Abstract
Background/Objective:
Spinal cord injury (SCI) occurring during adolescence poses additional challenges because of the concurrent age-specific bio-psychosocial development. Full understanding of the psychosocial dimensions of rehabilitation requires exploration of the patient perspective. The objective of this study was to focus on psychosocial factors from the patient perspective in persons who had previously sustained a SCI during early and mid-adolescence (11–15 years of age).
Methods:
Twenty-four of the 28 persons who had sustained a SCI in Sweden from 1985 to 1996 participated in the study. Semistructured interviews were made an average of 10 years after injury. Narratives were analyzed qualitatively according to content analysis.
Results:
Parents and peers were found to have formed a crucial network. Parents frequently acted as advocates in interactions with health care providers, as supporters, and as containers of sorrow, frustration, and anger. Peers acted as promoters of activity and identity development. However, health care providers were perceived as not making sufficient use of this network.
Conclusions:
Rehabilitation professionals might be encouraged to increase their knowledge of adolescence medicine to better meet the specific needs and demands of persons in this age group. It is further suggested that parents and peers be considered important partners in the joint rehabilitation effort.
Keywords: Spinal cord injuries, Adolescence, Disability, Psychosocial issues, Sexuality
INTRODUCTION
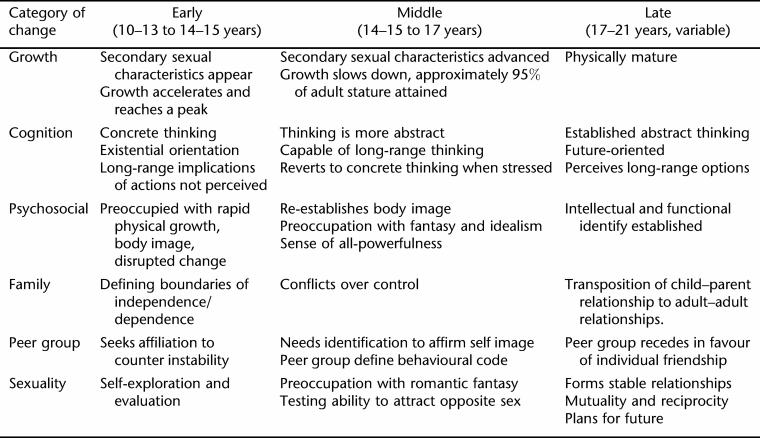
Persons in early to mid-adolescence (ie, 10–17 years of age) experience major biological and psychosocial changes in transition from childhood to adulthood. Such changes include the maturation of sexuality and reproductive capacity, rapidly changing emotional needs, and a gradual shift from concrete to abstract reasoning capabilities. Psychologically, there is a strong striving for independence. Socially, peer acceptance plays an increasingly important role (1–4).
The World Health Organization (WHO) has identified clinically relevant features of adolescence in its Orientation Program on Adolescent Health for Healthcare Providers (5). The program was created to improve and adapt health care services to young people's special needs and concerns. These factors are depicted in Table 1.
Table 1.
Characteristics of Phases of Adolescence (5)
When major injury or illness occurs during adolescence, it poses unique challenges because of the concurrent physical and psychosocial development processes (6–8). Principles of psychosocial rehabilitation during adolescence are to some extent generic (ie, irrespective of diagnosis) (9). Literature on chronic illness during adolescence underscores the importance of giving attention to the biological, emotional, and social needs of the young person (7,10–15). Furthermore, the social context has been identified as a key factor that sometimes is not given enough attention when caring for young persons (16–21).
Spinal cord injury (SCI) affecting adolescents is a devastating and life-altering event (8). The importance of age-related issues and the need for developmentally based care for SCI has been elaborated in several articles and studies (8,22–31).
Previous research has mainly focused on adjustment later in life (32–35) and on the transition to adult care settings (36–38), rather than on the primary rehabilitation process and the early readjustment thereafter. Few studies have specifically focused on psychosocial aspects of care from the perspective of the young persons themselves (13,14,18–20,39).
Little is known about the patient or first-person perspective of sustaining a SCI during adolescence. Our main purpose was to explore and describe adolescent SCI from that perspective. This motivated the choice of a qualitative study design. Specifically, we aimed at exploring psychosocial factors deemed as facilitating and impeding the rehabilitation process, respectively.
METHODS
Qualitative research is exploratory and inductive in nature. This approach allows more in-depth and comprehensive information. Respondents express their thoughts and experiences in their own words rather than by predefined response alternatives (40). The “experienced adolescent” has been found to be imaginative in suggesting ideas and solutions, many of which may not be obvious to health care professionals (12). Thus, individual narratives were obtained by semistructured open-ended personal interviews. Narratives were analyzed according to content analysis (ie, a well-established method of identifying, coding, and categorizing patterns in qualitative data) (40).
Interviewees
In an earlier incidence study, we identified persons who, at the age of 0 to15 years, had sustained a SCI in Sweden in the period from 1985 through 1996. Data from population registers, County Habilitation Centers, and from several informal sources were used (41). A total of 37 persons who survived at least 2 years after injury were thus identified. This group was made up of the total national prevalence population of pediatric-onset SCI during the time surveyed.
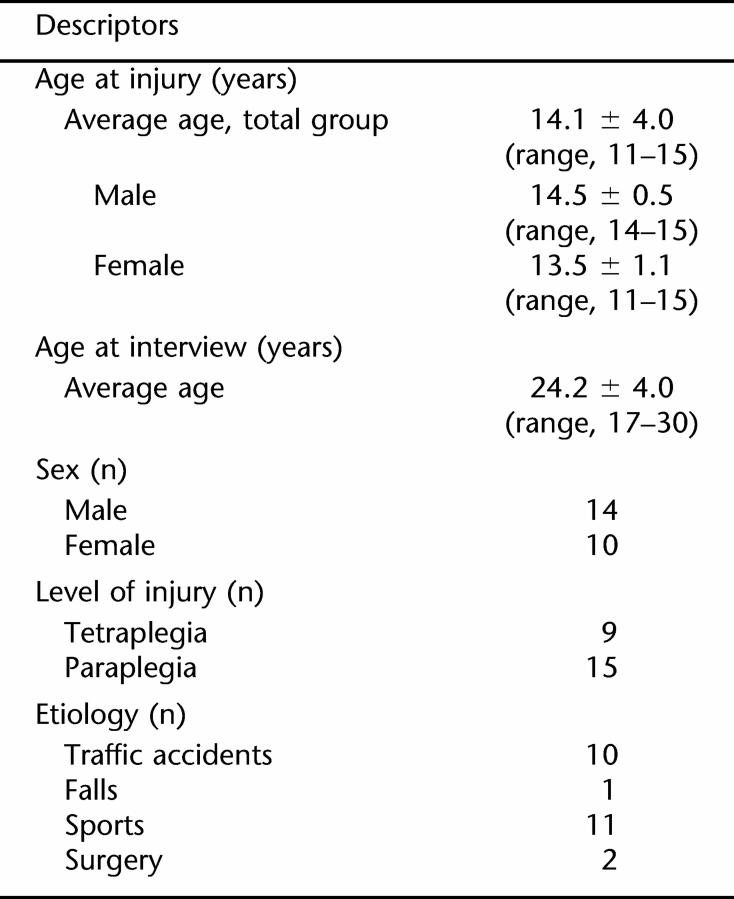
Twenty-eight of these 37 persons were 11 to15 years of age at the time of injury and were contacted for inclusion in this study. One man was excluded because of severe comorbid mental retardation, 1 man had died, and 2 men declined participation, leaving 24 persons to participate in this study. Nine persons had a complete lesion according to American Spinal Injury Association (ASIA) standards (42). Fifteen persons were wheelchair users. Twenty-two persons had been treated in adult care settings: 19 in SCI units, and 3 in orthopedic departments. Five persons had subsequently been referred to Habilitation Centers for follow-up. Further descriptors are depicted in Table 2.
Table 2.
Interviewee Descriptors by Age at Injury, Age at Interview, Sex, Level of Injury, and Etiology (n = 242)
Data Collection
Interviews lasted 60 to 90 minutes and were conducted by 1 of the authors (M.A.) at the venue of choice of the interviewee, typically his/her home. The recorded interviews were transcribed verbatim. Interviews were performed during 2002 to 2004, an average of 10 years (range, 4–15 years) after injury. Three themes were addressed: (a) factors felt to have been beneficial to the care and rehabilitation process; (b) factors felt to have been impeding the care and rehabilitation process; (c) suggestions for improvement of care and rehabilitation process. The dialogue was expanded by use of further open-ended questions, eg, “What do you mean by that?”; “Can you describe a little bit more about this?”; “What did you think about that?”
Data Analysis
Transcripts were analyzed by content analysis (40). This method is made up of a stepwise process where subcategories, categories, and core categories are identified inductively. It aims at revealing distinct themes within data: common patterns, topics, and categories emerge. Observed repetitive sequences, or regularities, allow for systematization and classification (40).
Narrative analysis was made in 5 steps, identifying manifest messages from the recollections (40): all tapes and transcripts were listened to and read iteratively for an overall understanding (43); a preliminary coding of each transcript was made, highlighting sentences that captured key concepts; the text was read through several times and so-called meaning units were identified (each such unit is comprised of words, sentences or paragraphs that cover aspects that are connected through content and context) (44); units were grouped into thematic subcategories (subcategories were further aggregated into categories and core categories) (40); and the process was iterated until no new patterns or themes emerged.
To assess concordance within and between narratives, frequency counts of the categorical aggregates were obtained. To further clarify categorical content, verbatim citations illustrative of each subcategory were selected. They are presented throughout the Results section of this paper.
Data Validation
Categories were subsequently validated by a consensus strategy, whereby the authors discussed and re-examined coding discrepancies to reach consistency.
Ethical Considerations
The study was approved by the regional research ethics committee. Interviewees gave informed consent and were granted confidentiality. Individual interviewees would not be identifiable in the subsequent report. Interviewees were informed that they could terminate their participation in the study at any time. The interviewer (MA) was not involved in the medical care of any interviewee at any time.
RESULTS
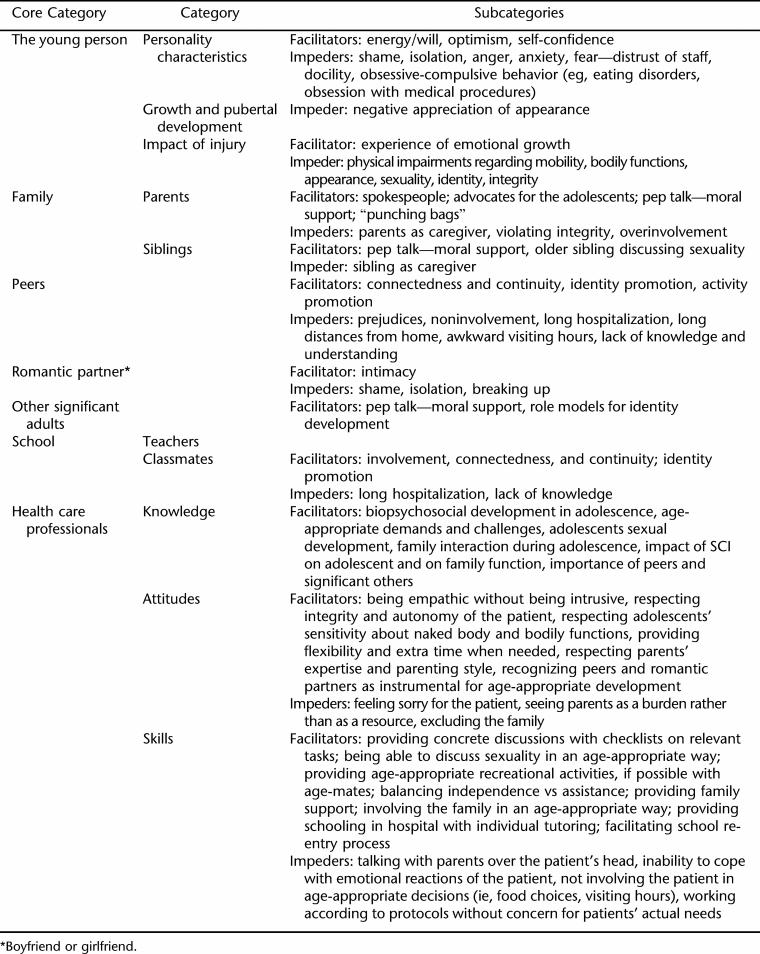
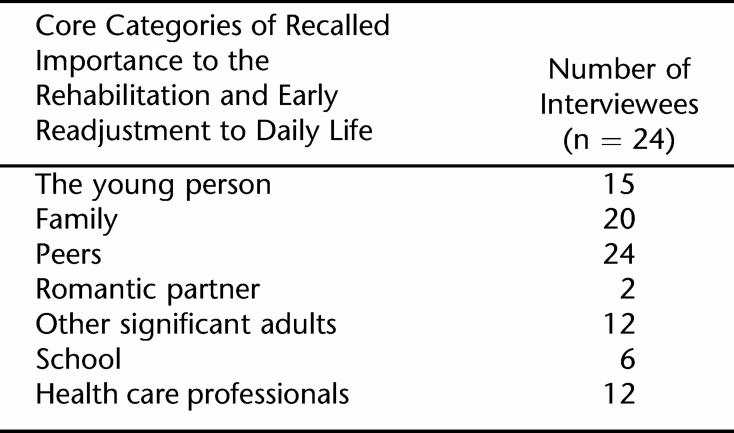
Seven core categories were identified: (a) the young person, (b) the family, (c) peers, (d) romantic partners, (e) other significant adults, (f) school, and (g) health care professionals. Specific actions within core categories were made up of a number of psychosocially relevant subcategories. These are summarized in Tables 3 and 4 and will be elaborated on in more detail in the following section.
Table 3.
Core Categories, Categories, and Subcategories Facilitating or Impeding Rehabilitation and Early Readjustment After SCI
Table 4.
Frequencies of Core Categories Recalled by the Interviewees as Having Promoted the Rehabilitation and Early Readjustment After SCI
The Young Person
Personality. The interviewee's ability to deal with the consequences of injury was reflected in statements, such as “ stubborn until you get what you want,” “pigheadedness,” “having a lot of guts,” and “being contrary.” A positive self-image, an optimistic outlook, and an ability to see possibilities rather than obstacles (15/24) were important assets. Seven of 24 interviewees recalled reacting with shame, isolation, or docility. Anger toward parents and health care professionals occurred frequently (13/24), and some interviewees described themselves as having been “difficult,” “obstinate,” and “rebellious.” Some (7/24) reacted by trying to gain control over their environment, eg, by checking medical procedures in detail, showing distrust for staff, becoming picky with food, even developing eating disorders: “I think I lost about 10 kilos during that period…. There must be something I can make my own decisions about! I think—I think that's why I did it. You have to be able to control something yourself and decide about it, don't you think?” (female, 13 years at injury, interviewed 4 years later).
Growth and Pubertal Development. No direct comments relating to pubertal development were found. However, one interviewee indirectly related to this issue: “I thought it was good to be able to stand up (on the tilt table) and have a quick look at my body to try to get an idea of what it was like. You miss out on the daily routines of getting up and taking a shower in the morning, washing yourself, and getting dressed. There is no contact with your body at any time; your body doesn't exist in the intensive care because you're nursed so much. I didn't feel my body then either. It was pretty weird when I started looking down at my body … Jesus, I've got some hair on my stomach kind of thing, I've never seen that before. You were always being tucked in with loads of blankets” (male, 15 years at injury, interviewed 10 years later).
Seven of 24 interviewees had felt physically unattractive, eg, by having a bad hairdo, wearing ugly hospital clothes, looking stupid walking with aids, or by not being able to wear tight jeans any more.
Impact of Injury. All interviewees (24/24) related to difficulties caused by neurologic impairment, eg, trying to master activities of daily living (ADL) techniques, experiencing altered or lost bodily function, eg, bladder and bowel control, as well as having to endure nursing procedures violating personal physical space. “Putting catheters in … I thought that was so gross. I refused to do it, I didn't want to touch myself or see myself down there. When I was staying in the hospital and wanted to go to the bathroom and pressed the buzzer, I hated it when a guy came. I think it's really degrading” (female, 13 years at injury, interviewed 10 years later).
Fifteen of 24 interviewees reported that they hadn't been adequately informed about sexual function: “It was different back in 1985. I was full of questions but never got any answers” (male, 15 years at injury, interviewed 15 years later). “Of course it (sexual issues) is something you think about when you're 13, I did anyway. It's obviously a big deal when you're that age. You're just starting to date guys …” (female, 13 years at injury, interviewed 10 years later).
In contrast to the frequent reports of various negative consequences of injury, some interviewees (8/24) attributed certain positive effects: “My self-confidence grew in some ways. I went through so much that I knew subconsciously that I could handle a lot of things and so I think I calmed down a bit. Yeah, I became more mature and maybe more myself” (male, 14 years at injury, interviewed 7 years later). “I'd love not to have this disability … but I don't regret having the accident as such, since it has had such a (positive) impact on me” (female, 13 years at injury, interviewed 4 years later).
One interviewee expressed grief over a “lost adolescence”: “I feel like I skipped some years between 14 and 18 years. Others could test different things; I had to be grown up fast; to be an adult at once” (female, 14 years at injury, interviewed 12 years later).
In summary, having a “fighting spirit” was frequently seen as a beneficial factor. Outwardly directed anger and aggression was common. Psychosocial problems related to physical disability were frequently recalled but also comments reflecting resilience.
Family
Parents. Parents were typically (20/24) recalled as having played a key role in helping the young person cope with the injury.
Parents acted as spokespeople and advocates (7/24) for their child in communications with staff. Parents also acted as trusted supporters (13/24), as discussion partners, and as “pep talkers”: “My father told me: Don't give up hope until you know the facts for sure. That made me able to struggle on” (male, 15 years at injury, interviewed 10 years later). “But (my father) has always said: you'll find someone who will like you and love you and have a family with you and you'll be very happy and have children and everything. But I'm like: nah, that won't happen to me, and you know that too. I said: Nobody will like me. He answered: Don't say that! He kinda saw all the good things in me, which I, like, couldn't see then” (female, 11 years at injury, interviewed 11 years later).
Parents “absorbed” the sorrow, frustration, and anger that interviewees hesitated to share with staff (10/24): “I think I turned a lot of this anger and frustration against my parents. They got more than their fair share. That's why I fell out so badly with my mom. There were periods when I couldn't even talk to her, didn't want her!! It was easier to take it out on my parents or some other relative or my friends than to take it out on the staff” (male, 15 years at injury, interviewed 14 years later).
One male interviewee reported to have become irritated when his mother repeatedly pushed him to follow the instructions of the physical therapist: “And then mom comes and says, “Look, you're going to ride the bike. I've spoken to the physical therapist now and she says you have to ride the bike so now you're going to ride the bike.” Like—ride the f******* bike yourself!” (male, 15 years at injury, interviewed 14 years later).
Eight of 24 parents took on, or were given, the role as caregivers, something that could be for better or worse: “They (the staff) dumped a lot of stuff like that (catheterization) on them (my parents) then. They took responsibility so that I could come home on visits and stuff. So they just learned how to do it” (female, 13 years at injury, interviewed 10 years later).
“Yeah, it feels really stupid, it felt really stupid with my mom helping me shower and stuff. But Mom told me that I shouldn't find it embarrassing because she did it when I was a baby … But it was really embarrassing, actually” (female, 15 years at injury, interviewed 4 years later).
The balance between adequate parental support vs overinvolvement was commented on by one interviewee: “When something like this happens in a family, you're so emotionally involved in each other's lives. That's what's happened here, so we have a problem. We're too close to each other, we interfere in each other's lives, it gets to be too much” (female, 13 years at injury, interviewed 10 years later).
In summary, parents played a key role. Frequently, hospital staff was perceived to have been insensitive in accommodating the important role of the parents. The role of parents as caregivers was double-edged.
Siblings. Overall, there was little mention of siblings in the narratives. However, 2 interviewees told of older siblings who helped out with daily care, moral support, or advice in sexual issues: “I don't know what I would have done without my sister. She told me about sex” (female, 13 years at injury, interviewed 10 years later).
Peers. All (24/24) interviewees expressed that peers and friends had played a key role. One man reported that he was very depressed, isolated himself, and refused to talk with the staff. When one of his old friends eventually visited him, this had a very positive impact: “When he entered, I just said “Hi, how are you” and suddenly I became my old self again” (male, 15 years at injury, interviewed 13 years later).
Fifteen of 24 narratives gave peers credit for having put them “back on the track”: “Many times, I felt that I just wanted to stay at home, but they (the friends) more or less carried and dragged me and the wheelchair out of the house. This, to have my friends around, was probably what made me come back again. They didn't let me sit at home; they basically forced me to get moving. This was the best of all, and it had to be done” (male, 15 years at injury, interviewed 15 years later).
Occasionally (4/24), feelings of shame led to isolation from peers: “I distanced myself from my friends, 'cause I didn't think I could do very much and that kind of thing. And like be seen in a wheelchair. I've always been the tough little girl, and then all of a sudden I became like the complete opposite” (female, 15 years at injury, interviewed 4 years later).
Eleven of 24 interviewees commented that they subsequently found a new circle of friends after injury. Twelve of 24 interviewees reported having lost contact with many of their peers after injury. Several reasons for this were given, such as spending long periods as an in-patient, traveling long distances from the hospital to the home environment, and restricted visiting hours. Five of 24 interviewees thought that their peers' lack of knowledge about SCI made them reluctant to maintain contact.
In summary, peers were of prime importance. Many interviewees apparently lost contact with their old circle of friends but managed to find a new social context.
Romantic Partner
Only 3 interviewees had a romantic partner (ie, boyfriend or girlfriend) at the time of injury. Two interviewees felt that their boyfriends were very important for emotional support and intimacy, even if time together was restricted, eg, by visiting hours: “I had a boyfriend at the time and I could talk about anything with him. I talked to him over the telephone and then everything went much better. There wasn't anyone else I could talk to. He wasn't allowed to sleep over. They had visiting hours, you know, but people could stay until 8 or 9 anyway. So the phone bill was pretty expensive” (female, 15 years at injury, interviewed 4 years later). One male interviewee ended his relationship, and explained this as follows: “I had a girlfriend when I was 15. I didn't want her to come and visit me. I felt so immobilized. It is a typical reaction that you isolate yourself in desperation instead” (male, 15 years at injury, interviewed 10 years later).
Other Significant Adults
Twelve of 24 interviewees mentioned that persons outside their core family had acted as support and provided pep talk. These were friends of the family, coaches, or health care professionals who continued this relationship after discharge from hospital. “My coach came almost every day. He was totally amazing. Every day he brought along some of my teammates. He was always positive … We're still in touch” (male, 14 years at injury, interviewed 9 years later).
Fourteen of 24 interviewees reported that they had been introduced to patient's organizations, role models, and training camps at an early stage. Reactions to this were mixed. The response was unfavorable if the role model was too old or had a different kind of disability. Male interviewees, in particular, reported benefits from being introduced to role models and praised them and camp attendance as being very important.
The importance of a role model could be significant: “She had two children then. She was around 38 (the role model) … She was a really open and very happy person. “Now I'm going to the bathroom and I'll be really quick” … amazing … she really showed what an easy life she had, nothing's a problem and she's like “I'm just going out for a while” and then she just went out to like get something. One kid hopped on by himself and she just rolled off you know, and “we don't need to take the wheelchair” and just backed out the car, and I just, really cool, and then I thought: Can it really be like this? …” (female, 11 years at injury interviewed 11 years later).
Psychologic benefits of camp visits were sometimes substantial: “The camp with other people with spinal cord injuries was a great kick. Dad said that when I came back home from camp he recognized me again and got very happy—I was finally back. I had found myself again” (male, 15 years at injury, interviewed 10 years later).
In summary, persons other than family members were often helpful in the rehabilitation process. Role models could be very important. Matching age and disability were recalled by some interviewees as necessary.
School Network
The social network at school, including teachers and classmates, was mentioned by 6 of 24 interviewees as being important, and return to school was vividly recollected. The importance of staying in touch with teachers and classmates was emphasized.
The way reintroduction to school occurred was of importance, in particular, allowing for the natural curiosity of peers and feeling in charge of the situation: “I told them (my classmates) what had happened and I received a lot of respect because of that. They thought it was exciting … Everyone asked me questions about the injury. I think this helped …” (male, 15 years at injury, interviewed 15 years later).
Twenty-one of 24 interviewees returned to their previous school, but 10/24 did not graduate with their class. In 1 case, architectural barriers precluded return to the previous school. Two interviewees mentioned that the long in-patient rehabilitation stay had complicated subsequent return to school, and another 2 interviewees felt that there was a lack of coordination between the rehabilitation facility and the school.
Health Care Professionals
Health care professionals were recalled in a positive way by 12 of 24 interviewees. Most comments reflected the importance of getting enough time; of being listened to; and of being allowed to actively participate in decision-making.
Eight of 24 interviewees emphasized the importance of the personality of the individual caregiver: “What's good (in rehabilitation) is the people; you can't ever get away from the fact that the people that work with this—they are the ones that made it good” (female, 14 years at injury, interviewed 11 years later).
Six of 24 interviewees complained that staff seemed to have lacked experience working with teenagers. One illustrative comment was: “They'd never had a stubborn 13-year-old with a temper before, they didn't know how to handle it” (female, 13 years at injury, interviewed 13 years later).
Positive factors, on the other hand, included the ability to support empowerment and peer involvement: “The physical therapist was great (because she said): “Now we're going to solve the problem of how you can get out of bed by yourself, how can we solve that?” (male, 15 years at injury, interviewed 10 years later).
“I got permission to have a TV and video and I put up loads of posters all over the room, and I got to keep a single-bed room the whole time I was there and I could have people come and sleep over. We watched videos and ate popcorn. I still remember my friends really well; I even remember which films we watched. It was so cool that everyone lived nearby and could visit. I can't remember ever lying there bored” (female, 14 years at injury, interviewed 14 years later).
Provision of clear rules of conduct and a straight-talking attitude was also perceived as being helpful: “I was a nightmare patient for over 6 months … was a real pain in the ass, causing trouble the whole f****** time, yelling at everyone and being overall unpleasant. I thought everyone was stupid, so they all tried to make a fuss of me and stuff. “Hello, honey, how are you today?” What the hell do you care? It's just your f****** job to ask. The only ones I had any respect for were the ones who fought back, “Jesus, what a b***** you are today. If you don't have anything nice to say don't bother opening your mouth.” I could respect them because I felt they were for real” (female, 14 years at injury, interviewed 11 years later).
Eight of 24 narratives reflected conflicts between parents and staff. Staff, in these cases, was felt to regard parents as a burden rather than a resource.
Fourteen of 24 interviewees reported having been “forced” by staff to see a psychologist for crisis intervention. Some interviewees thought that counseling by the regular staff would have been preferable. ”What should I talk about; I don't want to talk. I don't know her (the therapist) and it's demanding, they force themselves on you … Here she comes because it's on the schedule” (female, 11 years at injury, interviewed 11 years later). “I didn't like her (the therapist), even if she was very cheerful, and I couldn't talk to her. I could talk about what had happened that day, but nothing about other things. Even if I had a lot to say …” (female, 13 years at injury, interviewed 4 years later).
In summary, staff was generally appreciated for being knowledgeable, concrete, structured, and empathetic. However, there were also frequent reports of clashes between staff and patients, as well as negative memories of having been “forced” to meet with a psychologist.
DISCUSSION
To our knowledge, this is the first qualitative study of the psychosocial needs of young adolescents sustaining a SCI, focusing on the views and experiences of the young persons themselves. The 24 interviewees in this study constitute almost all persons who sustained a SCI in Sweden during 1985 to 1996 in their early or mid-adolescence. The findings illuminate the importance of the personal strengths of the young persons themselves, as well as that of their social network in helping them through rehabilitation and early readjustment to daily life.
Parents and peers in particular were found to play a crucial role. Parents were frequently recalled as acting as advocates in interactions with health care providers. They were also recalled as supporters and as absorbers of sorrow, frustration, and anger that the interviewees hesitated to share with staff. Peers played a key role as promoters of activity and identity development. However, health care providers were not perceived as promoting involvement of this network.
Apart from the inherent and inevitable limitations of a qualitative methodology, the most obvious limitation of this study is perhaps the recall bias imposed by the years gone by from injury to interview. However, recollections as such are of significance, regardless of their “objective” validity. Furthermore, the results reflect experiences consequential to the Swedish health care system of 10 to 20 years ago. According to a recent study from our group regarding pediatric SCI care in Europe (45), however, this health care system seem to differ little from what is typically the case in Sweden and parts of Europe today.
No attempts were made to relate the recollections of the early rehabilitation process to the present quality of life of the interviewees. It was felt that too many confounding factors, unrelated to the initial events, would have influenced the findings as to make them meaningful in this context.
Specialized SCI units have a high level of medical competence regarding the injury and its consequences in the view of the informants. However, insufficient biopsychosocial management as it pertains to young patients was reflected in this study. Because pediatric SCI remains a rare disorder in Sweden and elsewhere, young persons are still (41) typically treated in adult settings. It is doubtful, however, whether age-specific knowledge and skills are as yet incorporated in clinical management. During early adolescence, the young person is typically concerned with changes in body and body image (1,3,46). There is uncertainty about appearance and attractiveness, preoccupation with self, and an increased interest in sexuality. A young person with SCI may face these challenges in a situation where the injury has imposed drastic physical changes. In addition, a need for assistance with intimate body functions puts further stress on this issue, something that was reflected in the narratives. For health care professionals treating adolescents with SCI, it is thus important to understand and respect the need for privacy and acknowledge the sensitive issue of the naked body.
The expressed lack of information regarding sexual issues is notable, because sexuality is of central concern during adolescence and because SCI typically impairs sexual function. This issue has been highlighted in a previous Swedish study (47). Specifically, adolescents with SCI may benefit from having contact with other persons with SCI who can facilitate discussions and describe real-life experiences regarding sexuality and reproduction (8).
There were many examples in the narratives that communication with persons in early adolescence typically needs to be more distinct, concrete, and structured than what is typically necessary when addressing adults. Furthermore, there were many instances where the young person's inclination to act out led to conflicts with parents and staff. Behavioral expressions of distress, such as denial, depression, regression, anger, and withdrawal, are likewise common in chronic illness during adolescence and should as a rule be seen as an adaptive psychologic response to injury (7). It needs to be handled in an age-appropriate way (6). Initial refusal to comply with treatment may also often be regarded as developmentally appropriate in adolescence (12). Routine referral to a psychologist, as recalled in this study, may be counterproductive.
Contrary to what may be explicitly expressed, young persons typically do seek and need support and guidance from their parents (48). This was reflected in many interviews. These findings are in accordance with previous studies of young persons with chronic illness (16–21). A more active involvement of parents in the rehabilitation process and provision of support for them when needed might prevent many conflicts and misunderstandings (18). Typically, parents and the young person may become involved in power struggles about who should be in control of the treatment and rehabilitation process (7,22). Improved outcomes have been shown when parents are able to be supportive and maintain an appropriate balance between medical management requirements and the young person's developmental needs (7,16). However, as was reflected in our results, it is questionable from a developmental point of view if parents should take on a role as personal assistants, especially regarding intimate body functions.
The importance of connectedness with peers is emphasized in the literature on young persons with chronic illness (1–3,11,12,16–21,49). This was also reflected in many narratives in this study. All interviewees mentioned the positive impact of peer contact.
The key part played by role models in the rehabilitation of patients with SCI, both in promoting an active lifestyle and in helping to establish a new identity, has been proposed previously (50,51). Importantly, as was reflected in this study, the role model seems to achieve credibility by matching the patient with regard to age, sex, and type of disease.
Early school involvement has been reported as successful in facilitating the transition from rehabilitation to school (52–54). Only 6 interviewees in this study provided specific and strong comments on school reentry as having been important for readjustment.
CONCLUSIONS
Rehabilitation of adolescents with SCI might be improved by encouraging staff to acquire knowledge in adolescent medicine to better understand the specific needs and demands of persons of this age. Because parents and peers seem to play an important role, it is suggested that their active participation is facilitated in the joint rehabilitation effort of the young person with a SCI.
Acknowledgments
The authors thank the persons who shared their experiences with us. This study received grants from Stiftelsen Tekniska Hjälpmedel a °t Handikappade, the Cancer and Traffic Injury Fund, the LSR Foundation, the Folke Bernadotte Foundation, and the Mid Sweden Research and Development Center, Vasternorrland County Council.
REFERENCES
- Neinstein LS. Adolescent Health Care, A Practical Guide. 4th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2002. [Google Scholar]
- Hofmann AD, Greydanus DE. Adolescent Medicine. 3rd ed. Norwalk, CT: Appleton & Lange; 1997. [Google Scholar]
- Christie D, Viner R. Adolescent development. Br Med J. 2005;330:301–304. doi: 10.1136/bmj.330.7486.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg Kelly K. Ungdomsmedicin. Stockholm, Sweden: Liber AB; 1998. [Google Scholar]
- World Health Organization (WHO) Orientation Programme on Adolescent Health for Health-Care Providers. Module B: Meaning of Adolescence: B8. Geneva, Switzerland: WHO Department of Child and Adolescent Health and Development; 2006. [Google Scholar]
- Hofmann AD, Becher RD, Gabriel HP. The Hospitalized Adolescent: A Guide to Managing the Ill and Injured Youth. New York: Free Press; 1976. [Google Scholar]
- Hofmann AD. Chronic illness and hospitalization. In: Hofmann AD, Greydanus DE, editors. Adolescent Medicine. Stamford, CT: Appleton & Lange; 1997. pp. 740–754. [Google Scholar]
- Vogel LC, Hickey KY, Klaas SY, Anderson CJ. Unique issues in pediatric spinal cord injury. Orthop Nurs. 2004;23:300–308. doi: 10.1097/00006416-200409000-00004. [DOI] [PubMed] [Google Scholar]
- Stein R, Jessop D. A non-categorical approach to chronic childhood illness. Public Health Rep. 1982;97:354–362. [PMC free article] [PubMed] [Google Scholar]
- Suris JC. Chronically ill but still adolescent. Minerva Pediatr. 2002;54:507–510. [PubMed] [Google Scholar]
- Suris JC, Michaud PA, Viner R. The adolescent with a chronic condition. Part I: developmental issues. Arch Dis Child. 2004;89:938–942. doi: 10.1136/adc.2003.045369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaud PA, Suris JC, Viner R. The adolescent with a chronic condition. Part II: healthcare provision. Arch Dis Child. 2004;89:943–949. doi: 10.1136/adc.2003.045377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodgate RL. Health professionals caring for chronically ill adolescents: adolescents' perspectives. J Soc Pediatr Nurs. 1998;3:57–68. doi: 10.1111/j.1744-6155.1998.tb00029.x. [DOI] [PubMed] [Google Scholar]
- Woodgate RL. Adolescents' perspectives of chronic illness: “it's hard”. J Pediatr Nurs. 1998;13:210–223. doi: 10.1016/S0882-5963(98)80048-1. [DOI] [PubMed] [Google Scholar]
- Coupey S, Neinstein L, Zeltzer L. Chronic illness in the adolescent. In: Neinstein LS, editor. Adolescent Health Care A Practical Guide. Philadelphia, PA: Lippincott Williams & Wilkins; 2002. pp. 1511–1536.pp. 1634 [Google Scholar]
- Kyngas H, Hentinen M, Barlow JH. Adolescents' perceptions of physicians, nurses, parents and friends: help or hindrance in compliance with diabetes self-care? J Adv Nurs. 1998;27:760–769. doi: 10.1046/j.1365-2648.1998.00608.x. [DOI] [PubMed] [Google Scholar]
- Kyngas H. Compliance of adolescents with chronic disease. J Clin Nurs. 2000;9:549–556. doi: 10.1046/j.1365-2702.2000.00368.x. [DOI] [PubMed] [Google Scholar]
- Kyngas H. Support network of adolescents with chronic disease: adolescents' perspective. Nurs Health Sci. 2004;6:287–293. doi: 10.1111/j.1442-2018.2004.00207.x. [DOI] [PubMed] [Google Scholar]
- Woodgate RL. A different way of being: adolescents' experiences with cancer. Cancer Nurs. 2005;28:8–15. doi: 10.1097/00002820-200501000-00002. [DOI] [PubMed] [Google Scholar]
- Kendall L, Sloper P, Lewan RY, Parsons YM. The views of young people with congenital cardiac disease on designing the services for their treatment. Cardiol Young. 2003;13:11–19. doi: 10.1017/s1047951103000040. [DOI] [PubMed] [Google Scholar]
- Decker CL. Social support and adolescent cancer survivors: a review of the literature. Psychooncology. 2006;16:1–11. doi: 10.1002/pon.1073. [DOI] [PubMed] [Google Scholar]
- Anderson CJ. Pediatric-onset spinal cord injury: psychosocial issues. SCI Nurs. 2003;20:212–214. [PubMed] [Google Scholar]
- Flett PJ. The rehabilitation of children with spinal cord injury. J Paediatr Child Health. 1992;28:141–146. doi: 10.1111/j.1440-1754.1992.tb02629.x. [DOI] [PubMed] [Google Scholar]
- Merenda L. The pediatric patient with SCI—not a small adult! SCI Nurs. 2001;18:43–44. [PubMed] [Google Scholar]
- Mulcahey MJ. Unique management needs of pediatric spinal cord injury patients: rehabilitation. J Spinal Cord Med. 1997;20:25–30. [PubMed] [Google Scholar]
- Parnell M. When a child is physically disabled: impact on the child and the family. SCI Psychosoc Proc. 1991;4:16–21. [Google Scholar]
- Rutledge D, Dick G. Spinal cord in adolescence. Rehabil Nurs. 1983;8:18–21. doi: 10.1002/j.2048-7940.1983.tb02478.x. [DOI] [PubMed] [Google Scholar]
- Massagli T, Jaffe K. Pediatric spinal cord injury: treatment and outcome. Pediatrician. 1990;17:244–254. [PubMed] [Google Scholar]
- Vogel L. Unique management needs of pediatric spinal cord injury patients: etiology and pathophysiology. J Spinal Cord Med. 1997;20:10–13. [PubMed] [Google Scholar]
- Vogel LC, Anderson CJ. Spinal cord injuries in children and adolescents: a review. J Spinal Cord Med. 2003;26:193–203. doi: 10.1080/10790268.2003.11753682. [DOI] [PubMed] [Google Scholar]
- Geller B, Greydanus DE. Psychological management of acute paraplegia in adolescence. Pediatrics. 1979;63:562–564. [PubMed] [Google Scholar]
- Anderson CJ, Krajci KA, Vogel LC. Life satisfaction in adults with pediatric-onset spinal cord injuries. J Spinal Cord Med. 2002;25:184–190. doi: 10.1080/10790268.2002.11753620. [DOI] [PubMed] [Google Scholar]
- Anderson CJ, Vogel LC. Domain-specific satisfaction in adults with pediatric-onset spinal cord injuries. Spinal Cord. 2003;41:684–691. doi: 10.1038/sj.sc.3101533. [DOI] [PubMed] [Google Scholar]
- Kannisto M. Pediatric Spinal Cord Injury, Years After the Lesions. Hospital for Children and Adolescents [PhD thesis] Helsinki, Finland: University of Helsinki, Finland; 1999. [Google Scholar]
- Kennedy P, Gorsuch N, Marsh N. Childhood onset of spinal cord injury: self-esteem and self-perception. Br J Clin Psychol. 1995;34:581–588. doi: 10.1111/j.2044-8260.1995.tb01492.x. [DOI] [PubMed] [Google Scholar]
- Anderson CJ, Johnson KA, Klaas SJ, Vogel LC. Pediatric spinal cord injury: transition to adulthood. J Vocational Rehabil. 1998;10:103–113. [Google Scholar]
- Anderson CJ, Vogel LC, Betz RR, Willis KM. Overview of adult outcomes in pediatric-onset spinal cord injuries: implications for transition to adulthood. J Spinal Cord Med. 2004;27(Suppl 1):S98–S106. doi: 10.1080/10790268.2004.11753545. [DOI] [PubMed] [Google Scholar]
- Anderson CJ, Vogel LC, Willis KM, Betz RR. Stability of transition to adulthood among individuals with pediatric-onset spinal cord injuries. J Spinal Cord Med. 2006;29:46–56. doi: 10.1080/10790268.2006.11753856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hokkanen H, Erikssen E, Ahonen O, Salentera S. Adolescents with cancer: experience of life and how it could be made easier. Cancer Nurs. 2004;27:325–335. doi: 10.1097/00002820-200407000-00010. [DOI] [PubMed] [Google Scholar]
- Patton Q. Qualitative Evaluation and Research Methods. 2nd. ed. Newbury Park, CA: Sage Publications; 1990. [Google Scholar]
- Augutis M, Levi R. Pediatric spinal cord injury in Sweden: incidence, etiology and outcome. Spinal Cord. 2003;41:328–336. doi: 10.1038/sj.sc.3101478. [DOI] [PubMed] [Google Scholar]
- Marino RJ, Barros T, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003;26:S50–56. doi: 10.1080/10790268.2003.11754575. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. Qualitative analysis: what it is and how to begin. Res Nurs Health. 1995;18:371–375. doi: 10.1002/nur.4770180411. [DOI] [PubMed] [Google Scholar]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Augutis M, Abel R, Levi R. Pediatric spinal cord injury in a subset of European countries. Spinal Cord. 2006;44:106–112. doi: 10.1038/sj.sc.3101793. [DOI] [PubMed] [Google Scholar]
- Radzik M, Sherer S, Neinstein LS. Psychosocial development in normal adolescents. In: Neinstein LS, editor. Adolescent Health Care, A Practical Guide. Philadelphia, PA: Lippincott, Williams & Wilkins; 2002. pp. 52–58. [Google Scholar]
- Westgren N, Hultling C, Levi R, Seiger A, Westgren M. Sexuality in women with traumatic spinal cord injury. Acta Obstet Gynecol Scand. 1997;76:977–983. doi: 10.3109/00016349709034913. [DOI] [PubMed] [Google Scholar]
- Ungar M. The importance of parents and other caregivers to the resilience of high-risk adolescents. Fam Proc. 2004;43:23–41. doi: 10.1111/j.1545-5300.2004.04301004.x. [DOI] [PubMed] [Google Scholar]
- Wolfe D, Mash E. Behavioral and Emotional Disorders in Adolescents. Nature, Assessment, and Treatment. New York: The Guilford Press; 2006. [Google Scholar]
- Carpenter C. The experience of spinal cord injury: the individual's perspective-implications for rehabilitation practice. Phys Ther. 1994;74:614–628. doi: 10.1093/ptj/74.7.614. [DOI] [PubMed] [Google Scholar]
- Wahman K, Biguet G, Levi R. What promotes physical activity after spinal cord injury? An interview study from a patient perspective. Disabil Rehabil. 2006;28:481–488. doi: 10.1080/09638280500211932. [DOI] [PubMed] [Google Scholar]
- Sandford P, Falk-Palec D, Spears K. Return to school after spinal cord injury. Arch Phys Med Rehabil. 1999;80:885–888. doi: 10.1016/s0003-9993(99)90078-3. [DOI] [PubMed] [Google Scholar]
- Mulcahey MJ. Returning to school after a spinal cord injury: perspectives from four adolescents. Am J Occup Ther. 1992;46:305–312. doi: 10.5014/ajot.46.4.305. [DOI] [PubMed] [Google Scholar]
- Graham P, Weingarden S, Murphy P. School reintegration: a rehabilitation goal for spinal cord injured adolescents. Rehabil Nurs. 1991;16:122–127. doi: 10.1002/j.2048-7940.1991.tb01196.x. [DOI] [PubMed] [Google Scholar]