Abstract
Background/Objective:
To report a case of keratinizing squamous metaplasia of the bladder treated with radical cystectomy.
Design:
Case report and discussion of management options.
Methods:
Keratinizing squamous metaplasia of the bladder is a rare entity that can result from chronic irritative stimuli involving the bladder. It is considered a premalignant condition associated with invasive squamous cell carcinoma. A case report is presented describing the diagnosis and management of keratinizing squamous metaplasia of the bladder in a tetraplegic man with a chronic indwelling urinary catheter.
Results:
Radical cystectomy with an Indiana continent reservoir was performed after cystoscopy with biopsy confirmed keratinizing squamous metaplasia. Final pathology revealed focal erosion and diffuse keratinizing squamous metaplasia of the bladder with prostatic adenocarcinoma as an incidental finding.
Conclusions:
Patients with spinal cord injury who use indwelling catheters for bladder management are at higher risk of developing keratinizing squamous metaplasia. Surveillance for early detection of this entity is recommended. Prophylactic cystectomy is sometimes warranted; however, observation and frequent cystoscopic surveillance to identify potential malignant transformation can be an alternative strategy. An interdisciplinary approach is recommended before consideration of bladder resection.
Keywords: Spinal cord injuries, Cystectomy, Neurogenic bladder, Tetraplegia, Metaplasia, Squamous, Epithelial growth factor receptor, Prostate
INTRODUCTION
After exposure to chronic irritative stimuli, the transitional epithelium of the bladder can occasionally undergo a histologic transformation to keratinizing squamous metaplasia. Although several theories have been proposed, chronic inflammation and infection are considered the most likely etiologic factors. Because of the frequent use of chronic indwelling catheters for bladder management, patients with spinal cord injury (SCI) are at increased risk of developing this condition. The diagnosis is made histologically after cystoscopy and biopsy are performed. However, once the diagnosis is made, it is controversial whether to perform surveillance by cystoscopy to look for potential malignant transformation or to perform a prophylactic radical cystectomy. We describe a case of keratinizing squamous metaplasia identified in the bladder of a man with SCI who used a chronic indwelling urinary catheter.
CASE REPORT
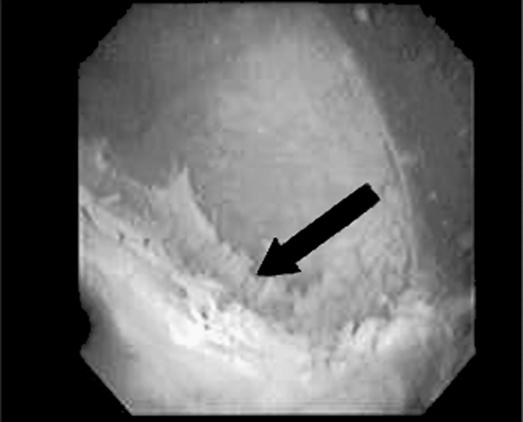
A 54-year-old man with tetraplegia who used a chronic indwelling catheter for bladder management was evaluated by the urology service for detrusor sphincter dyssynergia. As part of the work-up, a routine cystoscopy was performed. The bladder mucosa appeared abnormal, and the patient was taken to the operating room for repeat cystoscopy and biopsy, during which moderate to severe trabeculation was noted with multiple diverticula in the bladder wall. In addition, the mucosa was covered by flaky, white, plaque-like lesions (Figure 1). Multiple cold-cup biopsies were performed, and the pathologic diagnosis revealed squamous metaplasia with keratinization. The patient was subsequently taken back to the operating room for a cystoscopy and attempt at complete transurethral resection of this lesion; however, because of diffuse involvement of the bladder mucosa and growth within diverticula, complete resection was not possible. Pathologic diagnosis again revealed squamous metaplasia with keratin but no evidence of malignancy.
Figure 1. Bladder wall showing flaky, white, plaque-like lesions during cystoscopy (arrow).
An interdisciplinary team was formed in which medical providers, a social worker, nursing staff, and family members took an active role so that the patient was able to make an informed decision. He was offered continued observation vs prophylactic radical cystoprostatectomy. Because of the premalignant nature of this unresectable lesion, the patient elected to undergo radical cystectoprostatectomy with an Indiana pouch continent reservoir. The procedure was performed, and the patient experienced no complications in the perioperative period. Final pathologic diagnosis revealed diffuse keratinizing squamous metaplasia with no evidence of urothelial malignancy. However, incidentally, a small focus (<5%) of Gleason 3+4 adenocarcinoma of the prostate was identified with negative surgical margins. The patient has not needed additional treatment for prostate cancer, and his prostate-specific antigen remains undetectable. The patient was discharged home with instructions to perform clean intermittent catheterization of his continent reservoir every 4 hours. On 18-month follow-up, he had no evidence of malignancy and was able to manage his continent reservoir adequately.
DISCUSSION
Keratinizing squamous metaplasia is considered a pre-malignant condition with a reported incidence of 23% in patients with SCI who use indwelling catheters for bladder management (1,2). In patients diagnosed with keratinizing squamous metaplasia, the subsequent risk of developing bladder cancer has been estimated to be 21% to 32% (1,2). Khan et al (1) reviewed 34 patients with histologically proven keratinizing squamous metaplasia and postulated that some cases with synchronous or metachronous bladder cancer progress to carcinoma in situ and ultimately invasive tumor. Likewise, Guo et al (4) recently described findings of 5 patients diagnosed with keratinizing squamous metaplasia. Two of 5 (40%) were found to have invasive squamous cell carcinoma identified on cystectomy performed within 1 year of the initial diagnosis, and an additional 1 of 5 (20%) had persistent keratinizing squamous metaplasia on repeat bladder biopsy.
Although the exact pathophysiology underlying the transformation from keratinizing squamous metaplasia to squamous cell carcinoma is unknown, several etiologic factors have been linked its development (1,15). Chronic inflammation caused by indwelling catheters and stones, as well as infection secondary to parasites, are considered to be the most likely etiologic agents (1,3,4,8,12,13). Histopathologically, Guo et al (4) recently reported enhanced activity of epithelial growth factor receptor (EGFR) in keratinizing squamous metaplasia after cystectomy in patients with hematuria, as well as patients with urinary retention. EGFR is a tyrosine kinase that transduces signals controlling cell proliferation. Stonehill et al (2) reviewed 208 charts of patients with SCI with neurogenic bladder and chronic indwelling catheters and concluded that nearly all patients had inflammatory changes or squamous metaplasia of the bladder, whereas 1 patient had keratinizing squamous metaplasia.
Because of this increased risk, many centers recommend frequent surveillance to diagnosis lesions at a curable phase (2). For patients with SCI who have been managed with indwelling urinary catheters for less than 5 years and found to have limited keratinizing lesions, several investigators recommend annual cystoscopy and urinary cytology (1,2,6). For patients with SCI managed with indwelling urinary catheters for greater than 10 years with more extensive keratinizing lesions, attempts at reductive therapy with cauterization or silver nitrate fulguration are recommended (1,6). However, because of limited data on these types of protocols, no approach can be considered superior (1,2,10), and some have been proven ineffective (1,6,7). Most recently, some authors have suggested that EGFR could potentially be used as logic therapeutic target for keratinizing squamous metaplasia, among other bladder lesions, that are difficult to manage clinically (4,15). However, some investigators advocate for a more aggressive management with radical bladder resection to avoid development of malignant transformation (1,3,5–7).
Patients with SCI may experience significant difficulty adjusting to life-altering events including radical surgery (16–20). The psychologic and quality-of-life impact of prophylactic radical cystectomy in patients with keratinizing squamous metaplasia is unknown; however, performance of a radical cystectomy may affect many quality-of-life issues including stoma care, catheter use, and presence of incontinence, body image, and sexual dysfunction (21–25). Because of these significant concerns, we recommend that a team be formed including SCI specialists, urologists, nurses, social workers, psychologists, and family members to construct an individualized treatment for each affected patient.
CONCLUSION
Keratinizing squamous metaplasia of the bladder is a rare premalignant lesion, associated with chronic inflammation and infection. Management of this histologic entity remains controversial. Risk of development of keratinizing squamous metaplasia in patients with SCI is elevated, and radical bladder resection should be considered in certain cases. However, because of significant quality-of-life impact associated with prophylactic surgery, a team approach is advised to individualize treatment plans and to allow affected patients to make more informed decisions. Additionally, clinicians are encouraged to consider EGFR as a potential therapeutic target for interventions, although further research in this area is warranted.
REFERENCES
- Khan MS, Thornhill JA, Gaffney E, Loftus B, Butler MR. Keratinizing squamous metaplasia of the bladder: natural history and rationalization of management based on review of 54 years of experience. Eur Urol. 2002;42:469–474. doi: 10.1016/s0302-2838(02)00358-5. [DOI] [PubMed] [Google Scholar]
- Stonehill WH, Goldman HB, Dmochowski RR. The use of urine cytology for the diagnosing bladder cancer in spinal cord injured patients. J Urol. 1997;157:2112–2114. [PubMed] [Google Scholar]
- Ozbey, Aksoy Y, Polat O, Bicgi O, Demirel A. Squamous metaplasia of the bladder: findings in 14 patients and review of the literature. Int J Nephrol. 1999;31:457–461. doi: 10.1023/a:1007107110222. [DOI] [PubMed] [Google Scholar]
- Guo CC, Fine SW, Epstein JI. Noninvasive squamous lesions in the urinary bladder: a clinicopathologic analysis of 29 cases. Am J Surg Pathol. 2006;30:883–891. doi: 10.1097/01.pas.0000213283.20166.5a. [DOI] [PubMed] [Google Scholar]
- Kuruvilla S, Ramakrishna B, Nath V. Keratinising squamous metaplasia of the urinary bladder. Indian J Pathol Microbiol. 1994;37:S39–40. [PubMed] [Google Scholar]
- De Kock ML, Clark PB, Anderson CK. Vesical leucoplakia. S Afr Med J. 1980;58:725–728. [PubMed] [Google Scholar]
- Redman JF, Downs RA. Management of extensive leuko-plakia of bladder. Urology. 1975;6:759–761. doi: 10.1016/0090-4295(75)90815-8. [DOI] [PubMed] [Google Scholar]
- Wiener DP, Koss LG, Sablay B, Freed SZ. The prevalence and significance of Brunn's nests, cystitis cystica and squamous metaplasia in normal bladders. J Urol. 1979;122:317–321. doi: 10.1016/s0022-5347(17)56384-3. [DOI] [PubMed] [Google Scholar]
- Witherington R. Leukoplastic keratinizing tumor of the bladder. J Urol. 1967;1998:206–208. doi: 10.1016/S0022-5347(17)62856-8. [DOI] [PubMed] [Google Scholar]
- Bahnson RR. Squamous cell carcinoma of the bladder. Editorial. J Urol. 1997;157:2115. doi: 10.1016/s0022-5347(01)64689-5. [DOI] [PubMed] [Google Scholar]
- Hess MJ, Zhan EH, Foo DK, Yalla SV. Bladder cancer in patients with spinal cord injury. J Spinal Cord Med. 2003;26:335–338. doi: 10.1080/10790268.2003.11753702. [DOI] [PubMed] [Google Scholar]
- Kaufman JM, Fam B, Jacobs SC, et al. Bladder cancer and squamous metaplasia in spinal cord injury patients. J Urol. 1977;118:967–971. doi: 10.1016/s0022-5347(17)58266-x. [DOI] [PubMed] [Google Scholar]
- Locke JR, Hill DE, Walzer Y. Incidence of squamous cell carcinoma in patients with long-term catheter drainage. J Urol. 1985;133:1034–1035. doi: 10.1016/s0022-5347(17)49366-9. [DOI] [PubMed] [Google Scholar]
- West DA, Cummings JM, Longo WE, Virgo KS, Johnson FE, Parra RO. Role of chronic catheterization in the development of bladder cancer in patients with spinal cord injury. Urology. 1999;53:292–297. doi: 10.1016/s0090-4295(98)00517-2. [DOI] [PubMed] [Google Scholar]
- Tungerkar MF, Linehan J. Patterns of expressions of transforming growth factor and epidermal growth factor receptor in squamous cell lesions of the urinary bladder. J Clin Pathol. 1998;51:583–587. doi: 10.1136/jcp.51.8.583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brillhart B. Studying the quality of life and life satisfaction among persons with spinal cord injury undergoing urinary management. Rehabil Nurs. 2004;29:122–126. doi: 10.1002/j.2048-7940.2004.tb00328.x. [DOI] [PubMed] [Google Scholar]
- Lucke KT, Coccia H, Goode JS, Lucke JF. Quality of life in spinal cord injured individuals and their caregivers during the initial 6 months following rehabilitation. Qual Life Res. 2004;13:97–110. doi: 10.1023/B:QURE.0000015284.95515.17. [DOI] [PubMed] [Google Scholar]
- Lucke KT. Knowledge acquisition and decision-making: spinal cord injured individuals' perceptions of caring during rehabilitation. SCI Nurs. 1997;14:87–95. [PubMed] [Google Scholar]
- Moreno JG, Chancellor MB, Karasick S, King S, Abdill CK, Rivas DA. Improved quality of life and sexuality with continent urinary diversion in quadriplegic women with umbilical stoma. Arch Phys Med Rehabil. 1995;76:758–762. doi: 10.1016/s0003-9993(95)80531-1. [DOI] [PubMed] [Google Scholar]
- Kulaksizoglu H, Toktas G, Kulaksizoglu IB, Aglamis E, Unluer E. When should quality of life be measured after radical cystectomy? Eur Urol. 2002;42:350–355. doi: 10.1016/s0302-2838(02)00351-2. [DOI] [PubMed] [Google Scholar]
- Mansson A, Davidsson T, Hunt S, Mansson W. The quality of life in men after radical cystectomy with a continent cutaneous diversion or orthotopic bladder substitution: is there a difference? BJU Int. 2002;90:386–390. doi: 10.1046/j.1464-410x.2002.02899.x. [DOI] [PubMed] [Google Scholar]
- Mansson A, Mansson W. When the bladder is gone: quality of life following different types of urinary diversion. Review. World J Urol. 1999;17:211–218. doi: 10.1007/s003450050135. [DOI] [PubMed] [Google Scholar]
- Gerharz EW, Mansson A, Mansson W. Review. Quality of life after cystectomy and urinary diversion: an evidence based analysis. Urology. 2005;174:1729–1736. doi: 10.1097/01.ju.0000176463.40530.05. [DOI] [PubMed] [Google Scholar]
- Janzen J, Bersch U, Pietsch-Breitfeld B, Pressler H, Michel D, Bultmann B. Urinary bladder biopsies in spinal cord injured patients. Spinal Cord. 2001;39:568–570. doi: 10.1038/sj.sc.3101218. [DOI] [PubMed] [Google Scholar]
- Porter MP, Wei JP, Penson DF. Quality of life issues in bladder cancer patients following cystectomy and urinary diversion. Urol Clin North Am. 2005;32:207–216. doi: 10.1016/j.ucl.2005.01.002. [DOI] [PubMed] [Google Scholar]