Abstract
Background:
Spinal cord injury (SCI) is a devastating trauma suffered by many of the victims of an earthquake that struck Northern Pakistan on October 8, 2005. It rendered approximately 600 patients paraplegic, which is the highest number ever reported in any disaster. This study was conducted to evaluate the risk of complications.
Methods:
The cross-sectional retrospective study covering a 2-month period was conducted on 194 patients admitted to the surgical/neurosurgical wards of Rawalpindi Medical College and allied hospitals (Holy Family Hospital, Rawalpindi General Hospital, and District Headquarter Hospital) and Melody Relief and Rehabilitation Center, Islamabad.
Results:
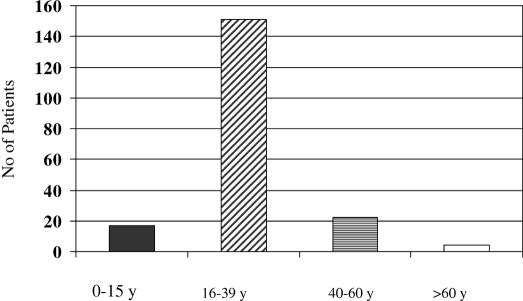
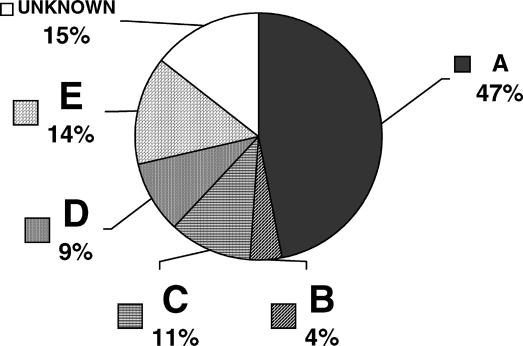
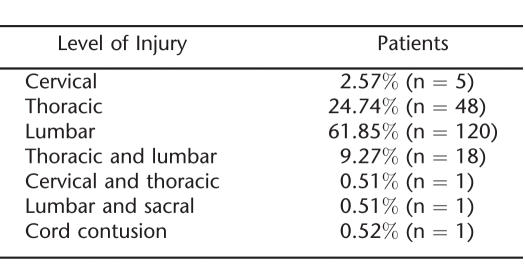
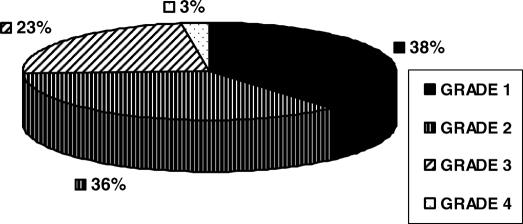
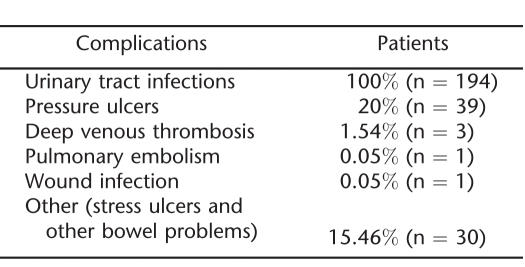
The male-to-female ratio was approximately 1:3 (n = 50 [26%] and n = 144 [74%], respectively). The majority (78% [n = 151]) were 16 to 39 years of age; 62% (n = 120) had lumbar-level injuries, 25% (n = 48) had thoracic-level injuries, 9% (n = 18) had thoracolumbar-level injuries, and a few had cervical- or sacral-level injuries. Forty-six percent (n = 90) had American Spinal Injury Association type A injuries; 4% (n = 8) were graded B, 11% (n = 21) were graded C, 9% (n = 18) were graded D, and 14% (n = 27) were graded E. Twenty percent (n =39) developed pressure ulcers, of which 38% (n = 15) had grade 1, 36% (n = 14) had grade 2, 23% (n = 9) had grade 3, and 3% (n = 1) had grade 4. All patients developed urinary tract infections; 15% (n = 30) had bowel complaints; 2% (n = 3) developed deep-vein thrombosis (1 died of pulmonary embolism); and 0.05% (n = 1) developed wound infection.
Conclusion:
Awareness of potential complications in patients with paraplegia is essential to care planning in the disaster setting. The priorities include skin, bowel, and bladder care and provision of prophylactic heparin. SCI post-disaster care requires comprehensive long-term planning.
Keywords: Spinal cord injuries, Complications, Earthquake, Pakistan, Paraplegia, Tetraplegia, Pressure ulcers, Neurogenic bladder
INTRODUCTION
This study was conducted on 194 patients who suffered spinal cord injuries (SCI) in the earthquake affecting Northern Pakistan on October 8, 2005. Almost 87,000 people died, 100,000 were severely injured, approximately 16,000 educational institutions were destroyed, and more than 2 million people were rendered homeless. Due to its geographical location, Rawalpindi Medical College (RMC) and its allied hospitals in Rawalpindi were the main hospitals where the casualties were brought, and, being final year medical students, we were involved in the care of these patients. The catchment area of RMC and its allied hospitals (tertiary care hospitals) is Azad Jammu Kashmir, including mainly Muzaffarabad, Balakot, Bagh, and Rawlakot. Besides serving the population of Rawalpindi and Islamabad, the teaching hospitals also served as major referral centers for northern Punjab and Azad Kashmir (1). Of all the earthquake victims, approximately 600 suffered SCI, many resulting in paraplegia (2). There are no data available regarding the exact proportion with tetraplegia, but in our study 4 patients of 194 had tetraplegia.
The aim of our research was to study the types of complications these patients developed and their exact number so that proper interventional measures could be adopted to prevent and treat these complications and so that the available health care providers and resources could be better utilized. The complications we anticipated in our study population included pressure ulcers, urinary tract infections (UTIs) due to long-term catheterization, constipation, wound sepsis, and thromboembolic events (eg, deep-vein thrombosis [DVT], pulmonary embolism).
PATIENTS AND METHODS
This was a hospital-based cross-sectional descriptive study conducted at the surgery/neurosurgery departments of District Headquarters Hospital (DHQ), Holy Family Hospital (HFH), Rawalpindi General Hospital (RGH), and Melody Relief and Rehabilitation Center (MRRC) Islamabad from October 10, 2005, through December 10, 2005.
Inclusion criteria: After obtaining the proper informed consent, we recruited all patients of any age who suffered SCI in the recent earthquake who were admitted in these above-mentioned hospitals. Excluded were patients with other diseases of the spinal cord and those who did not sustain their SCI in the recent earthquake.
A total of 194 patients with SCI were identified (122 in RMC and allied hospitals and 72 in MRRC, Islamabad). The level of injury was assessed clinically and radiologically, and grading was done on the basis of American Spinal Injury Association (ASIA) classification. The data included information about the demographics, treatment administered, and outcomes and various complications that developed in these patients. Except for 72 patients admitted to MRRC, the other patients included in our study were given 20 mg of low–molecular weight heparin (LMWH) (Enoxopion) subcutaneously once daily and were observed for thromboembolic complications.
RESULTS
One hundred and thirty-four patients with SCI were admitted to RMC and its allied hospitals, of which 12 were discharged very early and therefore could not be included in the study. Of 122 patients in RMC and allied hospitals and 72 patients in MRRC, Islamabad, 74% (n = 144) were female and 26% (n = 50) were male; 77% (n = 151) were 16 to 39 years of age; 62% of injuries occurred at the lumbar level, 25% (n = 48) at the thoracic level, 9% (n = 18) at the thoracolumbar level, and a few at the cervical or sacral levels. Forty-six percent (n = 90) had ASIA type A injuries; 4% (n = 8) were graded B, 11% (n = 21) were graded C, 9% (n = 18) were graded, D and 14% (n = 27) were graded E (Figures 1 and 2; Table 1). Twenty percent (n = 39) developed pressure ulcers, of which 38% (n = 15) had grade 1, 36% (n = 14) had grade 2, 23% (n = 9) had grade 3, and 3% (n = 1) had grade 4 (Figure 3). All patients developed UTIs (culture and sensitivity tests confirmed their presence), 15% (n = 30) had bowel complaints; 2% (n = 3) developed DVT (1 died of pulmonary embolism), and 0.05% (n = 1) developed a wound infection.
Figure 1. Age distribution of patients.
Figure 2. Grading according to the American Spinal Injury Association scoring classification.
Table 1.
Levels of Spinal Cord Injury
Figure 3. Pie chart showing grades of pressure ulcers.
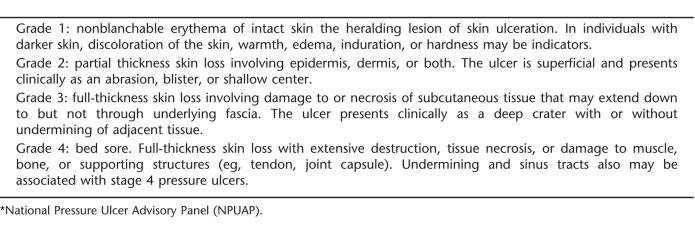
Of the 20% of patients who developed pressure ulcers, 69% (n = 27) were admitted to RMC and allied hospitals and 31% (n = 12) were admitted to MRRC (Table 2). Pressure ulcer grading was based on the guidelines of the National Pressure Ulcer Advisory Panel (3) (Table 3).
Table 2.
Complications Among Patients with Paraplegia
Table 3.
Pressure Ulcer Grading Guidelines*
DISCUSSION
Spinal cord injury is one of the most devastating of all traumatic events. It often results in loss of some or all of an individual's sensation and movement (4), rendering patients prone to both short- and long-term complications. Long-term complications include bowel problems, fractures due to demineralization of bones, psychological problems (eg, post-traumatic stress disorder), and pressure ulcers. Various short-term complications include pressure ulcers, DVT and pulmonary embolism, and UTI due to long-term indwelling catheters. Virtually all of the patients experienced UTI in our study. Their water intake was increased, and appropriate antibiotics were given according to the culture sensitivity reports. Certain structural and physiological factors, such as bladder overdistention, vesicoureteral reflux, high-pressure voiding, large postvoid residuals, stones in the urinary tract, and outlet obstruction, increase the risk of infection. The method of bladder drainage also influences the risk of UTI, and most persons with SCI on indwelling or intermittent catheterization develop UTI. The associations of behavioral and demographic factors with the risk of UTI are less well understood (5).
A complete SCI isolates the urinary apparatus from voluntary control and from the brain centers that coordinate contraction of the bladder with relaxation of the sphincter. Patients with upper-motor-neuron lesions may have a local reflex of bladder contraction (reflex voiding), but it often occurs against high sphincter pressure (bladder-sphincter dyssynergia), which in turn results in high intravesical pressure, thus contributing to the risk of infection and deterioration of the upper urinary tract. In patients with a flaccid bladder (eg, those with an injury of the conus medullaris), voiding can occur by overflow, with a large volume of residual urine and a high risk of infection (6).
Bladder function deteriorates immediately after a SCI and is a major complication. The incidence of UTI in the traumatic SCI population is as high as 67.1% (7). In a cohort study done in Thuringian Spinal Cord Rehabilitation Center, Sülzhayn, Germany, from January 1994 to December 1995, 170 patients with SCI (40 females, 130 males; mean age = 35.6 years) were studied. At the time of transfer to the rehabilitation center, 48.8% of the patients still had an indwelling urethral catheter, 29.4% had a suprapubic catheter, and only 16.5% of the patients were on intermittent catheterization. The urine cultures were positive in 100, 44, and 28.6%, respectively. Severe complications due to an indwelling urethral catheter were seen in 15 patients (8).
In our study, 39 of 194 (20%) patients developed pressure ulcers. Among patients who are neurologically impaired, pressure ulcers occur with an annual incidence of 5 to 8%, with the lifetime risk estimated to be 25 to 85%. Moreover, pressure ulcers are listed as the direct cause of death in 7 to 8% of all individuals with paraplegia (9–13). In our study, most of the pressure ulcers were grades 1 (38%) and 2 (36%); 23% were grade 3, and 3% were grade 4. After taking due care, (ie, daily dressings and 2-hour schedules for change of posture), most of the pressure ulcers healed.
Management of the bowels can be a challenging aspect of paraplegia, especially to the newly injured. However, because of limited alternatives, the methods of management have not changed significantly over the years (14). In our study, 15% of the miscellaneous complications consisted of bowel problems, mostly constipation. For this purpose, these patients were given laxatives and diets rich in fiber. They were also given Kleen enemas, and manual removal of stool was done in some severely constipated patients. A study by Glickman and Kamm (15) found that once a person adapted to paralysis, a major complaint or concern was bowel dysfunction. Another study by Levi et al (16) revealed that almost 41% of people rated bowel dysfunction as a moderate to severe life-limiting problem.
The general risk factors for thromboembolic complications are age, history of polytrauma, SCI with paralysis, long bone/pelvic fracture, family history of DVT, prolonged immobilization, and anesthesia time of more than 2 hours. Thromboembolic phenomena are also common in such patients because of prolonged immobilization. Therefore, the patients who were under study received prophylactic heparin, as did non-SCI patients determined to be at risk for thromboembolic complications. They were assessed clinically (examination of pulses, development of lower-limb swelling, chest auscultation for the development of pulmonary embolism) for the development of DVT because the inflow of patients was so high that it was not possible for us to do Doppler examination of each patient due to limited resources and time constraints. Of the SCI patients, 3 developed DVT and 1 died of pulmonary embolism in spite of receiving prophylactic heparin. Pulmonary complications are directly correlated with mortality, and both are related to the level of neurologic injury. Catheter-associated upper-extremity DVT carries a 12 to 36% risk of pulmonary embolism (17). In a recent retrospective study by Powell et al, 38.6% of patients admitted to a rehabilitation hospital were receiving DVT prophylaxis (18). Clinically apparent DVT occurs in approximately 15% of patients with acute SCI, and pulmonary embolism develops in approximately 5% of these patients. The risk of DVT is highest in the first 2 weeks after injury, with peak occurrence from days 7 to 10 post injury. Deep-vein thrombosis has been detected as early as 72 hours post injury; however, risk prior to this time appears to be low (18). Acute SCI is a thrombophilic state resulting from altered fibrinolytic and platelet function and abnormal concentrations of clotting factors. Patients with SCI are frequently burdened with the classic risk factors of Virchow's triad: stasis, hypercoagulability, and intimal trauma (18).
There were various limitations in our study. After 2 months, we lost contact with many patients, and so proper follow up could not be done. We studied only the short-term complications because it is too early to comment upon the long-term ones, but we are anticipating some long-term complications, including post-traumatic stress disorder. Pakistan is not fully equipped to cope with disasters of such magnitude. Immediately after the earthquake, it was a race against time as patients with all kinds of injuries were pouring in, including patients with SCI who needed a tremendous amount of care and attention. This study underscores the need for a proper health care system so that we are well prepared for such major disasters. A comprehensive approach is required that must include medical and nursing services; occupational, physical, and recreational therapy; counseling and social services; educational and instructional programs; and the follow-up services and rehabilitation that are essential to good health maintenance for individuals with SCI.
CONCLUSION
From our study, we concluded that patients with paraplegia are prone to develop various complications, especially UTIs, pressure ulcers, thromboembolic phenomenon (eg, DVT, pulmonary embolism), and bowel problems. Their surgical wounds may become infected if not properly treated, as happened with one of the patients in our study. We focused on short-term complications, but we are anticipating some long-term complications, including psychosocial problems. Only 3 proper rehabilitation centers are at present working in Pakistan: 1 in Peshawar, the Armed Forces Institute of Rehabilitation Medicine in Rawalpindi, and the National Institute of Health in Islamabad (19). A few rehabilitation centers are temporarily opened elsewhere, eg, the MRRC. More rehabilitation centers are needed because the number of people with SCI was greater than in previous disasters, and trained staff are also needed to handle such patients at the existing tertiary care centers.
REFERENCES
- Rawalpindi Medical College Allied hospitals. Available at http://www.rmc.edu.pk/allied_hospitals/. Accessed December 10, 2005.
- Naveed A. No special facilities for earthquake victims. THE NEWS. Islamabad edition 2005. December 19.
- National Pressure Ulcer Advisory Panel NPUAP Staging Report, November 2003. Available at http://www.npuap.org. Accessed January 4, 2007.
- Spinal Injuries Ireland The spine. Available at http://www.siairl.org/spinal/Main/The%20Spine.htm. Accessed December 15, 2005.
- Cardenas DD, Hooton TM. Urinary tract infection in persons with spinal cord injury. Arch Phys Med Rehabil. 1995;76(3):272–280. doi: 10.1016/s0003-9993(95)80615-6. [DOI] [PubMed] [Google Scholar]
- Ditunno JF, Formal CS. Chronic spinal cord injury. N Engl J Med. 1994;330:550–556. doi: 10.1056/NEJM199402243300808. [DOI] [PubMed] [Google Scholar]
- McKinley WO, Tewksbury MA, Godbout CJ. Comparison of medical complications following non traumatic and traumatic spinal cord injury. J Spinal Cord Med. 2002;25(2):88–93. doi: 10.1080/10790268.2002.11753607. [DOI] [PubMed] [Google Scholar]
- Zermann DH, Wunderlich H, Derry F, Schröder S, Schubert J. Audit of early bladder management complications after spinal cord injury in first-treating hospitals. Eur Urol. 2000;37(2):156–160. doi: 10.1159/000020133. [DOI] [PubMed] [Google Scholar]
- Berlowitz DR, Wilking SV. Risk factors for pressure sores: a comparison of cross-sectional and cohort-derived data. J Am Geriatr Soc. 1989;37:1043–1050. doi: 10.1111/j.1532-5415.1989.tb06918.x. [DOI] [PubMed] [Google Scholar]
- Brandeis GH, Ooi WL, Hossain M, Morris JN, Lipsitz LA. A longitudinal study of risk factors associated with the formation of pressure ulcers in nursing homes. J Am Geriatr Soc. 1994;42:388–393. doi: 10.1111/j.1532-5415.1994.tb07486.x. [DOI] [PubMed] [Google Scholar]
- Crenshaw RP, Vistnes LM. A decade of pressure sore research: 1977–1987. J Rehabil Res Dev. 1989;26:63–74. [PubMed] [Google Scholar]
- Dansereau JG, Conway H. Closure of decubiti in paraplegics. Plast Reconstr Surg. 1964;33:474–480. [PubMed] [Google Scholar]
- Staas WE, Jr, LaMantia JG. Decubitus ulcers and rehabilitation medicine. Int J Dermatol. 1982;21:437–444. doi: 10.1111/j.1365-4362.1982.tb03177.x. [DOI] [PubMed] [Google Scholar]
- Lansang RS, Krouskop AC. Bowel management. Available at: http://www.emedicine.com/pmr/topic230.htm (updated March 13, 2006). Accessed December 13, 2005.
- Glickman S, Kamm MA. Bowel dysfunction in spinal cord injury patients. Lancet. 1996;347(9016):1651–1653. doi: 10.1016/s0140-6736(96)91487-7. [DOI] [PubMed] [Google Scholar]
- Levi R, Hultling C, Nash M, Seger A. The Stockholm spinal cord injury study. 1. Medical problems in a regional SCI population. Paraplegia. 1995;33:308–315. doi: 10.1038/sc.1995.70. [DOI] [PubMed] [Google Scholar]
- McKinney D, Garstang SV. Prevention of thromboembolism in spinal cord injury. Available at http://www.emedicine.com/pmr/topic229.htm (updated March 22, 2006). Accessed December 15, 2005.
- Powell M, Kirshblum S, O'Connor KC. Duplex ultrasound screening for deep vein thrombosis in spinal cord injured patients at rehabilitation admission. Arch Phys Med Rehabil. 1999;80(9):1044–1046. doi: 10.1016/s0003-9993(99)90058-8. [DOI] [PubMed] [Google Scholar]
- Pakistan Link Amputees figure could reach to 1000 in various hospitals. Available at http://www.pakistanlink.com/Headlines/Nov05/19/08.htm. Accessed December 14, 2005.