Abstract
Background/Objective:
Spinal hydatid cyst is a serious form of hydatid disease affecting less than 1% of the total cases of hydatid disease. We present a case of pathologically confirmed primary intradural spinal cyst hydatid in an otherwise healthy patient who showed no other evidence of systemic hydatid cyst disease.
Case Report:
An 8-year-old boy presented with back pain, left leg pain, and difficulty in walking. The patient had no other signs of systemic hydatid cyst disease. An intradural extramedullary cystic lesion was identified with magnetic resonance imaging and was shown to be a hydatid cyst by histopathologic examination after the surgical removal.
Conclusion:
Although extremely rare, primary intradural extramedullary hydatid cyst pathology might be the cause of leg pain and gait disturbance in children living in endemic areas.
Keywords: Myelopathy, infectious; Hydatid disease, spinal, intradural, extramedullary; Echinococcus granulosus; Child
INTRODUCTION
Cases of cystic hydatid disease are mostly found in areas where dogs and livestock coexist. Adult worms mature in the intestine of the dog, wolf, and other carnivorous animals (definitive host), and the eggs are released in the feces. Intermediate hosts such as sheep and cattle ingest the eggs. Humans contract the disease by means of contamination through the direct contact with the definitive host or its feces or by ingesting food infected with parasite eggs; oncospheres hatch in the duodenum, which penetrate the intestine and are carried through the bloodstream to various organs (1).
The metacestode cyst develops over a course of years in the patient. Hydatid cysts are formed in the organs such as liver (60–70%), lungs, and brain. Spinal hydatid cysts account for 1% of all cases of hydatid disease (2–4). Primary spinal intradural extramedullary hydatid cysts are extremely rare (5–7). Disease usually spreads over the spine by the direct extension from pulmonary, abdominal, or pelvic infestation and most commonly affects the dorsal region of the spine (7–9). To our knowledge, this is the first pediatric case among the 25 cases of primary intradural extramedullary hydatid cyst reported in the literature.
CASE REPORT
An 8-year-old boy was admitted to our department with pains in the back and left leg and disability in walking. He had back pain for a month and complained about difficulty in walking and left leg pain for a week. His physical examination was normal. However, neurologic examination revealed left leg monoparesis that was most prominent proximally.
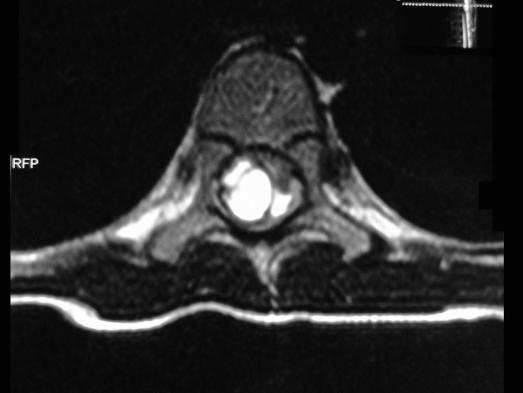
X-ray examinations of the chest and spine revealed no abnormalities. Abdominal ultrasonography scans and magnetic resonance images (MRIs) of the lumbar region were normal. MRIs of the thoracic region showed a lobulated 3 × 1-cm cystic lesion with a regular contour. The cyst was located in intradural extramedullary at the T7–T8 level. The lesion was hypointense on T1- and hyperintense on T2-weighted MRIs. With intravenous gadolinium injection, there was no contrast enhancement on T1-weighted images. The lesion was compressed mediolaterally to the dural sac, especially at right side at the T7–T8 level (Figures 1–3). Initially, the lesion was regarded as a hydatid cyst. A hydatid cyst hemagglutination test was positive (1/80).
Figure 1. Sagittal contrast-enhanced T1-weighted MRI shows there is no contrast enhancement and cord is compressed anteriorly.
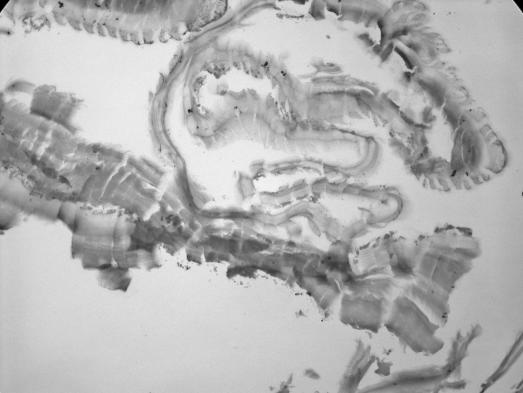
The patient underwent T7–T8–T9 laminotomy. An intradural extramedullary cystic lesion was removed totally with its capsule, and the cavity was irrigated with hypertonic saline. Histopathologic examination revealed a hydatid cyst (Figure 4). Albendazole treatment was started in the early postoperative stage. The postoperative stage was uneventful, and the patient has had no other additional problems. The patient was discharged on the seventh postoperative day. On his last neurologic examination, left leg monoparesis was improved, and eventually his back pain, left leg pain, and difficulty in walking were improved. The neurologic examination at the eighth month was normal, and pain symptoms resolved completely. Neurologic examination was normal at the 12th month postoperatively. However, follow-up MRIs showed a small relapse of the cystic lesion, which was located intradural and extramedullary at the T7–T8 level (Figure 5).
Figure 4. Histopathologic appearance of cystic material.
Figure 5. Long-term follow-up sagittal T1-weighted MRI at 1 year shows a small relapse of cystic lesion, which is located intradural and extramedullary at the T7–T8 level.
DISCUSSION
Cystic hydatid disease is generally caused by an infection by the tapeworm cestode Echinococcus granulosus and mostly seen in areas where sheep and cattle are raised, particularly in Mediterranean countries (3,6). Humans can be infected by ingesting the eggs of the parasite. Liver and lungs trap oncospheres that migrate from the intestine to the portal circulation. Spinal hydatid cysts account for 1% of all cases of hydatid disease (3,4). Disease usually spreads over the spine by direct extension from pulmonary, abdominal, or pelvic infestation and most commonly affects the dorsal region of the spine (7–9). Spinal hydatid cysts are located most commonly at the thoracic (52%), followed by the lumbar (37%) and then the cervical and sacral levels (2). Braithwaite and Lees (10) classified spinal hydatid cysts into 5 radiologic types: intramedullary, intradural-extramedullary, extradural, hydatid cyst of vertebrae, and paravertebral lesions extending to spinal structures.
Primary spinal intradural extramedullary cyst hydatid is extremely rare (3,5–7). Spinal hydatid cyst is a serious form of hydatid disease. In the most recent reviews by Chakir et al (11), 23 cases of intradural spinal hydatid cysts were recorded in the world literature. Recently, Hilmani et al (12) published a case of intradural spinal hydatid cyst. Moreover, recently, Kahilogullarl et al (3) also reported a case. All previously reported cases were in adults. Recently, Karadereler et al (8) reported a case of spinal hydatid seen in a child. Our case differs from these cases in that the hydatid cyst was intradural and extramedullary. To our knowledge, this is the first case of primary intradural extramedullary hydatid cyst in a child in the literature.
The symptoms of spinal hydatid disease are non-pathognomonic, and symptoms are usually related to compression of the spinal cord (3,13). Generally, the first symptoms are back pain and radicular pain. Weakness of the limbs occurs in the later phase of the disease, and paraplegia is reported in 25% to 84% of cases (3).
Recurrence remains a major problem in spinal hydatidosis; the literature cites rates of 30% to 100%. Given this high rate of recurrence, spinal hydatidosis has a poor prognosis and has been compared with spinal malignancy (2). The poor prognosis may be related to localization (intradurally vs extradurally) of the cyst because of weak penetration of antihelmintic drug, albendazole, metabolites into the intradural space by passive diffusion transport mechanism (14).
In MRI examination, the appearance of a hydatid cyst on the scan is quite characteristic; it has 2 dome-shaped ends, yet has no debris in its lumen and looks like a sausage. Cyst walls are very thin and regular and have no septation (3). Serologic findings may help find the diagnosis, but they are not reliable alone.
The choice of the treatment in spinal hydatid disease has been surgery for nearly all cases. The preferred operative procedure is usually laminectomy (15). The total removal of the cysts without rupture should be the aim of the operation. Irrigating the wound with hypertonic saline or diluted Betadine solution after the cyst removal helps destroy and disrupt the parasites (2). In the early postoperative stage, adjuvant antihelmintic drug therapy must be given. The appropriate duration of antihelmintic therapy has not been established, but studies show a mean recommended course duration of 3 to 4 months (2,15–18). There are no pathognomonic signs or symptoms of spinal hydatid disease other than the symptoms related to compression of the spinal cord.
CONCLUSION
Although extremely rare, primary intradural extramedullary hydatid cyst pathology was the documented cause of leg pain and gait disturbance in this child. MRI is the best imaging tool for diagnosis of spinal hydatid disease, and the treatment of choice is surgery for nearly all cases. High rate of recurrence is a major problem, and this issue may decline with the aggressive resection of the cyst with its capsule and the administration of antihelmintic drug therapy.
Figure 2. Sagittal T2-weighted MRI shows spinal cystic lesion that is almost isodense with cerebrospinal fluid, causing intradural extension and spinal cord compression.
Figure 3. T2-weighted axial MRI shows an intradural extramedullary multiseptate cystic lesion.
REFERENCES
- Pamir MN, Akalan N, Özgen T, et al. Spinal hydatid cyst. Surg Neurol. 1984. pp. 53–57. [PubMed]
- Schnepper G, Johnson WD. Recurrent spinal hydatidosis in North America. Case report and review of the literature. Neurosurg Focus. 2004;17:1–6. doi: 10.3171/foc.2004.17.6.8. [DOI] [PubMed] [Google Scholar]
- Kahilog ullarl G, Tuna H, Aydln Z, et al. Primary intradural extramedullary hydatid cyst. Am J Med Sci. 2005;329:202–204. doi: 10.1097/00000441-200504000-00006. [DOI] [PubMed] [Google Scholar]
- Pandey M, Chadudhari MP. Primary hydatid cysts of sacral spinal canal: case report. Neurosurgery. 1997;40:407–409. doi: 10.1097/00006123-199702000-00040. [DOI] [PubMed] [Google Scholar]
- Fahl M, Haddad FS, Huballah M, et al. Magnetic resonance imagining in intradural and extradural spinal echinococco-sis. Clin Imaging. 1994;18:179–183. doi: 10.1016/0899-7071(94)90078-7. [DOI] [PubMed] [Google Scholar]
- Islekel S, Zileli M, Ersahin Y. Intradural spinal hydatid cysts. Eur Spine J. 1998;7:162–164. doi: 10.1007/s005860050048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baybek M, Incl S, Tahta K, et al. Primary multiple spinal extradural hydatid cysts. Case report and review of the literature. Paraplegia. 1992;30:517–519. doi: 10.1038/sc.1992.108. [DOI] [PubMed] [Google Scholar]
- Karadereler S, Orakdöğen M, Kiliç K, Özdoğan C. Primary spinal extradural hydatid cyst in a child: case report and review of the literature. Eur Spine J. 2002;11:500–503. doi: 10.1007/s00586-002-0411-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özer AF, Özek MM, Pamir MN, Erzen C. Magnetic resonance imaging in the diagnosis of spinal hydatid cyst disease. Case report. Paraplegia. 1993;31:338–340. doi: 10.1038/sc.1993.58. [DOI] [PubMed] [Google Scholar]
- Braithwaite PA, Lees RF. Vertebral hydatid disease. Radiological assessment. Radiology. 1981;140:763–766. doi: 10.1148/radiology.140.3.7280247. [DOI] [PubMed] [Google Scholar]
- Chakir N, Akhaddar A, El-Quessar A, et al. L'hydatidose intradurale extramedullaire primitive. J Neuroradiol. 2002;29:177–182. [PubMed] [Google Scholar]
- Hilmani S, El Malki M, Bertal A, et al. Lumbar intradural hydatid cyst: case report. Neurochirurgie. 2004;50:57–60. doi: 10.1016/s0028-3770(04)98307-5. [DOI] [PubMed] [Google Scholar]
- Baysefer A, Gonul E, Canakcl Z, et al. Hydatid disease of the spine. Spinal Cord. 1996;34:297–300. doi: 10.1038/sc.1996.54. [DOI] [PubMed] [Google Scholar]
- Takayanagui OM, Bonata PS, Dreossi SA, Lanchote VL. Enantioselective distribution of albendazole metabolites in cerebrospinal fluid of patients with neurocysticercosis. Br J Clin Pharmacol. 2002;54:125–130. doi: 10.1046/j.1365-2125.2002.01634.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao S, Parikh S, Kerr R. Echinococcal infestation of the spine in North America. Clin Orthop. 1991;271:164–169. [PubMed] [Google Scholar]
- Charles RW, Govender S, Naidoo KS. Echinococcal infection of the spine with neural involvement. Spine. 1988;13:47–49. doi: 10.1097/00007632-198801000-00011. [DOI] [PubMed] [Google Scholar]
- Fiennes AG, Thomas DG. Combined medical and surgical treatment of spinal hydatid disease. A case report. J Neurol Neurosurg Psychiatry. 1982;45:927–930. doi: 10.1136/jnnp.45.10.927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singotinas EG, Leventis AS, Sakas DE, et al. Successful treatment of intracerebral hydatid cysts with albendazole. Case report and review of the literature. Neurosurgery. 1992;31:571–574. doi: 10.1227/00006123-199209000-00022. [DOI] [PubMed] [Google Scholar]