Abstract
Design:
Retrospective analysis of medical records.
Background/Objectives:
To determine frequency and degree of hypothermic episodes in patients with chronic spinal cord injury (SCI).
Setting:
Veterans Administration Medical Center.
Methods:
Research involved analysis of body temperature records of 50 chronic patients with tetraplegia. All patients were men with a length of injury of 19 ± 6 years. Mean age was 53 ± 15 (SD) years. Data were derived from the computerized patient record database system of the Veterans Administration Medical Center. Results were classified into 3 groups: (a) hypothermia (<95°F), (b) subnormal temperature (<97.7°F), and normal temperatures (97.7°F to 98.4°F). Body temperature was recorded during hospitalization (minimum duration of 30 days) using an oral probe twice a day. Ambient temperature was controlled by a central air-conditioning system and maintained at 72°F to 74°F.
Results:
A total of 867 measurements of body temperature were evaluated; normal temperature was recorded 298 times (35%), subnormal temperature was recorded 544 times (63%), and hypothermia was recorded 25 times (3%). There were 15 patients with 30 hypothermic episodes; subnormal temperature was found in all 50 patients from 1 to 47 times. Regression analysis of age and duration of SCI showed a nonsignificant relationship with body temperature.
Conclusions:
Our data suggest that patients with tetraplegia after SCI have significant dysfunction of thermoregulation associated with frequent episodes of subnormal body temperature in a normal ambient environment. Further studies are needed to evaluate possible consequences of low temperatures on the general health of patients and to develop preventive interventions.
Keywords: Spinal cord injuries, Hypothermia, Thermoregulation, Tetraplegia, Paraplegia
INTRODUCTION
Body temperature in humans is remarkably stable under normal conditions. It is usually measured orally, which accurately reflects the temperature of the blood (1,2. In a large population, normal oral temperature ranges from 36.5°C to 36.9°C or from 97.7°F to 98.4°F (2). Patients with spinal cord injury (SCI) may have abnormal regulation of body temperature or may be less able to respond to changes in the environment. With high-level SCI, the patient may be especially insensitive to changes in heat or cold. The exact mechanism(s) responsible for these abnormalities are uncertain, but they are most likely caused by loss of hypothalamic control, poor vasomotor reactions, or some other unknown factors. A MEDLINE search of the studies on hypothermia after SCI yielded several publications (3–13). Some of these studies evaluated the relationship of superficial and deep control of body temperature (3–5,10,13). Other publications reported a few cases or small case series describing the relationship of hypothermic episodes with different clinical conditions (6–13). However, we were not able to find clinical studies evaluating the extent and frequency of hypothermia in individuals with SCI. The goal of this study was to determine the degree and incidence of hypothermia using a retrospective analysis of medical records of patients with chronic SCI during long-term hospitalization.
METHODS
This study is a retrospective study on body temperature after SCI. The study and informed consent were approved by the Institutional Review Board committee of the Veterans Administration Medical Center (VAMC), Miami, FL.
Subjects
The records of body temperature were evaluated in 50 patients with chronic tetraplegia. All patients were men with tetraplegia and were 24 to 78 years of age (53 ± 15 [SD] years), and the length of injury was 5 to 34 years (19 ± 6 years).
Data
Data were derived from the computerized patient record system of the VAMC, Miami, FL. The results were classified into 3 groups: (a) hypothermia, (b) subnormal temperatures, and (c) normal temperature. Hypothermia was defined as a body temperature less than 95°F (1,14–17). Normal temperature was defined as a temperature of 97.7°F to 98.4°F, and subnormal temperature was defined as a temperature less than 97.7°F and more than 95°F. Data were analyzed by regression analysis for correlation between body temperature with age and time period after SCI. The mean value of all individual measurements was used for statistical analysis.
Temperature Recordings
Body temperature was recorded in all subjects during hospitalization for a period of 30 days. Temperature was obtained using an oral probe using Dinamap Vital Signs Monitor 81 OOT (Criticon, Tampa, FL). Each patient had 2 measurements recorded every day (7:00 to 9:00 AM and 5:00 to 7:00 PM). Nursing personnel were instructed to record temperature before giving any water or medication. Two different shifts of nursing staff were involved in measurements of vital signs. To avoid false-positive low readings, hypothermic readings were remeasured after 5 to 10 minutes. To determine the accuracy of measurements using the same probe, serial recordings (10 repetitions) were obtained in the same patient and in a control subject. The coefficient of variation of measurements was from 0.4% to 0.5%, respectively. Ambient temperature in the unit was controlled by a central air-conditioning system that was maintained in the range of 72 °F to 74°F.
RESULTS
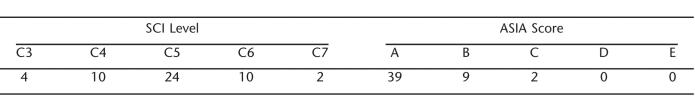
A total of 867 measurements were evaluated and classified in 3 groups as indicated in Figure 1. Subnormal temperatures were recorded 544 times (63%); hypothermia was recorded 25 times (3%), and normal body temperature was recorded 298 times (35%). Hypothermia was more frequently found in the morning than in the afternoon period (18 vs 7 measurements). In the group of patients with hypothermia, 11 were tetraplegic with an American Spinal Injury Association (ASIA) score of A, 3 had an ASIA score of B, and 1 had an ASIA score of C (Table 1). Four patients in this group had more than 1 episode of hypothermia during a 1-month period. Subnormal temperature was found in all 50 patients from 1 to 47 times. Linear regression analysis of data showed no relationship between patient age and mean body temperature (r =−0.064). The relationship between the duration of injury and mean body temperature showed no significant correlation (r = 0.011).
Figure 1. Body temperature readings in 50 hospitalized patients with tetraplegia or paraplegia caused by chronic SCI.
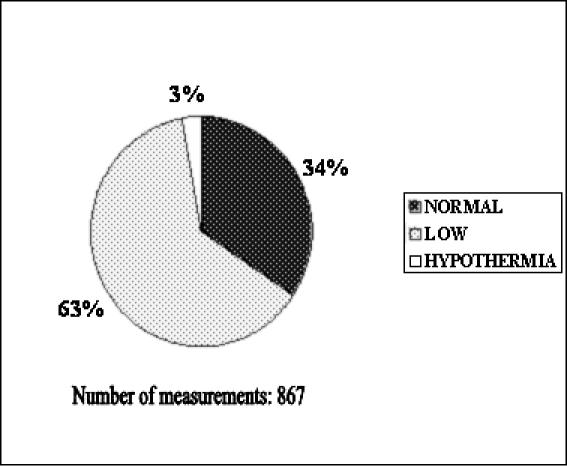
Table 1.
Level of Injury and American Spinal Injury Association (ASIA) Scores of 50 Patients in This Retrospective Study
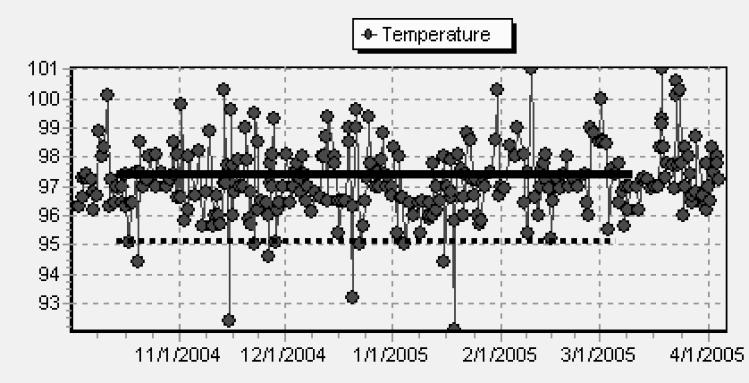
Figure 2 shows a representative graph of body temperature in a patient with tetraplegia. This graph shows measurements obtained over a period of 6 months. The patient had a subnormal recording of temperature more often than normal temperature. The elevations in temperature were associated with acute urinary tract infections.
Figure 2. Recordings of body temperature over a period of 6 months in a 48-year-old man with C4 tetraplegia. Interrupted line indicates temperature that was less than 1 SD of normal temperature (<97.7°F). Solid line indicates temperatures in hypothermic zone (<95°F).
DISCUSSION
Hypothermia is a well-recognized and life-threatening condition associated with increased mortality and morbidity (15–17). Accidental hypothermia is defined as an unintentional decrease of core body temperature to less than 35°C (<95°F). Hypothermia produces effects on many organ systems, resulting in a spectrum of clinical manifestations such as bleeding diathesis (15–18), metabolic acidosis from poor tissue perfusion (15–17), hemodynamic instability with arrhythmias, and depression of myocardial contractility (14). In humans, mechanisms of heat conservation and heat production maintain relatively constant body temperature during exposure to fluctuating ambient temperature. Cold exposure stimulates cold-sensitive receptors present in the skin, leading to a prompt vasoconstriction that preserves heat and stimulates shivering reaction that increases basal metabolic rate and heat production. These homeostatic mechanisms of heat conservation and production fail to function normally after SCI because they require an intact spinal cord and its hypothalamic feedback. With high-level SCI, a very large portion of the skin is insentient; therefore, patients may be especially insensitive to changes in cold and heat. Heat production is significantly diminished and may increase only 10% to 15% in response to a drop in ambient temperature, whereas a similar change of ambient temperature would prompt an increase in heat production from 200% to 500% in an able-bodied person (19).
Our study showed that subnormal body temperature is a very frequent finding in individuals with chronic SCI. In a group of 50 patients followed in the hospital for a period of 30 days, subnormal temperatures were recorded in all patients. Subnormal temperature recordings were twice as common as normal temperatures. In 66% of measurements, body temperature was lower than normal, whereas the remaining 34% of measurements were in the normal range. Critically low temperature in the hypothermic range (<95°F) that required therapeutic intervention was found in 3% of recorded measurements. It was more difficult to discern therapeutic recommendations for subnormal temperatures not reaching the hypothermic level. The majority of patients with subnormal temperature remained asymptomatic, without objective signs of shivering or discomfort. The studies by Downey et al (3,4,19) showed a delayed shivering reaction in individuals with tetraplegia or paraplegia. Individuals with tetraplegia, who have larger areas of insentient skin than their counterparts with paraplegia, started shivering at lower central temperatures. Similarly, paraplegic patients will start to shiver to increase heat production at a lower central temperature (36.4°C) than control subjects (36.8°C) (3,4,19). These inadequate physiologic responses to cold, with delayed adaptation to lower temperature, are most likely responsible for the frequent findings of subnormal body temperature in our patients.
CONCLUSION
Little is known about possible long-term effects of subnormal body temperature on organ systems and metabolism in patients with chronic SCI. Our study does not allow any conclusion on the long-term effects of “cold intolerance” after SCI. We can only speculate that chronic subnormal body temperature in patients with SCI may have some effect on the various abnormalities in metabolic functions that have been well documented after SCI (20–24). Future studies will need to evaluate possible effects of subnormal body temperature on metabolism in chronic SCI.
REFERENCES
- McCullough L, Arora S. Diagnosis and treatment of hypothermia. Am Fam Physician. 2004;70:2325–2332. [PubMed] [Google Scholar]
- Ivy AC. What is normal or normality? Q Bull Northwestern Univ Med School. 1957;18:22–32. [Google Scholar]
- Downey JA, Miller JM, Darling RC. Thermoregulatory responses to deep and superficial cooling in spinal man. J Appl Physiol. 1969;27:209–212. doi: 10.1152/jappl.1969.27.2.209. [DOI] [PubMed] [Google Scholar]
- Downey JA, Chiodi HP, Darling RC. Central temperature regulation in spinal man. J Appl Physiol. 1967;22:91–94. doi: 10.1152/jappl.1967.22.1.91. [DOI] [PubMed] [Google Scholar]
- Seckendorf R, Randall WC. Thermal reflex sweating in normal and paraplegic man. J Appl Physiol. 1961;16:798–800. [Google Scholar]
- Altus P, Hickman JW, Nord HJ. Accidental hypothermia in a healthy quadriplegic patient. Neurology. 1985;35:427–428. doi: 10.1212/wnl.35.3.427. [DOI] [PubMed] [Google Scholar]
- Berard EJJ, Boucand MH, Depasio J, Fyo JP. Effect of bethanechol and adreno-blockers on thermoregulation in spinal cord injury. Paraplegia. 1989;27:46–52. doi: 10.1038/sc.1989.7. [DOI] [PubMed] [Google Scholar]
- Schmidt HD, Chan CW. Thermoregulation and fever in normal persons and those with spinal cord injuries. Mayo Clin Proc. 1992;67:469–475. doi: 10.1016/s0025-6196(12)60394-2. [DOI] [PubMed] [Google Scholar]
- Johnson RH. Temperature regulation in paraplegia. Paraplegia. 1971;9:137–145. doi: 10.1038/sc.1971.24. [DOI] [PubMed] [Google Scholar]
- Claus-Walker J, Halstead LS, Carter RE, Campos RJ, Spencer WA, Canzoneri J. Physiological responses to cold stress in healthy subjects and subjects with cervical cord injuries. Arch Phys Med Rehabil. 1974;55:485–490. [PubMed] [Google Scholar]
- Menard MR, Hahn G. Acute and chronic hypothermia in a man with spinal cord injury: environmental and pharmacological causes. Arch Phys Med Rehabil. 1991;72:421–424. [PubMed] [Google Scholar]
- Odderson IR, Jaffe KM, Sleicher CA, Price R, Kropp RJ. Gel wheelchair cushions: a potential cold weather hazard. Arch Phys Med Rehabil. 1991;72:1017–1020. [PubMed] [Google Scholar]
- Attia M, Engel P. Thermoregulatory set point in patients with spinal cord injuries. Paraplegia. 1983;21:233–248. doi: 10.1038/sc.1983.37. [DOI] [PubMed] [Google Scholar]
- Greene PS, Cameron DE, Mohlala MI, et al. Systolic and diastolic left ventricular dysfunction due to mild hypothermia. Circulation. 1989;80:44–48. [PubMed] [Google Scholar]
- Jurkovich GJ, Greiser WB, Luterman A, Curreri PW. Hypothermia in trauma victims: an ominous predictor of survival. J Trauma. 1987;27:1019–1024. [PubMed] [Google Scholar]
- Luna GK, Maier RV, Pavlin EG, Anardi D, Copass MK, Oreskovich MR. Incidence and effect of hypothermia in seriously injured patients. J Trauma. 1987;27:1014–1018. doi: 10.1097/00005373-198709000-00010. [DOI] [PubMed] [Google Scholar]
- Tsuei BJ, Kearney PA. Hypothermia in trauma patients. Injury. 2004;35:7–15. doi: 10.1016/s0020-1383(03)00309-7. [DOI] [PubMed] [Google Scholar]
- Cosgriff N, Moore EE, Sauaia A, Kenny-Moynihan M, Burch JM, Galloway B. Predicting life threatening coagulopathy in the massively transfused trauma patient: hypothermia and acidosis revised. J Trauma. 1997;42:857–861. doi: 10.1097/00005373-199705000-00016. [DOI] [PubMed] [Google Scholar]
- Downey JA, Lemons DE. Human thermoregulation. In: Downey JA, Myers SJ, Gonzalez EG, Lieberman JS, editors. The Physiological Basis of Rehabilitation Medicine. 2nd ed. Stoneham, MA: Butterworth–Heinemann; 1994. pp. 351–363. [Google Scholar]
- Bauman WA, Spungen AM. Disorders of carbohydrate and lipid metabolism in veterans with paraplegia and quadriplegia: a model of premature aging. Metabolism. 2000;43:949–956. doi: 10.1016/0026-0495(94)90126-0. [DOI] [PubMed] [Google Scholar]
- Duckworth WC, Solomon SS, Jallepalli P, et al. Glucose intolerance due to insulin resistance in patients with spinal cord injuries. Diabetes. 1980;29:906–910. doi: 10.2337/diab.29.11.906. [DOI] [PubMed] [Google Scholar]
- Yekutiel M, Brooks ME, Ohry A, Yahrom J, Carel R. The prevalence of hypertension, ischemic heart disease and diabetes in traumatic spinal cord injured patients and amputees. Paraplegia. 1989;27:58–62. doi: 10.1038/sc.1989.9. [DOI] [PubMed] [Google Scholar]
- Bauman WA, Spungen AM, Zhong YG, Rothstein JL, Petry C, Gordon SK. Depressed serum high density lipoprotein cholesterol levels in veterans with spinal cord injury. Paraplegia. 1992;30:697–703. doi: 10.1038/sc.1992.136. [DOI] [PubMed] [Google Scholar]
- Maki KC, Briones ER, Langbein WE, et al. Associations between serum lipids and indicators of adiposity in men with spinal cord injury. Paraplegia. 1995;33:102–109. doi: 10.1038/sc.1995.24. [DOI] [PubMed] [Google Scholar]