Abstract
Background/Objective:
Approximately 250,000 patients are presently living with spinal cord injury (SCI) in the United States. Approximately 20% of patients with SCI are less than 20 years old, and 15% are less than 15 years old. The most common cause of pediatric SCI is a motor vehicle collision (MVC; ∼40%); lapbelt injuries and the seatbelt syndrome are seen more often in children involved in MVCs.
Methods:
A search and analysis of current literature on lapbelt injuries, seatbelt syndrome, and pediatric SCI using PubMed.
Results:
Children involved in MVCs who are improperly restrained are at higher risk of sustaining injuries. The risk of significant intra-abdominal injuries is increased almost fourfold in these children. Presence of abdominal wall ecchymosis (AWE) was associated with intra-abdominal injuries in up to 84% of children, with hollow viscus injury being the most common. Likewise, presence of AWE is associated with vertebral fractures, including Chance fractures, in up to 50% of patients. Vertebral fractures were associated with SCI in up to 11%. The presence of AWE in an improperly restrained child should warrant a thorough search for intra-abdominal injuries, vertebral fractures, and SCI.
Conclusions:
Lapbelt injuries and the seatbelt syndrome are often associated with pediatric SCI in improperly restrained children. This injury complex and its associated abdominal injuries are difficult to diagnose unless a high index of suspicion is maintained; delay in diagnosis increases morbidity, and early surgical intervention should be considered.
Keywords: Spinal cord injuries, Trauma, Child, Adolescence, Restraints, Lapbelt, Seatbelt syndrome, Motor vehicle crash, Intra-abdominal injuries, Vertebral fracture, Abdominal wall ecchymosis
INTRODUCTION
Spinal cord injury (SCI) remains a significant medical problem in the United States. According to the 2005 Annual Statistical Report for the Model Spinal Cord Injury Care Systems, approximately 250,000 people are living with SCI in the United States, with 11,000 new cases reported in 2005. Children and adolescents represent a significant fraction of patients (20% are <20 years of age and 5% are <15 years of age). Motor vehicle collisions (MVCs) account for approximately 40% of SCIs in the pediatric population. Boys are significantly more affected than girls, and the incidence increases with age, especially in late adolescence. Children 4 to 8 years of age are most likely to be suboptimally restrained (1,2).
Mechanisms of restraint are an important consideration for children, because improper restraints lead to a constellation of injuries during MVCs. Specifically, the constellation of findings resulting from wearing a 2-point restraint (lapbelt) include abdominal wall ecchymosis (AWE), intra-abdominal organ injuries (intra- and/or retroperitoneal), and vertebral fractures with SCI; together they characterize the seatbelt syndrome (3). Hence, when evaluating children involved in MVCs with any of the components of the seatbelt syndrome, a high index of suspicion must be maintained for associated injuries to avoid the devastating consequences of a delayed diagnosis.
METHODS
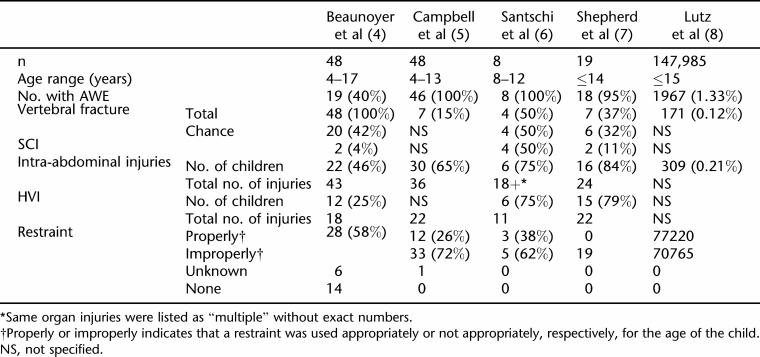
We searched the current literature using PubMed for “pediatric lapbelt injuries,” “seatbelt syndrome,” “pediatric spinal cord injury,” and “pediatric trauma.” Recent case series (1996–2006) that described restraint mechanisms, intra-abdominal injuries, vertebral fractures, and SCI were included in the analysis. We restricted our case series to a recent 10-year period to try to control historical variations in restraint use and injury patterns in MVCs. Four case series were included in the analysis, along with a larger cohort study (Table 1).
Table 1.
Collected Series of Pediatric Lapbelt Injuries Published in the Last 10 Years
Beaunoyer et al (4) presented a retrospective analysis of 48 children involved in MVCs who sustained a vertebral fracture. Analysis of type and location of vertebral fractures was performed, and associated injuries, including AWE, were documented. Details were provided on intra-abdominal injuries. Only data on presence or absence of a restraint were presented, without reference to mechanism of restraint (2-point vs 3-point harness). Other variables included location of patient within the motor vehicle, type of intra-abdominal injuries, findings on laparotomy, and survival rate.
Campbell et al (5) performed a retrospective analysis of 46 pediatric trauma patients with seatbelt contusions, with emphasis placed on radiographic study results and operative findings of intra-abdominal injuries. Incidence of vertebral fractures was also reported. The mechanism of restraint was described. Other variables included mechanism of impact, operative findings of specific intra-abdominal injuries, patient weight, and operative intervention (laparoscopy vs conversion to laparotomy).
Santschi et al (6) described a case analysis of 8 children involved in 3 separate multi-victim crashes. Extensive detail was given on all sustained injuries, including vertebral fractures, SCI, and intra-abdominal injuries. The mechanism of restraint was documented for each child. A case example of one child, including management and follow-up, was provided.
Shepherd et al (7) performed a retrospective analysis of 19 pediatric trauma admissions involved in MVCs and restrained with a lapbelt. Intra-abdominal and hollow viscous injury (HVI), with details regarding diagnostic imaging and laparotomy findings, were presented. Vertebral injuries and their types were also included. Presence of AWE was documented, and other sustained injuries were noted. Details regarding morbidity and mortality were present.
Finally, Lutz et al (8) conducted a large-scale population-based study on a cohort of children involved in MVCs based on data from Partners for Child Passenger Safety. Subjects were screened using a telephone interview and included restrained children who were involved in an MVC. Variables included AWE, intra-abdominal injuries, vertebral injuries, need for abdominal surgery, and optimal vs suboptimal restraint. Information was verified through medical records.
RESULTS
Our analysis of 4 recently published case series and a large population-based study of pediatric MVC trauma showed the increased risk of sustaining injuries associated with the seatbelt syndrome. A retrospective analysis of children with vertebral fractures revealed associated AWE in 40% and intra-abdominal injuries in 46%. HVIs accounted for approximately one half of cases of intra-abdominal injuries in this study (4). AWE is associated with significant intra-abdominal injuries (particularly HVI) in up to 75% (5–7). Among children presenting with AWE, up to 50% had a vertebral fracture (5–7).
In a large population-based study of MVCs, vertebral injuries were rare (0.12% of total population) but were more likely in children with abdominal wall bruising and far more likely with an intra-abdominal injury (14.56%) (8). Smaller series reveal that the majority (42–100%) of these fractures were Chance fractures (4,6,7). Although a clear association between SCI and vertebral fractures exists, our review revealed a wide range of 4% to 100% (4,6,7). A larger population-based study is needed for more conclusive results.
DISCUSSION
MVCs account for the majority of spinal injuries in children (1). Two-point restraints may cause flexion–distraction injuries of the thoracolumbar spine because the relatively rigid thoracic spine hyperflexes at the fixed fulcrum site of the lapbelt. Another predisposing factor of the lower thoracic and lumbar spine is the more sagittal location of the facet joints compared with the more frontal facet joints of the 1st through 10th thoracic vertebrae. The unique property of the Chance fracture is that the fracture line extends transversely through the spinous process, the laminae, transverse processes, pedicles, and into the superior surface of the vertebral body (9). Less common types of spinal injuries or SCI caused by the use of a lapbelt in a MVC include burst or compression fractures and SCI without radiographic abnormalities (SCIWORA).
In the seatbelt syndrome, the most common injury is intra-abdominal, which is thought to result from the compression of organs between the lapbelt anteriorly and the bony vertebral column posteriorly, especially considering the small anteroposterior diameter of a child (3,10). Moreover, the less muscular, thinner abdominal wall in children offers less protection against blunt trauma. The most common intra-abdominal injuries are HVIs, with the small intestine most commonly involved (3,4,11). The jejunum is the most common site of small intestine involvement, especially around the ligament of Treitz, because the fixation promotes shear stress tears; another vulnerable fixed site is the ileocecal valve (11). Other commonly involved intra-abdominal or retroperitoneal organs are the mesentery, solid organs such as liver, spleen, and kidneys, vascular structures, and the genitourinary system (ureters and bladder). Injuries to the vertebral column and SCI are the second most common within the seatbelt syndrome (4).
The evaluation of a pediatric patient involved in an MVC should include a complete work-up for vertebral, spinal cord, and intra-abdominal injuries in attempts to avoid devastating consequences of a missed injury. The presence of an AWE, abdominal and/or spine tenderness, and neurologic deficits on physical examination should mandate a search for other injuries associated with the seatbelt syndrome.
If the examination is noninformative or difficult to perform, diagnostic studies such as plain film radiography, computer tomography scans of abdomen and pelvis, and abdominal sonography or focused abdominal sonography for trauma (FAST) may provide useful information about intra-abdominal organ trauma. In cases where noninvasive diagnostic evaluation is non-contributory but HVI is suspected, peritoneal lavage or diagnostic laparoscopy may be appropriate (11).
Management of a child involved in an MVC presenting with AWE should involve initial spine immobilization at the scene. On arrival to the emergency department, intra-abdominal injuries take precedent over most spinal fractures and SCIs in the seatbelt complex. If HVI injury is diagnosed or highly suspected, exploratory laparotomy is indicated. Appropriate repair of any injuries to the hollow viscus and any other involved intra-abdominal organs should be undertaken; however, if the spine has not been cleared, spine precautions are essential during transfer to and from the operating room.
If vertebral fracture is diagnosed, correction of the misalignment may be indicated. Nonoperative treatment includes hyperextension of the spine and application of casts or orthosis for stabilization. Principles of operative treatment depend on level and severity of injury and whether injury to the spinal cord is present. Options include decompression and spinal fusion with or without use of instrumentation. In cases of SCI, the use of methylprednisolone may improve neurologic recovery, although this remains controversial (12). Close follow-up and rehabilitation are essential for proper healing and should be strongly encouraged.
CONCLUSION
Lapbelt injuries and the seatbelt syndrome are often associated with pediatric SCI in improperly restrained children. The presence of AWE in a child restrained with a lapbelt should warrant a search for other injuries, including spinal SCI, vertebral fractures, and intra-abdominal injuries. Although the most common findings are intra-abdominal injuries, the consequence of a missed SCI can be devastating. Therefore, prompt diagnosis and appropriate management of the pediatric trauma patient is necessary. This injury complex and its associated abdominal injuries are difficult to diagnose unless a high index of suspicion is maintained; delay in diagnosis increases morbidity and early surgical intervention should be considered. Proper restraint systems that are weight-and age-adjusted may prevent these injuries.
REFERENCES
- National Spinal Cord Injury Statistical Center . The 2005 Annual Statistical Report for the Model Spinal Cord Injury Care Systems. Birmingham, AL: National Spinal Cord Injury Statistical Center; 2005. [Google Scholar]
- Nance ML, Lutz N, Arbogast KB, et al. Optimal restraint reduces the risk of abdominal injury in children involved in motor vehicle crashes. Ann Surg. 2004;239:127–131. doi: 10.1097/01.sla.0000103068.51037.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman KD, Bowman LM, Eichelberger MR, et al. The lap belt complex: intestinal and lumbar spine injury in children. J Trauma. 1990;30:1133–1138. [PubMed] [Google Scholar]
- Beaunoyer M, St-Vil D, Blanchard H. Abdominal injuries associated with thoracolumbar fractures after motor vehicle collision. J Pediatr Surg. 2001;36:760–763. doi: 10.1053/jpsu.2001.22954. [DOI] [PubMed] [Google Scholar]
- Campbell DJ, Sprouse LR, II, Smith LA, et al. Injuries in pediatric patients with seatbelt contusions. Am Surg. 2003;69:1095–1099. [PubMed] [Google Scholar]
- Santschi M, Echave V, Laflamme S, et al. Seat-belt injuries in children involved in motor vehicle crashes. Can J Surg. 2005;48:373–376. [PMC free article] [PubMed] [Google Scholar]
- Shepherd M, Hamill J, Segedin E. Paediatric lap-belt injury: a 7 year experience. Emerg Med Aust. 2006;18:57–63. doi: 10.1111/j.1742-6723.2006.00809.x. [DOI] [PubMed] [Google Scholar]
- Lutz N, Nance ML, Kallan MJ, et al. Incidence and clinical significance of abdominal wall bruising in restrained children involved in motor vehicle crashes. J Pediatr Surg. 2004;39:972–975. doi: 10.1016/j.jpedsurg.2004.02.029. [DOI] [PubMed] [Google Scholar]
- Chance GQ. Note on a type of flexion fracture of the spine. Br J Radiol. 1948;21:452–453. doi: 10.1259/0007-1285-21-249-452. [DOI] [PubMed] [Google Scholar]
- Prince JS, LoSasso BE, Senac MO. Unusual seat-belt injuries in children. J Trauma. 2004;56:420–427. doi: 10.1097/01.TA.0000113256.49300.2B. [DOI] [PubMed] [Google Scholar]
- Bruny JL, Bensard DD. Hollow viscous injury in the pediatric patient. Semin Pediatr Surg. 2004;13:112–118. doi: 10.1053/j.sempedsurg.2004.01.007. [DOI] [PubMed] [Google Scholar]
- Bracken MB, Shepard MJ, Holford TR, et al. Administration of methylprednisolone for 24 or 48 hours or tirilazad mesylate for 48 hours in the treatment of acute spinal cord injury: results of the Third National Acute Spinal Cord Injury Randomized Controlled Trial. National Acute Spinal Cord Injury Study. JAMA. 1997;277:1597–1604. [PubMed] [Google Scholar]