Abstract
Background/Objective:
To examine and compare demographics and functional outcomes for individuals with spinal cord injury (SCI) clinical syndromes, including central cord (CCS), Brown-Sequard (BSS), anterior cord (ACS), posterior cord (PCS), cauda equina (CES), and conus medullaris (CMS).
Design:
Retrospective review.
Setting:
Tertiary care, level 1 trauma center inpatient rehabilitation unit.
Participants:
Eight hundred thirty-nine consecutive admissions with acute SCIs.
Main Outcomes Measures:
Functional independence measure (FIM), FIM subgroups (motor, self-care, sphincter control), length of stay (LOS), and discharge disposition.
Results:
One hundred seventy-five patients (20.9%) were diagnosed with SCI clinical syndromes. CCS was the most common (44.0%), followed by CES (25.1%) and BSS (17.1%). Significant differences (P ≤ 0.01) were found between groups with regard to age, race, etiology, total admission FIM, motor admission FIM, self-care admission and discharge FIM, and LOS. Statistical analysis between tetraplegic BSS and CCS revealed significant differences (P ≤ 0.01) with respect to age (39.7 vs 53.2 years) and a trend toward significance (P ≤ 0.05) with regard to self-care admission and discharge FIM. No significant differences (P ≤ 0.01) were found when comparing CMS to CES.
Conclusions:
SCI clinical syndromes represent a significant proportion of admissions to acute SCI rehabilitation, with CCS presenting most commonly and representing the oldest age group with the lowest admission functional level of all SCI clinical syndromes. Patients with cervical BSS seem to achieve higher functional improvement by discharge compared with patients with CCS. Patients with CMS and CES exhibit similar functional outcomes. Patients with ACS and PCS show functional gains with inpatient rehabilitation, with patients with ACS displaying the longest LOS of the SCI clinical syndromes. These findings have important implications for the overall management and outcome of patients with SCI.
Keywords: Central cord syndrome, Rehabilitation, Spinal cord injuries, Cord syndromes, Central, Anterior, Posterior, Conus medullaris, Cauda equina, Brown-Sequard syndrome, Functional outcome
INTRODUCTION
It is estimated that the annual incidence of spinal cord injury (SCI) is approximately 40 per million in the United States, with approximately 11,000 new cases each year (1). A subset of SCIs has been grouped by their clinical presentation into 6 SCI syndromes: central cord syndrome (CCS), Brown-Sequard syndrome (BSS), anterior cord syndrome (ACS), posterior cord syndrome (PCS), conus medullaris syndrome (CMS), and cauda equina syndrome (CES). Most patients will need inpatient rehabilitation during the acute period after an SCI before returning to the community. There is limited literature on functional outcomes after inpatient rehabilitation for patients with these SCI clinical syndromes as a group.
BSS is defined as a lesion that produces ipsilateral proprioceptive and motor loss and contralateral loss of sensitivity to pain and temperature below the level of the lesion (2,3). BSS accounts for 1% to 4% of all traumatic SCIs (4–6). Only a limited number of patients have the pure form of BSS—much more common is Brown-Sequard plus syndrome (7), which refers to a relative ipsilateral hemiplegia with a relative contralateral hemi-analgesia. Although BSS traditionally has been associated with knife injuries, a variety of etiologies may cause this syndrome (7–9). BSS has the best prognosis for ambulation of the SCI clinical syndromes. It has been shown that 75% to 90% of patients ambulate independently at discharge from rehabilitation (6,7). According to Roth et al (7), the most important predictor of function is whether the upper or lower limb is the predominant site of weakness; when the upper limb is weaker than the lower limb, patients are more likely to ambulate at discharge (7).
CCS was first described by Schneider in 1954: “It is characterized by disproportionately more motor impairment of the upper than the lower extremities, bladder dysfunction, usually urinary retention, and varying degrees of sensory loss below the level of the lesion” (10). Evidence from clinical-pathologic magnetic resonance imaging (MRI) correlation studies revealed that this pattern may not be based on locations of the arm and leg fibers within the corticospinal tract, but rather that the corticospinal tract subserves mainly distal limb musculature, and thus, the functional deficit would be more pronounced in the hands when the tract is the primary site of damage (11). It is considered the most common of the SCI syndromes, accounting for approximately 9% of all traumatic SCIs (6). The syndrome is classically known to affect older persons with cervical spondylosis and a hyperextension injury, where cord compression occurs between bony spurs anteriorly and infolded ligamenta flava posteriorly (10,12). Studies have reported fall as the most common etiology, followed by motor vehicle crashes (13). CCS generally has a favorable prognosis for functional recovery. Penrod et al (14) noted that older patients with CCS have a worse prognosis for ambulation (97% vs 41%) relative to younger patients (14). Favorable prognostic factors that have been previously documented include good hand function, evidence of early motor recovery, young age, absence of spasticity, higher admission Modified Barthel Index (MBI) scores, preinjury employment, absence of lower extremity neurologic motor impairment at rehabilitation admission, and presence of documented upper and lower extremity strength improvement during rehabilitation (13–18).
ACS was described by Schneider in 1955. This is a lesion that affects the anterior two thirds of the spinal cord while preserving the posterior columns. It is characterized by complete paralysis with hyperesthesia and hypoalgesia below the level of the lesion, together with preservation of touch, position, 2-point discrimination, and vibratory sense (6). Its reported incidence is 2.7% of all traumatic SCIs (6). It has been associated with flexion injuries, direct damage by bone fragment or disk compression, or from vascular insufficiency produced by the occlusion of the anterior spinal artery (6,19,20). This syndrome carries a poor prognosis for functional improvement, with only a 10% to 20% chance of muscle recovery, and even in those with some recovery, there is poor muscle power and coordination (21).
PCS is the least common of the SCI clinical syndromes, with an incidence of less than 1% (6). The American Spinal Injury Association (ASIA) has actually omitted this syndrome from recent versions of their international standards for classification of SCI (22,23). Clinically, it is described as a selective lesion of the posterior columns resulting in a loss of proprioceptive and vibration sense below the level of injury, but with preservation of muscle strength, temperature, and pain sensation. It has been linked to neck hyperextension injuries, posterior spinal artery occlusion, tumors, disk compression, and vitamin B12 deficiency.
CMS is an injury of the sacral cord (conus) and lumbar nerve roots within the spinal canal. This condition is characterized by a combination of upper and lower motor neuron signs. Findings include saddle anesthesia, areflexic bladder and bowel, and variable degrees of lower extremity weakness. Trauma and tumors are among the most common etiologies responsible for this condition.
CES is not considered a true SCI. Instead, it is an injury to the lumbosacral nerve roots within the neural canal. Clinically, it can present similarly to CMS with saddle anesthesia, bladder and bowel dysfunction, and variable lower extremity involvement. However, this is considered a pure lower motor neuron lesion with the absence of upper motor neuron signs, and it is characterized by asymmetric lower extremity weakness. CES can occur as the result of trauma, tumors, spinal stenosis, disc compression, infection, or postsurgical epidural hematoma. It can be an acute process or a chronic and slowly progressive condition. It is believed to have a better prognosis for neurological recovery than SCIs because nerve roots have the ability to regenerate. One study found that the most important predictors for favorable outcome in CES were early diagnosis and surgical decompression (24).
SCI clinical syndromes represent a significant proportion of SCI admissions to inpatient rehabilitation. There is limited literature available describing the demographics and functional outcomes of this population, as a group, in a rehabilitative setting. The objective of this study was to examine and compare the demographic and injury characteristics along with functional outcomes for individuals presenting with these SCI syndromes during inpatient rehabilitation. A greater understanding of these issues will hopefully enhance clinical care and rehabilitation outcomes for this patient population.
METHODS
Subjects
Data were reviewed from 839 consecutive patients with SCIs who were admitted to an acute rehabilitation unit of an urban tertiary care medical center from 1992 through 2004. Patients were examined by trained rehabilitation physicians and classified according to the ASIA examination (22,23) standards as having (a) SCI clinical syndrome (BSS, CCS, ACS, PCS, CMS or CES), (b) mixed-type SCI, or (c) complete SCI. For the purposes of this study, a complete SCI was defined as an injury resulting in the complete loss of sensory and motor function in the lowest sacral segment in the absence of an SCI clinical syndrome. A mixed-type SCI was defined as any incomplete SCI in the absence of a clinical syndrome. The criteria for inclusion in the study were (a) a diagnosis of an SCI clinical syndrome and (b) meeting admission criteria for acute inpatient rehabilitation. In this study, patients were classified as having an SCI clinical syndrome according to the following definitions: CCS, a lesion characterized by sacral sensory sparing and greater weakness in the upper limbs than in the lower limbs; BBS, a lesion that produces relatively greater ipsilateral proprioceptive and motor loss with contralateral loss of sensitivity to pain and temperature; ACS, a lesion that produces variable loss of motor function and of sensitivity to pain and temperature, while preserving proprioception; PCS, a lesion that produces loss of proprioceptive and vibration sense while preserving muscle strength, temperature, and pain sensation; CMS, injury of the sacral cord (conus) and lumbar nerve roots within the spinal canal characterized by upper and lower motor neuron signs producing bowel and bladder dysfunction with associated variable motor loss to the lower extremities; CES, injury to the lumbosacral nerve roots within the neural canal characterized by lower motor neuron signs with resulting in areflexic bladder, bowel, and lower limbs.
Measures
Data were collected and reviewed for each patient with a diagnosis of SCI clinical syndrome. Demographic characteristics included age, sex, race/ethnicity, and marital status. Injury characteristics included etiology of injury, ASIA impairment classification, and neurologic level of injury. Rehabilitation outcomes included rehabilitation length of stay, discharge disposition, and functional status as assessed by the functional independence measure (FIM) (25). The specific functional scores examined for this project included FIM motor scores, self-care scores, sphincter control scores, and mobility transfer scores; change and efficacy scores were also calculated for each variable. FIM motor scores ranged from 13 to 91, with higher scores reflecting greater levels of independence. Self-care scores reflect level of independence in eating, grooming, bathing, upper and lower body dressing, and toileting. Sphincter control scores reflect level of independence with bladder and bowel management. Mobility scores reflect level of independence with regards to bed/chair/wheelchair transfers, toilet transfers, and tub/shower transfers. FIM change scores were calculated based on the difference between rehabilitation admission and discharge. FIM efficiency scores were calculated by dividing change scores by the respective duration of stay in rehabilitation.
Data Analysis
Statistics, including proportions, means, and SD, were compiled for all demographic and outcome measures. One-way analysis of variance procedures were used to examine the group differences on continuous variables. Those variables that violated assumptions of homosce-dasticity were analyzed using nonparametric statistics (Kruskal-Wallis χ2). χ2 nonparametric statistics were also used to examine group differences on nominal and ordinal level outcomes. Because of the number of comparisons being conducted, an α level of P ≤ 0.01 was chosen. We chose not to use Rasch analysis scaling, which is often used to produce an interval scale of FIM motor items (an ordinal scale) and requiring that the data to be analyzed represent the influence of a single underlying unidimensional variable. Argument exists that there are limitations in applying Rasch analytical procedures to FIM data obtained using this type of scale, noting that FIM items may not conform closely enough to the Rasch model to support generalizable and useful measures (26,27).
RESULTS
Incidence
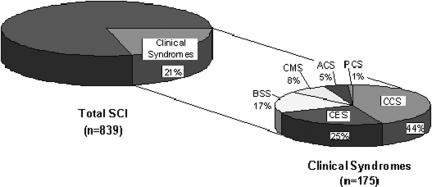
Of the 839 patients admitted for inpatient rehabilitation after an SCI, 20.9% (n =175) were diagnosed with an SCI clinical syndrome. CCS was the most common, accounting for nearly one half (44%) of the SCI clinical syndrome cases and representing 9.2% of all SCIs in this study. The incidences of CES and BSS were also significant, representing 5.2% and 3.6%, respectively, of all SCIs. CMS was only found in 1.7% of the SCI cases, whereas ACS and PCS were the least common, each with an incidence of less than 1% (Figure 1).
Figure 1. Incidence of SCI clinical syndromes (n = 839).
Demographics
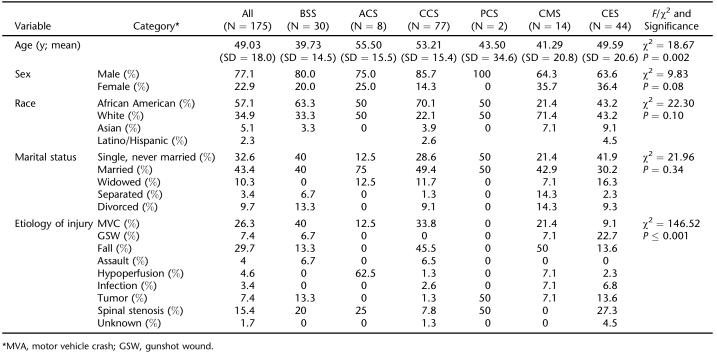
Of the 175 individuals with an SCI clinical syndrome, 77.1% were men, and 57.1% were African American (34.9% non-Hispanic white, 7.4% other). Age ranged from 17 to 95 years of age, and 43.4% of the participants were married (32.6% were single, never married). The demographic characteristics of SCI syndromes differed from one another. In general, patients with CCS, CES, and ACS were oldest, whereas those with BSS had the youngest mean age. No statistically significant differences were noted among the groups with regard to sex, race, or marital status (Table 1).
Table 1.
Demographic Characteristics
Injury Characteristics
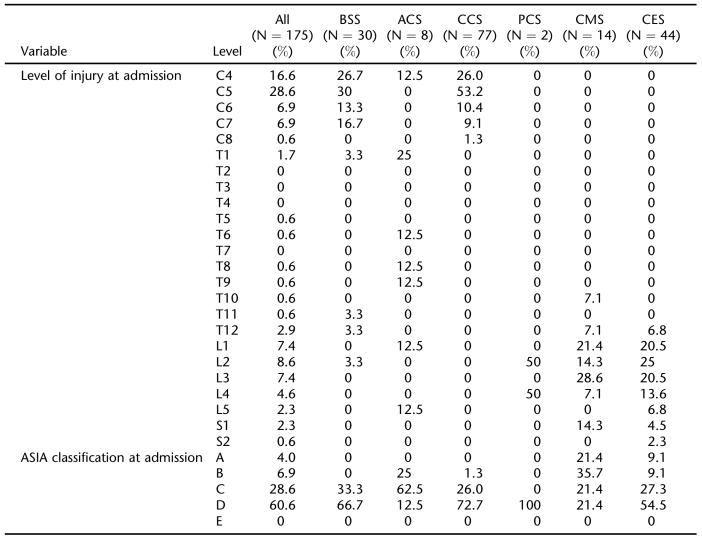
The level of injury at admission for patients with SCI syndromes, as a group, ranged from C4 to S2. The highest percentage of individuals suffered C5 and C4 injuries (28.6% and 16.6%, respectively). Although no inferential statistics were calculated, level of injury is distinctly different between syndromes. All of the patients diagnosed with CCS and most (87.2%) of those diagnosed with BSS had levels of injury between C4 and C8. In contrast, 100% of patients diagnosed with CES and 92.9% of patients with CMS were injured between T12 and S2 levels (Table 2).
Table 2.
Injury Characteristics
Although the majority of the patients with an SCI syndrome were classified as ASIA D at admission (60.6%), the degree of incompleteness also differed among the groups. Most patients with CCS (62.5%), BSS (66.7%), and CES (54.5%) and all of patients with PCS were diagnosed initially with ASIA D injuries. In contrast, ASIA B was the most frequent ASIA classification for individuals with CMS (35.7%), and ASIA C was the most common for patients with ACS (62.5%).
SCI clinical syndromes were found to be the result of both traumatic and nontraumatic etiologies, with falls and motor vehicle accidents accounting for more than 50% of the injuries. Patients with CCS and CMS were most likely to be injured by falls (45.5% and 50%, respectively), whereas motor vehicle accidents was the primary etiology for patients with BSS (40%). In contrast, ACS and PCS were more frequently the result of a nontraumatic etiology. CES injuries were almost equally caused by traumatic and nontraumatic etiologies.
Functional Outcomes
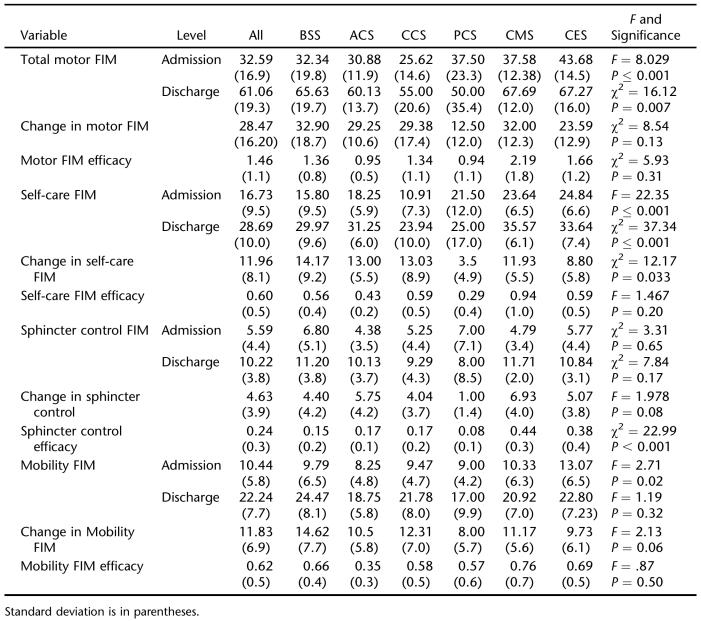
The average change in motor FIM score for patients diagnosed with an SCI clinical syndrome was 28.5, with average admission and discharge motor FIM scores of 32.6 and 61.1, respectively. Significant differences were found between patients with CCS and CES at both admission and discharge (P = 0.007 and P < 0.001, respectively). Patients with CCS had the lowest admission motor FIM (25.6), whereas patients with CES were the most motor independent at admission, with a FIM score of 43.7. However, no significant differences were noted related to change in motor FIM scores or motor FIM efficacy between diagnostic groups (Tables 3 and 4).
Table 3.
Rehabilitation Outcomes
Table 4.
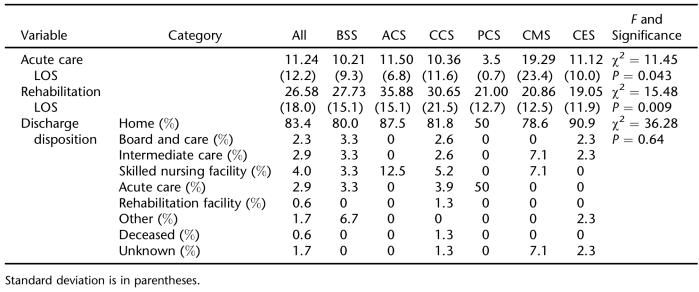
Length of Stay (LOS) and Disposition
Self-care FIM scores also improved in this population, as a group, from an average of 16.7 at admission to an average of 28.7 at rehabilitation discharge. With regard to admission self-care FIM scores, statistically significant differences were found between patients with CCS (10.9) and CES (24.8), CCS (10.9) and CMS (23.6) (P < 0.001), and BBS (15.8) and CES (24.8). Discharge self-care FIM scores were also statistically different between groups. Specifically, significance was found between CCS (23.9) and CMS (35.6), as well as CCS (23.9) and CES (33.6). Changes in self-care between groups approached significance (P =0.033). Individuals with PCS and CES showed the least progress, with changes in self-care FIM of 3.5 and 8.8, respectively, whereas patients with BSS showed the most improvement in this area, with a change in self-care FIM score of 14.2.
FIM scores related to sphincter control were not significant between groups at either admission or discharge. During admission, patients with PCS (7.00 ± 7.1 SD) and BSS (6.80 ± 5.1) showed the highest levels of control/independence; at discharge, patients with BSS (11.20 ± 3.8) and CMS (11.71 ± 2.0) showed the highest levels of independence. Although FIM change scores did not differ significantly between groups, FIM efficacy for sphincter control was significantly different between groups. Patients with BSS (0.15 ± 0.2) and CCS cord (0.17 ± 0.1) showed significantly (P < 0.001) less change per day than patients with CES (0.38 ± 0.4) and CMS (0.44 ± 0.3).
Mobility FIM scores improved for patients with an SCI syndrome, as a group, from 10.44 at admission to 22.24 at discharge during rehabilitation. However, no significant differences were found related to mobility scores among the syndromes.
The average rehabilitation length of stay for patients with an SCI clinical syndrome was 27 days. Patients with CES had a statistically significant (P = 0.008) shorter length of stay than those with CCS (19 and 31 days, respectively). Patients with ACS had the longest average rehabilitation length of stay (36 days). Discharge disposition did not differ significantly between the syndromes, with most patients (81.8%) being discharged home.
Finally, additional comparisons were performed between groups with similar neurologic levels of injury. Patients with cervical BSS were compared with those with CCS, and individuals with CMS were contrasted to those with CES. A few statistically significant differences were found between patients with CCS and those with BSS, including age at injury (P < 0.001), motor FIM at discharge (P = 0.022), self-care at admission (P = 0.011) and discharge (P = 0.008), and sphincter control at discharge (P = 0.02). Comparisons of patients with CMS with those with CES found only 1 trend toward differences—change in motor FIM (P = 0.049).
DISCUSSION
Characteristics of SCI Syndromes
SCI syndromes represent a significant percentage of SCI rehabilitation admissions. This study reports that nearly one fifth (20.9%) of all patients with SCI admitted to rehabilitation had injury patterns consistent with an SCI clinical syndrome (ie, CCS, BSS, ACS, PCS, CMS, and CES). It should be noted that this study reviewed both traumatic and nontraumatic SCI etiologies. As such, there is potential for overstating the effect of the SCI on the patient's disability secondary to differences in primary illness and comorbidities. SCI represents a challenging injury with potential long-term functional impairments and disability; thus, increased recognition of potential functional outcomes remains very important. Previous literature related to SCI incidences and outcomes have more often pertained to the overall SCI population or to those with complete injuries (1,28–31). Much less has addressed incomplete SCI or specific clinical syndromes.
The most commonly identified clinical syndrome in this study was CCS, representing nearly 50% of individuals with an SCI syndrome and accounting for approximately 9% of all SCIS. These findings are similar to previously reported incidence for traumatic CCS (6). CES and BSS also reflect a significant proportion of this patient population, with an incidence of 5% and 4% of all SCI rehabilitation admissions, respectively. The least frequently represented syndromes within this study included ACS and PCS. Combined, they were only diagnosed in 1% of all SCI admissions.
Patients with SCI syndromes were found to be more often men and African Americans. Male sex is more common in traumatic SCI, and this study found that this pattern is also seen in patients with SCI clinical syndromes. African American ethnic background represents approximately 22% of all SCIs; however, in this study, it represented 57% of all patients with an SCI clinical syndrome. This ethnic/racial breakdown likely reflects the local SCI population demographics (60% African American) and should not be taken to imply that SCI syndromes are necessarily more common in the African-American population.
Since 2000, the average age for patients with traumatic SCI has been 38 years, with persons older than 60 years representing 10.9% of SCI cases (1,32,33). This study showed that patients suffering from SCI clinical syndromes are significantly older than the general SCI population, with an average age of 49 years. BSS and CMS individuals tend to be the youngest with an average age of 40 years, whereas patients with ACS and CCS are the oldest, with average ages of 55 and 53 years, respectively. The difference in age found between the general SCI population and patients with SCI syndromes is probably a reflection of the etiologies and the mechanisms of injury associated with SCI syndromes. Tumors, spinal stenosis, and falls are primarily seen in older individuals, and they accounted for 52% of all SCI syndrome cases in this study (34–36).
SCI clinical syndromes were found to be the result of both traumatic and nontraumatic etiologies. In the SCI literature, it is estimated that about two thirds of all SCI are the result of a traumatic event (most frequently motor vehicle accidents and falls). As a group, SCI clinical syndromes were also found to be more frequently the result of trauma. Nontraumatic etiologies accounted for 31% of the SCI clinical syndromes (36,37). This is likely a reflection of the large number of patients diagnosed with CES secondary to a nontraumatic etiology such as spinal stenosis. Nontraumatic etiologies were more common than traumatic injuries for patients with ACS (89%) and PCS (100%), whereas it represented approximately one half of all CES. Our findings for CCS were consistent with the literature, which states that most cases are the result of trauma, most commonly falls and motor vehicles crashes (10,12). Trauma was by far the most common etiology for patients diagnosed with CMS. One half of the injuries in this study were the result of a fall.
The majority of patients with SCI clinical syndromes had motor incomplete SCIs at the time of their admission to rehabilitation. Greater than 75% of patients were classified as having an ASIA C or an ASIA D type of SCI, with ASIA D being the most common. Specifically, ASIA D was the most frequent impairment classification for most of the patients with CCS, BSS, and CES and for all of the patients with PCS. This indicates a high degree of incompleteness and the potential for a more favorable functional outcome. Unlike most patients with an SCI syndrome, individuals with CMS were primarily classified as ASIA A and ASIA B (21% and 36%, respectively). Therefore, these patients will generally have significant bowel and bladder dysfunction and need management training as part of their rehabilitation program. Classically, CES and CMS have been described as exhibiting similar clinical presentations. However, this study indicates that individuals with CES are more likely to be motor incomplete compared with those with a CMS injury, which tend to result in either a complete or only a sensory incomplete injury pattern.
Incomplete tetraplegia is the most frequent neurologic category of persons with SCI and those with SCI syndromes. Patients with CCS and BSS accounted for the vast majority of the patients in this category. As expected, patients with CMS and CES were all classified with paraplegia, with their neurologic level of injury more commonly between L1 and L3.
Functional Outcomes After SCI Syndromes
An important objective of acute SCI rehabilitation is to maximize patient functional outcomes. Completeness of injury and neurologic level of injury are important factors in predicting functional outcome after SCI (29,30,38). Incomplete SCIs tend to indicate a more favorable prognosis. Tetraplegia is clearly more functionally impairing than paraplegia; however, depending on the degree of motor-sensory sparing, there can be great variation in functional ability and recovery potential. As mentioned previously, most patients with SCI syndromes are diagnosed with either incomplete tetraplegia or incomplete paraplegia, and this study shows their favorable functional outcome after rehabilitation. As a group, patients with SCI syndromes showed improvement in all functional outcome areas measured in this study. Additionally, greater than 80% of these patients successfully discharged home after completion of their inpatient rehabilitation.
Individuals with a diagnosis of CCS had the lowest mean admission motor and self-care FIM scores (more functionally impaired). This is likely a reflection of their bilateral upper extremity (especially hand) weakness, which significantly impairs their ability to perform activities of daily living, as well as the use of mobility aids (walker, crutches, or wheelchair). Their older age and associated comorbidities may also be factors in these findings. Although their discharge motor and self-care FIM scores were among the lowest of the patients with SCI syndromes, individuals with CCS exhibited marked functional gains in both areas.
As noted previously, individuals with paraplegia are expected to have a higher admission functional level compared with those with tetraplegia, secondary to their ability to use the upper extremities to complete functional self-care and mobility tasks. This is consistent with our finding that patients with CMS and CES injuries had the highest admission motor and self-care FIM scores of the SCI syndromes. This was true despite the fact that the majority of patients with CCS and BSS were classified as ASIA D at admission, whereas patients with CMS more commonly were ASIA B.
The average rehabilitation length of stay (LOS) for patients with SCIs has continued to decline over the years (1,28,30). It has been reported that the average rehabilitation LOS for the general SCI population is 45 days (1). This study shows that patients with an SCI syndrome have shorter LOSs than the general SCI population (27 vs 45 days). This is likely secondary to the higher percentage of incomplete injuries found in individuals diagnosed with an SCI syndrome. LOS was shortest in patients with CES, a clinical group mostly classified as incomplete paraplegics in this study. This clinical group is associated with higher FIM scores, denoting increased functional abilities.
CONCLUSIONS
SCI clinical syndromes represent a significant proportion of admissions to acute SCI rehabilitation, with CCS presenting most commonly and representing the oldest age group with the lowest admission functional level of all SCI clinical syndromes. Individuals with cervical BSS seem to achieve higher functional improvement by discharge compared with patients with CCS. Patients with CMS or CES exhibit similar functional outcomes. ACS and PCS show functional gains with inpatient rehabilitation, with patients with ACS displaying the longest LOS of the SCI clinical syndromes. These findings have important implications for the overall management and outcome of patients with SCI. A greater understanding of incidence and outcomes may allow for enhanced goal-setting and functional expectations. Future research is needed to further define outcome within specific clinical groups and compare outcomes between like groups (ie, between CCS and cervical BSS or between CES and CMS).
Of Interest to SCI Professionals…
2007
-
August 27–29
American Paraplegia Society
53rd Annual Conference
Gaylord Palms & Resort
Kissimmee, Florida
-
September 17–20
International Meeting on Upper Limb in Tetraplegia
Shriners Hospitals for Children
Philadelphia, Pennsylvania
www.mcjconsulting.com/tetraplegia
 Abstract Deadline: March 1, 2007
Abstract Deadline: March 1, 2007
2008
-
June 19–22
ASIA 34th Annual Scientific Meeting
Loew's Coronado Bay Resort
San Diego, CA
-
August 11–13
American Paraplegia Society
54th Annual Conference
Gaylord Palms & Resort
Kissimmee, Florida
 Abstract Deadline Dec. 21, 2007
Abstract Deadline Dec. 21, 2007 -
August 29–September 3
47th ISCoS Annual Scientific Meeting
Durban, South Africa
http://www.iscos.org.uk/meetings.html
 Abstract Deadline Jan. 29, 2008
Abstract Deadline Jan. 29, 2008
Footnotes
This research was supported in part from the National Institute on Disability and Rehabilitation Research in the Office of Special Education and Rehabilitation Services in the US Department of Education to the Regional Spinal Cord Injury Center of Virginia Commonwealth University (H133N000015-05).
REFERENCES
- National Spinal Cord Injury Statistical Center . Spinal Cord Injury: Facts and Figures at a Glance. Birmingham, AL: National Spinal Cord Injury Statistical Center; 2005. [Google Scholar]
- American Spinal Injury Association . Standards for Neurological and Functional Classification of Spinal Cord Injury. Chicago, IL: American Spinal Injury Association; 1992. [Google Scholar]
- Burns SP, Golding DG, Rolle WA, et al. Recovery of ambulation in motor incomplete tetraplegia. Arch Phys Med Rehabil. 1997;78:1169–1172. doi: 10.1016/s0003-9993(97)90326-9. [DOI] [PubMed] [Google Scholar]
- Brown-Sequard CE. Lectures on the physiology and pathology of the central nervous system and the treatment of organic nervous affections. Lancet. 1868;2:593–595. 659–662, 755–757, 821–823. [Google Scholar]
- Bohlman HH. Acute fractures and dislocations of the cervical spine: an analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg Am. 1979;61:1119–1142. [PubMed] [Google Scholar]
- Bosch A, Stauffer ES, Nickel VL. Incomplete traumatic quadriplegia: a ten-year review. JAMA. 1971;216:473–478. [PubMed] [Google Scholar]
- Roth EJ, Park T, Pang T, et al. Traumatic cervical Brown-Sequard and Brown-Sequard plus syndrome: the spectrum of presentations and outcomes. Paraplegia. 1991;29:582–589. doi: 10.1038/sc.1991.86. [DOI] [PubMed] [Google Scholar]
- Gentleman D, Harrington M. Penetrating injury of the spinal cord. Injury. 1984;16:7–8. doi: 10.1016/0020-1383(84)90101-3. [DOI] [PubMed] [Google Scholar]
- Koehler PJ, Endtz LJ. The Brown Sequard syndrome: true or false? Arch Neurol. 1986;43:921–924. doi: 10.1001/archneur.1986.00520090051015. [DOI] [PubMed] [Google Scholar]
- Schneider RC, Cherry GR, Patek H. Syndrome of acute central cervical spinal cord injury with special reference to mechanisms involved in hyper-extension injuries of cervical spine. J Neurosurg. 1954;11:546–577. doi: 10.3171/jns.1954.11.6.0546. [DOI] [PubMed] [Google Scholar]
- Levi AD, Tator CH, Bunge RP. Clinical syndromes associated with disproportionate weakness of the upper versus the lower extremities after cervical spinal cord injury. Neurosurgery. 1996;38:179–185. doi: 10.1097/00006123-199601000-00039. [DOI] [PubMed] [Google Scholar]
- Waters R, Adkins R, Sie I, et al. Motor recovery following spinal cord injury associated with cervical spondylosis: a collaborative study. Spinal Cord. 1996;34:711–715. doi: 10.1038/sc.1996.129. [DOI] [PubMed] [Google Scholar]
- Tow AM, Kong KH. Central cord syndrome: functional outcome after rehabilitation. Spinal Cord. 1998;36:156–160. doi: 10.1038/sj.sc.3100618. [DOI] [PubMed] [Google Scholar]
- Penrod LE, Hegde SK, Ditunno JF. Age effect on prognosis for functional recovery in acute, traumatic central cord syndrome. Arch Phys Med Rehabil. 1990;71:963–968. [PubMed] [Google Scholar]
- Merriam WF, Taylor TKF, Ruff SJ, et al. A reappraisal of acute traumatic central cord syndrome. J Bone Joint Surg Br. 1986;68:708–713. doi: 10.1302/0301-620X.68B5.3782229. [DOI] [PubMed] [Google Scholar]
- Rand RW, Crandall PH. Central spinal cord syndrome in hyperextension injuries of the cervical spine. J Bone Joint Surg Am. 1962;44:1415–1422. [PubMed] [Google Scholar]
- Shrosbree RD. Acute central cervical spinal cord syndrome—aetiolgy, age incidence and relationship to the orthopaedic injury. Paraplegia. 1977;14:251–258. doi: 10.1038/sc.1976.42. [DOI] [PubMed] [Google Scholar]
- Roth EJ, Lawler MH, Yarkony GM. Traumatic central cord syndrome: clinical features and functional outcomes. Arch Phys Med Rehabil. 1990;71:18–23. [PubMed] [Google Scholar]
- Cheshire WP, Santos CC, Massey EW, et al. Spinal cord infarction: etiology and outcome. Neurology. 1996;47:321–330. doi: 10.1212/wnl.47.2.321. [DOI] [PubMed] [Google Scholar]
- Bauer RD, Errico TJ. Cervical spine injuries. In: Errico TJ, Bauer RD, Waugh T, editors. Spinal Trauma. Philadelphia, PA: JB Lippincott; 1991. pp. 71–121. [Google Scholar]
- Bohlman HH, Ducker TB. Spine and spinal cord injuries. In: Rothman RH, editor. The Spine. 3rd ed. Philadelphia, PA: WB Saunders; 1992. pp. 973–1011. [Google Scholar]
- American Spinal Injury Association/International Medical Society of Paraplegia . International Standards for Neurological and Functional Classification of Spinal Cord Injury Patients. Chicago, IL: American Spinal Injury Association/International Medical Society of Paraplegia; 1996. [Google Scholar]
- American Spinal Injury Association/International Medical Society of Paraplegia . International Standards for Neurological and Functional Classification of Spinal Cord Injury Patients. Chicago, IL: American Spinal Injury Association/International Medical Society of Paraplegia; 2000. [Google Scholar]
- Kennedy JG, Soffe KE, McGrath A, et al. Predictors of outcome in cauda equina syndrome. Eur Spine J. 1999;8:317–322. doi: 10.1007/s005860050180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton B, Granger C, Sherwin F, Zielezny M, Tashman JA. Uniform national data system for medical rehabilitation. In: Fuhrer MJ, editor. Rehabilitation Outcomes: Analysis and Measurement. Baltimore, MD: Brooks; 1987. pp. 137–147. [Google Scholar]
- Dickson HG, Köhler F. The multi-dimensionality of the FIM motor items precludes an interval scaling using Rasch analysis. Scand J Rehabil Med. 1996;26:159–162. [PubMed] [Google Scholar]
- Wright BD, Lincare JM, Smith RM, Heinemann AW, Granger CV. FIM measurement properties and Rasch model details. Scand J Rehabil Med. 1997;29:267–272. [PubMed] [Google Scholar]
- Eastwood EA, Hagglund KJ, Ragnarsson KT, Gordon WA, Marino RJ. Medical rehabilitation length of stay and outcomes for persons with traumatic spinal cord injury—1990–1997. Arch Phys Med Rehabil. 1999;80:1457–1463. doi: 10.1016/s0003-9993(99)90258-7. [DOI] [PubMed] [Google Scholar]
- Kirshblum S, O'Connor K. Levels of injury and outcome in traumatic spinal cord injury. Phys Med Rehabil Clin North Am. 2000;11:1–27. [PubMed] [Google Scholar]
- Stover S, DeLisa JA, Whiteneck GG. Spinal Cord Injury: Clinical Outcomes From the Model Systems. Gaithersburg, MD: Aspen Publishing; 1995. [Google Scholar]
- Ditunno JF, Jr, Cohen ME, Formal C, Whitehead GG. Functional outcomes. In: Stover SL, Whiteneck GG, DeLisa JA, editors. Spinal Cord Injury: Clinical Outcomes From the Model Systems. Gaithersburg, MD: Aspen Publishing; 1995. pp. 170–184. [Google Scholar]
- McKinley W, Cifu D, Seel R, Meade M. Age-related outcome in tetra and paraplegia: a summary paper. J Neurorehabil. 2003;18:83–90. [PubMed] [Google Scholar]
- DeVivo MJ, Kartus PL, Rutt RD, Stover SL, Fine PR. The influence of age at time of spinal cord injury on rehabilitation outcome. Arch Neurol. 1990;47:687–691. doi: 10.1001/archneur.1990.00530060101026. [DOI] [PubMed] [Google Scholar]
- McKinley WO, Conti-Wyneken A, Vokac C, Cifu D. Rehabilitative functional outcome of patients with neoplastic spinal cord compression. Arch Phys Med Rehabil. 1996;77:892–895. doi: 10.1016/s0003-9993(96)90276-2. [DOI] [PubMed] [Google Scholar]
- McKinley W, Tellis A, Cifu D, et al. Rehabilitation outcome of individuals with nontraumatic myelopathy resulting from spinal stenosis. J Spinal Cord Med. 1998;21:131–136. doi: 10.1080/10790268.1998.11719521. [DOI] [PubMed] [Google Scholar]
- McKinley W, Seel R, Gadi R. Nontraumatic vs traumatic SCI, rehab outcome comparison. Am J Phys Med Rehabil. 2001;80:693–699. doi: 10.1097/00002060-200109000-00010. [DOI] [PubMed] [Google Scholar]
- McKinley WO, Hardman J, Seel R. Nontraumatic spinal cord injury: incidence, epidemiology and functional outcome. Arch Phys Med Rehabil. 1998;79:1186–1187. doi: 10.1016/s0003-9993(99)90162-4. [DOI] [PubMed] [Google Scholar]
- Ditunno J, Flanders A, Kirshblum S, Graziani V, Tessler A. Predicting outcome in traumatic spinal cord injury. In: Kirshblum S, Campagnolo D, DeLisa J, editors. Spinal Cord Medicine. Philadelphia, PA: Lippincott Williams & Wilkins; 2002. pp. 108–122. [Google Scholar]