Abstract
Activation of hepatic stellate (Ito) cells is a final common pathway of liver fibrosis. The findings presented in this paper indicate that expression of Na+/Ca2+ exchanger (NCX) emerges in rat hepatic stellate cells after activation in vitro during primary culture or in vivo in response to intoxication with CCl4. NCX mRNA became detectable by Northern blot analysis in cultured stellate cells on day 3, as was α-smooth muscle actin, an indicator not only of smooth muscle differentiation but also of stellate cell activation. Western blot analysis showed expression of the exchanger protein in the activated stellate cells. Functional expression of the exchanger, monitored by Ni2+-sensitive, verapamil-insensitive intracellular free Ca2+ increases in response to reduction of extracellular Na+ concentration, became sizable by using Fura-2 in stellate cells by 7 days in culture. Furthermore, increased expression of the exchanger mRNA was found predominantly in stellate cells freshly isolated from the CCl4 model rat of hepatic fibrosis. Thus, it is concluded that NCX expression is closely associated with activation of hepatic stellate cells in vitro and in vivo. Because, even at the whole liver level, increased expression of NCX mRNA became observable after induction of liver fibrosis, it is suggested that NCX expression serves a useful diagnostic marker of liver fibrosis or cirrhosis.
The hepatic stellate cell or Ito cell (also called hepatic lipocyte, fat-storing cell, peri- or parasinusoidal cell) is a nonparenchymal cell of mesenchymal origin and resides in the space of Disse in close contact with hepatocytes on one side and with endothelial cells on the other. The stellate cell is known to be activated during hepatic fibrosis by producing potentially injurious connective tissue components, thereby exerting a pivotal action in the development of liver fibrogenesis (1, 2). Thus, the mechanism of stellate cell activation is of major interest with respect to the pathogenesis and could provide hints for diagnostic and therapeutic intervention in fibrotic liver disease or cirrhosis.
Activation of stellate cells takes place either in vitro during primary culture (3–9) or in vivo by responding to intoxication, inflammation, and injury in the liver (10–13). After activation, stellate cells undergo a series of phenotypic and functional changes from quiescent vitamin A-storing cells to myofibroblast-like cells characterized by diminished retinoid content (9, 14), increased proliferative activity (3, 8, 9, 12), increased production or gene expression of contractile cytoskeletal proteins (5, 7, 12–14, 16) and of extracellular matrix proteins (3, 8, 9, 12, 14), and expression of the ferritin receptor (14). However, the precise mechanism of stellate cell activation is as yet largely unknown.
One of most important indicators of activation of hepatic stellate cells is the expression of α-smooth muscle actin (α-SMA) (5–7, 13, 16), the actin isoform typical of smooth muscle cell differentiation (17). Also, hepatic stellate cells have been shown to respond to a number of vasoconstrictors with an increase in the intracellular free Ca2+ [Ca2+]i and with contraction (16, 18). Therefore, it is very important to study the activities of Ca2+-transporting channels and transporters. Recently, a voltage-gated Ca2+ channel activity has been examined in stellate cells by using the Fura-2 fluorimetric technique (19) and by using the patch-clamp technique (20), although those results were controversial. However, there has been no report about Ca2+ exit pathways such as Ca2+ pump and Na+/Ca2+ exchanger (NCX) in hepatic stellate cells. Therefore, in the present study NCX expression in stellate cells was examined by using the Fura-2 fluorimetric and molecular biological techniques. We found that NCX expression emerges in rat stellate cells after activation either in vitro by primary culture or in vivo during liver fibrosis or cirrhosis induced by administration of carbon tetrachloride (CCl4).
METHODS
Animals.
Male Wistar rats (SLC, Shizuoka, Japan) weighing 450–500 g, fed ad libitum on a standard chow diet and distilled water (plus phenobarbital 40 mg/dl for CCl4-treated rats), were used in all experiments. All animals received humane care in compliance with the institution’s guidelines. Liver cirrhosis was induced by the oral administration of CCl4 once a week for 6 or 12 weeks according to a method described previously (21).
Cell Isolation and Culture.
Under ether anesthesia, a midline incision was made in the abdomen of the rat. The portal vein was cannulated with a cut down tube, and the liver was perfused in situ with Ca2+-free Hanks’ solution containing 0.5 mM EGTA at 10 ml/min for 3 min and was subsequently perfused at ≈5 ml/min with 200 ml of Hanks’ solution at 37°C containing 5 mM Ca2+ and 0.05% collagenase (Wako Pure Chemical, Osaka). The anesthetized rat was killed by exsanguination during perfusion. Immediately after excision the liver was minced, suspended in the same collagenase solution, and filtered through a mesh, and then the cell suspension was centrifuged at 450 × g for 10 min at 4°C. The cell pellets were resuspended in Hanks’ solution and centrifuged twice at 50 × g for 2 min at 4°C. In some experiments, the parenchymal cell (hepatocyte)-enriched pellet was used for Northern blot analysis immediately after isolation or the Fura-2 study after 1-day culture. The supernatant, rich in nonparenchymal cells (stellate cells, endothelial cells, and Kupffer cells), was subsequently resuspended after centrifugation at 450 × g for 10 min (at 4°C). For some experiments Kupffer cells and sinusoidal endothelial cells were separately enriched from the non-parenchymal-cell-rich fraction with the centrifugal elutriator rotor by the method reported previously (22). These cells were used immediately for the Northern blot analysis or for Fura-2 study after 1-day culture. Stellate cells were enriched from the non-parenchymal-cell-rich fraction, according to the method reported previously (23), by density gradient centrifugation at 1500 × g for 10 min by using a 13% Nycodenz cushion at 4°C. In some experiments, the stellate cell-deficient, non-parenchymal-cell-rich fraction, mainly consisting of Kupffer cells and sinusoidal endothelial cells, was provided for the Northern blot analysis. The stellate cell-enriched fraction was further purified by density gradient centrifugation at 1,500 × g with 11% Nycodenz cushion. After centrifugation at 450 × g for 10 min at 4°C, the cell pellets were resuspended in minimal essential medium (Nissui Seiyaku, Tokyo) supplemented with 10% fetal bovine serum. Stellate cells were identified by the multiple lipid droplets in the cytosol under light microscopy and by the autofluorescence of vitamin A under fluorescence microscopy, and the purity was >90%. Immediately after isolation, the viability of all cell types, assessed by trypan blue exclusion test, was ≈80%. Enriched stellate cell preparation could be successfully isolated from the rat liver with cirrhosis induced by CCl4 administration for 6 weeks but not from that for 12 weeks, presumably caused by a decreased content of fat droplet in stellate cells.
The cells were cultured on type I collagen-coated (8) plastic dishes or coverslips at a density of ≈1 × 105 cells/cm2 at 37°C with 5% CO2 in air. The culture medium was changed 24 h later and then every other day.
Northern Blot Analysis.
The probe for rat heart NCX was prepared as reported (24). In brief, 5 μg of rat heart total RNA was reverse-transcribed with random primers. The synthesized cDNA mixture was subjected to 30 cycles of PCR, each consisting of denaturation for 1 min at 94°C, annealing of primers for 1 min at 55°C, and elongation for 1 min at 72°C, with a DNA thermal cycler (Astec, Fukuoka, Japan), Taq DNA polymerase (Toyobo, Osaka), and specific NCX primers. The 20-mer oligonucleotide primers, based on the rat heart NCX cDNA sequence (24), were as follows: sense primer, 5′-AGAGGCAGAAACAGGAGGAA-3′ (nt 165–184); and antisense primer, 5′-AGCGAACACAACACAGATGG-3′ (nt 782–801). The 637-bp PCR product was essentially identical among the various NCX isoforms (25). This PCR product was cloned into the EcoRV site of pBluescript SK(−) plasmid, and the insert was confirmed by sequencing. The insert was purified and used as a probe for Northern blot analysis.
The total RNA of stellate cells was prepared by using TRIzol Reagent (BRL). In some experiments, the total RNA of whole liver or isolated liver cell types was used without proceeding to cell culture. Total RNA prepared from normal rat heart was used as a control. Twenty micrograms of total RNA was applied into 1% agarose-formaldehyde gel and electrophoresed, transferred to nitrocellulose membrane, and hybridized to a probe, which was labeled with [α-32P]deoxycitidine 5′-triphosphate at 65°C for 2 h after prehybridization for 1 h at 65°C. In some experiments, the membrane was simultaneously hybridized with an oligonucleotide complementary to glycerol-3-phosphate dehydrogenase (G3PDH) (Cloneteck, Talo Alto, CA).
Western Blot Analysis.
The membrane fraction of 1 or 7 day-cultured stellate cells was enriched by density gradient centrifugation as reported (26). The membrane fraction prepared from normal dog heart (supplied by M. Matsumoto, Kyoto University) was used as a control. Samples containing 50 μg of protein, solubilized and denatured at 95°C for 4 min in SDS sample buffer, were separated by SDS/PAGE. Proteins were then transferred to a membrane (GVHP00010; Nihon Millipore, Tokyo). The blot was blocked with 0.5% BSA and 5% skimmed milk in Tris-buffered saline containing 0.1% Tween-20 (TBS-T) for 24 h at 4°C. Detection was performed by using the ECL Western blotting system (Amersham) and a mouse mAb raised against the dog cardiac sarcolemmal NCX (#6H3, a gift from M. Shigekawa, National Cardiovascular Center Research Institute, Osaka).
Fura-2 Measurements.
The [Ca2+]i concentration was monitored at room temperature (22–25°C) by the Fura-2 fluorescence ratio image method as described (27, 28). Stellate cells cultured for 1 to 9 days or other cell types cultured for 1 day on collagen-coated coverslips were loaded with Fura-2 by incubating them for 60 min at 37°C in medium containing 20 μM Fura-2/AM (Dojindo, Kumamoto, Japan). The coverslips were transferred to a chamber on a microscope stage where they were perfused for 10 min before experiment at room temperature with control Hepes-buffered saline solution (HBS). HBS contained 137.5 mM NaCl, 4.2 mM KCl, 0.9 mM CaCl2, 2 mM MgCl2, 8 mM Hepes, 6 mM Na-Hepes, and 20 mM mannitol (pH 7.4). Changes in Na+ concentrations were made by replacing NaCl with equimolar N-methyl-d-glucamine (NMDG) following pH adjustment with HCl. In some experiments, the K+ concentration was increased to 40 mM by replacing NaCl with KCl. A nominally Ca2+-free solution was prepared by removing CaCl2 from the above HBS. In some experiments NiCl2 (5 mM), verapamil (100 μM), nifedipine (100 μM), or thapsigargin (50 nM) was added to the HBS.
The fluorescence images at excitation wavelengths of 340 and 380 nm were collected every 15 s and digitized by an image processor (Argus 50; Hamamatsu Photonics, Hamamatsu City, Japan). The [Ca2+]i was evaluated from the ratio images by in vitro calibration with 2.5 μM Fura-2 free acid (Dojindo), as described in a previous paper (27).
Differences between mean [Ca2+]i values were statistically evaluated by Student’s t test.
Immunostaining of α-SMA.
Hepatic stellate cells cultured for the indicated period on coverslips were washed twice in Ca2+-free PBS solution and then fixed by immersion in acetone at −20°C for 20 min. After immersing in PBS containing 1% BSA for 15 min, the cells were then incubated with fluorescein isothiocyanate-conjugated mouse monoclonal anti-α-SMA antibody (F-3777; Sigma) or control nonimmunized mouse antibody (F-6522; Sigma) at room temperature for 1 h. After washing three times in PBS, the specimens were visualized under a fluorescence microscope (BX-FLA or BX-60; Olympus).
RESULTS
Morphological Changes of Hepatic Stellate Cells During Primary Culture.
Immediately after isolation stellate cells were round in shape and contained multiple fat droplets. After culturing for 1–3 days the cells exhibited a “star-like” appearance with extending processes. After 3–5 days, the cells became spread and the number of fat droplets diminished. Over 5 days a number of cells apparently began to proliferate. By day 7 most cells had lost their fat droplets and become more prominently spread. These observations are in good agreement with previous reports (6, 8, 9).
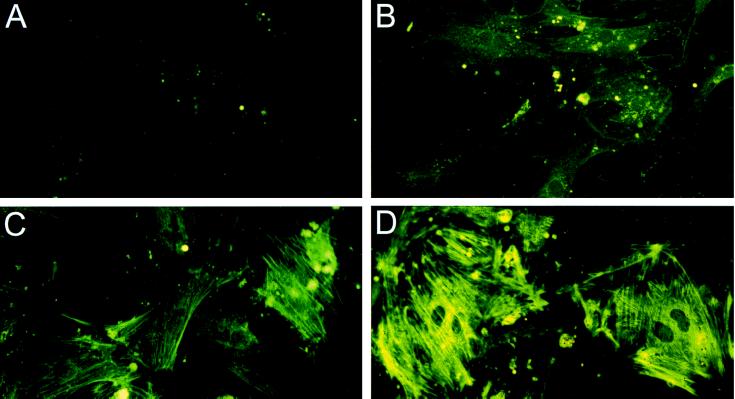
Immunostaining with a mAb against α-SMA, which is a good indicator of the transformation of stellate cells to myofibroblast-like cells (5–7, 13, 16), demonstrated the activation of stellate cells during primary culture, as reported previously (7, 13, 16). α-SMA could not be detected on day 1 (Fig. 1A), but became readily detectable over 3 days (Fig. 1 B–D). Stellate cells cultured for 7 days displayed stress-fiber-like structures (Fig. 1D).
Figure 1.
Immunofluorescence staining of the α-SMA with the fluorescein isothiocyanate-labeled anti-α-SMA antibody in rat hepatic stellate cells cultured for 1 day (A), 3 days (B), 5 days (C) and 7 days (D).
Molecular Expression of NCX in Stellate Cells After Activation in Primary Culture.
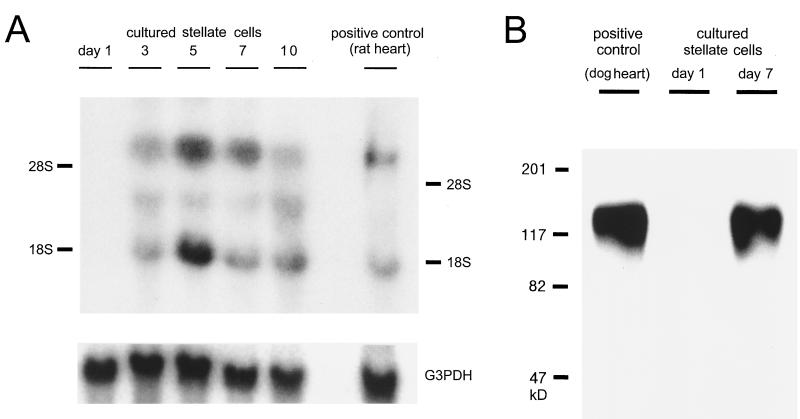
Expression of NCX mRNA was examined by Northern blot analysis by using the probe based on the rat cardiac NCX. As shown in Fig. 2A, NCX mRNA was not detectable after culturing for 24 h but became detectable after culturing for more than 3 days. The relative level of the exchanger mRNA evaluated by densitometric normalization against G3PDH mRNA gradually increased with increasing the duration of culture (see the legend for Fig. 2A). The reason for the appearance of three major bands is not clear. However, similar bands of ≈7, 3, and 1.8 kb were obtained with the rat heart positive control (Figs. 2A and 4B). Moreover, bands similar to the 7-kb and 1.8-kb bands of this report have also been obtained with Northern blot analysis of NCX mRNA expression in human heart and rabbit kidney (29, 30). A band similar to the 3-kb band of this report has been found by Northern blot analysis with RNA from rat kidney (25). Taken together, these facts suggest that the three bands observed in this study correspond to NCX mRNA.
Figure 2.
Northern blots (A) and Western immunoblots (B) of NCX in cultured rat hepatic stellate cells. (A) NCX mRNA expression in stellate cells cultured for 1–7 days and in rat heart (positive control). (Lower) The same blot reprobed with G3PDH probe as a control. The relative level of NCX mRNA expression at the 1.8-kb band against G3PDH mRNA expression was determined by densitometric normalization to be 0.44, 1.18, 1.42, 2.38, and 2.93 on days 1, 3, 5, 7, and 10 of cultured rat stellate cells, respectively, when the relative level for rat heart was set at 1.00. (B) NCX protein expression in the membrane fraction of cultured rat stellate cells and in that of dog heart (positive control). Lanes: 1, control dog heart; 2, stellate cell cultured for 1 day; 3, stellate cell cultured for 7 days. Molecular weight markers in kDa are indicated on the left.
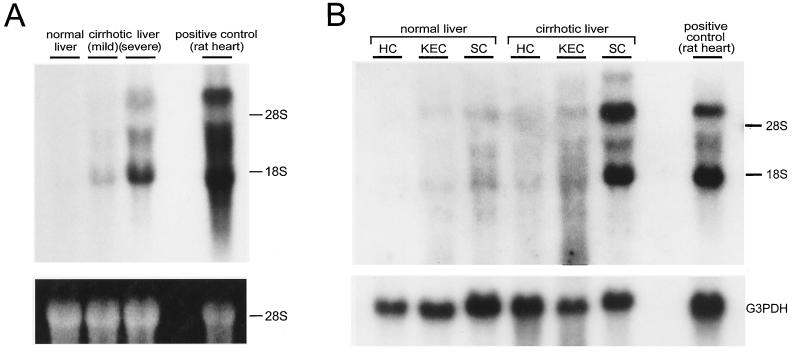
Figure 4.
Northern blot analysis of the exchanger mRNA in whole livers (A) and in different cell types isolated from rat livers (B). (A) RNA isolated from whole livers of normal rat (lane 1) and cirrhotic rat after treatment with CCl4 for 12 weeks (lanes 2 and 3). Macroscopic inspections indicate that the CCl4-treated livers were nodular, shrunken, and hard, and that fibrosis was judged to be mild for a sample liver of lane 2 and severe for that of lane 3. Amount of loaded RNA was monitored by ethidium bromide-staining (Lower). (B) RNA prepared from cells isolated from normal or fibrotic rat livers. Twenty micrograms of total RNA were run per lane. Lanes 1–3 represent the fraction rich in hepatocytes (HC), stellate-cell-deficient fraction rich in other nonparenchymal cells (Kupffer cells and sinusoidal endothelial cells) (KEC), and the stellate-cell-rich-fraction (SC) obtained from normal liver, respectively. Lanes 4–6 correspond to the same fractions from fibrotic livers (treatment with CCl4 for 6 weeks). (Lower) The same blot reprobed with G3PDH.
Western blot analysis showed that a mouse mAb raised against the canine cardiac sarcolemmal NCX protein cross-reacts with NCX of rat hepatic stellate cells (Fig. 2B). A band of apparent molecular weight of 120 kDa, which is identical with that of the canine (ref. 31; also see Fig. 2B, positive control) or bovine cardiac isoform (32), was clearly detected in the membrane fraction of stellate cells cultured for 7 days, but not of those cultured for 1 day.
Functional Expression of NCX in Stellate Cells Activated After Primary Culture.
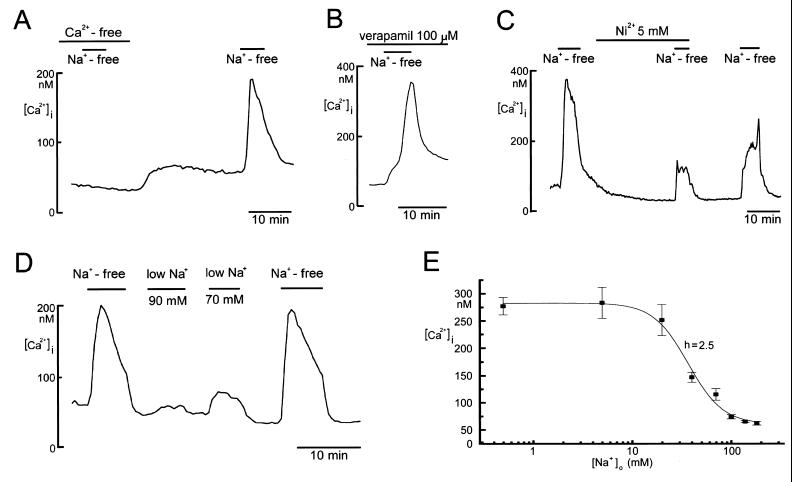
The Fura-2 fluorimetric technique was used to examine the functional activity of NCX in single stellate cells cultured for 7 days. As shown in Fig. 3A, [Ca2+]i was transiently increased from 64.7 ± 1.9 nM (SEM) (n = 147) to 277.3 ± 15.8 nM (n = 49) upon deprivation of extracellular Na+ from the bathing solution containing 0.9 mM Ca2+, whereas no [Ca2+]i increase was observed in the nominally Ca2+-free extracellular solution. Similar Ca2+ increases were observed in response to removal of extracellular Na+ even in the presence of 50 nM thapsigargin, an inhibitor of endoplasmic reticulum or sarcoplasmic reticulum Ca2+-ATPase (n = 20; data not shown). Thus, it appears that the Na+ removal-induced [Ca2+]i rise was mainly caused by Ca2+ influx from the extracellular space. An involvement of voltage-dependent Ca2+ channels in the Na+ removal-induced Ca2+ response is unlikely because the extracellular K+ concentration was maintained constant at 4.2 mM upon Na+ removal to prevent depolarization. Also, high K+-induced depolarization failed to induce a significant increase in cytosolic-free Ca2+ in the presence of 101.7 mM Na+ (40 mM K+: n = 5; data not shown), the fact excluding the existence of functional voltage-gated Ca2+ channels in stellate cells cultured for 7 days under the present experimental conditions. Moreover, the Ca2+ response to Na+ removal was not affected by extracellular application of a blocker of voltage-dependent Ca2+ channels, such as verapamil (100 μM, Fig. 3B) and nifedipine (100 μM, n = 21; data not shown).
Figure 3.
[Ca2+]i changes upon deprivation (A–D) or reduction (D and E) of extracellular Na+ in single rat hepatic stellate cells cultured for 7 days. In A–C, Fura-2 measurements were performed in the nominal absence of Ca2+, in the presence of 100 μM verapamil and in the presence of 5 mM Ni2+, respectively. The data shown in B and C is representative of 5 and 15 separate experiments, respectively. In E, the mean peak [Ca2+]i values were plotted against the extracellular Na+ concentration ([Na+]o). A smooth line represents a best fit to the Hill equation with the Hill coefficient (h) of 2.48 ± 0.55. Vertical bars indicate SEM (n = 16–147).
The Na+ removal-induced Ca2+ response was markedly suppressed (Fig. 3C) by extracellular application of 5 mM Ni2+, which is a potent blocker of NCX (33) in all cells examined. In 7 of 15 experiments the reduction was so substantial that the Ca2+ response could no longer be observed (data not shown). The mean peak [Ca2+]i value upon Na+ deprivation was 215.7 ± 33.6 and 48.9 ± 8.0 nM (n = 15, P = 0.0002) in the absence and presence of 5 mM Ni2+, respectively.
A [Ca2+]i rise was also induced by decreasing the extracellular Na+ concentration ([Na+]o), as shown in Fig. 3D. The magnitude of peak Ca2+ response exhibited a sigmoidal dependence on the [Na+]o level with a Hill coefficient (h) of 2.5 (Fig. 3E). These results indicate that stellate cells cultured for 7 days exhibit functional expression of NCX.
Similar Ca2+ responses to Na+ deprivation could be observed in stellate cells cultured for 8 days (n = 46) or 9 days (n = 23). A discernible Ca2+ response to Na+ removal was, however, never observed in stellate cells cultured for 1–4 days (n = 25–36) and could be observed in only 1 of 27 stellate cells cultured for 5 days (data not shown).
In hepatocytes, sinusoidal endothelial cells, and Kupffer cells, no Ca2+ response to Na+ removal was observed (n = 20–29; data not shown).
Expression of NCX mRNA in Stellate Cells in Cirrhotic Livers.
As shown in Fig. 4A, total RNA extracted from a whole liver of rat administered with CCl4 for 12 weeks was found to be distinctly cross-hybridized to probes of rat cardiac NCX, whereas virtually no hybridization was observed in total RNA from a whole liver of a normal rat. The level of expression of NCX mRNA was correlated with the macroscopic severity of cirrhosis (see in the legend for Fig. 4A).
In the rat liver with early-phase cirrhosis induced by 6-week treatment with CCl4, as shown in Fig. 4B, expression of NCX mRNA was found to be prominently increased in stellate cells (SC). The expression level in stellate cells in cirrhotic liver was much higher than that in stellate cells isolated from normal liver as well as that in hepatocytes (HC) or in the nonparenchymal cell fraction rich in Kupffer cells and sinusoidal endothelial cells (KEC) in normal or cirrhotic liver.
DISCUSSION
NCX is a transporter protein that couples the translocation of Ca2+ to that of Na+ in the opposite direction and contributes to the maintenance of intracellular Ca2+ homeostasis in a wide variety of cell types (34, 35). Because the canine cardiac NCX was first cloned and sequenced (31), a number of the isoforms have been identified in human heart (36), bovine heart (32), rat heart (24), rabbit kidney (30, 37), rat kidney (25), rat aortic smooth muscle (20), and rat brain (38). By using oligonucleotide primers derived from NCX of human heart and rat kidney, NCX expression was demonstrated in human and rat livers (25, 29), although the level was weakest among the tissues tested. However, there has been no report as to which cell type exhibits NCX expression. In the present study, we report that not only the molecular expression of NCX but also functional expression of the exchanger are found predominantly in activated stellate cells. Both the expression levels of NCX protein and of its mRNA in activated rat stellate cells were found to be as high as those in dog or rat heart (Figs. 2 and 4B, positive control).
Previous studies (2, 5, 7) have reported that the best indicator for activation of stellate cells is α-SMA, which is also an indicator of smooth muscle differentiation (17). The present study showed that NCX mRNA in stellate cells became detectable on spontaneous activation during primary culture as early as α-SMA (on day 3) and that functional expression of NCX in stellate cells could be monitored by [Ca2+]i measurements with Fura-2 by 7 days in culture. Thus, the molecular and functional expression of NCX may serve as a marker of hepatic stellate cell activation.
Because stellate cell activation is a final common pathway of liver fibrogenesis, it is possible that the NCX activity in activated stellate cells is involved in the pathogenesis of liver fibrosis or cirrhosis. Here, we showed evidence for the in vivo expression of NCX mRNA in stellate cells isolated from the rat liver in a CCl4 model of hepatic fibrosis. Also, the present study demonstrated that enhanced expression of NCX mRNA in cirrhotic rat liver can be detected at the whole liver level. This fact suggests that detection of NCX mRNA may provide a diagnostic marker of liver fibrosis or cirrhosis.
After activation stellate cells are known to exhibit prominent contractile activity (6, 39). An increase in the [Ca2+]i level must contribute to the Ca2+-dependent contractile function of activated stellate cells. In fact, increased [Ca2+]i is known to be associated with contraction under stimulation with a number of vasoactive substances, such as thrombin, angiotensin II, endotheline 1, and prostaglandin F2α (16, 18). Therefore, NCX may play a physiological role in regulation of intracellular Ca2+ in activated stellate cells by extruding the excess divalent cations out of cells, presumably together with an ATP-dependent Ca2+ pump. Because activated stellate cells are known to take part in liver fibrogenesis by secreting injurious extracellular matrix components (1, 2), NCX may also play a pathophysiological role in regulation of Ca2+-dependent secretory functions.
Acknowledgments
We are grateful to A. F. James (King’s College, London) for critical reading the manuscript, to M. Shigekawa and S. Wakabayashi (National Cardiovascular Center Research Institute, Osaka) for reading the manuscript and providing a mAb for dog cardiac NCX, to T. Niki (Free University, Brussels) for helpful advice on the Ito cell isolation method, and to A. Miwa and M. Ohara (National Institute for Physiological Sciences, Okazaki) for technical assistance. This work was supported by a Grant-in-Aid for Scientific Research on Priority Areas of “Channle-Transporter Correlation” (07276104) from the Ministry of Education, Science, and Culture of Japan.
ABBREVIATIONS
- NCX
Na+/Ca2+ exchanger
- α-SMA
α-smooth muscle actin
- G3PDH
glycerol-3-phosphate dehydrogenase
- [Ca2+]i
intracellular free Ca2+ concentration
- [Na+]o
extracellular Na+ concentration
References
- 1.Blomhoff R, Wake K. FASEB J. 1991;5:271–277. doi: 10.1096/fasebj.5.3.2001786. [DOI] [PubMed] [Google Scholar]
- 2.Friedman S L. N Engl J Med. 1993;328:1828–1835. doi: 10.1056/NEJM199306243282508. [DOI] [PubMed] [Google Scholar]
- 3.Friedman S L, Roll F J, Boyles J, Arenson D M, Bissell D M. J Biol Chem. 1989;264:10756–10762. [PubMed] [Google Scholar]
- 4.Geerts A, Vrijsen R, Rauterberg J, Burt A, Schellinck P, Wisse E. J Hepatol. 1989;9:59–68. doi: 10.1016/0168-8278(89)90076-7. [DOI] [PubMed] [Google Scholar]
- 5.Ramadori G, Veit T, Schwögler S, Dienes H P, Knittel T, Rieder H, Meyer zum Büschenfelde K-H. Virchows Arch. 1990;59:349–357. doi: 10.1007/BF02899424. [DOI] [PubMed] [Google Scholar]
- 6.Kawada N, Klein H, Decker K. Biochem J. 1992;285:367–371. doi: 10.1042/bj2850367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rockey D C, Boyles J K, Gabbiani G, Friedman S L. J Submicrosc Cytol Pathol. 1992;24:193–203. [PubMed] [Google Scholar]
- 8.Senoo H, Hata R. Biochem Biophys Res Commun. 1994;200:999–1006. doi: 10.1006/bbrc.1994.1549. [DOI] [PubMed] [Google Scholar]
- 9.Friedman S L, Rockey D C, McGuire R F, Maher J J, Boyles J K, Yamasaki G. Hepatology. 1992;15:234–243. doi: 10.1002/hep.1840150211. [DOI] [PubMed] [Google Scholar]
- 10.McGee J O’D, Patrick R S. Lab Invest. 1972;26:429–440. [PubMed] [Google Scholar]
- 11.Minato Y, Hasumura Y, Takeuchi J. Hepatology. 1983;3:559–566. doi: 10.1002/hep.1840030414. [DOI] [PubMed] [Google Scholar]
- 12.Ogawa K, Suzuki J, Mukai H, Mori M. Am J Pathol. 1986;125:611–619. [PMC free article] [PubMed] [Google Scholar]
- 13.Rockey D C, Housset C N, Friedman S L. J Clin Invest. 1993;92:1795–1804. doi: 10.1172/JCI116769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramm G A, Britton R S, O’Neill R, Blaner W S, Bacon B R. Am J Physiol. 1995;269:G532–G541. doi: 10.1152/ajpgi.1995.269.4.G532. [DOI] [PubMed] [Google Scholar]
- 15.Shiratori Y, Geerts A, Ichida T, Kawase T, Wisse E. J Hepatol. 1986;3:294–303. doi: 10.1016/s0168-8278(86)80481-0. [DOI] [PubMed] [Google Scholar]
- 16.Kawada N, Tran-Thi T-A, Klein H, Decker K. Eur J Biochem. 1993;213:815–823. doi: 10.1111/j.1432-1033.1993.tb17824.x. [DOI] [PubMed] [Google Scholar]
- 17.Skalli O, Ropraz P, Trzeciak A, Benzonana G, Gillessen D, Gabbiani G. J Cell Biol. 1986;103:2787–2796. doi: 10.1083/jcb.103.6.2787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pinzani M, Failli P, Ruocco C, Casini A, Milani S, Baldi E, Giotti A, Gentilini P. J Clin Invest. 1992;90:642–646. doi: 10.1172/JCI115905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oide H, Thurman R G. Hepatology. 1994;20:1009–1014. doi: 10.1002/hep.1840200433. [DOI] [PubMed] [Google Scholar]
- 20.Kashiwagi S, Suematsu M, Wakabayashi Y, Kawada N, Tachibana M, Koizumi A, Inoue M, Ishimura Y, Kaneko A. Am J Physiol. 1997;272:G742–G750. doi: 10.1152/ajpgi.1997.272.4.G742. [DOI] [PubMed] [Google Scholar]
- 21.Proctor E, Chatamra K. Gastroenterology. 1982;83:1183–1190. [PubMed] [Google Scholar]
- 22.Sakisaka S, Noguchi K, Kawahara T, Gondo K, Akashi T, Ishii Y, Ueno T, Yishitake M, Abe H, Tanikawa K. Acta Hepatol Jpn. 1986;27:487–496. [Google Scholar]
- 23.De Bleser P J, Jannes P, van Buul-Offers S C, Hoogerbrugge C M, van Schravendijk C F H, Niki T, Rogiers V, Van den Brande J L, Wisse E, Geerts A. Hepatology. 1995;21:1429–1437. doi: 10.1002/hep.1840210529. [DOI] [PubMed] [Google Scholar]
- 24.Low W, Kasir J, Rahamimoff H. FEBS Lett. 1993;316:63–67. doi: 10.1016/0014-5793(93)81737-k. [DOI] [PubMed] [Google Scholar]
- 25.Lee S-L, Yu A S L, Lytton J. J Biol Chem. 1994;269:14849–14852. [PubMed] [Google Scholar]
- 26.Maeda T, Balakrishnan K, Mehdi S Q. Biochim Biophys Acta. 1983;731:115–120. doi: 10.1016/0005-2736(83)90404-2. [DOI] [PubMed] [Google Scholar]
- 27.Ueda S, Okada Y. Biochim Biophys Acta. 1989;1012:254–260. doi: 10.1016/0167-4889(89)90105-5. [DOI] [PubMed] [Google Scholar]
- 28.Hazama A, Okada Y. Pflügers Arch. 1990;416:710–714. doi: 10.1007/BF00370619. [DOI] [PubMed] [Google Scholar]
- 29.Kofuji P, Hadley R W, Kieval R S, Lederer W J, Schulze D H. Am J Physiol. 1992;263:C1241–C1249. doi: 10.1152/ajpcell.1992.263.6.C1241. [DOI] [PubMed] [Google Scholar]
- 30.Reilly R F, Shugrue C A. Am J Physiol. 1992;262:F1105–F1109. doi: 10.1152/ajprenal.1992.262.6.F1105. [DOI] [PubMed] [Google Scholar]
- 31.Nicoll D A, Longoni S, Philipson K D. Science. 1990;250:562–565. doi: 10.1126/science.1700476. [DOI] [PubMed] [Google Scholar]
- 32.Aceto J F, Condrescu M, Kroupis C, Nelson H, Nelson N, Nicoll D, Philipson K D, Reeves J P. Arch Biochem Biophys. 1992;298:553–560. doi: 10.1016/0003-9861(92)90449-7. [DOI] [PubMed] [Google Scholar]
- 33.Kimura J, Miyamae S, Noma A. J Physiol (London) 1987;384:199–222. doi: 10.1113/jphysiol.1987.sp016450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.van Breemen C, Saida K. Annu Rev Physiol. 1989;51:315–329. doi: 10.1146/annurev.ph.51.030189.001531. [DOI] [PubMed] [Google Scholar]
- 35.Reeves J P. Curr Top Membr Transp. 1985;25:77–127. [Google Scholar]
- 36.Komuro I, Wenninger K E, Philipson K D, Izumo S. Proc Natl Acad Sci USA. 1992;89:4769–4773. doi: 10.1073/pnas.89.10.4769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kofuji P, Lederer W J, Schulze D H. Am J Physiol. 1993;265:F598–F603. doi: 10.1152/ajprenal.1993.265.4.F598. [DOI] [PubMed] [Google Scholar]
- 38.Furman I, Cook O, Kasir J, Rahamimoff H. FEBS Lett. 1993;319:105–109. doi: 10.1016/0014-5793(93)80046-w. [DOI] [PubMed] [Google Scholar]
- 39.Sakamoto M, Ueno T, Kin M, Ohira H, Torimura T, Inuzuka S, Sata M, Tanikawa K. Hepatology. 1993;18:978–983. doi: 10.1002/hep.1840180432. [DOI] [PubMed] [Google Scholar]