or other biliary complications such as acute cholecystitis, obstructive jaundice, cholangitis or pancreatitis.8 However, little is known about the relationship between time spent on a waiting list and the risk of emergency admission in these patients.
We describe the distribution of times spent waiting for the operation and assess the relationship between waiting-list times and the risk of emergency admission.
Methods
The Department of Surgery, Queen's University, is housed at 2 tertiary referral centres that provide services to more than 500 000 residents of southeastern Ontario.
Eight general surgeons perform cholecystectomy. There is no priority ranking system. Each surgeon's office operates its waiting list independently.
Surgeons on call made the decision to operate on patients who presented to the emergency department by evaluating (a) the clinical presentation for symptoms of increased pain or fever and signs of persisting or worsening abdominal tenderness, guarding or rebound or (b) the ultrasonographic finding of a thick-walled gallbladder with pericholecystic fluid or a positive finding of hepatobilary iminodiacetic acid on radionuclide scan or (c) both (a) and (b).
Data on the timing and type of surgery were retrieved from the electronic hospital information system. We identified all adult patients who underwent emergency or elective cholecystectomy from 1997 to 2000 after being seen in clinic for biliary colic. Information on the date of the consultation visit was obtained from patient records through the quality assurance program at the Department of Surgery. Patients who underwent emergency surgery without a prior clinic appointment were not included. All cholecystectomies were initially attempted as laparoscopic procedures. Conversion to the open procedure was required when the dissection was not technically feasible or safe. Forty-one patients were excluded from the analysis because they had immediate (within 3 days) access to planned surgery, leaving a study group of 761.
The primary outcome was emergency admission for cholecystectomy due to the worsening of symptoms while awaiting elective surgery. A waiting-list time was calculated for each patient based on the number of weeks from the last consultation visit to elective or emergency surgery. This approach assumes the last visit before surgery is the date when the decision to operate was made.9
Cumulative probability of undergoing surgery electively as a function of the waiting-list time was estimated by the product-limit method, with emergency cases being treated as censored observations.10,11 To calculate the average weekly emergency rate among waiting patients, we divided the number of emergency admissions by the total number of patient-weeks on the list. To determine if the risk of emergency admission varied with the duration of the wait, the rate was calculated for the following 7 intervals of time on the waiting list: less than 4, 4–7, 8–11, 12–19, 20–27, 28–39 and 40–52 weeks. Because the population at risk decreases over time, the later time intervals were increased so that they would include a sufficient number of events. For each interval of waiting time, crude rate ratios were estimated relative to the first 4 weeks using the Poisson regression.12 Age decade, sex, enrolment period and the surgeon's annual volume of cholecystectomies were entered as independent variables in multivariate regression to obtain adjusted rate ratios. The conditional probability of an emergency admission was estimated for the 7 waiting-list intervals as the number of admissions during a given interval among patients who had waited until the beginning of the interval.
Results
Elective admission
Elective patients spent a total of 5712 person-weeks waiting to be admitted. The average weekly number of elective operations was 12.4 (95% confidence interval [CI] 11.6–13.3) per 100 patients on the list. The rate differed across enrolment periods, from 10.3 (9.1–11.5) in fiscal year 1997/98 to 15.1 (13.4–16.9) in fiscal year 1998/99 to 13.2 (11.5–15.0) in fiscal year 1999/2000. The median length of stay on the list was 6 weeks. However, there was considerable variation in individual waiting times. The probability of undergoing elective surgery increased rapidly from 25% within 3 weeks of the last clinic visit to 50% at 6 weeks and 75% at 10 weeks, and then gradually reached a plateau. Although 90% of patients underwent surgery by 17 weeks, the remaining 10% waited another 1 to 3 weeks (total 18–52 weeks) for their operation. Surgeons with a low volume of cholecystectomies (less than 20 per year) operated on the majority of patients with extended delays. In general, low-volume surgeons had a primary interest in surgical oncology. This may explain the order in which their patients accessed cholecystectomy during the waiting period.
Emergency admission
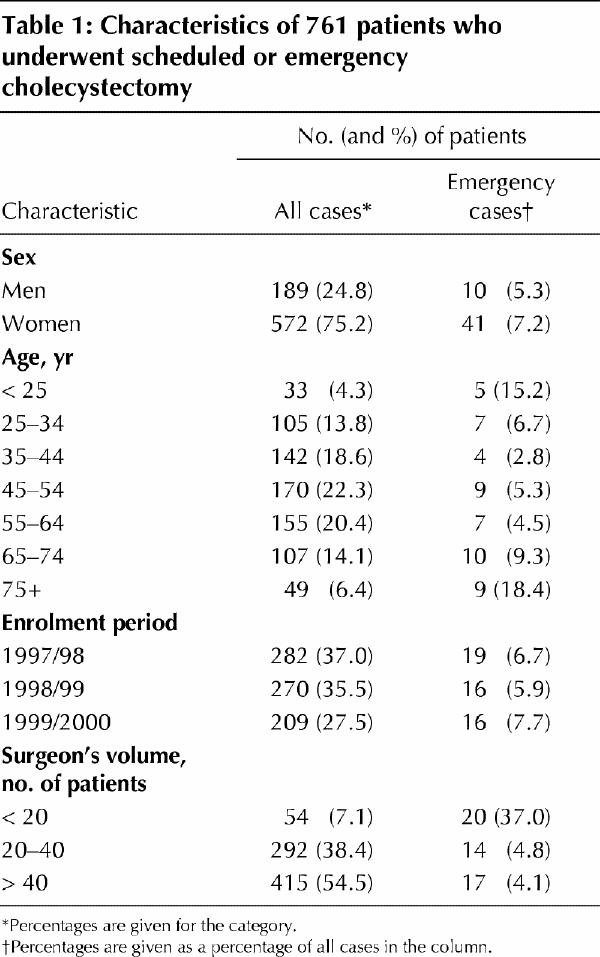
Overall, 51 patients (6.7%) waiting for elective cholecystectomy had emergency admissions. The proportion varied significantly across the categories of patient and service characteristics (Table 1). Women, the youngest (less than 25 years) and oldest (more than 75 years) groups, and patients enrolled in fiscal year 1999/2000 and operated on by lower-volume surgeons were admitted as emergency cases more often.
Table 1
The average weekly emergency admission rate of patients on the waiting lists was 0.9 (95% CI 0.7–1.2) per 100 patients. Table 2 shows that the weekly emergency admission rate increased from 0.8 to 5.7 per 100 patients from the first 4 weeks to the interval of 40–52 weeks. When adjusted for sex, age, enrolment period and surgeon volume, the emergency admission rate was more than 1.5 times higher after 20 weeks, 2 times higher after 28 weeks and 7 times higher after 40 weeks relative to the first 4 weeks of waiting-list time.
Table 2
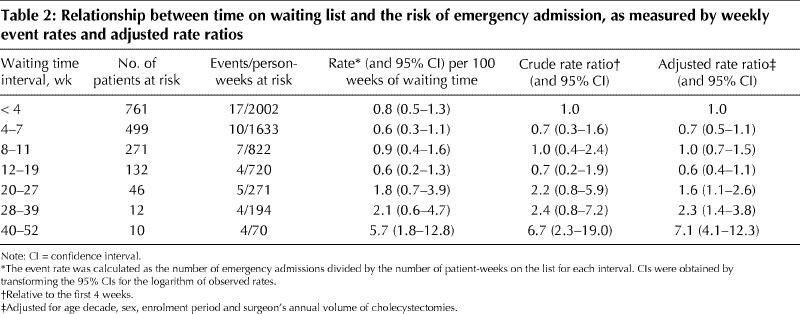
Figure 1 shows the conditional probability of emergency admission during the 7 waiting-list intervals compared with the corresponding figures for elective admission. Although the probability of emergency admission during the first 19 weeks was low, after 20 weeks the probability started increasing and approached 40% in the interval of 40–52 weeks. Of 46 patients who waited for more than 20 weeks, 28% were admitted as emergency cases, compared with 5% of those who waited less than 20 weeks (715 patients). The average weekly rates were 2.4 (95% CI 1.3–4.0) and 0.7 (95% CI 0.5–1.0) per 100 patients in these 2 groups, respectively, with the adjusted rate ratio being 2.7 (95% CI 2.0–3.7).
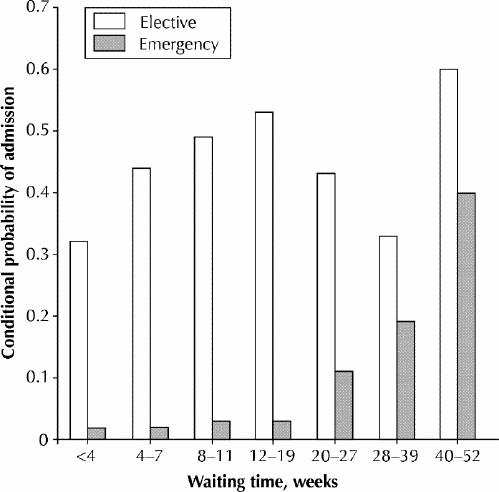
Fig. 1. Probabilities of elective and emergency admission by different intervals of time on the waiting list, conditional on remaining on the list until the start of each interval.
Discussion
We assessed the risk of emergency surgery among patients awaiting elective cholecystectomy in relation to the duration of the wait and found that patients waiting 20 weeks or more were more likely to undergo emergency admission than those waiting shorter times after adjustment for sex, age, enrolment period and surgeon volume. Other studies concerned with waiting for elective cholecystectomy reported on waiting times,9,13 return visits to the emergency department,14 worsening symptoms8 and the morbidity associated with long waits.15 However, the frequency of emergency admission for patients with biliary colic who were on a waiting list for cholecystectomy has not been previously described.
The retrospective nature of our data may be considered an important limitation of the study. Prospective studies examine how long patients accepted for treatment wait for surgery, whereas retrospective studies examine how long the patients who were admitted were required to wait after enrolment.16 If every wait ended in admission, the 2 study designs would generate equivalent results. However, patients accepted for treatment may expect to be removed from the waiting list for reasons other than admission.17 If patients removed from the list without surgery are not accounted for, the estimated probabilities of undergoing treatment may be biased toward a higher rate.18 Also, our analysis lacks data on coexisting diseases. In general, a large number of comorbid conditions may prevent aggressive treatment. Therefore, given its possible association with delay in treatment, comorbidity is a potentially confounding factor for the observed relationship between time on the waiting list and emergency admission.
In this study we used emergency cholecystectomy for worsening symptoms as a readily identifiable consequence of delay in surgical treatment. This type of adverse event should be examined for other surgical procedures. Clinical conditions that may require emergency surgery while patients are on a waiting list include inguinal hernia, spinal cord conditions, abdominal aortic aneurysm or the need for coronary artery bypass grafting, among others. Our results have implications for developing waiting-time limits for elective surgery. The findings suggest that patients with biliary colic awaiting elective cholecystectomy for longer than 20 weeks have a substantially increased risk for development of acute symptoms that require an emergency operation.
Footnotes
This article has been peer reviewed.
Contributors: Drs. Sobolev, Mercer, Brown and Jalink were responsible for study concept and design and contributed to data analysis and interpretation. Dr. FitzGerald also contributed to data analysis and interpretation. Mr. Shaw assisted with linking cases to hospital databases and contributed to data analysis. All authors were involved in the writing of the manuscript and reviewed and approved the final version.
Competing interests: None declared.
Correspondence to: Dr. Boris Sobolev, Research Pavilion, 828 West 10th Ave., Vancouver BC V5Z 1L8; fax 604 875-5179; sobolev@interchange.ubc.ca
References
- 1.Naylor CD. A different view of queues in Ontario. Health Aff (Millwood) 1991;10:110-28. [DOI] [PubMed]
- 2.McGurran J, Noseworthy T. Improving the management of waiting lists for elective healthcare services: public perspectives on proposed solutions. Hosp Q 2002;5:28-32. [DOI] [PubMed]
- 3.Turnbull RG, Taylor DC, Hsiang YN, Salvian AJ, Nanji S, O'Hanley G, et al. Assessment of patient waiting times for vascular surgery. Can J Surg 2000;43:105-11. [PMC free article] [PubMed]
- 4.Derrett S, Paul C, Morris JM. Waiting for elective surgery: effects on health-related quality of life. Int J Qual Health Care 1999;11:47-57. [DOI] [PubMed]
- 5.Morgan CD, Sykora K, Naylor CD. Analysis of deaths while waiting for cardiac surgery among 29293 consecutive patients in Ontario, Canada. Heart 1998;79:345-9. [PMC free article] [PubMed]
- 6.Naylor CD, Basinski A, Baigrie RS, Goldman BS, Lomas J. Placing patients in the queue for coronary revascularization: evidence for practice variations from an expert panel process. Am J Public Health 1990;80:1246-52. [DOI] [PMC free article] [PubMed]
- 7.Buhaug H. Long waiting lists in hospitals. BMJ 2002;324:252-3. [DOI] [PMC free article] [PubMed]
- 8.Friedman GD. Natural History of asymptomatic and symptomatic gallstones. Am J Surg 1993;165:399-404. [DOI] [PubMed]
- 9.DeCoster C, Carriere KC, Peterson S, Walld R, MacWilliam L. Waiting times for surgical procedures. Med Care 1999;37:JS187-JS205. [DOI] [PubMed]
- 10.Hosmer DW Jr, Lemeshow S. Descriptive methods for survival data. In: Applied survival analysis: regression modeling of time to event data. New York: John Wiley & Sons; 1998. p. 27-86.
- 11.Altman DG, Bland JM. Time to event (survival) data. BMJ 1998;317:468-9. [DOI] [PMC free article] [PubMed]
- 12.Holford TR. The analysis of rates and of survivorship using log-linear models. Biometrics 1980;36:299-305. [PubMed]
- 13.Olson DW, de Gara CJ. How long do patients wait for elective general surgery? Can J Surg 2002;45:31-3. [PMC free article] [PubMed]
- 14.Rutledge D, Jones D, Rege R. Consequences of delay in surgical treatment of biliary disease. Am J Surg 2000;180:466-9. [DOI] [PubMed]
- 15.Cheruvu CV, Eyre-Brook IA. Consequences of prolonged wait before gallbladder surgery. Ann R Coll Surg Engl 2002;84:20-2. [PMC free article] [PubMed]
- 16.Armstrong PW. Unrepresentative, invalid and misleading: are waiting times for elective admission wrongly calculated? J Epidemiol Biostat 2000;5:117-23. [PubMed]
- 17.Sobolev B, Brown P, Zelt D. Variation in time spent on the waiting list for elective vascular surgery: a case study. Clin Invest Med 2000;23:227-38. [PubMed]
- 18.Sobolev B, Brown P, Zelt D, Shortt S. Bias inherent in retrospective waiting-time studies: experience from a vascular surgery waiting list. CMAJ 2000;162:1821-2. [PMC free article] [PubMed]


