Abstract
Background/Objective:
Upper-extremity reconstruction for people with tetraplegia is underused, and we felt that physicians' beliefs could be contributing to this phenomenon. This research sought to determine whether (a) physicians underestimate the importance of upper-extremity function for people with tetraplegia, (b) physiatrists and hand surgeons disagree on the quality of life of those with tetraplegia, (c) surgeons believe that social issues make people with tetraplegia poor surgical candidates, and (d) the 2 specialties disagree on the benefits of upper-extremity reconstruction.
Methods:
A self-administered questionnaire was mailed to a national sample of 384 physiatrists and 379 hand surgeons. The data were analyzed with bivariate statistics.
Results:
The response rate was 62%. 65% of surgeons and 49% of physiatrists (P < 0.001) ranked upper-extremity function as the most important rehabilitative goal for people with tetraplegia. Both specialties believed the quality of life with tetraplegia was low (less than 60 on a scale of 0 to 100, with 100 representing perfect health). The 2 specialties have significantly different opinions regarding patient compliance, social support, and the effectiveness of surgery.
Conclusions:
The majority of physicians believe that upper-extremity function is a rehabilitative priority for people with tetraplegia. However, physiatrists and hand surgeons have significantly different views about people with tetraplegia and the benefits of reconstructive surgery. Physician preconceptions and interdisciplinary divergence may be contributing to the underuse of these procedures, and these issues should be considered when designing programs to improve access to these procedures.
Keywords: Outcome assessment (healthcare), Health care surveys, Tetraplegia, Upper extremity reconstruction, Physiatry, Hand surgery, Attitude of health personnel
INTRODUCTION
Approximately 100,000 Americans live with tetraplegia, and many of these people struggle through long and complicated rehabilitations (1). They look to their doctors for guidance in achieving their primary goal of improved independence. But are physicians knowledgeable enough about their patients' needs and desires to serve as guides? This question is relevant, because there appears to be a discrepancy between what people with tetraplegia want and what they are receiving. In the 1970s Hanson and Franklin found that upper-extremity function was the most important physical priority for people with tetraplegia (2). A qualitative study by Manns and Chad also found that upper-extremity function was paramount, which is demonstrated by a quote from a participant in that study: “I've often thought how much easier things would be, even if I were a para. Even if I had use of my hands … How useful they are, they're great, everyone should have working hands” (3). However, surgeries that enhance the use of the upper limbs in tetraplegia are profoundly underused; we found that fewer than 10% of people with tetraplegia receive these operations (4).
Physicians are critical to the receipt of health care; thus, to better understand the underuse of upper-extremity reconstruction in tetraplegia, we focused on the relevant physicians: physiatrists and hand surgeons. Our initial work showed that at a health care system level, good interdisciplinary relationships between hand surgeons and physiatrists are critical to appropriate upper-limb reconstruction (5). Next, we wanted to look in more detail at the individual providers. We speculated to what extent physician perceptions might be affecting the decision-making process in regard to upper-extremity reconstruction. Therefore, this project's goal was to explore physician attitudes (physiatrists and surgeons) toward upper-limb reconstructive procedures for people with tetraplegia. We asked the following research questions: (a) Do physicians recognize the importance of upper-extremity function for the person with tetraplegia? (b) Do physiatrists and hand surgeons have disparate views on the quality of life with tetraplegia and the gain in quality of life after upper-extremity reconstruction? (c) Do hand surgeons, who are less familiar with this population than the physiatrists, believe that people with tetraplegia have social issues that make them poor surgical candidates? and (d) Do these specialties disagree on the effectiveness and benefits of upper-extremity reconstruction?
The policy implication of this project is to better understand the reasons behind the current underuse of upper-limb surgery for people with tetraplegia. Recognizing and understanding provider beliefs can help policy makers plan national strategies to promote better care for this population.
METHODS
Participants
This study analyzed the results of a national mailed survey that focused on physicians' attitudes and beliefs toward people with tetraplegia and the reconstruction of their upper extremities. This survey was mailed to physiatrists with an interest in spinal cord medicine and to hand surgeons. The physiatrists were either members of the American Spinal Injury Association or the American Paraplegia Society or they were spinal cord specialists practicing in Model Spinal Cord Injury Systems. The Model Systems are clinical centers sponsored by the National Institute on Disability and Rehabilitative Research; these centers focus on improving care for people with spinal cord injury and promoting collaborative research. Using these sources, we found 384 physiatrists who could be contacted for this survey. We also surveyed hand surgeons, who were identified from the full member list of the American Society for Surgery of the Hand. We took a random sample, using a random number generator, to select 379 hand surgeons from the member list; this represented approximately 30% of the membership.
Survey Design
We designed the survey after discussions with physiatrists and hand surgeons regarding their opinions and attitudes toward upper-limb reconstruction for tetraplegia. After these discussions, several research questions were generated on how physician attitudes may differ between the specialties and what beliefs may affect clinical decision making for upper-extremity reconstruction. The majority of the questions were designed using a 5-point Likert scale ranging from “strongly disagree” (score = 1) to “strongly agree” (score = 5). The assessment of surgical candidacy included an analysis of the social factors that may impact treatment success, such as compliance issues, social support, and insurance availability. To assess the perceived quality of life of people with tetraplegia, we used a range of 0 to 100, with 0 = death and 100 = perfect health. This type of rating scale is a simple method of assessing the value of a particular health state (6).
The survey was pilot tested with local physicians using concurrent think-aloud protocols (7). A think-aloud protocol consists of observing subjects taking the survey while encouraging them to state out loud what they believe each question means. The survey took approximately 10 minutes to finish and was formatted to standard survey design (8). The survey used a mailed self-administered instrument. The surveys were coded to identify who had responded to the survey (to allow for follow-up mailings), but completed surveys were blinded after receipt, thereby rendering the final data set anonymous. Because these data were anonymous and were of a nonsensitive nature, formal written informed consent was waived. Data collection occurred from June through October 2003, after approval by the University of Michigan Institutional Review Board.
Data Analysis
Bivariate analysis included the chi-square test for comparisons of proportions and Student's t test for comparisons of means. To analyze the Likert scale responses, we used the Wilcoxon rank sum test. For clarity in data presentation, data were dichotomized as positive attitudes (“strongly agree” or “agree”) vs neutral/negative attitudes (“neutral,” “disagree,” and “strongly disagree”). All analyses were performed using statistical software (Stata 9.0; Statacorp, College Station, TX).
RESULTS
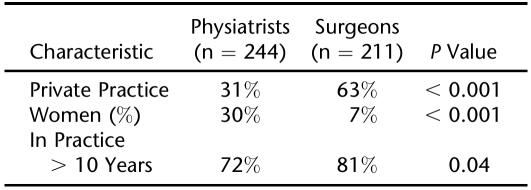
Surveys were sent to 763 physicians; 25 surveys were undeliverable because the subjects had wrong addresses, had retired, or were engaged in military duty. We received a total of 455 completed surveys (62% of the eligible subjects). There was no significant difference in gender or geographic location between the responders and nonresponders (gender and geographic location were the only data available on the nonresponders). Respondents' demographic characteristics are shown in Table 1. The demographics of the 2 physician groups reflected the characteristics of these very different specialties. For example, physiatrists were less likely to be in private practice (P < 0.001), which is consistent with spinal cord rehabilitation programs' frequent residence in tertiary care centers.
Table 1.
Characteristics of a National Sample of Hand Surgeons and Physiatrists
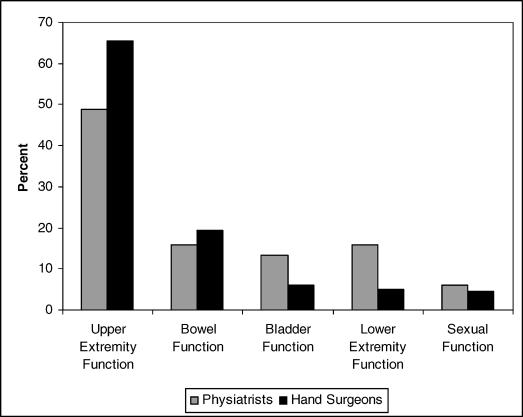
Our first question addressed whether physicians recognized the importance of upper-extremity function for persons with tetraplegia. To assess this question, we asked the physicians how they believed people with tetraplegia would prioritize the reconstruction of different lost physical functions; the results are shown in Figure 1. This figure displays several physical functions and the percentage of physicians who ranked each function as the top priority for people with tetraplegia. Overall, 57% of the physicians ranked improving upper-extremity function as the most important priority for people with tetraplegia. However, we found significant differences between the 2 specialties on this question, with far fewer physiatrists believing that upper-extremity function was the most important reconstructive priority, that is, 49% of physiatrists vs 65% of hand surgeons (P = 0.001).
Figure 1. Relative percentage of physiatrists and hand surgeons who rated different physical functions as the top reconstructive priority for people with tetraplegia.
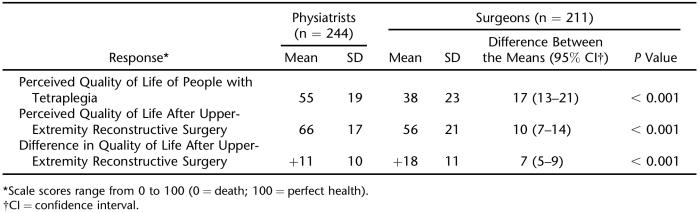
The second portion of the survey determined whether physiatrists and hand surgeons had disparate views on both patient quality of life with tetraplegia and the difference in quality of life after upper-extremity reconstruction. We approached this topic by asking 2 questions. First, we asked how the physicians within each specialty viewed the quality of life of people with tetraplegia; second we asked how much the quality of life would improve with upper-extremity reconstruction. Physicians were asked to estimate the baseline quality of life of a person with tetraplegia as well as the quality of life after upper-extremity reconstructive surgery. Scores were reported on a scale of 0 to 100, with 0 representing death and 100 perfect health. The results (Table 2) showed that these 2 specialties had sharp differences in their beliefs about both the impact of tetraplegia on quality of life and the benefits of upper-extremity surgery. Physiatrists rated the quality of life of people with tetraplegia as significantly higher than surgeons (55 vs 38, P < 0.001). In addition, the surgeons believed there was a greater increase in postsurgical quality of life after upper-extremity reconstruction in comparison to the physiatrists, an increase of 18 vs 11 quality-of-life points (P < 0.001). These results again demonstrate the disparate positions of these 2 specialties.
Table 2.
Physician Perceptions of Quality of Life for People With Tetraplegia Before and After Surgery
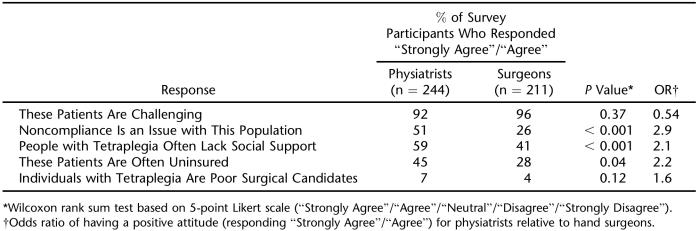
The third question was: do hand surgeons, who are less familiar with this population than the physiatrists, believe that people with tetraplegia have social issues that make them poor surgical candidates? To address this question, we examined the physicians' perceptions of people with tetraplegia, focusing upon issues of social support, insurance concerns, and general compliance (Table 3). Interestingly, compared to the hand surgeons, the physiatrists felt that this population was more likely to be noncompliant, uninsured, and lacking social support. The greatest differences between the specialists involved the perception of noncompliance, as physiatrists were 2.9 times more likely to respond that these patients were noncompliant. Large percentages of both specialties agreed with the statement that “these patients are challenging” (92% of physiatrists and 96% of surgeons) and disagreed with the statement that “individuals with tetraplegia are poor surgical candidates” (only 7% of physiatrists and 4% of surgeons agreed). These findings suggest that the physiatrists (not the surgeons) were more likely to have concerns about social issues that could negatively impact surgical candidacy.
Table 3.
Physician Beliefs About Patients With Tetraplegia
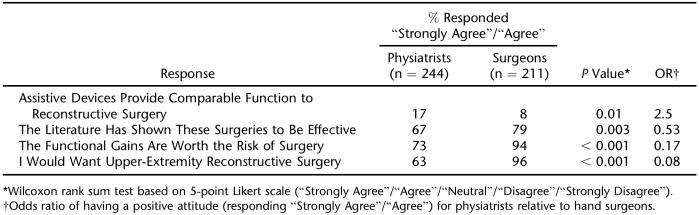
Finally, we explored possible differences that these 2 specialties may have on the perceived effectiveness and benefits of upper extremity reconstruction. Table 4 compares the specialties' attitudes and beliefs regarding assistive devices and upper-extremity reconstructive surgery. A majority of both physiatrists and hand surgeons surveyed believe that the literature has shown upper-extremity reconstructive procedures to be effective (67% vs 79%, P = 0.003). The greatest difference in the perceived effectiveness of the surgical procedures between the specialists could be seen by the desire of physicians to have these procedures if they themselves ever suffered a cervical spinal cord injury. Surgeons were 12.5 times more likely to say that they would want this procedure for themselves when compared to the physiatrists. Overall, the data showed general agreement between these specialties that the procedures are effective.
Table 4.
Physician Opinions on the Effectiveness of Treatments for Persons With Tetraplegia
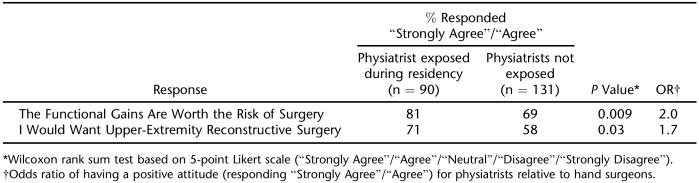
We also wanted to evaluate the effect on exposure to the other specialty during residency on these views (Table 5). Physiatrists who had been exposed to upper-extremity reconstruction during residency were more likely to believe that the functional gains from these procedures were worth the risks of surgery (81% vs 69%, P = 0.009). Furthermore, physiatrists who had been exposed to these surgical procedures during residency were more likely to want these procedures for themselves if they ever suffered a cervical spinal cord injury (71% vs 58%, P = 0.03).
Table 5.
Effects of Interdisciplinary Exposure on Physician Opinion
DISCUSSION
Physicians help construct patient treatment plans, but physicians' preconceptions about their patients may lead to imperfect or inappropriate recommendations. This study examined the perceptions of physicians within 2 different medical specialties of people with tetraplegia and upper-extremity reconstructive procedures. We chose to focus on this issue because there is an apparent discrepancy between what patients desire and how many patients receive these treatments. Studies suggest that upper-extremity function is a high priority for people with tetraplegia (2,3). However, there appears to be profound underuse of procedures to enhance upper-extremity function in this population. There are roughly 5,000 new cervical spinal cord injuries a year, and fewer than 10% of these people receive upper-extremity reconstruction (1,4). Even the most stringent surgical eligibility criteria would likely recommend that more than 10% of people with tetraplegia should receive upper-extremity reconstruction. To begin to understand this phenomenon, we felt it was important to better understand physicians' preconceptions about this population. We focused on hand surgeons and physiatrists because both specialties play an important role in the delivery of upper-extremity reconstruction. In addition, we wanted to understand the views of these 2 specialties, as disparate views may inhibit smooth interdisciplinary communication. Ultimately, we hope that better understanding of provider beliefs will help promote better access to care.
The first question we examined was how well physicians understood the rehabilitative goals of this patient population. Although patient perspectives in the literature are underrepresented, there are 2 small studies that suggest that people with tetraplegia would be most interested in improved upper-extremity function (2,3). Earlier literature had mentioned that providers may not know the goals of these patients and may overestimate the importance of other lost physical abilities, such as sexual function (2). Differences in the perceptions of physicians and patients have the potential to interfere with effective treatment (9). If physicians believe that other functions are of higher priority, upper-extremity restoration could take a back seat. Our study found that both physiatrists and hand surgeons have a clear understanding of the value of upper-extremity function for people with tetraplegia. Although there was some difference between the specialties, the largest percentage in both specialties ranked improvement of upper-extremity function as the most important rehabilitation goal. This finding shows that physicians do understand the rehabilitative priorities of people with tetraplegia.
We next looked at how physicians imagine life with tetraplegia. We know that able-bodied people have difficulty perceiving life with chronic illness, often greatly underestimating the quality of life of those with illnesses. For example, in one study, the general public estimated the health-related quality of life (HRQoL) of people on dialysis at a value of 0.39 (on a scale where 0 indicates conditions as bad as death and 1 indicates perfect health), whereas dialysis patients estimated their HRQoL at 0.56 (10). Across a wide range of health conditions, patients typically report greater happiness and quality of life than healthy people imagine if they were to experience similar circumstances (11). This type of misconception has been referred to as the disability paradox (12). We hypothesized that these misconceptions might also be present in the providers of care for patients with spinal cord injury and that these perceptions would differ between physiatrists and hand surgeons. We are concerned that underestimating a person's quality of life can have an impact on how aggressively one would pursue medical treatment, including upper-extremity reconstruction for people with tetraplegia (13). We found that both specialties ranked quality of life with tetraplegia low, with a mean score of 38 (standard deviation of 23) for surgeons and 55 (standard deviation of 19) for physiatrists on a 0-to-100 scale. It was not surprising that the surgeons, who were less familiar with people with spinal cord injury, would rank the quality of life lower. This result is consistent with a phenomenon known as the focusing illusion, which occurs when people unfamiliar with a scenario overvalue the perceived differences and discount the things that will stay the same (14). For example, students from California and the Midwest both believe that people in California have higher levels of happiness, but in reality, people in both locations have the same level of happiness. The students overestimate the impact of the weather on happiness and underrate things that are unchanged, such as jobs and relationships (15). Our study suggests that physiatrists' frequent contact and familiarity with patients with spinal cord injury prevent them from having their views distorted by the focusing illusion. We believe that highlighting these different perspectives between these specialties can improve the dialogue between physiatrists and surgeons. In addition, physiatrists can help dispel the focusing illusion of their surgical colleagues.
Medical decision making is a complex process. Before recommending surgery, physicians should consider factors that may affect success, such as social support and patient compliance. For example, a patient with no social support may not be able to complete the required rehabilitation following these procedures. After our discussions with surgeons, we wondered whether surgeons, who are less familiar with this population, would be more likely to believe that people with tetraplegia have issues that limit their ability to cope with surgery. We found quite the opposite: physiatrists perceived more issues with noncompliance and lack of social support than surgeons. These surprising findings suggest that closer contact with this population promotes an awareness of the difficulties that these patients face. Indeed, the physiatrists, who act as gatekeepers, likely limit surgical referrals to patients with adequate social support. This might cause surgeons to underestimate the difficulties faced by people with spinal cord injury. Nevertheless, physiatrists should be cautious that their concerns do not exert undue influence, such that the rehabilitation of the upper extremities only includes less aggressive measures such as assistive devices. It is important that physiatrists be cognizant of the social concerns of their patients and still be able to recommend more aggressive care for appropriate patients.
We also explored physicians' attitudes toward these procedures. We found that the majority of providers would want this intervention for themselves, which is an excellent indicator of perceived benefit. Although both specialties judged reconstructive surgery as valuable, physiatrists' ratings of the effectiveness of these procedures were significantly lower than those of surgeons. This divergence of opinions between specialties is not unique to hand surgeons and physiatrists (16–18). Family physicians and rheumatologists, for example, showed substantial differences on the indications for referring patients with osteoarthritis for knee replacement (19). Urologists and radiation oncologists were also shown to have markedly divergent attitudes regarding the most effective treatment for prostate cancer (20). The establishment of multiple-specialty panels has been recommended to disseminate and clarify appropriate treatment guidelines to physicians when such disagreements arise, and these panels have been shown to blunt subspecialty treatment biases (21). This type of panel would be helpful not only in minimizing the differences in clinical management of the upper extremities; it might also centralize these specialties' disparate perceptions about tetraplegia and upper-extremity reconstruction.
Finally, we looked for an exposure effect on physician attitudes. We hypothesized that physiatrists exposed to recent technologic advances during training may have more favorable attitudes toward reconstructive procedures. Interspecialty exposure has not always been found to reduce differences of opinion. For example, a study of rheumatologists' opinions on the effectiveness of rheumatoid hand surgery found that exposure to hand surgery, either currently or during their training, was not associated with positive attitudes toward rheumatoid hand surgery (22). We found that, in the case of upper-extremity reconstructive surgery, interspecialty exposure does affect physician attitudes. Physiatrists who had been exposed to upper-extremity reconstructive surgery during their residency rated the effectiveness of upper-extremity reconstructive procedures higher than their colleagues who did not have such exposure. Other specialty groups experiencing similar difference of opinions have recommended increasing interspecialty exposure during the medical education process (20). We believe this would also be beneficial for those involved with the care of those with tetraplegia.
This survey research has limitations. Self-reported attitudes of physiatrists and hand surgeons may not translate into actual practice patterns. Most important, we do not have sufficient information from the literature outlining the desires of people with tetraplegia. For now, we must rely on qualitative work and small studies available in the literature to gauge patient preferences (2,3).
CONCLUSION
We believe that physician preconceptions have an impact on clinical decision-making. To change the standard of practice, it is imperative to better understand physician beliefs and recognize the different perspectives across specialties. This study found that many physicians understand the importance of upper-extremity function for people with tetraplegia. However, there is a significant divergence of opinions between these specialties on the benefits of surgery. Therefore, to meet our goal of improving utilization of upper-extremity reconstruction, we believe that physicians should first be made aware of the goals of people with tetraplegia. Second, these 2 specialties have disparate views, and we believe that increasing interdisciplinary exposure and multidisciplinary panels would improve communication and minimize divergence. Finally, we believe that better education about these procedures could empower patients to help direct their providers to the best care for them.
Footnotes
This study was supported by the Robert Wood Johnson Foundation and the Department of Veterans Affairs.
REFERENCES
- Go BK, DeVivo MJ, Richards JS. The epidemiology of spinal cord injury. In: Stover SL, DeLisa JA, Whiteneck GG, editors. Spinal Cord Injury Clinical Outcomes From the Model Systems. Gaithersburg, MD: Aspen Publishers; 1995. pp. 21–55. [Google Scholar]
- Hanson RW, Franklin MR. Sexual loss in relation to other functional losses for spinal cord injured males. Arch Phys Med Rehabil. 1976;57:291–293. [PubMed] [Google Scholar]
- Manns PJ, Chad KE. Components of quality of life for persons with a quadriplegic and paraplegic spinal cord injury. Qual Health Res. 2001;11:795–811. doi: 10.1177/104973201129119541. [DOI] [PubMed] [Google Scholar]
- Curtin CM, Gater DR, Chung KC. Upper extremity reconstruction in the tetraplegic population, a national epidemiological study. J Hand Surg. 2005;30A:94–99. doi: 10.1016/j.jhsa.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Curtin CM, Hayward RA, Kim M, Gater DR, Chung KC. Physician perceptions of upper extremity reconstruction for the person with tetraplegia. J Hand Surg. 2005;30A:87–93. doi: 10.1016/j.jhsa.2004.08.014. [DOI] [PubMed] [Google Scholar]
- Hunik M, Glasziou P, Siegel J, et al. Valuing outcomes. In: Hunik M, Glasziou P, editors. Decision Making in Health and Medicine, Integrating Evidence and Values. Cambridge, UK: Cambridge University Press; 2003. pp. 88–127. [Google Scholar]
- Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2nd ed. New York: Wiley; 2000. pp. 142–193. [Google Scholar]
- Fink A. How to design survey studies. In: Fink A, editor. The Survey Kit. 2nd ed. Vol. 60. London: Sage; 1995. pp. 97–105. [Google Scholar]
- Cleeland CS, Gonin R, Hatfield AK, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330:592–596. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- Sackett DL, Torrance GW. The utility of different health states as perceived by the general public. J Chronic Dis. 1978;31:697–704. doi: 10.1016/0021-9681(78)90072-3. [DOI] [PubMed] [Google Scholar]
- Ashby J, O'Hanlon M, Buxton MJ. The time trade-off technique: how do the valuations of breast cancer patients compare to those of other groups/ Quality Life Res. 1994;3:257–265. doi: 10.1007/BF00434899. [DOI] [PubMed] [Google Scholar]
- Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med. 1999;48:977–988. doi: 10.1016/s0277-9536(98)00411-0. [DOI] [PubMed] [Google Scholar]
- Nantais D, Kuczewski M. Quality of life: the contested rhetoric of resource allocation and end-of-life decision making. J Med Philos. 2004;29:651–664. doi: 10.1080/03605310490883000. [DOI] [PubMed] [Google Scholar]
- Ubel PA, Loewenstein G, Schwarz N, Smith D. Misimagining the unimaginable: the disability paradox and healthcare decision making. Health Psychol. 2005;24:S57–S62. doi: 10.1037/0278-6133.24.4.S57. [DOI] [PubMed] [Google Scholar]
- Schkade DA, Kahneman D. Does living in California make people happy/A focusing illusion in judgments of life satisfaction. Psychol Sci. 1998;9:340–346. [Google Scholar]
- Kahan JP, Park RE, Leape LL, et al. Variations by specialty in physician ratings of the appropriateness and necessity of indications for procedures. Med Care. 1996;34:512–523. doi: 10.1097/00005650-199606000-00002. [DOI] [PubMed] [Google Scholar]
- Huetson WJ, Applegate JA, Mansfield CJ, King DE, McClaflin RR. Practice variations between family physicians and obstetricians in the management of low-risk pregnancies. J Fam Pract. 1995;40:345–351. [PubMed] [Google Scholar]
- Rigter H, Meijler AP, McDonnell J, Scholma JK, Bernstein SJ. Indications for coronary revascularization: a Dutch perspective. Heart. 1997;77:211–218. doi: 10.1136/hrt.77.3.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyte PC, Hawker G, Croxford R, Attard C, Wright JG. Variation in rheumatologists' and family physicians' perceptions of the indications for and outcomes of knee replacement surgery. J Rheumatol. 1996;23:730–738. [PubMed] [Google Scholar]
- Fowler FJ, Jr, McNaughton CM, Albertsen PC, Zietman A, Elliott DB, Barry MJ. Comparison of recommendations by urologists and radiation oncologists for treatment of clinically localized prostate cancer. JAMA. 2000;283:3217–3222. doi: 10.1001/jama.283.24.3217. [DOI] [PubMed] [Google Scholar]
- McDonnell J, Meijler AP, Kahan JP, Rigter H, Bernstein SJ. Effect of physician specialty on treatment recommendation to patients with coronary artery disease. Int J Technol Assess Health Care. 2000;16:190–198. doi: 10.1017/s0266462300161161. [DOI] [PubMed] [Google Scholar]
- Alderman AK, Chung KC, Kim HM, Fox DA, Ubel PA. Effectiveness of rheumatoid hand surgery: contrasting perceptions of hand surgeons and rheumatologists. J Hand Surg. 2003;28:3–11. doi: 10.1053/jhsu.2003.50034. [DOI] [PubMed] [Google Scholar]