Abstract
Background/Objectives:
Respiratory complications are a major cause of illness and death in persons with spinal cord injuries and dysfunction (SCI&Ds). The objectives of this study were to examine rates of outpatient visits over 5 years for acute respiratory tract infections (ARIs), including pneumonia and influenza (P&I), lower respiratory tract infections (LRIs), and upper respiratory tract infections (URIs), in veterans with SCI&Ds and to determine whether individual characteristics were associated with the number of annual visits for each type of ARI.
Methods:
This was a longitudinal (fiscal years 1998–2002) study of ARI visits at the Veterans Health Administration (VA) in 18,693 veterans with SCI&Ds. To examine the associations between time, patient characteristics, and annual number of ARI visits, we used random effect negative binomial models.
Results:
Veterans with SCI&Ds had a total of 11,113 ARI visits over the 5-year period. There was a slightly decreasing trend for LRI visits over time (P < 0.01) but no significant change for other ARIs over time. There were 30 to 35 pneumonia visits and 21 to 30 acute bronchitis visits per 1,000 SCI&D veterans per year. Older veterans were more likely than younger to have P&I visits and less likely to have URI visits (P < 0.01). Veterans with paraplegia had fewer P&I visits than subjects with tetraplegia (IRR = 0.58; CI = 0.51–0.67).
Conclusions:
Visit rates for ARIs are stable for veterans with SCI&Ds. Identifying risk factors associated with ARI visits is an important first step to improve prevention and treatment of ARIs and to improve the health of veterans with SCI&Ds.
Keywords: Spinal cord injuries, Veterans, Acute respiratory tract infection, Pneumonia, Influenza, Bronchitis, Paraplegia, Tetraplegia
INTRODUCTION
Respiratory complications and illnesses are a major cause of morbidity and mortality for persons with spinal cord injuries and dysfunction (SCI&Ds). Spinal cord injuries and disorders cause physiological changes that increase the risks of respiratory complications (1,2), which are a leading cause of death (3–6) and of hospitalizations after SCI&Ds (7,8). Existing research on health care utilization for respiratory conditions for persons with SCI&Ds has focused mostly on hospitalizations and pneumonia. Previous studies found that characteristics associated with an increased risk of pneumonia include older age (9), complete tetraplegia (9), longer duration of injury (10), and traumatic injury (11). Visit rates for acute respiratory tract infections (ARIs) have not previously been reported for those with SCI&Ds. In the general population, hospitalization rates for pneumonia have been increasing, particularly in older age groups, and this has been attributed to an increasing prevalence of chronic medical conditions (12,13).
The major objectives of this study were to determine whether there was a change in the rate of yearly outpatient visits for ARIs for veterans with SCI&Ds during a 5-year period and to determine whether certain patient characteristics are associated with having an increased number of respiratory visits, specifically for lower respiratory tract infections (LRIs), upper respiratory tract infections (URIs), and pneumonia and influenza (P&I). Examining outpatient visits for a large cohort of veterans with SCI&Ds over time will provide a more complete picture of the burden and risks associated with respiratory tract infections for persons with SCI&Ds.
METHODS
Design and Setting
This 5-year (fiscal years 1998–2002; October 1, 1997–September 30, 2002) retrospective dynamic cohort analysis study was conducted to examine trends and rates of outpatient encounters for respiratory tract infections for veterans with SCI&Ds receiving care at any of the approximately 850 Department of Veterans Affairs (VA) ambulatory care facilities and community-based outpatient clinics throughout the United States. The study was reviewed and approved by the Edward Hines Jr VA Hospital Institutional Review Board.
Subjects
The sample population included all veterans with SCI&Ds who had any outpatient visits during the 5-year study period. Veterans with SCI&Ds were identified using an algorithm based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes and VA inpatient and outpatient administrative data. The algorithm also identifies patients with multiple sclerosis, all of whom were excluded from this analysis. Subjects were included beginning with fiscal year 1998 or in a subsequent year if their date of injury was after 1998, while subjects who died during the 5-year period were excluded from the calculation of rates for years subsequent to death. Patients who were not veterans were also excluded. An additional 837 patients were excluded because they had missing data for race. The total number of subjects with complete data was 18,693.
Measures
To obtain demographic and clinical characteristics and frequency of respiratory visits, we acquired data from the VA Medical Inpatient and Outpatient SAS data sets. Information about level and completeness of injury was captured from the VA Spinal Cord Dysfunction Registry. Dates of death were obtained from the VA Benefit Information Retrieval and Location System database.
The utilization variables included the number of annual visits for URIs, LRIs, and P&I. These variables were defined using both primary and secondary diagnosis fields in the outpatient encounter files in the SAS files. The ICD-9-CM codes were used to identify diagnoses and classify them into categories. A visit was defined as a respiratory visit if any of the codes mentioned later in this section were included in either a primary or a secondary diagnostic field. We examined both primary and secondary diagnoses for ARIs because the use of SCI-related diagnostic codes as the primary diagnosis is widespread. If we only used primary codes, we would eliminate approximately 10% of visits that had a primary diagnosis related to SCI. Upper respiratory tract infection codes included 034: streptococcal sore throat; 460 to 465: common cold, acute sinusitis, pharyngitis, and laryngitis, acute URI not otherwise specified; and 475: peritonsillar abscess. Lower respiratory tract infection codes included 466: acute bronchitis/bronchiolitis; 031.0: pulmonary diseases due to other mycobacteria; 033: whooping cough; 073.0: ornithosis, with pneumonia; 510: empyema; 511: pleurisy; 513: lung/mediastinal abscess; 515: postinflammatory pulmonary fibrosis; and 516.0: pulmonary alveolar proteinosis. Finally, ICD9-CM codes 480 to 487 were included in the P&I category.
Patient age was determined by subtracting the year of birth from the last fiscal year. Three age categories were included in the analyses: <50 years, 50–64 years, and ≥65 years. Race and ethnicity were collapsed into 2 groups: white and a reference group including persons with other races and ethnicities. This reference group included subjects who had been identified at least once as Black, Hispanic, Asian or Pacific Islander, American Indian, or “other” ethnicity during any outpatient visit. Level of injury was defined as paraplegia or tetraplegia, and extent of injury was categorized as incomplete and complete. Etiology was categorized as nontraumatic or traumatic. Four duration of injury categories were created: <10 years, 10–20 years, 20–30 years, and >30 years, with durations of less than 10 years used as the reference group.
Analyses
Subject characteristics were described using frequencies and means. The mean number of visits for P&I, LRIs, and URIs were calculated and plotted. To examine the time trend over the 5 years and the association between individual characteristics and the number of visits per year, we used negative binomial regression models. This type of model is used for count data and is more appropriate than an ordinary least-squares model because this model assumes that the dependent variable is continuous and normally distributed (14). The dependent variables were the number of URIs, LRIs, and P&I during the fiscal year, and the independent variables were the patient characteristics and time. Goodness-of-fit tests indicated that negative binomial models were more appropriate than Poisson models, which are also often used to analyze count data. A random effect was included in the models to account for possible correlation between the numbers of visits a subject had from one fiscal year to the next because previous history of infection may be correlated with the number of future visits. Likelihood ratio tests were used to compare the models with and without effects, and the results for all 3 models indicated that including a random effect for the individual to address potential correlations between observations improved the fit for all of the models. All results are presented using the random effects models. Marginal effects were calculated based on the model results as well as IRRs and 95% CIs. The IRR is also known as a relative risk. Finally, more than half of veterans had missing data for one or more of the SCI&D neurological and etiological characteristics; variables were included to indicate that the subject was missing those data, so that those subjects would not be eliminated, and to examine the association between missing characteristics and the number of ARI visits. The models were also estimated excluding subjects with missing SCI characteristics, and the results were similar to the results from the model that included the entire sample. All analyses were conducted using STATA SE/8.2; STATA Corp, College Station, TX.
RESULTS
We identified 18,693 veterans with SCI&Ds who had a total of 80,165 observations over 5 years, with 11,113 visits receiving a respiratory diagnosis. The mean age of the veterans in the study was 56.4 years (SD = 13.7 years), and most were white (65%). The population was overwhelmingly male (98%). Approximately one third had paraplegia, one third had tetraplegia, and one third was missing level of injury data. More than half were missing completeness of injury, while 23% of veterans had an incomplete injury and 22% of veterans had a complete injury. The etiology of the injury was missing for 32% of subjects, but more than half had a traumatic cause of injury. The mean duration of injury was almost 20 years.
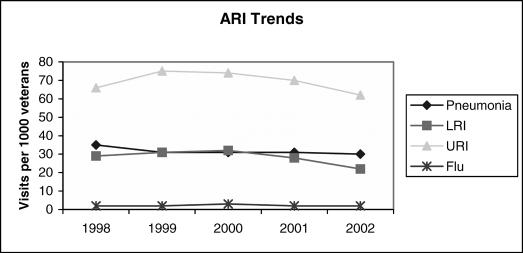
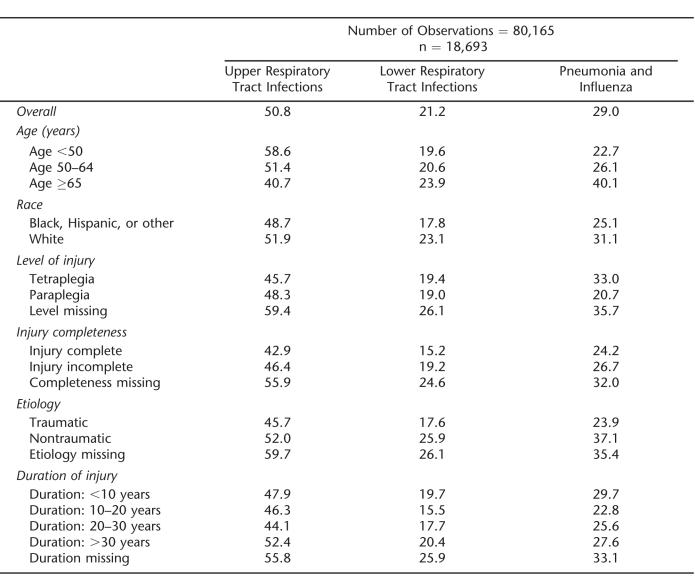
The mean number of visits per year by type of infection is presented in Figure 1. Upper respiratory tract infection visits were most prevalent; the annual number of URI visits per 1,000 veterans ranged from 62 to 75. Annual pneumonia visits ranged from 30 to 35/1,000 veterans, while the range of influenza visits was from 1.7 to 2.7/1,000 veterans. Lower respiratory tract infection visits ranged from 22 to 32/1,000 veterans; if LRI visits are restricted to acute bronchitis only (97.5% of all LRI visits), the range is slightly lower (21 to 30/1,000). When the trend of visits was examined without including any other patient characteristics in the model, there was no significant trend for either URI or P&I visits, but there was a decreasing trend in LRI visits over time (IRR=0.95, 95% CI =0.92–0.98). The numbers of visits per 1,000 veterans for each type of infection are presented in Table 1.
Figure 1. Visits per thousand veterans.
Table 1.
Event Rate by Risk Group: Rate of Visits per Thousand Veterans
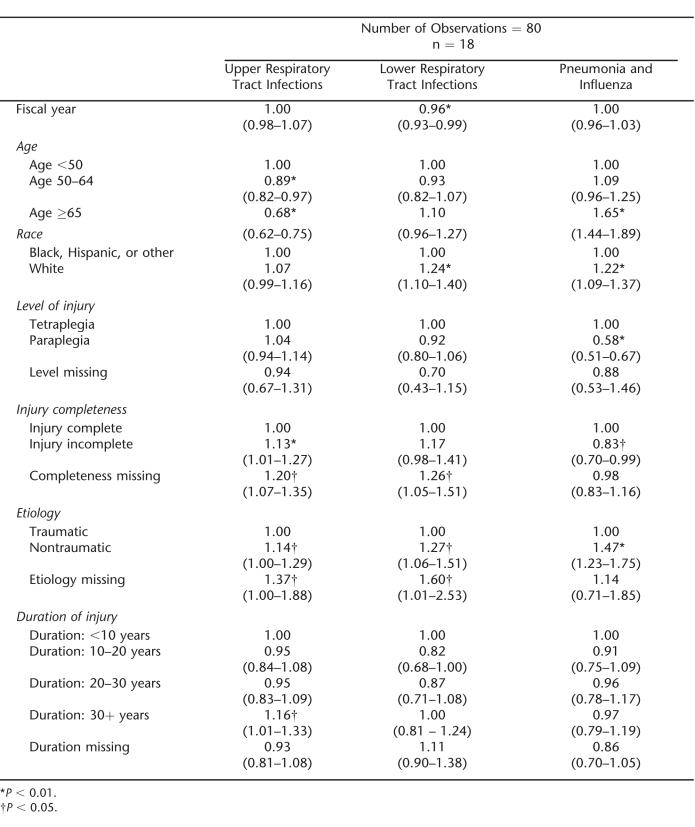
To examine the association of patient characteristics and time with the number of annual ARI visits for each patient, a multivariable negative binomial regression model was estimated for each of the 3 types of ARIs. The results of the models are presented in Table 2. Upper respiratory tract infection visit rates were stable over time. Subjects from 50 to 64 years of age were less likely to have a URI visit (IRR = 0.89, 95% CI = 0.82–0.97) than were younger veterans, as were veterans who were 65 years of age or older (IRR = 0.68, 95% CI = 0.62–0.75). Some characteristics of a veteran's SCI were also associated with the number of visits in a year. Subjects with incomplete injuries and missing completeness of injury had higher rates of annual URI visits (IRR = 1.13, 95% CI =1.01–1.27 and IRR =1.20, 95% CI =1.07–1.35, respectively) than did veterans with complete injuries. In addition, higher rates of URI visits were seen in patients with nontraumatic injuries and those missing etiology compared with those with traumatic injuries. A duration of injury 30 or more years compared with 10 years or less was associated with a higher rate of URI visits (IRR =1.16, 95% CI = 1.01–1.33).
Table 2.
Trends and Risk Factors Associated With Respiratory Tract Infection Visits: IRRs and 95% CI Levels
There was a slight decreasing trend over time for LRI visits (IRR = 0.96, 95% CI = 0.93–0.99). White race was associated with increased LRI visits compared with nonwhites. Missing completeness data were associated with more LRI visits (IRR =1.26, 95% CI =1.05–1.51) than having a complete injury. Having a nontraumatic injury or missing etiology was also associated with a higher number of LRI visits.
The fiscal year variable was not significant for P&I visits, indicating that the number of visits remained stable over the 5-year period. Veterans 65 years of age and older were more likely to have P&I visits than were veterans younger than 50 years of age (IRR = 1.65, 95% CI = 1.44–1.89). White veterans were more likely than veterans of other races and ethnicities to have visits for P&I. Veterans with paraplegia and an incomplete injury had a lower rate of P&I visits than veterans with tetraplegia or a complete injury (IRR = 0.58; 95% CI = 0.51–0.67, IRR =0.83; 95% CI =0.70–0.99, respectively). Having a nontraumatic injury was associated with higher numbers of P&I visits than having a traumatic injury (IRR =1.47, 95% CI = 1.23–1.75).
DISCUSSION
In contrast to prior work, this study used administrative data to determine rates of outpatient visits for ARIs in a large population with chronic SCI&Ds, averaging 20 years post injury. The average number of P&I and acute URI visits per year did not change significantly over 5 years, whereas there was a slight decrease in LRI visits. Nearly all LRI visits were due to acute bronchitis. These results suggest that respiratory illness rates have been stable for veterans with SCI&Ds. Studies have found a decreasing trend in pneumonia incidence during initial rehabilitation hospitalizations in SCI (11) but to our knowledge have not examined trends in outpatient visits for ARIs by veterans with SCI&Ds. The rate for P&I visits in this population was similar to the 3.5% rate reported for pneumonia and atelectasis in the period between initial rehabilitation discharge and 1-year follow up at Model SCI System centers (9). A Canadian study that used administrative data reported that 3.5% of 213 individuals with SCIs were hospitalized for pneumonia between initial hospital discharge and 6-year follow up (8).
The rates for pneumonia visits in this study are approximately twice as high as the rates for pneumonia visits overall for veterans (15). Similarly, the annual rate of 30 to 35 annual visits/1,000 persons with SCI&Ds for P&I (of which 91.5% was pneumonia) was substantially higher than the approximate rate of 16 ambulatory care visits for pneumonia per 1,000 persons for the overall US population (16). The rate of acute bronchitis visits is also higher than in the general population. The LRI rate (97.5% of which was acute bronchitis) was 22 to 32 visits/1,000 SCI&D veterans compared with an estimated rate of 18 visits/1,000 for acute bronchitis in the general population (16). On the other hand, the visit rate for URIs was much lower in our population, with 62 to 75 visits/1,000 SCI&D veterans vs 155 visits/1,000 for the general population (16). The rates for SCI&Ds are likely underestimates because patients with SCI&Ds may seek care from non-VA providers more frequently for less severe infections, such as URI. We were unable to assess non-VA care in this population. Additionally, some veterans with SCI&Ds may be less inclined to seek medical evaluation for mild URI symptoms due to their mobility limitations and increased difficulty traveling to nonessential appointments.
The result that older veterans are more likely to have visits for P&I is consistent with previous studies of both persons with SCI&Ds (9) and the general population. This is also evident in a similar study assessing antibiotic use in veterans with SCI&Ds with ARIs, in which pneumonia visits were more frequent in the older populations compared with younger groups (17).
The association between higher levels of injuries and increased risks of pneumonia has been well documented in the literature (7). Limited research exists on the relationship between level of injury and other types of respiratory tract infections. It is not surprising that level of injury did not affect the number of URIs because viral infections of the upper respiratory tract account for the majority of these and the risk of exposure and infection should be unaffected by injury level. Similarly, most cases of acute bronchitis are thought to be secondary to viral infections (7), and there is no evidence for increased susceptibility to viral infections with higher injury level. However, the visit rate for P&I was 42% lower for veterans with paraplegia compared with veterans with tetraplegia. Patients with tetraplegia have impaired cough, difficulty mobilizing respiratory secretions, and microatelectasis, which all can contribute to their increased susceptibility to P&I (2). The data on neurological classification (tetraplegia vs paraplegia; complete vs incomplete injury) were missing for many patients. Using these categories causes grouping of some patients with dissimilar neurological status. For example, patients with complete paralysis but preserved sensation below injury level (American Spinal Injury Association Impairment Scale [AIS] B classification) are grouped with patients having only slight weakness (AIS D) (18). With more precise measurements of injury level and completeness, greater differences in pneumonia and possibly LRI visit rates may have been seen across neurological classifications.
The finding that duration of injury was associated with an increased risk of pneumonia is consistent with 20-year longitudinal data from the National SCI Statistical Center (11) but not a Canadian study with 6-year follow-up (8). The results of the current study were not consistent with past studies that found that the persons with traumatic injuries were more likely to have pneumonia (7). This may be a result of the large amount of missing data for SCI&D characteristics. For example, veterans missing completeness or etiology data were more likely to be older than veterans with these data, and age is associated with risk of ARIs.
There are a number of limitations to this study. First, the administrative data might not reflect the true incidence of ARIs. Infections may not be properly coded, and/or patients may not contact a provider when they have an infection. As noted earlier, patients may have sought care from non-VA providers. Also, a single respiratory tract infection may have required multiple visits, so the visit rates may overestimate infection rates. Second, the number of years examined in the study was relatively short because of the limited availability of complete administrative data. The analysis would be more sensitive to detection of trends with a longer period, as with the general population studies of pneumonia that used 12 to 14 years of administrative data (12,13). Another limitation of these findings is that we did not control for other factors that may affect rates of respiratory tract infections, including smoking, comor-bid illnesses, and prevention activities, such as receipt of influenza and pneumococcal pneumonia vaccinations. However, this is a large population-based study of veterans with SCI&Ds, which may be generalized to other persons with SCI&Ds. This study also provides longitudinal data, including all ambulatory episodes of care in the VA, which are less prone to survivorship bias than other studies, which rely on patient report of complications at specific follow-up points (7,9).
CONCLUSION
Visits for ARIs do not appear to be declining for veterans with SCI&Ds, and the prevention and treatment of these infections should be a continuing priority. Characteristics that are associated with increased risk of P&I visits include an older age and higher level injuries, and these risk factors are similar for LRIs. Younger veterans, however, are more likely to have more visits for URIs. Identifying the risk factors associated with ARI visits is an important first step to improve efforts to prevent and treat ARIs, avoid complications, and improve the health and quality of life of veterans with SCI&Ds.
Footnotes
This work was supported by VA Health Services Research and Development Program (VA H5R&D), SCI QUERI, and VA Medical Research Service, Seattle Epidemiological Research and Information Center.
The views expressed in this paper are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
REFERENCES
- Lucke KT. Pulmonary management following acute SCI. J Neurosci Nurs. 1998;30(2):91–104. doi: 10.1097/01376517-199804000-00003. [DOI] [PubMed] [Google Scholar]
- Viroslav J, Rosenblatt R, Tomazevic SM. Respiratory management, survival, and quality of life for high-level traumatic tetraplegics. Respir Care Clin N Am. 1996;2(2):313–322. [PubMed] [Google Scholar]
- DeVivo MJ, Black KJ, Stover SL. Causes of death during the first 12 years after spinal cord injury. Arch Phys Med Rehabil. 1993;74(3):248–254. [PubMed] [Google Scholar]
- Minaire P, Demolin P, Bourret J, et al. Life expectancy following spinal cord injury: a ten-year survey in the Rhone-Alpes Region, France, 1969–1980. Paraplegia. 1983;21(3):11–15. doi: 10.1038/sc.1983.2. [DOI] [PubMed] [Google Scholar]
- Jackson AB, Groomes TE. Incidence of respiratory complications following spinal cord injury. Arch Phys Med Rehabil. 1994;75(3):270–275. doi: 10.1016/0003-9993(94)90027-2. [DOI] [PubMed] [Google Scholar]
- Soden RJ, Walsh J, Middleton JW, Craven ML, Rutkowski SB, Yeo JD. Causes of death after spinal cord injury. Spinal Cord. 2000;38(10):604–610. doi: 10.1038/sj.sc.3101080. [DOI] [PubMed] [Google Scholar]
- Cardenas DD, Hoffman JM, Kirshblum S, McKinley W. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil. 2004;85(11):1757–1763. doi: 10.1016/j.apmr.2004.03.016. [DOI] [PubMed] [Google Scholar]
- Dryden DM, Saunders LD, Rowe BH, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord. 2004;42(9):513–525. doi: 10.1038/sj.sc.3101629. [DOI] [PubMed] [Google Scholar]
- McKinley WO, Jackson AB, Cardenas DD, DeVivo MJ. Long-term medical complications after traumatic spinal cord injury: a regional model systems analysis. Arch Phys Med Rehabil. 1999;80(11):1402–1410. doi: 10.1016/s0003-9993(99)90251-4. [DOI] [PubMed] [Google Scholar]
- Levi R, Hultling C, Seiger A. The Stockholm Spinal Cord Injury Study: 2. Associations between clinical patient characteristics and post-acute medical problems. Paraplegia. 1995;33(12):585–594. doi: 10.1038/sc.1995.125. [DOI] [PubMed] [Google Scholar]
- McKinley W, Cifu D, Keyser-Marcus L, Wilson K. Comparison of rehabilitation outcomes in violent vs non-violent traumatic SCI. J Spinal Cord Med. 1998;21(1):32–36. doi: 10.1080/10790268.1998.11719508. [DOI] [PubMed] [Google Scholar]
- Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA. 2005;294(21):2712–2719. doi: 10.1001/jama.294.21.2712. [DOI] [PubMed] [Google Scholar]
- Simonsen L, Conn LA, Pinner RW, Teutsh T. Trends in infectious disease hospitalizations in the United States, 1980–1994. Arch Intern Med. 1998;158(17):1923–1928. doi: 10.1001/archinte.158.17.1923. [DOI] [PubMed] [Google Scholar]
- Cameron AC, Trivedi PK. Regression Analysis of Count Data. 1st ed. New York, NY: Cambridge University Press; 1998. [Google Scholar]
- Lee TA, Bartle B, Weiss KB. Final report for HSR&D project #42.066. Assessment of Community-Acquired Pneumonia in the VA: December 17, 2002. Available from the Center for Management of Complex Chronic Illness, Hines, IL.
- Schappert SM, Burt CW. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 2001–2002. Vital Health Stat. 2006;13(159):1–70. [PubMed] [Google Scholar]
- Evans CT, Smith B, Parada JP, Kurichi JE, Weaver FM. Trends in antibiotic prescribing for acute respiratory infection in veterans with spinal cord injury and disorder. J Antimicrob Chemother. 2005;55(6):1045–1049. doi: 10.1093/jac/dki137. [DOI] [PubMed] [Google Scholar]
- American Spinal Injury Association . International Standards for Neurological Classification of Spinal Cord Injury. Chicago, IL: American Spinal Injury Association; 2000. [Google Scholar]