Abstract
Background/Objective:
Determine the effects of a nutrition education and exercise intervention on the health and fitness of adolescents with mobility impairment due to spinal cord dysfunction from myelomeningocele and spinal cord injury. Subjects participated in a 16-week intervention consisting of a behavioral approach to lifestyle change, exercise, and nutrition education to improve fitness (BENEfit) program. Participants were given a schedule of aerobic and strengthening exercises and attended nutrition education and behavior modification sessions every other week along with their parent(s).
Subjects:
Twenty adolescents (aged 11–18 years, mean 15.4 ± 2.2 years) with spinal cord dysfunction.
Methods:
Subjects were tested immediately prior to starting and upon completion of the program. Aerobic fitness was measured using a ramp protocol with an arm ergometer. Heart rate and oxygen uptake were measured. Values at anaerobic threshold and maximum oxygen uptake were recorded. Peak isokinetic arm and shoulder strength were determined with a dynamometer. Body composition was estimated with dual-energy x-ray absorptiometry. Serum chemistry included measures of cholesterol, high-density lipoprotein, low-density lipoprotein, and triglycerides.
Results:
Fourteen individuals completed all testing sessions. There was no significant overall change in weight, body mass index, body mass index z-scores, or serum chemistry. Overall, there was a significant increase in whole body lean tissue without a concomitant increase in whole body fat. Fitness measures revealed a significant increase in maximum power output, work efficiency as measured by the amount of power output produced aerobically, and resting oxygen uptake. Strength measurements revealed a significant increase in shoulder extension strength and a trend towards increased shoulder flexion strength. There were no significant changes in high-density lipoprotein, low-density lipoprotein, total cholesterol, or triglycerides.
Conclusions:
The BENEfit program shows promise as a method for improving the health and fitness of adolescents with mobility impairments who are at high risk for obesity and obesity-related health conditions.
Keywords: Spinal cord injuries, Adolescence, Disability, Rehabilitation, Myelomeningocele, Spina bifida, Nutrition, Obesity, Paraplegia, Quality of life, Exercise, Body composition, Weight control
INTRODUCTION
According to the Healthy Children 2010 Report, people with disabilities are less likely than able-bodied individuals to participate in sustained exercise (1,2). Children with chronic diseases are among the least active subgroup of children and are at additional risk of a variety of health conditions associated with a sedentary lifestyle (3,4). Due to loss of motor function, adolescents with myelomenin-gocele (MM) and spinal cord injury (SCI) are restricted in the performance of their normal everyday activities, which leads to an increasingly sedentary life style. This, in turn, leads to a decrease in physical fitness and an increase in body fat. Deficits in lean muscle tissue in children with motor impairments are associated with a high prevalence of obesity and suboptimal physical fitness.
The prevalence of adolescents who are overweight or obese increased from 56% in 1988 to 1994 to 65% in 1999 to 2000; obesity is 2.5 times more evident among individuals with lower extremity disabilities than among those without any disability (5,6). Obesity can exacerbate problems associated with disability, such as limited ambulation, difficulty in transferring, risk of pressure sores, psychological morbidity, and possible complications during surgery. Several studies have found that risk of morbidity from coronary disease and atherosclerosis was increased among men and women who had been overweight adolescents (7–9).
Recent scientific information suggests that the most effective interventions to address excess weight and obesity in children should include behavioral modification and education to improve eating habits and increase energy expenditure (10–14). “Shapedown” is a program developed by the University of California, San Francisco, School of Medicine that was designed to address some underlying psychosocial correlates of the child or adolescent's weight (10). It is a family-based program that incorporates family therapy and psychoeducational techniques to enhance self-esteem, improve peer relationships, and adopt healthier habits (10). Similar programs from the University of California, Davis, called “Fit Kids” (for children aged 6–10 years) and “Fit Teens” (for children aged ≥10 years) employ a 10-week behavior modification program to develop a healthy lifestyle. A child or teenager and his/her parents participate in a variety of “hands-on” activities every week that address nutrition, exercise, and psychosocial habits. In addition, daily and weekly goals are used to reinforce positive lifestyle changes.
Although many of the concepts in these programs, specifically those related to nutrition and portion sizes, are applicable to all individuals, few of them address the special nutritional needs of individuals with mobility impairment or their barriers to physical activity (15). One program that is designed for adults with SCI, Shake-It-Up by Block et al (11), consists of weekly classes covering nutrition, physical activity, lifestyle management, and behavior modification. But the lessons and materials developed have been shown to be inappropriate for adolescents with disabilities. Of the references to programs designed for children or adolescents, only a few have addressed the special health, nutrition, and fitness needs of children and adolescents with mobility impairment (15–17).
In response to this glaring need, we developed a pilot intervention referred to as the BENEfit program (behavioral approach to exercise and nutrition education to improve fitness) designed specifically to improve the health and fitness of children with mobility impairment by using nutrition and exercise education and aerobic and strengthening exercises, along with behavior modification. The program consisted of 9 biweekly sessions covering 16 weeks with alternating topics of exercise education and nutrition concepts. Participants were given a schedule of aerobic and strengthening exercises and attended nutrition education and behavior modification sessions every other week along with their parent(s). We sought to determine whether the health promotion activities conducted through the BENEfit program would reduce weight, improve body composition characteristics (increase lean muscle tissue and/or reduce fat tissue), increase strength, increase fitness, and improve nutritional understanding and food choice habits. The effects of the program were evaluated by measuring changes in body composition by dual-energy x-ray absorptiometry (DXA), changes in isokinetic strength, and changes in aerobic fitness.
METHODS
Subjects
A total of 20 adolescents (aged 11–18 years, mean age 15.4 ± 2.2 years) were recruited from MM and SCI clinics at the Shriners Hospital for Children Northern California. All subjects and their parents provided written assent and consent. Eight individuals were enrolled in the first pilot session and 12 in the second. All of the subjects had mobility impairments due to spinal cord dysfunction (MM or SCI). Fifteen subjects used a wheelchair for mobility, 1 subject used a wheelchair for some mobility needs, and 4 subjects were fully ambulatory but had impaired gait that excluded them from mainstream physical activities.
Tests
Anthropometrics, strength, aerobic fitness, and serum chemistry tests were conducted during the pre- and post-test assessments.
Anthropometrics. For all subjects able to stand erect, height was measured to the nearest centimeter with a wall-mounted stadiometer. For subjects unable to stand erect, stature was measured with a supine stadiometer. Every effort was made to account for any contractures. Weight was obtained to the nearest kilogram with a wheelchair balance scale (Detecto, St Louis MO). Body composition was obtained with DXA (Hologic QDR 4500, Hologic, MA).
Strength. Peak dynamic strength values were obtained with a LIDO Dynamometer (Loredan Biomedical, Davis, CA). For shoulder flexion and extension, the subjects sat on a chair with their feet flat on the floor, wrists in neutral position, and elbows in full extension. Subjects who used wheelchairs sat in their wheelchair with feet supported on the footrests and with the wheels locked. Range of motion was from 90° flexion (arm pointed forward at shoulder height) to 180° flexion (arm pointed straight up). For elbow flexion and extension, subjects were supine with the upper arm in approximately 45° of abduction. Range of motion was from 0° (fully extended) to 90° of elbow flexion. Subjects performed 3 maximum extensions and 3 maximum flexions for each elbow and shoulder. The peak value for torque was calculated as the mean peak value between the right and left arms and recorded in Newton meters.
Aerobic Fitness. Values for resting heart rate (HRrest) and oxygen uptake at rest (Vo2rest) were obtained after the subjects were seated quietly for 3 minutes. These values were obtained while the subjects were seated in order to best represent the functional aerobic capacity starting values for exercise. It has been shown that some individuals with spinal cord dysfunction exhibit an increased HR and Vo2 while lying (18), so that any increase in these values due to exercise performed while seated may misrepresent the relative effort of the exercise.
There are no prediction equations available to estimate values for maximum oxygen uptake (Vo2max), anaerobic threshold (AT), or maximum heart rate (HRmax) (19,20) in adolescents with disabilities using upper extremity exercise. Therefore, peak oxygen uptake (Vo2peak), AT, and peak heart rate (HRpeak) were determined for each subject by arm crank ergometry using a standard ramp protocol on a magnetically braked arm ergometer (Lode, The Netherlands). Subjects were asked to crank the arm ergometer at a constant speed of 70 rpm for 2 minutes at 0 watts of resistance. The resistance was then increased in a ramp fashion at a rate of 10 watts/minute. Subjects were verbally encouraged to continue until exhaustion. Heart rate, Vo2, carbon dioxide production (Co2), and power output (PO) were recorded breath-by-breath with a metabolic cart (Medgraphics, St Paul, MN) using a facemask. The values obtained for Vo2peak and HRpeak were used as proxy measures for Vo2max and HRmax. Additionally, POmax was recorded.
Serum Chemistry. After a fast greater than 12 hours, 15 mL of blood was obtained and analyzed for total cholesterol, high-density lipoprotein, low-density lipoprotein, and triglycerides.
BENEfit Program
The structure of the BENEfit session was modeled after the Shapedown program and included an interactive lecture on a specific nutrition or exercise concept followed by an activity designed to reinforce the concept in a visual or tactile mode. During the activity, the parents/guardians participated in a moderated discussion group and discussed such topics as problem-solving, support, stress management, and behavior change strategies. Games, rewards, and motivational tools were used to promote active participation in the nutrition and exercise curriculum. The activities were focused on practical and fun ways for subjects to achieve lifetime exercise benefits.
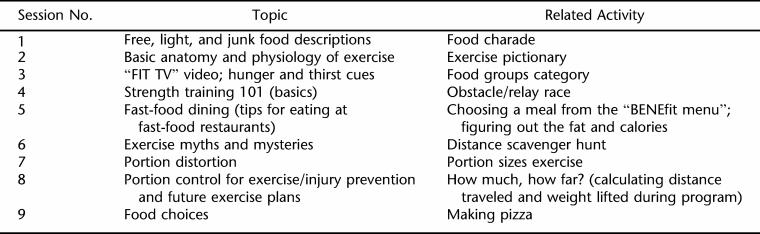
The first half of the nutrition class was designed to discuss the topics covered (Table 1), and the second half of the nutrition class encouraged active participation to emphasize the lesson. The first lesson taught participants to put food into each category: free, light, and junk. The second nutrition topic highlighted the importance of physical activity in the “FIT TV” video and of learning to identify hunger and thirst cues. The third lesson involved teaching participants how to be aware of the nutritional intake when dining out The participants were taught “buzz words” that help them decide whether a particular type of food is healthy and how to reduce their intake of high-caloric and high-fat foods, such as sauces, gravy, and dressings. The exercise for this lesson asked participants to choose from “BENEfit Menu,” which has both high/low calories and fat choices, and to figure out their total calories and fat for that meal. The fourth lesson educated subjects on appropriate portion control by using visuals, such as food models and props. Subjects were asked to portion out pasta, cereal, meat, and drink during the portion-distortion exercise and compare these to the food models. The last lesson was designed to incorporate all the lessons learned previously by using an activity of “creating your own pizza.” Participants were instructed to create their own pizzas and calculate the amount of fat and calories based on the items placed on the pizza and the type of pizza they made.
Table 1.
BENEfit Class Topics and the Order in Which They Were Presented
All participants were required to keep daily food records and complete nutrition assignments each week. The nutrition classes were intended to increase the knowledge of general nutrition on healthful eating, provide skills necessary to change eating behaviors, and help set realistic measurable and attainable dietary goals. The exercise topics covered basic anatomical and physiological benefits, exercise components (aerobic vs resistive), exercise myths, precautions, and injury prevention. Lessons were designed to be interactive and involve the subjects in discussions about their knowledge and attitudes regarding exercise. Subjects were also encouraged to share their experiences from the previous weeks in completing their BENEfit exercise program. During the second half of the session, activity-based group tasks were designed to reinforce the lesson.
In addition to the group sessions, participants completed an in-home exercise program of aerobic and resistance training components designed to improve their strength and cardiovascular health. The aerobic training program involved use of an arm ergometer connected to a video game (GameCycle, Three Rivers, Mesa, AZ). The games were delivered to the subjects' homes for use during the study. During the pretest session, the initial resistance level of the game was determined for each subject. After the AT was calculated from the arm crank ergometry, each subject was asked to crank the video game without the game playing for 1 minute at each resistance level while HR and Vo2 were recorded. The resistance level that elicited the HR and Vo2 just below the subject's AT was designated as the starting resistance level. The HR associated with the subject's AT was designated as the target heart rate. During the game play, the subjects wore heart monitors and were told to maintain their heart rates at that predetermined heart rate.
The resistance training program consisted of upper extremity strengthening exercises using hand weights (dumbbells). The exercises were selected according to previous studies describing primary muscles involved in wheelchair propulsion and functional activities in wheelchair-using patients (21–25). The specific exercises were demonstrated during the initial BENEfit session and on an instructional video provided to each subject. The starting weight for each movement was determined by using the nearest lesser weight from the 6-repetition maximum level. Subjects were given the weights to take home and perform the exercise program.
Subjects were instructed to perform aerobic and resistance programs 3 days a week with alternating days for each program. A 5-minute warm-up period was followed by a 5-minute stretch period prior to beginning either program. Each program also involved a 5-minute cool-down period at the end of the exercise session. Resistance training was done at 3 sets of 10 repetitions with a 1-minute rest between sets. Aerobic sessions started with 10 minutes per session for the first 2 weeks, increasing by 5 minutes every 2 weeks.
Subjects recorded daily exercise and perceived levels of exertion on a progress record. The record included weights used, duration, and a 0 to 10 exertion scale. The exertion scale included descriptive terms and the Wong-Baker faces (26) (as a graphic representation of effort) associated with each numerical value. Subjects recorded the score that most closely described how they felt at the end of each exercise.
For the aerobic program, the number of minutes performed and the level of exertion were recorded. For the resistance program, the weight used for each exercise was recorded along with the exertion scale score. An exertion score of 5 to 7 was the desired range and used as a guideline for changing resistance. Weights from 1 to 10 pounds were changed in 2-pound increments, while weights more than 10 pounds were modified in 5-pound increments. The progress sheets were also used as compliance monitoring for exercise participation. The progress logs for both programs were reviewed at each of the 16 biweekly BENEfit sessions.
During each biweekly session, the physical therapist met individually with each subject and parent to review the program and address any questions. Subjects with recurring noncompliance issues were given short-term goals with rewards for successful completion.
Two separate pilot sessions of the BENEfit program were conducted. The first session began in April 2005 and ended in July 2005; the second session started in July 2005 and ended in November 2005. In both groups, the lessons were conducted on alternate Saturday afternoons at the Shriners Hospital for Children Northern California.
RESULTS
Compliance
Twenty adolescents were enrolled into the program, and 14 subjects completed both the pre- and the post-BENEfit assessments. There were no significant differences in age, weight, height, percent fat, or body mass index (BMI) percentile for age between the 6 subjects who dropped out of the study and the 14 subjects who remained in the study. However, a proportionately higher percentage of girls dropped out of the study (5 of 6) compared with the number who completed the whole study (7 of 14). There were various reasons for not completing the study. Three of the girls with spina bifida did not return for the post-test, despite numerous phone calls and prodding by the staff. One girl with spina bifida had a pressure sore that prevented her from continuing the study. One girl with SCI dropped out after the second session because she was not comfortable being in this group of adolescents. One boy with SCI dropped out because his parent had a time conflict after the third session that prevented him from continuing the program. All who dropped out came from the second group. In the first group, all 8 subjects completed the pre- and post-tests and attended at least 7 of the 9 sessions. However, only 6 of the 12 subjects from the second group completed the pre- and post-tests and attended at least 6 sessions.
Body Composition
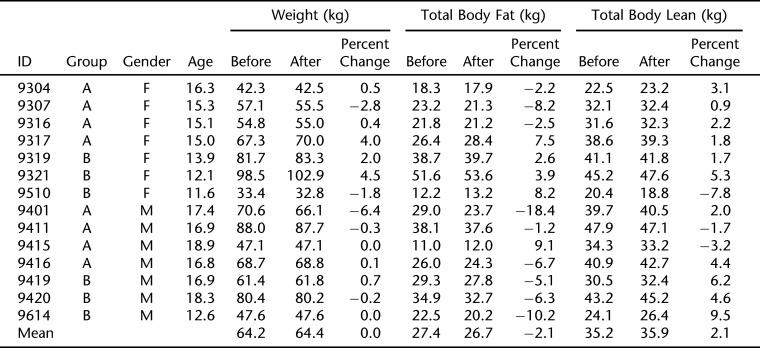
The individual changes in weight, total body fat, and total body lean are shown in Table 2. Overall, the mean body weight did not change significantly (64.2 ± 4.99 kg pre-BENEfit and 64.4 ± 5.2 kg post-BENEfit), nor was there a significant change in BMI from the 29.3 kg/m2 pre-BENEfit level. However, there was a 2.1% increase in total body lean tissue (P = 0.02) with a concomitant, nonsignificant reduction in total body fat tissue (−2.1%). Nine subjects decreased total body fat, and 8 of those 9 also increased lean tissue.
Table 2.
Subjects and Body Composition
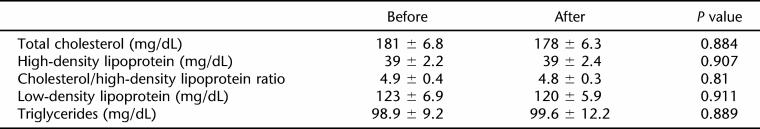
Serum Chemistry
One subject declined to provide a blood sample during the post-test assessment. There were no significant changes in mean values for total cholesterol, high-density lipoprotein, low-density lipoprotein, or triglycerides.
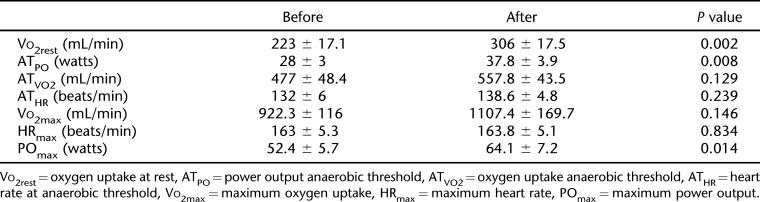
Aerobic Fitness
There was a 27% increase (P < 0.002) in Vo2rest, reflecting the increase in lean tissue. There was no significant change in Vo2max before and after the BENEfit program. However, the Pomax, which represents work capacity, increased 22% (P = 0.014). There was also a 35% increase in the aerobic efficiency as measured by the power output at the anaerobic threshold (POAT). There was no difference in HRmax achieved, which would indicate that the subjects gave maximal effort during both the pre-and the post-test.
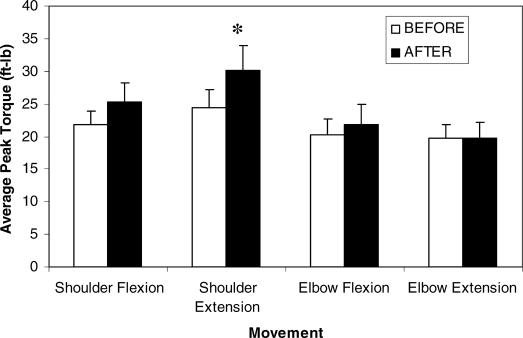
Strength
Most of the subjects improved their shoulder strength, with a 23% increase in peak shoulder extension (P = 0.016) (Figure 1). For the group, shoulder flexion strength increased by more than 15% but was not significantly greater than the pre-BENEfit assessment (P = 0.056). Elbow flexion and extension strength did not increase significantly.
Figure 1. Peak strength changes before and after the behavioral approach to lifestyle change, exercise, and nutrition education to improve fitness (BENEfit) program.
DISCUSSION
The purpose of this study was to develop a model program that utilized nutritional education and behavior modification to develop healthy lifestyles that would help overweight and obese children with mobility impairments increase their strength and physical activity and adopt a healthy diet. After the program, the subjects exhibited no significant increase in weight or total body fat but had a significant increase in lean tissue, shoulder strength, and aerobic fitness. This program emphasized increased physical activity, healthful eating, and appropriate portions for age and did not focus on restricting caloric intake. Thus, we did not expect to observe significant reductions in weight and/or BMI as a result of their participation in the BENEfit program. However, as a group, the subjects did not increase their weight significantly (+0.2 ± 0.2 kg) during the 16-week program. This could be viewed as an improvement, because children and adolescents at a comparable age and BMI would have been expected to gain approximately 1.5 kg during this 16-week period due to growth alone. In addition, the DXA results revealed a significant increase in total lean tissue, without a concomitant increase in total fat tissue.
However, this improvement in body composition was not reflected in BMI because BMI is a much less sensitive measure of adiposity than DXA and is much more prone to error. Several studies have showed that BMI is an insensitive measure of body composition in subjects with paraplegia due to problems in measuring weight and height (27–29). In addition, BMI does not appropriately account for regional losses of lean tissue and redistribution of lean and fat tissue in children with paraplegia (30).
The subjects exhibited an increase in shoulder strength but no increase in elbow strength, which suggests that the increase in strength was not just due to their increased age and growth. The changes in strength were likely attributed to the aerobic exercise and weight training's working the shoulder extensors and flexors to a greater extent than the biceps or triceps. Increasing shoulder strength has been shown effective at reducing the high incidence of shoulder pain and shoulder impingement syndrome among wheelchair users because of the repetitive nature of wheelchair locomotion injuries (25,31). Future research should focus on identifying functional limitations as applied to strength deficits. A correlation between gains in strength and increased independence in performance of activities of daily living might increase compliance and long-term follow through of concepts taught during the BENEfit program.
The subjects who participated in this study also had a 27% increase (P < 0.002) in VO2rest, which reflects an overall increase in lean tissue. Subjects who participated in the BENEfit training also had a 22% increase in work capacity and a 35% increase in the aerobic efficiency. These changes in aerobic fitness should allow the subjects to perform more work and may help their independence.
Despite the improvements in body composition, strength, and aerobic fitness, there were no significant improvements in serum lipids. This probably reflects that the program only provided nutrition education and did not require the participants to restrict their caloric intake. Our program's goal for the diet and nutrition was mainly to encourage healthful eating and offer participants useful tools to help them make the appropriate choice of food selection and portion sizes appropriate for age and diagnosis. Future programs may be able to affect this more by implementing a more aggressive program of reducing caloric and fat intake. However, because severe calorie restriction programs have been shown to induce a cycle of weight loss followed by weight gain (32,33), the focus of BENEfit was to gradually introduce sustainable changes in food choices that would, over time, lead to positive changes in health.
Subjects who had excellent family support appeared to be more successful in long-term weight loss maintenance (34). Social integration can have a positive effect on self-esteem by increasing an individual's social and emotional support. This was apparent in our participants, who became friends and exchanged phone numbers and email addresses at the end of the intervention. The impact of a family history of overweight on weight loss suggests the influences of genetic predisposition and poor food choices on body weight and weight loss maintenance. Having the support of family and friends is typically one of the most fundamental aspects of successfully coping with behavior changes. The support can take many forms: emotional (someone to talk to and share feelings with), practical (someone to help with food choices or act as a reminder), and spiritual (someone to help answer the big questions that surface when facing discouragement). It can provide the encouragement needed for individuals to get out and exercise on days when watching their favorite TV show seems like a better option. People who have the support of friends/family are less likely to drop out of a weight-control program and are more likely to maintain their weight loss over a 6-month period than people without such support (35). Many of our participants who did extremely well had one thing in common: excellent support of family and friends.
The first group had a better attendance record than the second group. The instructors reported that, as a group, they were more homogenous in terms of intellectual functioning, social skills, physical abilities, and family structure. The second group had a wide range of age (11–18 years), intellectual abilities, and physical functional level. One individual (16 years old) who dropped out after the second lesson had a fairly recent (2 years) SCI and reported being very uncomfortable in a group that included individuals who not only were younger but also had significant developmental delays. Surprisingly, the distance each individual traveled to the sessions did not have a significant influence on attendance. In fact, some of the individuals who had near-perfect attendance had to travel more than 2 hours one way to attend the lessons, and some of the subjects who dropped from the program lived less than 30 minutes from the meeting location. Despite the transportation barriers and time commitments of the program, it was evident from the participants and their parents' evaluations that the BENEfit program, as designed and implemented in this pilot study, was thought to be extremely useful, fun, and easy to understand. They would have no hesitation in recommending the program to others.
In addition to the improvement in body composition that occurred during the study, approximately 80% of the subjects learned and adopted healthier eating habits and maintained or lost weight when seen back in the outpatient clinic 3 to 6 months after intervention (R. A. L., personal observation). During these follow-up visits, parents and participants were able to identify the appropriate portions, as well as recognize foods that were high in calories and fat.
The limitation of our program includes lack of a control or comparison group, nonrandomized design, small sample size, and the short timeframe. The small sample size may have reduced the statistical power, and the short timeframe made it unlikely that measurable changes would be evident. In fact, the subject who gained 10 kg during the study continued to gain weight in the clinic and was later diagnosed with abnormal thyroid function, which added to the heterogeneity of the sample. By increasing sample sizes, replications of this study would benefit by focusing on subjects with the same disease and age to enhance the homogeneity of the test subjects.
CONCLUSIONS
A 16-week intervention consisting of a BENEfit program increased the strength and improved the aerobic capacity and endurance of overweight and obese children with mobility impairments and helped them adopt a healthy diet. Although there were no significant changes in the weight and BMI measures for our subjects, there were improvements in body composition, including an increase in total lean tissue and no increase in total fat tissue. The most disappointing result was that there was little to no change in blood lipids, which has been identified as a heavily weighted factor in assessing the risk of cardiovascular disease. Nevertheless, this study presents a model program and provides baseline data that can be used in planning subsequent randomized controlled trials.
Table 3.
Blood Lipids
Table 4.
Aerobic Fitness Measures
Footnotes
Supported in part by Shriners Hospitals for Children Project number 8600: Exercise and Dietary Intervention in Obese Children with Paraparesis Due to Spinal Cord Dysfunction; National Institute of Disability and Rehabilitation Research Grant #H133B031118; Rehabilitation Research and Training Center in Neuromuscular Diseases: Enhancing Health, Function, and Quality of Life; and National Institute of Child Health and Human Development Grant # RO1 HD35714: Child Mobility: Role of Strength, Body Fat and Energy Cost.
REFERENCES
- Healthy Children 2010 . Washington, DC: US Department of Health and Human Services, Office of Disease Prevention and Health Promotion; 2002. [Google Scholar]
- Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: US Dept of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [Google Scholar]
- Dyken EM, Rosner BA, Butterbaugh G. Exercise and sports in children and adolescents with developmental disabilities: positive physical and psychosocial effects. Child Adolesc Psychiatr Clin N Am. 1998;7:757–771. [PubMed] [Google Scholar]
- Durstine JL, Painter P, Franklin BA, et al. Physical activity for the chronically ill and disabled. Sports Med. 2000;30:207–219. doi: 10.2165/00007256-200030030-00005. [DOI] [PubMed] [Google Scholar]
- Troiano RP, Flegal KM, Kuczmarski RJ, Campbell SM, Johnson CL. Overweight prevalence and trends for children and adolescents: the National Health and Nutrition Examination Surveys, 1963 to 1991. Arch Pediatr Adolesc Med. 1995;149:1085–1091. doi: 10.1001/archpedi.1995.02170230039005. [DOI] [PubMed] [Google Scholar]
- Weil E, Wachterman M, McCarthy EP, et al. Obesity among adults with disabling conditions. JAMA. 2002;288:1265–1268. doi: 10.1001/jama.288.10.1265. [DOI] [PubMed] [Google Scholar]
- Bauman WA, Spungen AM. Carbohydrate and lipid metabolism in chronic spinal cord injury. J Spinal Cord Med. 2001;24:266–277. doi: 10.1080/10790268.2001.11753584. [DOI] [PubMed] [Google Scholar]
- Imai K, Kadowaki T, Aizawa Y, Fukutomi K. Morbidity rates of complications in persons with spinal cord injury according to the site of injury and with special reference to hypertension. Paraplegia. 1994;32:246–252. doi: 10.1038/sc.1994.44. [DOI] [PubMed] [Google Scholar]
- Yekutiel M, Brooks ME, Ohry A, Yarom J, Carel R. The prevalence of hypertension, ischaemic heart disease and diabetes in traumatic spinal cord injured patients and amputees. Paraplegia. 1989;27:58–62. doi: 10.1038/sc.1989.9. [DOI] [PubMed] [Google Scholar]
- Mellin LM, Silnkard LA, Irwin CE. Adolescent obesity intervention: validation of the SHAPEDOWN program. J Am Diet Assoc. 1987;87(3):333–338. [PubMed] [Google Scholar]
- Block P, Skeels SE, Keys CB, Rimmer JH. Shake-It-Up: health promotion and capacity building for people with spinal cord injuries and related neurological disabilities. Disabil Rehabil. 2005;27(4):185–190. doi: 10.1080/09638280400019583. [DOI] [PubMed] [Google Scholar]
- Bar-Or O. Obesity: The optimal exercise program. In: Godberg E, editor. Sports and Exercise for Children With Chronic Health Conditions. Champaign, IL: Human Kinetics; 1995. [Google Scholar]
- Bar-Or O, Foreyt J, Bouchard C, et al. Physical activity, genetic, and nutritional considerations in childhood weight management. Med Sci Sports Exerc. 1998;30:2–10. doi: 10.1097/00005768-199801000-00002. [DOI] [PubMed] [Google Scholar]
- Sothern MS, Schumacher H, von Almen TK, Carlisle LK, Udall JN. Committed to Kids: an integrated, four-level approach to weight management in adolescents. J Am Dietet Assoc. 2002;102:S81–S85. doi: 10.1016/s0002-8223(02)90429-3. [DOI] [PubMed] [Google Scholar]
- Taylor WC, Baranowski T, Rohm Young D. Physical activity interventions in low-income, ethnic minority, and populations with disability. Am J Prev Med. 1998;15(4):334–343. doi: 10.1016/s0749-3797(98)00081-6. [DOI] [PubMed] [Google Scholar]
- Andrade CK, Kramer J, Garber M, Longmuir P. Changes in self-concept, cardiovascular endurance and muscular strength of children with spina bifida aged 8 to 13 years in response to a 10-week physical-activity programme: a pilot study. Child Care Health Dev. 1991;17:183–196. doi: 10.1111/j.1365-2214.1991.tb00689.x. [DOI] [PubMed] [Google Scholar]
- Ekblom B, Lundberg A. Effect of physical training on adolescents with severe motor handicaps. Acta Paediatr Scand. 1968;57:17–23. doi: 10.1111/j.1651-2227.1968.tb07280.x. [DOI] [PubMed] [Google Scholar]
- Janssen TW, van Oers CA, van der Woude LH, Hollander AP. Physical strain in daily life of wheelchair users with spinal cord injuries. Med Sci Sports Exerc. 1994;26(6):661–670. doi: 10.1249/00005768-199406000-00002. [DOI] [PubMed] [Google Scholar]
- Armstrong N, Welsman JR. Peak oxygen uptake in relation to growth and maturation in 11- to 17-year-old humans. Eur J Appl Physiol. 2001;85(6):546–551. doi: 10.1007/s004210100485. [DOI] [PubMed] [Google Scholar]
- Hui SS, Chan JW. The relationship between heart rate reserve and oxygen uptake reserve in children and adolescents. Res Q Exerc Sports. 2006;77(1):41–49. doi: 10.1080/02701367.2006.10599330. [DOI] [PubMed] [Google Scholar]
- American College of Sports Medicine position stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness in healthy adults. Med Sci Sports Exerc. 1990;22:265–274. [PubMed] [Google Scholar]
- Lockette KF, Keyes AM. Conditioning With Physical Disabilities. Champaign, IL: Human Kinetics; 1994. [Google Scholar]
- Glaser RM. Arm exercise training for wheelchair users. Med Sci Sports Exerc. 1989;21:S149–S157. [PubMed] [Google Scholar]
- Davis GM, Shephard RJ. Strength training for wheelchair users. Br J Sports Med. 1990;24:25–30. doi: 10.1136/bjsm.24.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulroy SJ, Gronley JK, Newsam DJ, Perry J. Electromyo-graphic activity of shoulder muscles during wheelchair propulsion by paraplegic persons. Arch Phys Med Rehabil. 1996;77:187–193. doi: 10.1016/s0003-9993(96)90166-5. [DOI] [PubMed] [Google Scholar]
- Wong D, Baker C. Pain in children: comparison of assessment scales. Pediatr Nurs. 1988;14(1):9–17. [PubMed] [Google Scholar]
- Buchholz AC, Bugaresti JM. A review of body mass index and waist circumference as markers of obesity and coronary heart disease risk in persons with chronic spinal cord injury. Spinal Cord. 2005;43(9):513–518. doi: 10.1038/sj.sc.3101744. [DOI] [PubMed] [Google Scholar]
- Spungen AM, Adkins RH, Stewart CA, et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol. 2003;95(6):2398–2407. doi: 10.1152/japplphysiol.00729.2002. [DOI] [PubMed] [Google Scholar]
- Jones LM, Legge M, Goulding A. Healthy body mass index values often underestimate body fat in men with spinal cord injury. Arch Phys Med Rehabil. 2003;84(7):1068–1071. doi: 10.1016/s0003-9993(03)00045-5. [DOI] [PubMed] [Google Scholar]
- McDonald CM, Widman LM, Abresch-Meyer AL. Body mass index and body composition measured by dual-energy x-ray absorptiometry in adolescents with spinal cord injury. J Spinal Cord Med. 2007;30(Suppl):S100–S107. doi: 10.1080/10790268.2007.11754612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabick MB, Kotajarvi BR, An KN. A new method to quantify demand on the upper extremity during manual wheelchair propulsion. Arch Phys Med Rehabil. 2004;85(7):1151–1159. doi: 10.1016/j.apmr.2003.10.024. [DOI] [PubMed] [Google Scholar]
- National Task Force on the Prevention and Treatment of Obesity, National Institutes of Health. Very low-calorie diets. JAMA. 1993;270(8):967–974. [PubMed] [Google Scholar]
- Barlow SE, Trowbridge FL, Klish WJ, Dietz WH. Treatment of child and adolescent obesity: reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002;110(1 pt 2):205–209. [PubMed] [Google Scholar]
- Verheijden MW, Bakx JC, van Weel C, Koelen MA, van Staveren WA. Role of social support in lifestyle-focused weight management interventions. Eur J Clin Nutr. 2005;59(suppl 1):S179–S186. doi: 10.1038/sj.ejcn.1602194. [DOI] [PubMed] [Google Scholar]
- Kelsey K, Earp JAL, Kirkley BG. Is social support beneficial for dietary change? A review of the literature. Fam Community Health. 1997;20:70–82. [Google Scholar]