Abstract
Background. Cholangitis requires bactibilia and increased biliary pressure. Pancreatitis may be initiated by elevated intraductal pressure. The sphincter of Oddi regulates pancreatobiliary pressures and prevents reflux of duodenal contents. However, following biliary bypass or pancreatoduodenectomy, increased intra-abdominal pressure may be transmitted into the bile ducts and/or pancreas. The aim of this analysis is to document that cholangitis or pancreatitis may be exercise-induced.
Methods. The records of patients with one or more episodes of cholangitis or pancreatitis precipitated by exercise and documented to have patent hepatico- or pancreatojejunostomies were reviewed. Cholangitis was defined as fever with or without abdominal pain and transiently abnormal liver tests. Pancreatitis was defined as abdominal pain, with transient elevation of serum amylase and documented by peripancreatic inflammation on computerized tomography.
Results. Twelve episodes of cholangitis occurred in six patients who had undergone hepaticojejunostomy for biliary stricture (N=3), Type I choledochal cyst (N=2), or pancreatoduodenectomy for renal cell carcinoma metastatic to the pancreas (N=1). Four episodes of pancreatitis occurred in two patients who had undergone pancreatoduodenectomy for ampullary carcinoma or chronic pancreatitis. Workup and subsequent follow-up for a median of 21 months have not documented anastomotic stricture. Each episode of cholangitis and pancreatitis was brought on by heavy exercise and avoidance of this level of exercise has prevented future episodes.
Conclusion. Following biliary bypass or pancreatoduodenectomy, significant exercise may increase intra-abdominal pressure and cause cholangitis or pancreatitis. Awareness of this entity and behavior modification will avoid unnecessary procedures in these patients.
Keywords: Cholangitis, exercise-induced, pancreatitis, postoperative
Introduction
Acute cholangitis occurs when biliary pressures are increased and bacteria are present in the biliary tract. In this setting, bacteria can reflux into the systemic circulation via the hepatic veins and perihepatic lymphatics and cause bacteremia and/or septicemia 1. The classic clinical picture, as described by Charcot, is that of fevers and chills, right upper abdominal pain, and jaundice 2. In addition, laboratory findings of elevated white blood cell count, bilirubin, transaminases, and alkaline phosphatase support the diagnosis 3,4. The spectrum of severity can range from subclinical to life threatening with septic shock and mental obtundation 5. The etiologies of acute cholangitis include clinical entities that cause biliary obstruction, such as choledocholithiasis, benign stricture, malignancy, and postoperative anastomotic stricture 6.
Pancreatitis, like cholangitis, can be initiated by elevated intraductal pressures. The most common etiologies include gallstone impaction, alcohol, hyper-lipidemia, hypercalcemia, and medications 7. The typical clinical picture includes epigastric abdominal pain, associated with nausea, vomiting, and elevated pancreatic enzymes. With normal anatomy, the sphincter of Oddi regulates the pressure of the biliary and pancreatic ductal systems and prevents the reflux of duodenal contents 8. In patients who have had either biliary bypass or pancreatoduodenectomy, the sphincter has been circumvented, resulting in loss of the above-mentioned regulation. In that setting, significant increases in intra-abdominal pressure may transmit both the elevated pressure and gastrointestinal contents into the pancreatobiliary ductal systems and cause cholangitis or pancreatitis. Therefore, the aim of this analysis is to document that cholangitis or pancreatitis may be caused by an exercise-induced increase in abdominal pressure in the absence of a strictured anastomosis in patients whose sphincter of Oddi has been removed or bypassed.
Methods
Patient population
A series of eight patients who had previously undergone hepatico- or pancreaticojejunostomy at the Froedtert Memorial Hospital/Medical College of Wisconsin over a 7-year period from 1998 to 2004, and had one or more episodes of postoperative cholangitis or pancreatitis precipitated by exercise, was analyzed. All patients were evaluated for patent biliary-enteric or pancreato-enteric anastomosis as well as small bowel obstruction. Patients with a strictured anastomosis or distal small bowel obstruction as the cause of cholangitis or pancreatitis were excluded from this analysis. The demographic, clinical, and laboratory data were obtained from both hospital and outpatient records. Institutional Review Board (IRB) approval was obtained for this analysis.
Cholangitis/pancreatitis
Cholangitis was defined as fever and chills with or without the presence of abdominal pain, along with transiently elevated serum liver function tests. Pancreatitis was defined as abdominal pain associated with elevation of serum amylase and/or lipase and documented by peripancreatic inflammation on computed tomography (CT) scans.
Follow-up
Follow-up and survival information was obtained from clinic notes, inpatient records, and the Social Security Death Index database. Patients were all counseled on behavior modification during clinic visits and subsequently followed for any additional episodes of cholangitis or pancreatitis.
Results
Cholangitis
Cholangitis occurred in six patients who had surgery that bypassed or removed the sphincter of Oddi, was precipitated by strenuous activity, and had a patent, non-strictured, biliary-enteric anastomosis (Table I). Two of these six patients had a type I choledochal cyst and underwent cyst resection along with Roux-y-hepaticojejunostomy. One of these two had a history of cholangitis prior to surgery secondary to the choledochal cyst. Both of these patients experienced one episode of cholangitis following heavy exercise. Patient 2 had her episode after lifting a heavy box of canned tomatoes (Figure 1) and cholangitis was precipitated by moving heavy furniture in Patient 4. The other four patients with postoperative cholangitis, Patients 1, 3, 5, and 6, had a right hepaticojejunostomy, a Roux-y-choledochojejunostomy, a Roux-y-hepatico-jejunostomy, and a pancreatoduodenectomy, respectively. The indications for surgery in these patients were a right hepatic duct stricture, chronic pancreatitis, a common hepatic duct stricture, and a metastatic renal cell carcinoma, respectively. Only Patient 5 exhibited any cholangitis preoperatively. Patient 1 had five episodes of exercise-induced cholangitis, most notably occurring after lifting a heavy wheelbarrow, but all related temporally to heavy gardening activity. Patient 3 had three episodes after heavy exercise while Patients 5 and 6 each had one episode, also after working out and heavy lifting. These 12 episodes of cholangitis occurred an average of 27 months after surgery. All patients were studied with ultrasound, cholescintigraphy, and/or computed tomography, and none were found to have evidence of an anastomotic stricture or bowel obstruction. Follow-up since the last episode averaged 32 months, and liver function tests have been stable in all six patients.
Table I. Cholangitis population.
| Cholangitis |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Age (years) | Gender | Diagnosis | Surgery | Pre-op | Post-op | Activity | Episodes | Time after surgery (months) | Follow-up (months) |
| 1 | 62 | M | Right hepatic duct stricture | Right hepaticojejunostomy | No | Yes | Lifting a wheelbarrow, gardening | 5 | 3, 20, 34, 44, 67 | 9, 32, 42, 56, 73 |
| 2 | 38 | F | Choledochal cyst Type I | Cyst resection Roux-y-hepatico-jejunostomy | No | Yes | Lifting box of tomato cans | 1 | 35 | 12 |
| 3 | 68 | M | Chronic pancreatitis | Roux-y-choledochol-jejunostomy | No | Yes | Heavy exercise | 3 | 5, 26, 28 | 13, 15,36 |
| 4 | 38 | M | Choledochal cyst Type I | Cyst resection Roux-y-hepatico-jejunostomy | Yes | Yes | Moving furniture | 1 | 3 | 57 |
| 5 | 46 | M | Common hepatic duct stricture | Hepatico-jejunostomy | Yes | Yes | Working out | 1 | 32 | 10 |
| 6 | 65 | M | Metastatic renal cell carcinoma | Pylorus-preserving pancreatoduodenectomy | No | Yes | Heavy lifting | 1 | 27 | 29 |
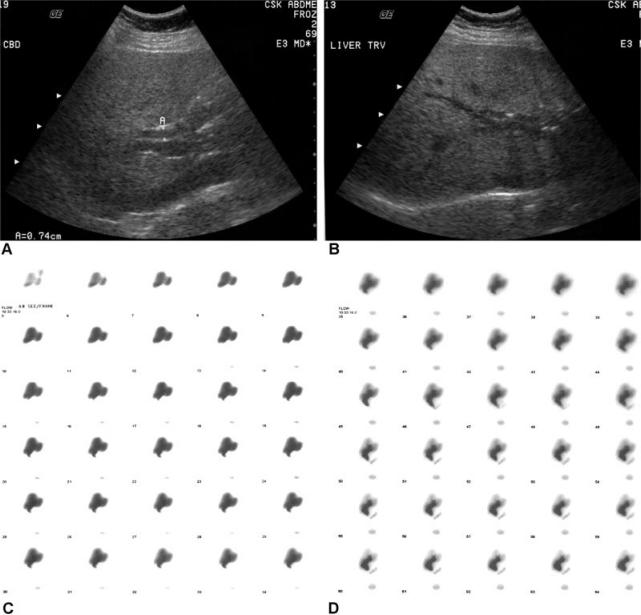
Figure 1A, IB, 1C, 1D. .
Patient 2 is a 38-year-old female, with a Type I choledochal cyst, who underwent resection and hepaticojejunostomy in May 2000. She presented 35 months after surgery with fevers, chills, and abdominal pain. Her pain began a few hours after lifting several boxes of canned tomatoes. The white blood cell count, aspartate aminotransferase (AST), and alanine aminotransferase (ALT) were all transiently elevated. Workup revealed a normal ultrasound and HIDA scan. The patient was treated with oral antibiotics and counseled on avoiding that level of behavior. She has been without any further episodes of cholangitis for 12 months. Ultrasound of the liver shows a patent, non-dilated common hepatic duct at the anastomosis (1A) and likewise a normal, non-dilated biliary tree with visible air (IB). Nuclear Medicine scans show normal hepatic uptake and excretion (1C) followed by appropriate emptying into the jejunum (1D).
Pancreatitis
Pancreatitis occurred in two patients after heavy physical activity following a pancreatic-enteric anastomosis (Table II). Patients 7 and 8 both underwent pylorus-preserving pancreatoduodenectomy for ampullary carcinoma and chronic pancreatitis, respectively. Patient 7 experienced one episode of pancreatitis following heavy exertion, and Patient 8 had three episodes after moving appliances, shoveling large amounts of dirt and other similar extreme activity. These two patients experienced four episodes of pancreatitis a mean of 31 months after surgery. Both of these patients had computed tomography (CT) before, at the time of, and after the episode(s) of pancreatitis (Figure 2). CT evidence of acute pancreatitis was only evident at the time of the acute episode. Subsequent CT scans with a mean follow-up of 18 months have not demonstrated pancreatic ductal dilatation. The degree of exercise that induced the cholangitis or pancreatitis was unusual for these patients. All of the patients were instructed on behavioral modification focusing on limiting activity that is overly strenuous and prolonged in nature.
Table II. Pancreatitis population.
| Cholangitis |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Age (years) | Gender | Diagnosis | Surgery | Pre-op | Post-op | Activity | Episodes | Time after surgery (months) | Follow-up (months) |
| 7 | 47 | F | Ampullary carcinoma | Pylorus-preserving pancreatoduodenectomy | No | Yes | Heavy exertion | 1 | 29 | 21 |
| 8 | 66 | M | Chronic pancreatitis | Pylorus-preserving pancreatoduodenectomy | Yes | Yes | Moving appliances, shoveling dirt | 3 | 26, 32, 36 | 13, 17, 21 |
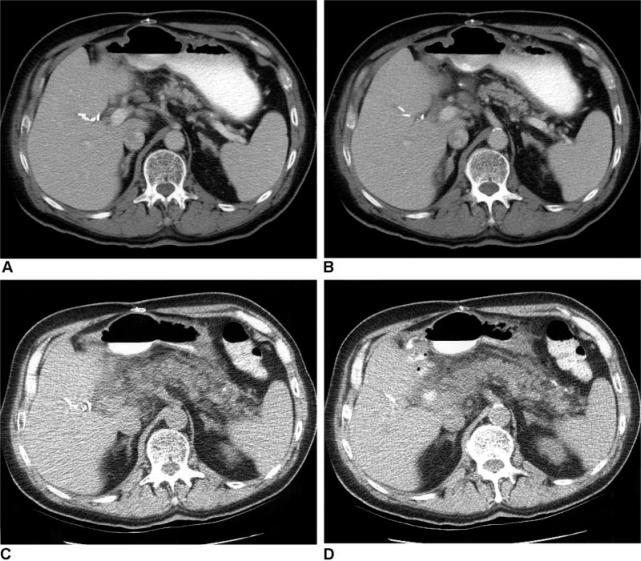
Figure 2A, 2B, 2C, 2D. .
Patient 8 is a 66-year-old male with a history of pancreatoduodenectomy for chronic pancreatitis who has had three episodes of pancreatitis, at 26, 32, and 36 months after surgery. One episode followed moving appliances and one followed shoveling dirt. At his last episode workup revealed a lipase of 3,049 and peripancreatic inflammation but not a dilated pancreatic duct. Following resolution of the pancreatitis, the patient was advised to avoid further heavy physical activity. He has had no further episodes for 13 months. Postoperative CT scan shows an atrophic pancreas with no evidence of inflammation or dilation of the pancreatic duct (2A, 2B). CT scan during pancreatitis episode shows peripancreatic inflammation without a dilated pancreatic duct (2C, 2D).
Discussion
This analysis reports eight patients who had previously undergone surgery where the sphincter of Oddi was bypassed or removed, and exhibited postoperative cholangitis (N = 6) or pancreatitis (N = 2) brought on by strenuous exercise. Twelve episodes of cholangitis occurred in six patients who had undergone a biliary-enteric anastomosis for benign biliary stricture (N = 3), Type I choledochal cyst (N = 2), or renal cell carcinoma (N=l). Four episodes of pancreatitis occurred in two patients who had undergone pancreatoduodenectomy for ampullary carcinoma or chronic pancreatitis. In all eight patients, work-up at the time of cholangitis or pancreatitis did not reveal any evidence of an anastomotic stricture or distal bowel obstruction. Behavior modification has prevented further attacks.
For cholangitis to occur, two elements are required, bactibilia and elevated intraductal pressures 9. The sphincter of Oddi normally functions to prevent the reflux of colonized duodenal contents into the biliary tree and regulates the pressure of the biliary ductal system 8. With normal anatomy and physiology, the pressures in the biliary tree range from 7–14 cmH20 10. Jacobson etal. have shown that at pressures greater than 15 cmH20, radiolabeled bacteria reflux into the systemic circulation 1. Patients with benign biliary strictures, choledochal cysts, or pancreatobiliary tumors require a biliary-enteric anastomosis that circumvents the sphincter of Oddi. In this patient population, postoperative cholangitis can occur most commonly due to a strictured anastomosis, intrahepatic stones, recurrent tumor, or small bowel obstruction 6. In this case report, six patients experienced cholangitis, marked by fevers, chills, and a transient increase in liver function tests, in the absence of a known cause of postoperative cholangitis. In addition, all of these patients related a story of heavy physical activity immediately prior to the episode of cholangitis. In healthy volunteers during Valsalva, intra-abdominal pressure can exceed 200 mmHg 11. Thus, this degree of increase in abdominal pressure, along with a circumvented or missing sphincter of Oddi can cause a bacteremia in these patients. Without any other obvious etiology for these episodes of cholangitis and resolution with changed behavior, an exercise-induced cause is assumed.
In patients who have undergone a pancreatic-enteric anastomosis, postoperative pancreatitis can also occur. The etiology may be the same as the usual causes of acute pancreatitis or related to a strictured pancreatic-enteric anastomosis. The most common causes of pancreatitis in this setting include alcohol, recurrent tumor, an anastomotic stricture, hypertriglyceridemia, hypercalcemia, and medications. Two patients were included in this analysis who experienced postoperative pancreatitis, but lacked any obvious etiology. Similar to the patients with exercise-induced cholangitis, careful history taking documented that their pain occurred shortly after some abnormally heavy physical activity that presumably led to an increase in intraabdominal pressure. In the absence of the sphincter of Oddi, jejunal contents with bile and bacteria may reflux into the pancreatic ductal system, leading to an inflammatory pancreatic response that can be described as exercise-induced pancreatitis.
The 16 episodes of exercise-induced cholangitis or pancreatitis described here did not occur in the setting of ‘routine’ activity for these patients. These patients all described some unusual physical activity that presumably led to an increased abdominal pressure for an extended period. This prolonged elevation in pressure, in combination with bacteria in the bile or jejunal contents, is the precipitating factor for exercise-induced cholangitis and pancreatitis. All of the patients described in this study were counseled on avoidance of this level of activity, with good results for those who were or eventually became compliant.
Following biliary bypass or pancreatoduodenectomy, where the function of the sphincter of Oddi is eliminated, significant exercise may cause elevated intra-abdominal pressures that may eventually lead to cholangitis or pancreatitis. To our knowledge, this etiology of cholangitis or pancreatitis has not been previously described. Awareness of this entity, careful history taking, non-invasive workup, and behavior modification can avoid unnecessary invasive procedures in patients with postoperative, exercise-induced cholangitis or pancreatitis.
Footnotes
Presented at: The World Congress of the International Hepato-Pancreato-Biliary Association, Washington DC, 2–6th June 2004.
References
- 1.Jacobson K, Ellander J, Rosengren B. Cholangiovenous reflux. Acta Chir Scan. 1962;123:316. [PubMed] [Google Scholar]
- 2.Charcot JM. Lecons sur les maladies du fore des voices biliares et des veins. Paris, Faculte de Medicine de Paris. Recuellies et Publices Par. Bourneville et Sevestre;1877. [Google Scholar]
- 3.Saharia PC, Cameron JL. Clinical management of cholangitis. Surg Gynecol Obstet. 1976;142:369. [PubMed] [Google Scholar]
- 4.Thompson JE, Jr, Pitt HA, Doty JE, Coleman J, Irving C. Broad spectrum penicillin as adequate therapy for acute cholangitis. Surg Gynecol Obstet. 1990;171:275. [PubMed] [Google Scholar]
- 5.Reynolds BM, Dargan EL. Acute obstructive cholangitis: A distinct clinical syndrome. Ann Surg. 1959;150:299. doi: 10.1097/00000658-195908000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lipsett PA, Pitt HA. Blumgart LH, Fong Y. WB Saunders; London: 2000. Cholangitis, Surgery of the Liver and Biliary Tract3rd Edition. [Google Scholar]
- 7.Yeo C, Cameron JL. Exocrine Pancreas, Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice16th Edition. In:. WB Saunders, 2001. p. 1112. [Google Scholar]
- 8.Ahrendt S, Pitt HA. Townsend CM, Sabiston DC. WB Saunders; Philadelphia: 2001. Biliary Tract, Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice16th Edn; p. 1776. [Google Scholar]
- 9.Flemma RJ, Flint LM, Osterhout S, Shingleton WW. Bacteriologic studies of biliary infection. Ann Surg. 1967;166:563. doi: 10.1097/00000658-196710000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mallet-Guy P. Value of preoperative manometric and roent- genographic examination in the diagnosis of pathologic changes and functional disturbances of the biliary tract. Surg Gynecol Obstet. 1952;94:385. [PubMed] [Google Scholar]
- 11.Harman EA, Frykman PN, Clagett ER, Kraemer WJ. Intraabdominal and intra-thoracic pressures during lifting and jumping. Med Sci Sports Exerc. 1988;20:195. doi: 10.1249/00005768-198820020-00015. [DOI] [PubMed] [Google Scholar]