Abstract
Background/Objective:
For persons with spinal cord injury (SCI), severe bodily pain is related to a lower quality of life. However, the effect of pain from a specific body region on quality of life has yet to be determined. The shoulder joint is a common site of pain among persons with SCI. Therefore, our purpose was to identify the relationship of self-reported shoulder pain with quality of life, physical activity, and community activities in persons with paraplegia resulting from SCI.
Methods:
Eighty participants with shoulder pain who propel a manual wheelchair (mean age: 44.7 years; mean duration of injury: 20 years; injury level T1-L2) completed the following questionnaires: Wheelchair User's Shoulder Pain Index, Subjective Quality of Life Scale, Physical Activity Scale for Individuals with Physical Disabilities, and Community Activities Checklist. Correlations between shoulder pain scores and quality of life, physical activity, and community activities were determined using Spearman's rho test.
Results:
Shoulder pain intensity was inversely related to subjective quality of life (rs = − 0.35; P =0.002) and physical activity (rs = − 0.42; P < 0.001). Shoulder pain intensity was not related to involvement in community activities (rs =− 0.07; P = 0.526).
Conclusions:
Persons with SCI who reported lower subjective quality of life and physical activity scores experienced significantly higher levels of shoulder pain. However, shoulder pain intensity did not relate to involvement in general community activities. Attention to and interventions for shoulder pain in persons with SCI may improve their overall quality of life and physical activity.
Keywords: Spinal cord injuries, Paraplegia, Shoulder pain, Wheelchair, Quality of life
INTRODUCTION
For persons with spinal cord injury (SCI), lower limb paralysis places a heavy reliance on the upper limbs for mobility and for performance of daily activities. In this case, the upper limbs sustain repetitive and often weight-bearing loads incurred by activities such as wheelchair propulsion (1–4), transfers (5), and raises (6,7). Since the shoulder is optimally designed for reaching and locating the hand in the environment (8,9), these weight-bearing loads lead to mechanical trauma and place the shoulder joint at risk for overuse (10). The sequela of this pattern of use is pain. When shoulder pain occurs in a person with SCI, mobility and daily activities are even further limited by this “secondary” disability. Unlike the nondisabled person who experiences shoulder pain, persons with SCI are not able to rest their shoulders when pain develops, as the upper limbs are required for all activities of daily living.
As a result, it is common for persons with SCI to experience shoulder pain at some point in their lives (11–14). Jensen and colleagues surveyed persons with SCI who were experiencing pain and determined that the shoulder was the most frequently (61%) reported site of pain (14). In a smaller study of women with paraplegia by Pentland and Twomey, the shoulder joint was also the most frequently reported site of pain (15).
Improvements in acute care of persons with SCI has resulted in increasing life expectancies (16). As a result, research in the area of quality of life (QOL) has become increasingly prominent in SCI literature. In persons who have recently been injured, QOL has been reported to, at least temporarily, decrease (17,18). Over time (within 2 to 5 y), psychosocial issues tend to stabilize and QOL tends to improve (17,19). Whether QOL returns to levels comparable to the nondisabled population is inconclusive (17–20). In a recent meta-analysis, however, Dijkers examined 22 studies and determined that the QOL of people with SCI was lower than in a non-SCI group in most instances (21).
There is a consensus among researchers that QOL is negatively impacted when individuals with SCI experience generalized bodily pain that limits their daily activities (19,22,23). Severity of pain levels in individuals with SCI has been shown to impact QOL. Lundqvist et al determined that severe bodily pain is related to lowered QOL scores (19). In addition, changes in QOL occurred when a change in bodily pain levels interfered with day-to-day activities (ie, work outside the home and housework) for those with SCI (23). However, the effect of isolated shoulder pain on the limitation of daily activities and QOL has not been studied.
It has been shown that for persons with SCI, involvement in community activities is significantly correlated with QOL (24). These activities include caring for one's self and participating in socially pleasurable events. Jensen and colleagues demonstrated that the presence of bodily pain in persons with SCI did not significantly affect their level of community integration (14). The impact of isolated shoulder pain on community involvement in persons with SCI has not been studied.
Despite the high prevalence of shoulder pain in this population, the relationship between shoulder pain intensity and quality of life, physical activity, and community involvement has not been established. Therefore, the purpose of this study was to investigate the relationship of shoulder pain intensity with quality of life, physical activity, and community activities in persons with paraplegia who propel a manual wheelchair. We hypothesized that increased shoulder pain intensity would be associated with decreased quality of life, decreased physical activity, and decreased community activity. A secondary purpose was to determine the influence of gender on subjective reports of shoulder pain intensity, quality of life, physical activity, and community activity.
METHODS
Eighty persons with traumatic paraplegia following a SCI participated in the study. These participants were recruited primarily from Rancho Los Amigos National Rehabilitation Center in Downey, California. Of the 80 participants recruited, 58 were men and 22 were women (73% and 27%, respectively). The mean age of the participants was 44.7 years (range 22–72 y). The mean duration of spinal injury was 20.2 years (range 3–53 y), and the level of injury ranged from T1 to L2 (complete SCI = 65, incomplete SCI = 15). The mean duration of shoulder pain experienced by the participants was 5.4 years (range: 1 mo–38 y). Sixty-three study participants (79% of our sample) utilized a manual wheelchair 100% of the time. Only 10 participants utilized a manual wheelchair 75 to 99% of the time, and 7 participants used a manual wheelchair 50 to 74% of the time. Of the 17 participants who did not use a manual wheelchair 100% of the time, 12 relied on a power wheelchair, and 5 ambulated part time.
Inclusion criteria for this study required that participants report shoulder pain in one or both arms that interfered with at least one daily activity and utilized a manual wheelchair for mobility at least 50% of the time. All participants were adults who experienced paraplegia as a result of a SCI with duration of injury of at least 3 years. Exclusion criteria were hospitalization within the last month for any medical condition, fracture within the last year to the painful arm, a surgical procedure within the last year to the painful arm, new injury within the last year to the painful arm, diagnosis of reflex sympathetic dystrophy/complex regional pain syndrome in the last year to the painful arm, a diagnosis of adhesive capsulitis in the last year to the painful arm, a diagnosis of rheumatoid arthritis, a cortisone injection to the painful shoulder within the last 4 months, and any serious medical condition. All participants signed an Institutional Review Board–approved informed consent form and were given the Human Subject's Bill of Rights.
Participants completed a series of questionnaires administered by an interview process. These instruments were administered in a consistent order and all questionnaires were completed during the same visit. Shoulder pain was assessed utilizing the Wheelchair User's Shoulder Pain Index score (WUSPI) (25). If participants were experiencing bilateral shoulder pain, the more painful shoulder was studied. The WUSPI provides an aggregate index of the intensity of shoulder pain during transfers, activities of daily living, and mobility performed from a wheelchair (25). The questionnaire utilizes a series of 15 visual analogue scales (VAS) consisting of 10-cm lines anchored by “no pain” and “worst pain ever experienced.” Participants were asked to mark an “X” on the line to describe their shoulder pain intensity during that activity. The responses were measured in centimeters and summed, allowing for a maximum total raw score of 150. Not all participants performed all the activities listed on the WUSPI. Therefore, the WUSPI was scored by using the performance-corrected score (PC-WUSPI), whereby the total raw score was divided by the number of activities performed and multiplied by 15 (26) The WUSPI has been shown to be both reliable and valid for people with SCI (27).
Subjective QOL status was recorded using the Subjective Quality of Life Scale (SQOL) (28). In this global measure of an individual's perception of his or her QOL, respondents are asked to “take everything in their life into account.” The SQOL Scale utilizes an ordinal scale from 1 to 7, where 1 means “life is very distressing; it's hard to imagine how it could get much worse”; 7 means “life is great; it's hard to imagine how it could get much better”; and 4 means “life is neither good nor bad.” The participant was asked to make a mark on the scale based on his/her subjective and global judgment of his/her QOL.
The Physical Activity Scale for Individuals With Physical Disabilities (PASIPD) queries information about the number of days and average hours in a day spent in a variety of activities (13 in total, including leisure, household, and work-related activities) over the last 7 days. The total score is the product of the average hours spent in an activity daily and the metabolic equivalents (MET) summed over each item for questions 2 through 13 (question 1 functions as a practice question) (29).
Finally, community involvement was determined using the Community Activities Checklist (CAC) (24). This 16-item questionnaire asks the individual to identify the number of times he or she participated in activities that pertain to social activities (7 questions), mobility items (4 questions), and attention-to-self activities (5 questions) within the last 7 days. These values are then summed for one overall score.
Data from the WUSPI, PASIPD, SQOL, and CAC were screened for normality using the Shapiro-Wilks test and were found to be significantly different than a normal curve; therefore, nonparametric statistics were chosen for analysis. Correlations between shoulder pain intensity scores and subjective QOL, physical function, and community activities were determined using Spearman's rho test. A Bonferroni correction for multiple comparisons was applied to this analysis, with a resultant level of significance of P < 0.02. A Mann-Whitney test was used to compare shoulder pain intensity and physical activity between men and women (P < 0.05).
RESULTS
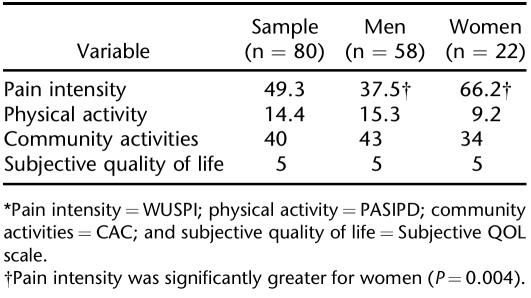
The overall median shoulder pain index score (WUSPI) for all 80 subjects was 49.3 (interquartile range: 14.7–72.2). Women reported significantly higher levels of shoulder pain than men did (66.2 vs 37.5, respectively: P =0.004) (Table 1).
Table 1.
Median Data for the 4 Primary Variables Measured*
The median physical activity score (PASIPD score) of all participants was 14.4 average metabolic equivalent (MET) hours per day (interquartile range: 7.5–24.0 h/d). The overall median SQOL was 5 (interquartile range: 4–6). The median community involvement (CAC) of the participants was a frequency of 40 activities per week (interquartile range: 26.3–57.0). There was no significant difference in physical activity (women 9.2 vs men 15.3; P = 0.096), SQOL (women 5 vs men 5; P = 0.469), or community activities (women 34 vs men 43; P = 0.203) between men and women (Table 1).
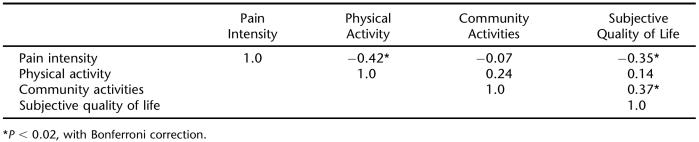
The intensity of shoulder pain was not related to duration of SCI (rs =− 0.11; P = 0.355) or the duration of shoulder pain (rs = − 0.02; P = 0.897). Shoulder pain intensity scores were inversely related to SQOL (rs = − 0.35; P = 0.002) (Table 2). There was a moderate, inverse relationship between shoulder pain intensity and physical activity, as measured by the PASIPD (rs = − 0.42; P < 0.001) (Table 2). There was no relationship, however, between shoulder pain intensity and community activities (rs = − 0.07; P = 0.526). The level of community activity was positively related to SQOL (rs = 0.37; P < 0.02) (Table 2).
Table 2.
Correlation Matrix for All Variables
DISCUSSION
The present investigation supported our hypothesis that higher levels of shoulder pain intensity would be associated with lower levels of subjective QOL and reduced levels of physical activity for persons with paraplegia following SCI. Higher levels of shoulder pain intensity, however, were not associated with reduced involvement in the community.
In this sample, higher levels of shoulder pain were associated with lower subjective QOL scores. Our study utilized a global QOL measure, which asks the participant to view life as a whole and does not guide users to think of particular domains of their lives (eg, physical function, socioeconomic status, relationships). With this understanding, it is not known which domain was used to determine their overall QOL. The relationship between shoulder pain and subjective QOL established in this investigation highlights the importance of addressing physical impairment in persons with SCI to improve overall QOL.
The overall distribution of the physical activity (PASIPD) scores was similar to those previously reported by Washburn and colleagues (29). In a population that mostly consisted of individuals with SCI, these researchers demonstrated that the majority of PASIPD scores were from 0 to 38 (29). Participants in this study reported participation in physical activities with an average MET hours/day value of 3.4, which corresponds to the lower end range of what is deemed as a moderate (3–6 METs) intensity level of physical activity by the Centers for Disease Control and Prevention (30). The relationship between shoulder pain intensity and physical activity indicates that persons experiencing greater shoulder pain had lower levels of physical activity.
Finally, for the population studied, higher intensities of shoulder pain were not related to the level of involvement in the community. However, the level of community activity was related to subjective quality of life. Our data suggest that some individuals are able to maintain high levels of community activity despite shoulder pain.
The limitation of the PASIPD measurement tool used in this study is that it utilizes a standard (average) MET for each activity that does not distinguish how the activity was actually performed, thereby resulting in similar scores for individuals who might have performed the activity at quite different intensity levels. The limitation of using the CAC in those with shoulder pain is that the vast majority of items in this questionnaire are social activities that do not necessarily require mobility. In this case, individuals with shoulder pain may be able to maintain higher community activity scores by participating in social activities that do not require increased use of the arms. An additional limitation of our study is that in many instances our subjects experienced pain in other regions of their bodies in addition to their shoulder pain; however, this information was not recorded.
Women experienced more intense levels of shoulder pain than men did. This finding is supported by previous research in nondisabled individuals revealing that women report higher levels of musculoskeletal pain (31). Furthermore, Andersson and colleagues identified that non-disabled women also experienced a greater prevalence of shoulder pain than men did (32). In the SCI literature, Cardenas et al determined that gender differences did not exist in the severity of generalized bodily pain (33). Higher levels of shoulder pain have been demonstrated in women with paraplegia compared to matched able-bodied women (15). Our study identified significant gender differences, with women reporting twofold higher levels of shoulder pain than men did. This is the first time men and women have been compared as a cohort using the same measure. Although women reported higher shoulder pain intensities, men and women had similar levels of physical activity.
These findings on the relationship of shoulder pain to quality of life and physical activity demonstrate the need to explore effective treatments to reduce or prevent shoulder pain in wheelchair users who have suffered a SCI. Currently, there is a lack of randomized controlled trials investigating the effectiveness of shoulder pain treatment strategies in this population.
CONCLUSION
Shoulder pain intensity negatively correlated with both physical activity and subjective quality of life. However, activities that keep individuals with SCI bonded with their community were maintained despite shoulder pain levels. Although women reported higher levels of shoulder pain, men and women had similar levels of physical activity.
Acknowledgments
This study was supported in part by a grant from the Foundation for Physical Therapy to establish PTClinRes-Net, a clinical research network to evaluate the efficacy of physical therapist practice. The authors thank Craig J. Newsam, DPT for his feedback on early drafts of this manuscript.
Footnotes
Funded by the Foundation for Physical Therapy, Inc., and the National Institute of Disability and Rehabilitation Research (Grant No.: H133B031002).
REFERENCES
- Mulroy SJ, Gronley JK, Newsam CJ, Perry J. Electromyo-graphic activity of shoulder muscles during wheelchair propulsion by paraplegic persons. Arch Phys Med Rehabil. 1996;77:187–193. doi: 10.1016/s0003-9993(96)90166-5. [DOI] [PubMed] [Google Scholar]
- Mulroy SJ, Farrokhi S, Newsam CJ, Perry J. Effects of spinal cord injury level on the activity of shoulder muscles during wheelchair propulsion: an electromyographic study. Arch Phys Med Rehabil. 2004;85:925–934. doi: 10.1016/j.apmr.2003.08.090. [DOI] [PubMed] [Google Scholar]
- Kulig K, Rao SS, Mulroy SJ, et al. Shoulder joint kinetics during the push phase of wheelchair propulsion. Clin Orthop Rel Res. 1998;354:132–143. doi: 10.1097/00003086-199809000-00016. [DOI] [PubMed] [Google Scholar]
- Kulig K, Newsam CJ, Mulroy SJ, et al. The effect of level of spinal cord injury on shoulder joint kinetics during manual wheelchair propulsion. Clin Biomech. 2001;16:744–751. doi: 10.1016/s0268-0033(01)00066-3. [DOI] [PubMed] [Google Scholar]
- Perry J, Gronley JK, Newsam CJ, Reyes ML, Mulroy SJ. Electromyographic analysis of the shoulder muscles during depression transfers in subjects with low-level paraplegia. Arch Phys Med Rehabil. 1996;77:350–355. doi: 10.1016/s0003-9993(96)90083-0. [DOI] [PubMed] [Google Scholar]
- Reyes ML, Gronley JK, Newsam CJ, Mulroy SJ, Perry J. EMG analysis of shoulder muscles of men with low-level paraplegia during a weight relief raise. Arch Phys Med Rehabil. 1995;76:433–439. doi: 10.1016/s0003-9993(95)80572-9. [DOI] [PubMed] [Google Scholar]
- Newsam CJ, Lee AD, Mulroy SJ, Perry J. Shoulder EMG during depression raise in men with spinal cord injury: the influence of lesion level. J Spinal Cord Med. 2003;26:59–64. doi: 10.1080/10790268.2003.11753662. [DOI] [PubMed] [Google Scholar]
- Walker-Bone K, Cooper C. Hard work never hurt anyone: or did it? A review of occupational associations with soft tissue musculoskeletal disorders of the neck and upper limb. Ann Rheum Dis. 2005;64:1381–1396. doi: 10.1136/ard.2004.026484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svendsen SW, Bonde JP, Mathiassen SE, Stengaard-Peder-sen K, Frich LH. Work related shoulder disorders: quantitative exposure-response relations with reference to arm posture. Occup Environ Med. 2004;61:844–853. doi: 10.1136/oem.2003.010637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soslowsky LJ, Thomopoulos S, Esmail A, et al. Rotator cuff tendinosis in an animal model: role of extrinsic and overuse factors. Ann Biomed Eng. 2002;30:1057–1063. doi: 10.1114/1.1509765. [DOI] [PubMed] [Google Scholar]
- Gellman H, Sie I, Waters RL. Late complications of the weight-bearing upper extremity in the paraplegic patient. Clin Orthop Rel Res. 1988;233:132–135. [PubMed] [Google Scholar]
- Dalyan M, Cardenas DD, Gerard B. Upper extremity pain after spinal cord injury. Spinal Cord. 1999;37:191–195. doi: 10.1038/sj.sc.3100802. [DOI] [PubMed] [Google Scholar]
- Sie IH, Waters RL, Adkins RH, Gellman H. Upper extremity pain in the post-rehabilitation spinal cord injured patient. Arch Phys Med Rehabil. 1992;73:44–48. [PubMed] [Google Scholar]
- Jensen MP, Hoffman AJ, Cardenas DD. Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord. 2005;43:704–712. doi: 10.1038/sj.sc.3101777. [DOI] [PubMed] [Google Scholar]
- Pentland WE, Twomey LT. The weight-bearing upper extemity in women with long term paraplegia. Paraplegia. 1991;29:521–530. doi: 10.1038/sc.1991.75. [DOI] [PubMed] [Google Scholar]
- National Spinal Cord Injury Statistical Center Spinal cord injury: facts and figures at a glance. J Spinal Cord Med. 2004;27:S139–S140. [PubMed] [Google Scholar]
- Stensman R. Adjustment to traumatic spinal cord injury: a longitudinal study of self-reported quality of life. Paraplegia. 1994;32:416–422. doi: 10.1038/sc.1994.68. [DOI] [PubMed] [Google Scholar]
- Dijkers MP. Quality of life of individuals with spinal cord injury: a review of conceptualization, measurement, and research findings. J Rehabil Res Dev. 2005;42:87–110. doi: 10.1682/jrrd.2004.08.0100. [DOI] [PubMed] [Google Scholar]
- Lundqvist C, Siosteen A, Blomstrand C, Lind B, Sullivan M. Spinal cord injuries: clinical, functional and emotional status. Spine. 1991;16:78–83. [PubMed] [Google Scholar]
- Krause JS. Longitudinal changes in adjustment after spinal cord injury: a 15-year study. Arch Phys Med Rehabil. 1992;73:564–568. [PubMed] [Google Scholar]
- Dijkers MP. Quality of life after spinal cord injury: a meta analysis of the effect of disablement components. Spinal Cord. 1997;35:829–840. doi: 10.1038/sj.sc.3100571. [DOI] [PubMed] [Google Scholar]
- Tate DG, Kalpakjian CZ, Forchheimer MB. Quality of life issues in individuals with spinal cord injury. Arch Phys Med Rehabil. 2002;83:S18–S25. doi: 10.1053/apmr.2002.36835. [DOI] [PubMed] [Google Scholar]
- Putzke JD, Richards JS, Hicken BL, DeVivo MJ. Interference due to pain following spinal cord injury: important predictors and impact on quality of life. Pain. 2002;100:231–242. doi: 10.1016/S0304-3959(02)00069-6. [DOI] [PubMed] [Google Scholar]
- Kemp BJ, Ettelson D. Quality of life while living and aging with a spinal cord injury and other impairments. Top Spinal Cord Inj Rehabil. 2001;6:116–127. [Google Scholar]
- Curtis KA, Roach KE, Applegate EB, et al. Development of the Wheelchair User's Shoulder Pain Index (WUSPI) Paraplegia. 1995;33:290–293. doi: 10.1038/sc.1995.65. [DOI] [PubMed] [Google Scholar]
- Curtis KA, Drysdale GA, Lanza RD, Kolber M, Vitolo RS, West R. Shoulder pain in wheelchair users with tetraplegia and paraplegia. Arch Phys Med Rehabil. 1999;80:453–457. doi: 10.1016/s0003-9993(99)90285-x. [DOI] [PubMed] [Google Scholar]
- Curtis KA, Roach KE, Applegate EB, et al. Reliability and validity of the Wheelchair User's Shoulder Pain Index (WUSPI) Paraplegia. 1995;33:595–601. doi: 10.1038/sc.1995.126. [DOI] [PubMed] [Google Scholar]
- Kemp BJ. Quality of life, coping and depression. In: Kemp BJ, Mosqueda L, editors. Aging With a Disability. Baltimore, MD: The John Hopkins University Press; 2004. pp. 48–67. [Google Scholar]
- Washburn RA, Zhu W, McAuley E, Frogley M, Figoni SF. The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil. 2002;83:193–200. doi: 10.1053/apmr.2002.27467. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Physical activity for everyone: measuring physical activity intensity: metabolic equivalent (MET) level. 2005. http://www.cdc.gov/nccdphp/dnpa/physical/measuring/met.htm. Accessed January 29, 2007.
- Unruh AM, Ritchie J, Merskey H. Does gender affect appraisal of pain and pain coping strategies? Clin J Pain. 1999;15:31–40. doi: 10.1097/00002508-199903000-00006. [DOI] [PubMed] [Google Scholar]
- Andersson HI, Ejlertsson G, Leden I, Rosenberg C. Chronic pain in a geographically defined general population: studies of differences in age, gender, social class, and pain localization. Clin J Pain. 1993;9:174–182. doi: 10.1097/00002508-199309000-00004. [DOI] [PubMed] [Google Scholar]
- Cardenas DD, Bryce TN, Shem K, Richards JS, Elhefni H. Gender and minority differences in the pain experience of people with spinal cord injury. Arch Phys Med Rehabil. 2004;85:1774–1781. doi: 10.1016/j.apmr.2004.04.027. [DOI] [PubMed] [Google Scholar]