Abstract
Background/Objective:
To determine factors associated with falls among a sample of ambulatory individuals with incomplete spinal cord injury (SCI).
Study Design:
Cross-sectional mail survey.
Methods:
A survey instrument of participant characteristics and fall-related variables was developed using relevant items from existing measures and was mailed to 221 individuals with incomplete SCI, who were identified from records of a large specialty hospital in the southeastern United States. Of the 221 prospective participants, 119 completed the questionnaire (54%). Multivariable logistic regression models were used to determine factors that were independently associated with having had a fall in the past year.
Results:
After adjusting for covariates, having fallen in the past year was significantly (P < 0.05) associated with greater numbers of medical conditions (odds ratio [OR] = 1.3; 95% confidence interval [CI] = 1.0–1.7), having arthritis (OR = 3.4, 95% CI = 1.2–9.6), experiencing dizziness (OR = 5.6, 95% CI = 1.1–27.7), greater numbers of days with poor physical health (OR = 1.1; 95% CI = 1.0–1.3), and the restriction of community activities because of fear of falling (OR = 1.5, 95% CI = 1.1–2.1). The multivariable models also showed that the odds of having fallen were significantly lower among those with better current perceived physical health (OR = 0.5; 95% CI = 0.3–0.9), those with better perceived health compared to a year ago (OR = 0.4; 95% CI = 0.2–0.8), individuals who exercised more frequently (OR = 0.2; 95% CI = 0.1–0.7), and those who used a walker (OR = 0.3; 95% CI = 0.1–0.9).
Conclusions:
Results suggest that interventions that address exercise frequency, walker use, and dizziness have promise for reducing falls for individuals with incomplete SCI.
Keywords: Spinal cord injuries, Incomplete, Walking, Falls, Prevention and control, Injury, Risk factors
INTRODUCTION
Although traumatic spinal cord injury (SCI) generally results in the need for a wheelchair as the sole mode of mobility, individuals with neurologically incomplete injuries sometimes have sufficient preserved function for ambulation (1). However, the quality and degree of ambulation may be affected by spasticity, muscle weakness, and coactivation of muscle groups (2). Thus, ambulation may be restricted to certain locations such as the home, may be limited to shorter distances, and may require the support of an assistive device.
The ability to ambulate may be impacted over time by physiologic changes in body systems. Neurologic decline, a frequent complication in the years after SCI, may lead to new weakness, numbness, and diminished function (3). Musculoskeletal system disorders, particularly osteoporosis and osteoarthritis, are also common and may limit overall function (4). Diseases of the cardiovascular system such as atherosclerosis appear earlier in life for those with SCI compared with the able-bodied population (5,6), Atherosclerosis may affect carotid and vertebral arteries and cause dizziness and visual disturbances with certain head positions. All of these factors can contribute to an increase in falls and related injuries.
The incidence of injuries subsequent to SCI was first investigated in a study of 1,328 persons who were at least 1-year posttraumatic SCI (7). Individuals who were ambulatory had a greater incidence of subsequent injuries in the 12 months before the study because of a variety of causes, including falls. Impaired balance or gait associated with falls may have contributed to the greater occurrence of injuries in this group. Although falls may have accounted for a number of injuries, this study considered injuries of a variety of causes and did not address falls exclusively.
The incidence, circumstances, and consequences of falls were recently reported for 119 ambulatory individuals with incomplete SCI (8). This study revealed that 75% of participants (n = 89) sustained at least 1 fall over the previous year. The majority of falls occurred in the home during the afternoon or evening. Less severe injuries such as bruises, scrapes, and cuts occurred most often followed by muscle/ligament strain or sprain. However, 18% of individuals with SCI who fell sustained a fracture as a result of a fall. Even though most injuries were minor, the ability to get out into the community and engage in productive activity after the fall was reportedly limited in almost one half of individuals (45%) who fell.
Although limited research exists on falls among ambulatory individuals with incomplete SCI, the incidence and consequences of falls have been studied extensively with older adults. In the United States, one third of community-dwelling older adults fall each year (9). Nearly one half of older adults who fall state they are afraid of falling, and one fourth of fallers restrict their physical and social activity because of this fear (10). Approximately 3% to 5% of older adults who fall sustain a fracture (11,12), and falls are the leading cause of injury deaths among adults 65 years of age and older (13). Although falls have not been associated with death, recent research indicates that those with SCI have a greater incidence of falls, more reported fractures caused by a fall, and greater restriction in community activities compared with older adults (8).
For healthy older adults and those with neurologic disease, physiologic changes and environmental hazards have been linked with falls (10,14–17). Commonly cited physiologic risk factors include problems with muscle activation (14–16), muscle weakness, gait and balance disturbances (10), visual impairment, cognitive decline, depression, functional decline, and adverse medication response (17). In addition, environmental hazards such as slippery or uneven walking surfaces, obstacles in the walking path, inadequate lighting, and loose carpets or rugs have been identified as a primary cause of imbalance in about one half of all falls (10). Although hazards in the environment create conditions likely to cause falls for any individual, they pose a particular danger to those who already have multiple risk factors for loss of balance.
To date, factors associated with falls among individuals with SCI have not been studied. Because of the increased incidence of falls and potentially serious consequences, a better understanding of the factors associated with falls among ambulatory individuals with incomplete SCI may assist health care professionals to identify individuals at risk and develop interventions to prevent injury. The purpose of this study was twofold: (a) to compare the demographic, SCI characteristics, health, and physical activity data for those with and without a history of falls over the previous year and (b) to identify potentially modifiable factors associated with falls among a community sample of ambulatory persons with incomplete SCI. This study is a direct follow-up to the previously discussed study of subsequent injuries by Krause (7) and uses a subsample of participants who were ambulatory.
METHODS
Participants
The sample was identified from outpatient files of a large free-standing specialty hospital in the southeastern United States. To participate in this study, subjects had to meet the following criteria: (a) a traumatic incomplete SCI; (b) ability to ambulate independently for a minimum of 10 m with or without an assistive device; (c) a minimum of 1-year post-SCI; and (d) 18 years of age or older at the time of the study. Two hundred eighty-one individuals from the initial participant pool (7) met the inclusion criteria, 60 of whom could not be located or were deceased, resulting in a working sample of 221.
Procedure
Prospective participants were sent a letter to explain the purpose of the study and to alert them that a questionnaire on falls and related injuries would be forthcoming. A cover letter, with all of the elements of informed consent, and a survey instrument were mailed 4 to 6 weeks later. Participants were asked to return the questionnaire within 2 weeks. Nonrespondents received a follow-up mailing approximately 4 weeks later. They were offered $20 remuneration as an incentive to complete the instrument. All procedures were approved by the Institutional Review Boards of the collaborating institutions.
Instrument
A questionnaire was developed to collect information on falls history over the previous year and factors potentially associated with falling for ambulatory individuals with incomplete SCI. For the purpose of this study, a fall was defined as an unplanned, unexpected contact with the supporting surface (18) and was provided for the participants on the questionnaire. The questionnaire included subsets of items from several measures and the addition of fall-related items. The use of subsets of several measures was necessitated by absence of appropriate existing measures as available instruments are performance based and include tests such as the Timed Up and Go (19), Berg Balance Scale (20), and Performance Oriented Mobility Assessment (21). Items were selected from the Falls Assessment Questionnaire (22) and the Behavioral Risk Factor Surveillance System (BRFSS) (23), a national survey aimed at gathering information on health behaviors of adults. Other items elicited information on demographics, SCI characteristics, and current health and activity.
The questionnaire was developed with the assistance of an expert from the Survey Research Unit of a southeastern medical university and feedback from experts in the field of physical therapy. It was pilot tested on a small sample of persons with SCI to determine whether questions were unclear, incomplete, or misleading and to solicit suggestions for any additional questions that should be included. Further revisions to the questionnaire were made based on feedback from this group. Closed-ended questions were used, which required the respondent to select from among several choices.
Data Analysis
Initially, t tests and χ2 tests were used to compare responders to nonresponders with regard to age, sex, race, marital status, years of education, and injury level. Unadjusted logistic regression models were used to determine whether demographic, SCI, and health data differed significantly between fallers and nonfallers. Unadjusted models were models that only compared a given variable between fallers and nonfallers without consideration of any mediating effects from other variables. With the exception of certain selected control variables (age, sex, race, education, living arrangements, and years since injury), the independent associations between falls and each of the subject characteristics were assessed using a series of multivariable logistic regression models. In each of these models, the dependent variable of interest was a dichotomous (yes/no) indicator of whether or not the subject had fallen in the past year, and the independent variable was the subject characteristic of interest. Characteristics that were ordinal in nature (ie, those such as perceived health with Likert-style responses) were entered into the models as categorical variables; however, the sample sizes within some of the categories were occasionally too small for proper comparisons. All models included the control variables mentioned above as additional explanatory variables. The significance level was set at P < 0.05 for all logistic regression modeling procedures, and results were reported in the form of unadjusted and adjusted odds ratios (ORs) with corresponding 95% confidence intervals (CIs). Finally, one additional multivariable model was created to examine factors independently associated with having had a fall. This model was developed using only the variables identified in the earlier multivariable models as having a statistically significant (P < 0.05) association with having had a fall.
All statistical analyses were performed using SAS software (SAS Institute, Cary, NC).
RESULTS
Subject Characteristics
Of 221 individuals invited to complete the questionnaire, 119 responded, for a response rate of 54%. Average age of the participants was 52.2 years. The majority of individuals were white (74%), most were men (69%), and more than one half were married (54%). The average number of years since the SCI was 13.6 years, and most participants sustained their injury in a motor vehicle crash (52%) or from a fall or flying object (28%). The sample included 89 (75%) subjects who had fallen in the past year and 30 (25%) who had not. When responders were compared with nonresponders, there were no significant differences by sex, race, marital status, years of education, or injury level. Compared to responders, nonre-sponders were significantly younger (44.3 vs 52.2 years; P < 0.01).
Differences Between Fallers and Nonfallers: Unadjusted and Multivariable-adjusted Comparisons
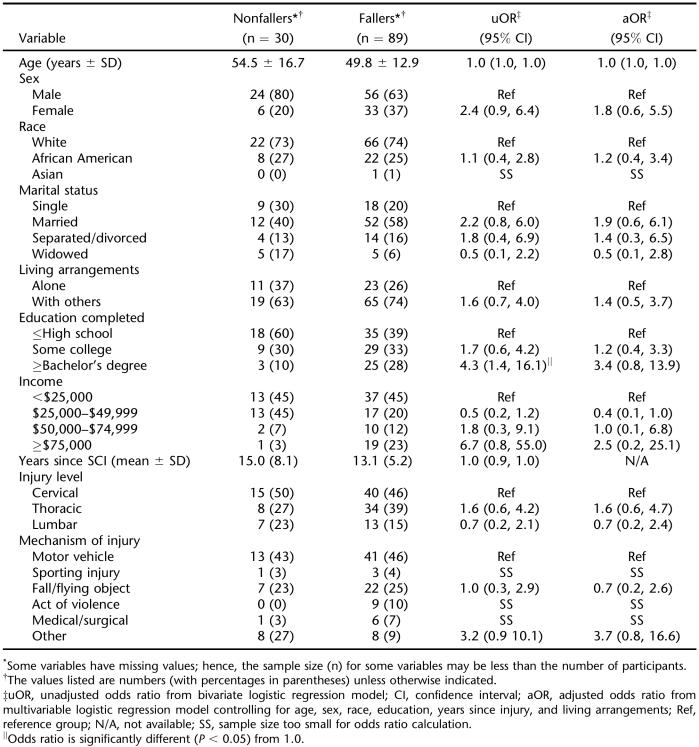
As shown in Table 1, unadjusted analyses suggested that few statistically significant differences in demographic and injury characteristics existed between fallers and nonfallers. Of the demographic variables, only level of education differed among the groups, with the odds of reporting a fall in the past year being significantly higher among those with a Bachelor's degree or higher than those with a high school education or less; however, this association was diminished slightly and no longer statistically significant in the multivariable model. No differences were found among the groups for injury characteristics in the unadjusted or multivariable-adjusted comparisons.
Table 1.
Demographic and Injury Characteristics: Unadjusted and Adjusted Comparisons
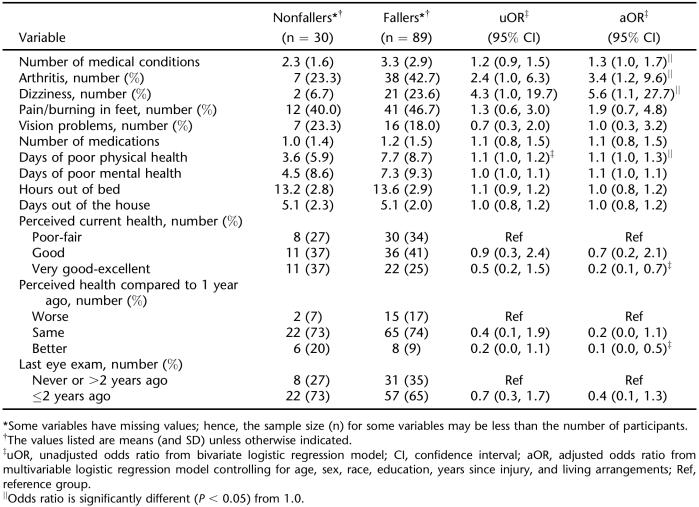
The data in Table 2 show that there were a number of significant differences in health data between fallers and nonfallers. In an unadjusted comparison, having fallen in the past year was significantly associated with more days of poor physical health; this finding remained significant even after multivariable adjustment. In addition, there were a number of characteristics that only became significant after multivariate adjustment. In the multivariable models, the odds of reporting a fall were significantly associated with greater numbers of medical conditions, having arthritis, experiencing dizziness, worse perceived current health, and worse perceived health compared to a year ago. None of the other variables in Table 2 were statistically significant in either the unadjusted or adjusted comparisons.
Table 2.
Health Data: Unadjusted and Adjusted Comparisons
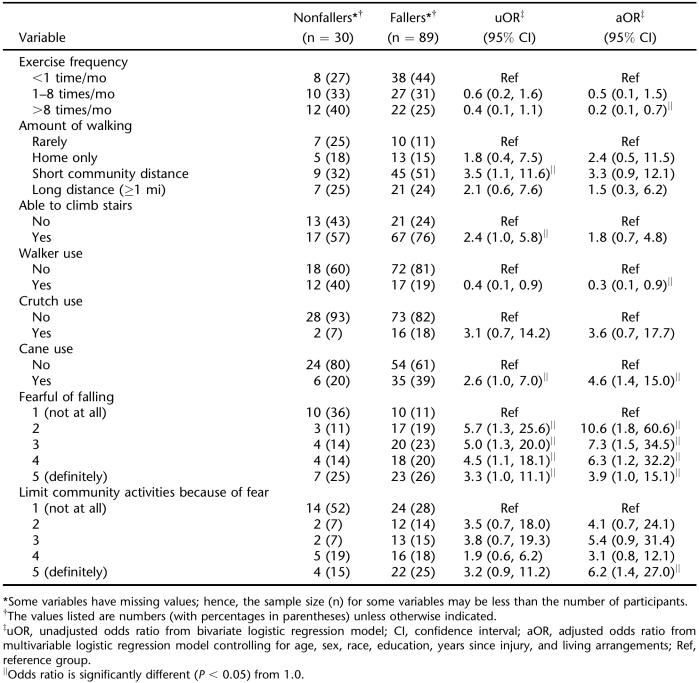
The unadjusted and adjusted comparisons of physical activity between fallers and nonfallers are presented in Table 3. In one of the unadjusted comparisons, subjects who routinely walked short distances within their communities were significantly more likely to have experienced a fall than subjects who rarely walked; however, this association did not achieve significance in the multivariable model. In another unadjusted comparison, the odds of reporting a fall were significantly higher among subjects reporting being able to climbs stairs than those who were not able. Again, this effect was diminished in the multivariable model.
Table 3.
Physical Activity Data: Unadjusted and Adjusted Comparisons
There were several significant findings in the multivariable models shown in Table 3, with the odds of falling being significantly associated with exercise frequency, walker use, cane use, being fearful of falling, and limiting participating in community activities because of a fear of falling, even after adjusting for the control variables. Subjects who reported exercising more than 8 times per month were less likely to have fallen than subjects who exercised less than once per month. Subjects who used a walker were less likely to have fallen than subjects who did not use a walker, but individuals who used a cane were more likely to have fallen than those who did not use a cane. Those who reported being fearful of falling were significantly more likely to have fallen than those who reported having no fear. Last, subjects who limited their participation in community activities because of a fear of falling exhibited greater odds of having fallen within the past year.
The final multivariable model that only included factors previously found to be significantly associated with having had a fall thus consisted of a logistic regression model with the following explanatory variables: number of medical conditions, arthritis, dizziness, perceived current health status, perceived health compared with 1 year ago, number of days in past month of poor physical health, exercise frequency, walker use, cane use, being fearful of falling, and limiting community activities because of a fear of falling. In this large multivariable model, there were only 2 variables that remained statistically significant. Respondents who exercised more than 8 times per month were much less likely to have had a fall compared with those who exercised less than once per month (OR = 0.15; 95% CI = 0.03–0.73). Additionally, respondents who used a walker were much less likely to have had a fall compared with those who did not use a walker (OR = 0.22; 95% CI = 0.06–0.85).
DISCUSSION
Ambulatory individuals with incomplete SCI have a higher incidence of falls and more significant consequences of falls compared with healthy older adults and those with disease. Seventy-five percent of those with incomplete SCI fell over the previous year, whereas healthy individuals 65 years of age and older had fall rates of approximately 30% (9,10,24). Older individuals with conditions such as peripheral neuropathy had fall rates of 50% (25), whereas those with Parkinson's disease had rates of 38% (26) and 62% (27). Moreover, fracture occurrence among persons with incomplete SCI (18%) (8) exceeded that reported in studies of healthy older adults (11,12). Declines in community and productive activities provide further evidence of the of the impact of falling for ambulatory individuals with incomplete SCI.
Differences in health were noted among the fallers and nonfallers in this study. Overall, those who had fallen seemed to have poorer health as evidenced by more medical conditions, more days of reported poor physical health, and worse perceived health compared to a year ago. The association between falls and poor physical health has also been found in studies of fall risk factors with healthy older adults (24) and individuals with diagnoses such as diabetes (28). Unlike older adults, use of a greater number of prescription medications (17,24) was not associated with falls in our sample. This finding may be attributed to the younger age of the participants in this study and use of fewer medications.
Two medical conditions found to be associated with falls for those with SCI were dizziness and arthritis. Both polyarthritis (29) and dizziness (17,30) are well-documented risk factors for falls among elderly persons. In a review of the epidemiology of falls, dizziness was reported as the cause of a fall in 13% of 3,628 reported falls among both community-dwelling and institutionalized elderly (17). Interventions for arthritis and dizziness may lead to control or elimination of symptoms, reduction in falls and related injuries, and improvement of overall health status.
Ambulatory individuals with SCI who exercised more frequently were found to have lower odds of having a fall. Exercise, particularly resistance training, has been linked to reduction in fall risk for healthy older adults (31,32). In addition to reducing fall risk, the 1996 Report of the Surgeon General states that regular physical activity is associated with reduced risk of developing diabetes, hypertension, and colon cancer and reduces the risk of dying from heart disease, helps control weight, and reduces feelings of depression and anxiety (33). Thus, implementation of an exercise program may lead to a reduced number of medical conditions, fewer days for poor physical health, and increased confidence in the ability to engage in community activities.
Other variables related to activity that were associated with falls in those with SCI were walker use, being fearful of falling, and limiting participation in community activities because of a fear of falling. More of the nonfallers used a walker, which is the most stable of all assistive devices for ambulation. The increased stability provided by a walker may account for the reduction in falls with these persons. The need for a device that provides greater stability may be evidenced by greater cane use among those who fell. A fear of falling and subsequent limitation in community activity has long been recognized as a risk factor for falls in older adults (34). Recent research indicates that a fear of falling continues to be associated with falls (35–37). Implementation of an exercise program and/or use of a walker may reduce the fear of falling and increase confidence in the ability to engage in community activities for ambulatory individuals with SCI.
In the final multivariable model, only exercise frequency and walker use were associated with having had a fall. Because of the small sample size, the analyses were not powered to be able to detect multiple significant independent effects. Although the ultimate and final multivariable model reduces to 2 statistically significant variables, this does not necessarily preclude the possibility of the other omitted variables being associated with falls. However, in models adjusting for age, sex, race, education, years since injury, and living arrangements, there are several variables with strong significant associations with falls, and of these, 2 variables (exercise frequency and walker use) seem to be significant even after adjusting for other possibly important subject characteristics.
There are several noteworthy limitations in this study. First, all data are self-report. Data from observance of actual behaviors or from diaries updated on a regular basis may have identified somewhat different results. Second, there was a relatively large percentage of nonresponders, which could affect the factors associated with falls. With only demographic and injury data available for comparison, no differences were found in sex, race, marital status, years of education, or injury level between responders and nonresponders. Compared to responders, nonresponders were significantly younger (44.3 vs 52.2 years; P < 0.01); however, age was not a significant risk factor for falls in this study. Based on the limited available data, the nonresponders seem to be similar to the responders and should be similar with regard to their risk factors for falls. Third, the analyses were not able to detect multiple significant independent effects because of the small sample size. The study's main strength was to highlight the variables that are most strongly associated with falls (with respect to magnitude, not necessarily with respect to statistical significance). Fourth, participants were selected from a specialty hospital rather than a population-based cohort. Nevertheless, the specialty hospital captures 85% of all SCI persons within that state where the facility is located, suggesting that the sample would not differ substantially from a population-based cohort. Last, because data are cross-sectional, and because the timing of certain factors was not fully elicited by the items in our questionnaire, the findings do not establish causation. For example, our analyses cannot distinguish whether a respondent's walker use contributed to him/her falling (ie, acting as a causative agent).
CONCLUSIONS
Given that ambulation is a highly coveted goal after SCI, rehabilitation professionals should consider including falls history, clinical measures of balance and gait, and assessment of factors associated with falls into the examination of these individuals to identify potential factors that may be associated with falls. Identification of risk and protective factors can guide the design of appropriate interventions that may be implemented to remediate deficits and potentially reduce the incidence of falls and subsequent injuries. Laboratory assessment of balance and gait may provide additional objective data that would allow an even better analysis of the factors associated with falls among individuals with incomplete SCI.
Footnotes
This project was supported by the South Carolina Spinal Cord Injury Research Fund Grant 0703.
REFERENCES
- Crozier K, Graziani V, Ditunno J, Herbison G. Spinal cord injury: prognosis for ambulation based on sensory examination in patients who are initially motor complete. Arch Phys Med Rehabil. 1991;72:119–121. [PubMed] [Google Scholar]
- Winter DA. The Biomechanics and Motor Control of Human Gait. Waterloo, Canada: University of Waterloo Press; 1987. [Google Scholar]
- Little JW, Burns SP, James JJ, Stiens SA. Neurologic recovery and neurologic decline after spinal cord injury. Top Spinal Cord Inj Med. 2000;11:73–89. [PubMed] [Google Scholar]
- Goldstein B. Musculoskeletal conditions after spinal cord injury. Top Spinal Cord Inj Rehabil. 2000;11:91–108. [PubMed] [Google Scholar]
- Bauman WA, Raza M, Spungen AM, Machac J. Cardiac stress testing with thallium-201 imagining reveals silent ischemia in individuals with paraplegia. Arch Phys Med Rehabil. 1994;75:946–950. [PubMed] [Google Scholar]
- Bauman WA, Spungen AM. Disorders of carbohydrate and lipid metabolism in veterans with paraplegia or quadriplegia: a model of premature aging. Metabolism. 1994;43:749–756. doi: 10.1016/0026-0495(94)90126-0. [DOI] [PubMed] [Google Scholar]
- Krause JS. Factors associated with risk for subsequent injuries after traumatic spinal cord injury. Arch Phys Med Rehabil. 2004;85:1503–1508. doi: 10.1016/j.apmr.2004.01.017. [DOI] [PubMed] [Google Scholar]
- Brotherton SS, Krause JS, Nietert PJ. Falls in individuals with incomplete spinal cord injury. Spinal Cord. 2007;45:37–40. doi: 10.1038/sj.sc.3101909. [DOI] [PubMed] [Google Scholar]
- Hausdorff JM, Rios DA, Edlber HK. Gait variability and fall risk in community dwelling older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–1056. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1706. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- Wilkins K. Health care consequences of falls for seniors. Health Rep. 1999;10:47–55. [PubMed] [Google Scholar]
- Murphy SL. Deaths: Final Data for 1998. Hyattsville, MD: National Center for Health Statistics, National Vital Statistics Reports; 2000. [PubMed] [Google Scholar]
- Horak FB, Shupert C, Mirka A. Components of postural dyscontrol in the elderly: a review. Neurobiol Aging. 1989;10:727–745. doi: 10.1016/0197-4580(89)90010-9. [DOI] [PubMed] [Google Scholar]
- Quoniam C, Hay L, Roll J, Harlay F. Age effects on reflex and postural responses to propriomuscular inputs generated by tendon vibration. J Gerontol A Biol Sci Med Sci. 1995;50:B155–B165. doi: 10.1093/gerona/50a.3.b155. [DOI] [PubMed] [Google Scholar]
- Woollacott MH, Shumway-Cook A, Nashner LM. Aging and postural control: changes in sensory organization and muscular coordination. Int J Aging Hum Dev. 1986;23:97–114. doi: 10.2190/VXN3-N3RT-54JB-X16X. [DOI] [PubMed] [Google Scholar]
- Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;182:141–158. doi: 10.1016/s0749-0690(02)00002-2. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Woollacott MH. Control of posture and balance. In: Shumway-Cook A, Woollacott MH, editors. Motor Control: Theory and Practical Applications. 2nd ed. Baltimore, MD: Williams and Wilkins; 2000. pp. 222–247. [Google Scholar]
- Podsiadlo D, Richardson S. The timed ''up and go'': a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Berg KO, Wood-Dauphinee SL, Williams JT, Gayton D. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304–311. [Google Scholar]
- Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34:119–126. doi: 10.1111/j.1532-5415.1986.tb05480.x. [DOI] [PubMed] [Google Scholar]
- Rapport LJ, Webster JS, Flemming KL, et al. Predictors of falls among right hemisphere stroke patients in the rehabilitation setting. Arch Phys Med Rehabil. 1993;74:621–626. doi: 10.1016/0003-9993(93)90160-c. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Overview Behavioral Risk Factor Surveillance System (BRFSS): 2002. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2003. [Google Scholar]
- Gill T, Taylor AW, Pengelly A. A population-based survey of factors relating to the prevalence of falls in older people. Gerontology. 2005;51:340–345. doi: 10.1159/000086372. [DOI] [PubMed] [Google Scholar]
- Richardson JK, Hurvitz EA. Peripheral neuropathy: a true risk factor for falls. J Gerontol A Biol Sci Med Sci. 1995;50:M211–M215. doi: 10.1093/gerona/50a.4.m211. [DOI] [PubMed] [Google Scholar]
- Stack E, Ashburn A. Fall events described by people with Parkinson's disease: implications for clinical interviewing and research agenda. Physiother Res Int. 1999;4:190–200. doi: 10.1002/pri.165. [DOI] [PubMed] [Google Scholar]
- Hirsh MA, Toole T, Maitland CG, Rider RA. The effects of balance training and high-intensity resistance training on persons with idiopathic Parkinson's disease. Arch Phys Med Rehabil. 2003;84:1109–1117. doi: 10.1016/s0003-9993(03)00046-7. [DOI] [PubMed] [Google Scholar]
- Quandt SA, Stafford JM, Bell RA, Smith SL, Snively BM, Arcury TA. Predictors of falls in a multiethnic population of older rural adults with diabetes. J Gerontol A Biol Sci Med Sci. 2006;61:M394–M398. doi: 10.1093/gerona/61.4.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oswald AE, Pye SR, O'Neill TW, et al. Prevalence and associated factors for falls in women with established polyarthritis. J Rheumatol. 2006;33:690–694. [PubMed] [Google Scholar]
- Graafmans WC, Ooms ME, Hofstee HMA, Bezemer PD, Bouter LM, Lips P. Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol. 1996;143:1129–1136. doi: 10.1093/oxfordjournals.aje.a008690. [DOI] [PubMed] [Google Scholar]
- Liu-Ambrose T, Khan KM, Eng JJ, Janssen PA, Lord SR, McKay HA. Resistance and agility training reduce fall risk in women aged 75 to 85 with low bone mass: a 6-month randomized, controlled trial. J Am Geriatr Soc. 2004;52:657–665. doi: 10.1111/j.1532-5415.2004.52200.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord SR, Tiedmann A, Chapman K, Munro B, Murray SM, Sherrington C. The effect of an individualized fall prevention program on fall risk and falls in older people: a randomized controlled trial. J Am Geriatr Soc. 2005;53:1296–1304. doi: 10.1111/j.1532-5415.2005.53425.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Physical Activity and Health: a Report of the Surgeon General. Available at: http//www.cdc.gov/nccdphp/sgr/ataglan.htm. Accessed March 16, 2006.
- Maki BE, Holliday PJ, Topper AK. Fear of falling and postural performance in the elderly. J Gerontol A Biol Sci Med Sci. 1991;46:M123–M131. doi: 10.1093/geronj/46.4.m123. [DOI] [PubMed] [Google Scholar]
- Belgen B, Beninato M, Sullivan PE, Narielwalla K. The association of balance capacity and falls self-efficacy with history of falling in community dwelling people with chronic stroke. Arch Phys Med Rehabil. 2006;87:554–561. doi: 10.1016/j.apmr.2005.12.027. [DOI] [PubMed] [Google Scholar]
- Ozcan A, Donat H, Gelecek N, Ozdirenc M, Karadibak D. The relationship between risk factors for falling and the quality of life in older adults. BMC Public Health. 2005;90:1–6. doi: 10.1186/1471-2458-5-90. Available at: http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=1208910&blobtype=pdf. Accessed January 2, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold CM, Busch AJ, Schachter CL, Harrison L, Olszynski W. The relationship of intrinsic fall risk factors to a recent history of falling in older women with osteoporosis. J Orthop Sports Phys Ther. 2005;35:452–460. doi: 10.2519/jospt.2005.35.7.452. [DOI] [PubMed] [Google Scholar]