Abstract
Objective:
To delineate the natural history of ambulation of children and youth with spinal cord injuries (SCIs).
Design:
Retrospective single-center.
Participants/Methods:
One hundred sixty-nine subjects who sustained SCI at 18 years of age or younger and who were followed up for at least 4 years.
Results:
Ambulation was significantly associated with age at injury and neurological impairment but not gender. Younger age at injury was associated with greater likelihood of ambulation, higher level of ambulation, and greater duration of ambulation. Lesser severity of neurological impairment was associated with greater likelihood of ambulation. Excluding ASIA D lesions, household ambulation was noted in 5% of subjects with tetraplegic, 26% with high thoracic, 30% with low thoracic, 44% with upper lumbar, and 33% with lower lumbar lesions. Of the 7 community-level ambulators with non-ASIA D lesions, none had cervical or high thoracic injuries, 3 had low thoracic, 1 had upper lumbar, and 3 had lower lumbar lesions. Using multiple regression analysis, predictive factors for ambulation were younger age at injury, total ASIA motor score, and ASIA impairment scale score. Less cumbersome orthotics were associated with higher levels of ambulation.
Conclusion:
Ambulation status is a function of neurological impairment, age at injury, and type of orthotic.
Keywords: Adolescence; Children; Spinal cord injuries, Pediatric onset; Rehabilitation; Shriners Hospital; Ambulation; Bracing; Orthotics; Paraplegia; Tetraplegia; Mobility
INTRODUCTION
After sustaining a spinal cord injury (SCI), a major goal of patients and their families is ambulation. In addition to the obvious psychological benefits of ambulation, there are a variety of potential medical benefits such as reduction of osteoporosis and improved cardiovascular fitness (1,2). However, a variety of factors limit the ability to ambulate, such as energy requirements, efficiency, financial costs, and cosmetics (3–6). A clear understanding of the natural history of ambulation in pediatric SCI will assist clinicians in counseling patients and their families on ambulation options. This study expands on previous reports on ambulation from one pediatric SCI program, with an increased number of subjects and longer duration of follow-up (7,8). There are no comparable published reports of ambulation in a large population of children and youth with SCI. Therefore, the purpose of this study is to delineate the natural history of lower extremity bracing and ambulation in children and youth with SCI, including identification of factors associated with the level and duration of ambulation.
MATERIALS AND METHODS
Subjects
Eligible subjects included patients who sustained SCI when they were 18 years of age or younger and who received care for at least 4 years at the Shriners Hospitals for Children, Chicago. All data reviewed were for patients who were injured between 1978 and 2000; 191 patient charts met the criteria. Patients were excluded if they had American Spinal Injury Association (ASIA) Impairment Scale scores of E, significant medical complications that would interfere with ambulation, or extended periods of absenteeism during their course of treatment at the Chicago Shriners Hospitals for Children.
METHODS
A review of medical records of eligible subjects was performed by a physical therapist who had not provided care for any of the patients. This retrospective study was approved by the Institutional Review Board at the Chicago Shriners Hospitals for Children. Impairment was measured using neurological level, ASIA Impairment Scale, and ASIA Motor Score as defined by the American Spinal Injury Association and the International Medical Society of Paraplegia (ASIA/IMSOP) International Standards for the Neurological Classification of Spinal Cord Injury (9,10).
Ambulatory status was categorized by the Hoffer classification as nonambulatory, therapeutic, household, and community (11). Individuals were considered community ambulators if they were able to walk indoors and outdoors for most of their activities, although they may use a wheelchair for long trips in the community. Household ambulators were patients who walked only indoors at home or school, and otherwise used a wheelchair for some indoor activities at home and school and for all activities in the community. Therapeutic ambulators were individuals who only walked in therapy sessions at home, at school, or in the hospital. Patients who required a wheelchair for all of their mobility needs were classified as nonambulatory. For purposes of this study, subjects who did not ambulate or ambulated for less than 1 year were considered as nonambulators. Individuals who were nonambulatory but who utilized a standing wheelchair or standing frame were defined as standers. Individuals who were either household or community ambulators were considered functional ambulators. Subjects whose last visit was within 1 year of chart review were considered active and those for whom the last clinical contact was greater than 1 year from the date of the chart review were considered as inactive.
Statistical analyses were performed using SPSS 11.5. For analyses utilizing duration of brace wear, the data utilized were from 73 patients for whom we had both a starting and end point for brace wear. This included 4 subjects who ambulated for less than 1 year and are otherwise classified as nonambulators for other analyses. Individuals who were still ambulating when they were discharged from our SCI program at age 21 years were not included in these analyses. Logistic regression analyses were performed for the dependent variable of ambulation (ambulation vs nonambulation), with and without ASIA D lesions. Independent variables included age at injury, gender, neurological level, ASIA impairment scale, and ASIA motor scores (both total and lower extremity scores).
RESULTS
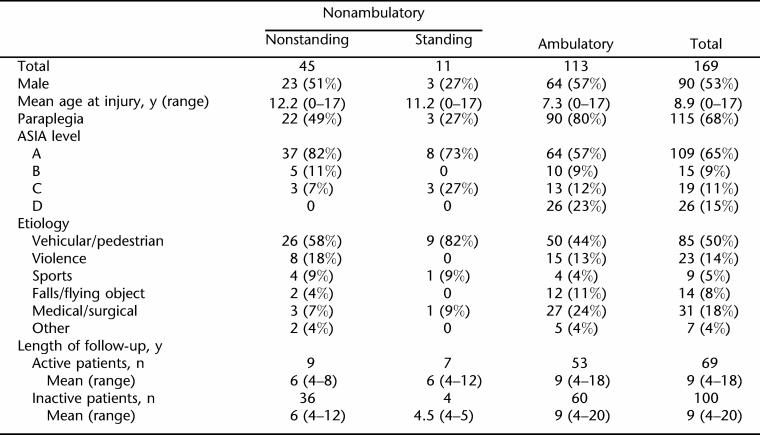
Of the 191 patients who were eligible for the study, 22 were excluded because of medical comorbidities (8 patients), inadequate follow-up (12 patients), or ASIA E lesions (2 patients). Medical comorbidities that excluded patients included lower extremity burns, lupus erythematosus, lower extremity amputations, Guillain-Barré syndrome, and juvenile rheumatoid arthritis. Characteristics of the 169 study subjects are detailed in Table 1. Of the 169 subjects, 69 (41%) subjects were actively being followed at the time of this study, 100 (59%) subjects were no longer being followed at the time of the retrospective review, and both groups had a mean follow-up of 9 years.
Table 1.
Summary Characteristics of Study Population
Of the 169 patients included in this study, 56 (33%) individuals were classified as nonambulators, including 4 subjects who utilized braces for less than 1 year (Table 1). All 4 of these individuals had paraplegia with ASIA Impairment Scale scores of A or B and were 2 to 16 years of age when injured. Of the 56 nonambulators, 11 utilized standing frames or standing wheelchairs. There were 113 subjects who ambulated for more than 1 year, with 17 (15%) being community ambulators, 42 (37%) household ambulators, and 54 (48%) therapeutic ambulators.
In this study population, ambulation was significantly associated with age at injury and neurological impairment but not gender. Female patients were more likely to be standers compared to male patients but the difference was not statistically significant (10% vs 3%; χ2 =3.19, P = 0.074).
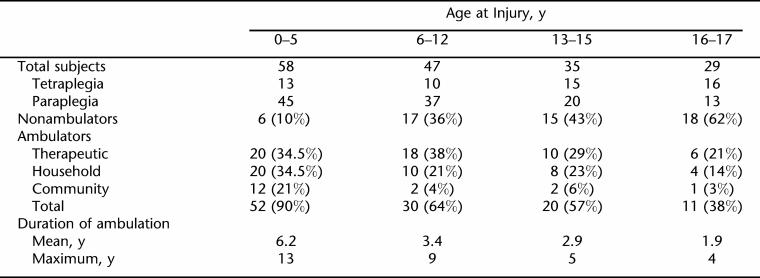
Younger age at injury was associated with greater likelihood of ambulation, a higher level of ambulation, and longer duration of ambulation. Children injured when they were 5 years of age or younger were 7.1 (95% confidence interval = 2.82–17.9) times more likely to ambulate compared to the 3 older age at injury categories (χ2 = 33.428, P < 0.001) (Table 2). The mean age at injury for those who were ambulators was 7 years compared to 12 years for nonambulators (P < 0.001). The vast majority of those injured at 5 years of age and younger were ambulators (90%) with 21% being community ambulators. In contrast, among those injured at an older age, only 55% ambulated, with 5% being community ambulators. These differences were statistically significant for both ambulation and community ambulation (χ2 = 20.703, P < 0.001; χ2 = 11.030, P = 0.001, respectively). In addition, those injured at 5 years of age or younger demonstrated a significantly longer duration of ambulation (mean of 6.2 years) compared to those injured in the 3 older age groups (means of 1.9 to 3.4 y) (P < 0.001). Of the 73 subjects who discontinued their ambulation while still under our care, only 19% (4/21) of subjects injured between ages 6 and 12 years and none of those injured in adolescence ambulated for more than 5 years; whereas 55% (16/29) of those injured at 5 years of age or younger ambulated beyond 5 years (χ2 = 20.7, P < 0.0001).
Table 2.
Ambulation Status as a Function of Age at Injury
In order to determine whether the neurological level was responsible for the finding of greater ambulation in those injured at younger ages, ambulatory status was studied separately for paraplegia and tetraplegia. Among those with paraplegia, 91% (41/45) injured at 5 years of age or younger ambulated compared to 70% (49/70) injured at older ages (χ2 =7.175, P =0.007). Community ambulation was achieved by 20% (9/45) of those injured at 5 years of age or younger compared to 6% (4/70) injured at older ages (χ2 = 5.575, P = 0.018). Among those with tetraplegia, 85% (11/13) injured at 5 years of age or younger ambulated compared to 29% (12/41) injured at older ages (χ2 = 12.366, P < 0.001). Community ambulation was achieved by 23% (3/13) of those injured at 5 years of age or younger compared to 2% (1/41) of those injured at older ages (χ2 = 6.129, P = 0.013).
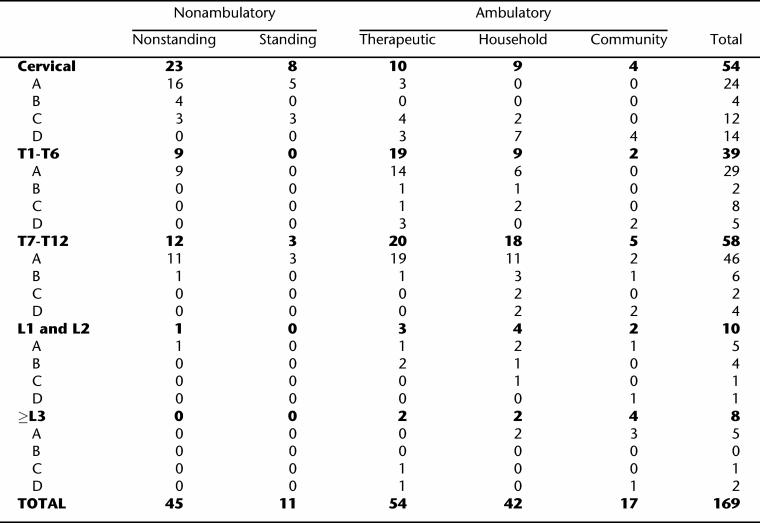
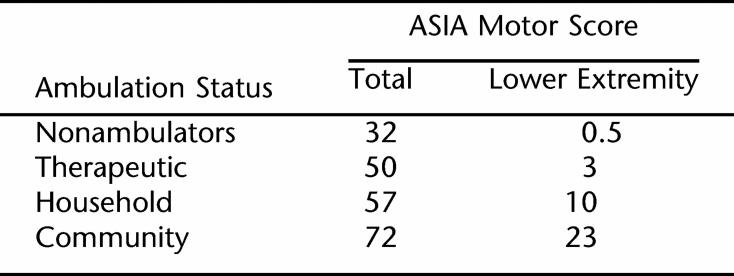
Lesser severity of neurological impairment was associated with greater likelihood of ambulation. Individuals with paraplegia were 4.85 (95% CI of 2.41–9.75) times more likely to be ambulators compared to those with tetraplegia (78% vs 43%; χ2 =21.100, P < 0.001). Among those with paraplegia, individuals with lumbar-level lesions were more likely to ambulate than those with thoracic-level lesions, but the differences were not statistically significant (94% vs 75%; χ2 = 3.285, P = 0.070) (Table 3). However, those with lumbar paraplegia were significantly more likely to be community ambulators compared to those with thoracic paraplegia (33% vs 7%; χ2 = 14.6, P = 0.002). Higher levels of ambulation were significantly associated with higher total ASIA motor scores (P < 0.001) as well as higher lower extremity motor scores (P < 0.001) (Table 4).
Table 3.
Ambulation Status as a Function of Neurological Impairment
Table 4.
ASIA Motor Scores and Ambulation Status
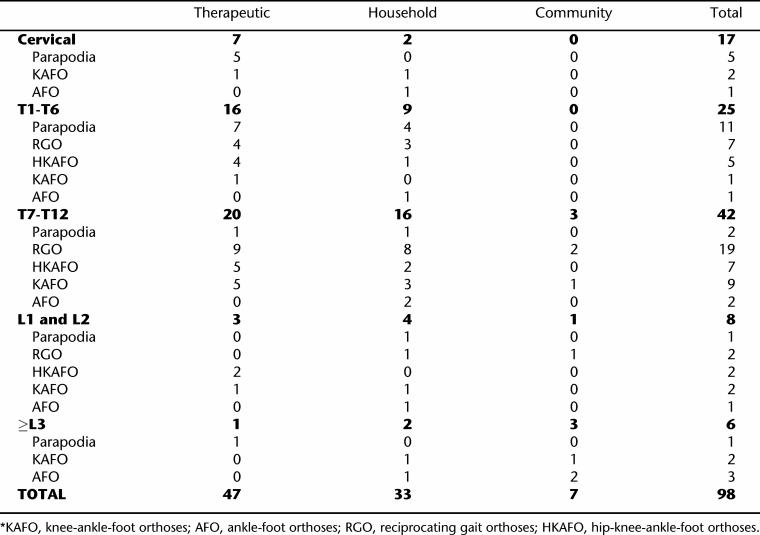
All 26 subjects with ASIA D lesions were ambulators, with 38% achieving community ambulation, 35% household, and 27% therapeutic. There were a total of 17 community ambulators with 10 having ASIA D lesions, including 4 with tetraplegia. Excluding subjects with ASIA D lesions, there were no community ambulators among subjects with tetraplegia or high-thoracic paraplegia (χ2 = 7.894, P =0.005) (Table 5). Furthermore, there were only 2 subjects with tetraplegia who were household ambulators, and both had ASIA C lesions.
Table 5.
Ambulation Status as a Function of Neurological Impairment and Type of Orthotics, Excluding Subjects With ASIA D Lesions*
Less cumbersome orthotics were associated with higher levels of ambulation. Table 5 describes the ambulatory status as a function of neurological level and type of brace used by subjects with non-ASIA D lesions. There were no community ambulators among users of parapodia or hip-knee-ankle-foot orthoses (HKAFO), whereas community ambulation was achieved by 11% (3/28) of the reciprocating gait orthoses (RGO) users, 12.5% (2/16) of knee-ankle-foot orthoses (KAFO) users, and 25% (2/8) of ankle-foot orthoses (AFO) users. Household or community ambulation (functional ambulation) was achieved in 21% to 30% of parapodia or HKAFO users, in approximately one-half of those who utilized RGOs or KAFOs, and in 100% of those who utilized AFOs.
Among subjects with ASIA D lesions, functional ambulation was not achieved by the 2 subjects who utilized RGOs or HKAFOs. In contrast, functional ambulation was achieved by 50% (3/6) of those utilizing KAFOs, 85% (11/13) utilizing AFOs, and all 5 who required no orthotics.
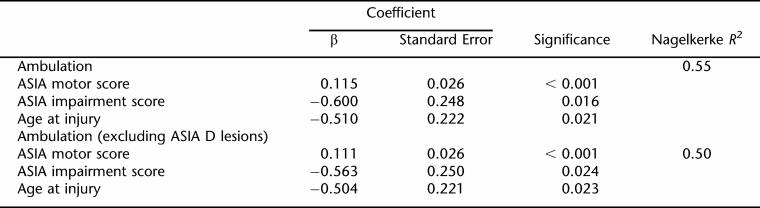
Table 6 demonstrates regression models for ambulation for all subjects and those with non-D lesions, with both having relatively high R2 values. In both models, total ASIA motor score, younger age at injury, and ASIA Impairment Scale were predictive factors.
Table 6.
Summary of Regression Analyses for Ambulation
DISCUSSION
Mobility is a critical factor for successful community participation and life satisfaction for individuals of all ages with SCI (12–15). For children and adolescents, community mobility must be viewed from a developmental perspective (7,8). This developmental perspective should encompass community activities that the child or adolescent would typically participate in as well as independence issues that change as children grow up. For infants and toddlers, the home is their primary community, which expands to the playground for the toddler, school and the neighborhood for the school-aged child, and the community-at-large for the adolescent. At all ages and for all community activities, mobility must be viewed as one of the key means of accomplishing goals. Mobility must be efficient, facilitate independence, and be acceptable to the child or the adolescent. Although walking is a pre-eminent goal for patients and their families, it is critical for clinicians to address ambulation as one component of mobility and not as an end in itself. An accurate appreciation of the natural history of ambulation in pediatric SCI can assist clinicians to accurately prescribe orthotics and counsel patients and their families on realistic expectations of ambulation.
The ability to walk and the extent of ambulation are a function of several factors, including age at injury and severity of neurological impairment (7,8). Using multiple regression analyses, age at injury and neurological impairment, as measured by total ASIA motor scores, were key predictors of ambulation, including community ambulation. Compared with those injured at older ages, children who were injured when they were 5 years of age or younger were more likely to ambulate, to be household or community ambulators, and ambulate for longer durations. The fact that children injured at younger ages are more likely to have paraplegia compared to those injured at older ages could explain these findings (16). However, younger age at injury remained a predictive factor for ambulation in regression analyses when level of injury was taken into account. In addition, younger age at injury was significantly associated with ambulation when studied separately for both those with paraplegia and those with tetraplegia. Although total ASIA motor scores, as well as lower extremity ASIA motor scores, were significantly associated with ambulation in univariate analyses, only the total motor score was a predictive factor. One possibility for this unexpected finding could have been the impact that subjects with ASIA D had on the regression models. However, in the regression model where subjects with ASIA D lesions were excluded, the total ASIA motor score and not the lower extremity ASIA motor score remained a predictive factor for ambulation. This finding may reflect the importance of upper extremity strength in addition to that of the lower extremities.
In previous reports of ambulation on 76 children and adolescents from the same patient population, similar findings were reported, including the impact of age at injury and neurological impairment on the ability and extent of ambulation (7,8). The prior reports had found that contractures and scoliosis were common antecedents to the discontinuance of ambulation. Because of the difficulty in ascribing a cause-and-effect relationship between complications (such as scoliosis, contractures, or pressure ulcers) and ambulation status, this was not studied in the current project.
This study provides evidence to support ambulation training as an integral component of rehabilitating children and adolescents with SCI. The outcomes of ambulation training observed in this study provide a baseline that future studies can utilize to determine whether improvements in outcomes can be obtained by different strategies, such as initiation of ambulation at different times after injuries.
The findings of this study are limited by the retrospective nature of this project, limitations of the ambulation and impairment classifications, the relatively small number of subjects in the 2 older age groups, and the fact that the subjects were all cared for at one tertiary healthcare setting. The retrospective nature of a chart review is limited by patient and parent report and accuracy of clinical documentation. The Hoffer classification scheme for ambulation status is limited by its lack of clear-cut endpoints for the different categories of ambulation. The International Standards for the Neurological Classification of Spinal Cord Injury are well established and widely used. However, the use of this impairment scale in the pediatric SCI population, especially in children age 8 years and younger, has not been validated, and the scale would most likely would be less accurate in younger children (17).
Although the current study may assist clinicians in prescribing orthotics and providing patients and their families with realistic expectations, a prospective study is needed to provide the foundation for an evidence-based practice for ambulation. In addition to the Hoffer classification, which is a relatively subjective assessment, other more quantitative measures of ambulation should be used. Objective tests of ambulation that may be useful outcome measures include the revised Walking Index for Spinal Cord Injury (WISCI II) and timed walking tests, such as the Timed Up & Go (TUG) test, the 10-meter walk test, and the 6-minute walk test (18–23). A prospective study is needed to more accurately elucidate predictive factors for ambulation, as well as factors that contribute to discontinuing ambulation. In addition to demographic and impairment factors and complications (such as scoliosis, contractures, or pressure ulcers), other potential features that may impact ambulation such as environment, participation, and personal factors should be studied. Personal preference, depression, accessibility of rehabilitation resources, and family issues are several factors that may significantly impact the ability and extent of ambulation. Potential benefits of ambulation need to be delineated in prospective studies. These may include cardiovascular fitness, prevention or correction of osteoporosis, and prevention of secondary conditions, such as pressure ulcers and urological complications. The impact of ambulation on the level of community participation and quality of life, in both the short and long term, would be valuable information with respect to the value of ambulation.
CONCLUSION
Because walking is such an important goal for most patients with SCI and their families, ambulation or standing should be an integral part of all rehabilitation plans. As with all aspects of pediatric rehabilitation, ambulation must be a part of an integrated program that is developmentally based and flexible to the changing needs of the child and youth with SCI. An ambulation program must balance realistic goals and effort involved in training with a positive, supportive, and developmentally based approach. Progression to different orthotics, assistive devices, and wheelchairs must be viewed from a developmental perspective and considered as natural progression rather than failure. It is important that all who are involved in caring for children and youth with SCI appreciate the limited role of ambulation in community mobility for the vast majority of patients with SCI. Effective, efficient, and feasible community mobility must be considered a primary goal for all children and youth with SCI, and ambulation should be one of the potential forms of mobility and not an end in itself.
Footnotes
This work was supported by Shriners Hospitals for Children.
REFERENCES
- Ogilvie C, Bowker P, Rowley DI. The physiological benefits of paraplegic orthotically aided walking. Paraplegia. 1993;31:111–115. doi: 10.1038/sc.1993.19. [DOI] [PubMed] [Google Scholar]
- Chantraine A, Crielaard JM, Onkelinx A, Pirnay F. Energy expenditure of ambulation in paraplegics: effects of long term use of bracing. Paraplegia. 1984;22:173–181. doi: 10.1038/sc.1984.31. [DOI] [PubMed] [Google Scholar]
- Massucci M, Brunetti G, Piperno R, Betti L, Franceschini M. Walking with the Advanced Reciprocating Gait Orthosis (ARGO) in thoracic paraplegia patients: energy expenditure and cardio respiratory performance. Spinal Cord. 1998;36:223–227. doi: 10.1038/sj.sc.3100564. [DOI] [PubMed] [Google Scholar]
- Waters R, Lunsford B. Energy cost of paraplegic locomotion. J Bone Joint Surg. 1985;67:1245–1250. [PubMed] [Google Scholar]
- Bernardi M, Canale I, Castellano V, Di Filippo L, Felici F, Marchetti M. The efficiency of walking of paraplegic patients using a reciprocating gait orthosis. Paraplegia. 1995;33:409–415. doi: 10.1038/sc.1995.91. [DOI] [PubMed] [Google Scholar]
- Nene AV, Hermens HJ, Zilvold G. Paraplegic locomotion: a review. Spinal Cord. 1996;34:507–524. doi: 10.1038/sc.1996.94. [DOI] [PubMed] [Google Scholar]
- Vogel LC, Lubicky JP. Ambulation in children and adolescents with spinal cord injuries. J Pediatr Orthop. 1995;15:510–516. doi: 10.1097/01241398-199507000-00020. [DOI] [PubMed] [Google Scholar]
- Vogel LC, Lubicky JP. Ambulation with parapodia and reciprocating gait orthoses in pediatric spinal cord injury. Dev Med Child Neurol. 1995;37:957–964. doi: 10.1111/j.1469-8749.1995.tb11950.x. [DOI] [PubMed] [Google Scholar]
- American Spinal Injury Association, International Medical Society of Paraplegia . International Standards for Neurological Classification of Spinal Cord Injury. Chicago, IL: American Spinal Injury Association; 2002. rev 2002. [Google Scholar]
- Marino RJ, Barros T, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003;26(Suppl 1):S50–S56. doi: 10.1080/10790268.2003.11754575. [DOI] [PubMed] [Google Scholar]
- Hoffer MM, Feiwell E, Perry R, Perry J, Bonnett C. Functional ambulation in patients with myelomeningocele. J Bone Joint Surg. 1973;55:137–148. [PubMed] [Google Scholar]
- Anderson CJ, Krajci KA, Vogel LC. Life satisfaction in adults with pediatric-onset spinal cord injury. J Spinal Cord Med. 2002;25:184–190. doi: 10.1080/10790268.2002.11753620. [DOI] [PubMed] [Google Scholar]
- Dijkers MP. Correlates of life satisfaction among persons with spinal cord injury. Arch Phys Med Rehabil. 1999;80:867–876. doi: 10.1016/s0003-9993(99)90076-x. [DOI] [PubMed] [Google Scholar]
- Fuhrer MJ, Rintala DH, Hart KA, Clearman R, Young ME. Relationship of life satisfaction to impairment, disability, and handicap among persons with spinal cord injury living in the community. Arch Phys Med Rehabil. 1992;73:552–557. [PubMed] [Google Scholar]
- Richards JS, Bombardier CH, Tate D, et al. Access to the environment and life satisfaction after spinal cord injury. Arch Phys Med Rehabil. 1999;80:1501–1506. doi: 10.1016/s0003-9993(99)90264-2. [DOI] [PubMed] [Google Scholar]
- DeVivo MJ, Vogel LC. Epidemiology of spinal cord injuries in children and adolescents. J Spinal Cord Med. 2004;27:S4–S10. doi: 10.1080/10790268.2004.11753778. [DOI] [PubMed] [Google Scholar]
- Mulcahey MJ, Gaughan J, Betz RR, Johansen KJ. The international standards for neurological classification of spinal cord injury: reliability of data when applied to children and youths. Spinal Cord. 2007;45:452–459. doi: 10.1038/sj.sc.3101987. [DOI] [PubMed] [Google Scholar]
- van Hedel HJ, Wirz M, Dietz V. Assessing walking ability in subjects with spinal cord injury: validity and reliability of 3 walking tests. Arch Phys Med Rehabil. 2005;86:190–196. doi: 10.1016/j.apmr.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Ditunno PL, Ditunno JF. Walking index for spinal cord injury (WISCI II): scale revision. Spinal Cord. 2001;29:654–656. doi: 10.1038/sj.sc.3101223. [DOI] [PubMed] [Google Scholar]
- Mathias S, Nayak USL, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil. 1986;67:387–389. [PubMed] [Google Scholar]
- Guyatt GH, Sullivan MJ, Thompson PJ. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J. 1985;32:919–923. [PMC free article] [PubMed] [Google Scholar]
- Butland RJ, Pang J, Gross ER, Woodcock AA, Geddes DM. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J. (Clin Res Ed) 1982;284:1607–1608. doi: 10.1136/bmj.284.6329.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collen FM, Wade DT, Bradshaw CM. Mobility after stroke: reliability of measures of impairment and disability. Int Disabil Stud. 1990;12:6–9. doi: 10.3109/03790799009166594. [DOI] [PubMed] [Google Scholar]