Abstract
Objective:
Rectal lesions have an effect on the urinary bladder and its sphincters. Patients with constipation sometimes complain of difficult micturition or of retention. Urinary retention may also occur after anorectal operations. We investigated the hypothesis that rectal distension affects vesical dilatation through a reflex action.
Methods:
The study comprised 22 healthy volunteers (14 men, 8 women, age 42.3 ± 10.3 SD years). The rectum was distended by rectal balloon inflated with air in increments of 50 mL. The vesical and posterior urethral pressures were recorded before and after individual anesthetization of the rectum, bladder, and posterior urethra.
Results:
Fifty-milliliter rectal distension effected no vesicourethral pressure response (P > 0.05). At 100 and up to 300-mL distension, the vesical pressure decreased (P < 0.05), while the urethral pressure increased (P < 0.05). The response showed no significant difference upon increase of the distending volume. The mean latency was 16.8 ± 2.4 milliseconds. Vesicourethral pressure did not respond to rectal distension when the bladder, urethra, or rectum was individually anesthetized.
Conclusions:
Rectal distension seems to induce diminished vesical, but increased urethral sphincter tone, an effect that is presumably mediated through a reflex that we call the “recto-vesicourethral reflex.” This reflex is apparently evoked at defecation to abort simultaneous micturition. The clinical significance of the reflex needs to be established.
Keywords: Rectum, Rectal physiology, Constipation, Urinary retention, Anorectal lesions, Urethral sphincter, Reflex, Defecation
INTRODUCTION
Rectal lesions have an effect on the urinary bladder and its sphincters. Some patients with constipation have been reported to complain of difficult micturition or of urinary retention (1). Also after anorectal operations, urinary retention is not uncommonly encountered (2,3. The mechanisms of defecation and urination are under the control of voluntary and reflex actions (4–6). The rectum and urinary bladder receive their sympathetic supply from L1, L2, and L3, while the parasympathetic supply derives from S2, S3, and S4(7). When sympathetic fibers enter the pelvic plexus, they intermingle with the sacral parasympathetic pathway as well as postganglionic axons from the sympathetic chain.
The relation of micturition to the anorectal function has been studied by other investigators (8,9. It was reported that anal distension was associated with an increase in vesical pressure (8), while bladder distension increased the internal anal sphincter tone (9). We investigated the hypothesis that rectal distension affects vesical dilatation and that this action is reflex in nature.
METHODS
Subjects
Twenty-two healthy volunteers (14 men, 8 women) of a mean age of 42.3 ± 10.3 SD years (range 30–55 years) were studied. They had no anorectal or urinary complaint in the past or at the time of presentation. For all subjects, physical examination, including neurologic and anorectal findings, was normal, as were stool frequency, barium enema, and colonoscopy. Urinalysis, plain radiographs of the urinary tract and intravenous pyelography showed normal findings.
All the subjects gave a written consent after having been informed about the nature of the study, the tests to be done, and their role in the study. The study was approved by the Review Board and Ethics Committee of the Cairo University Faculty of Medicine.
Procedure
A balloon, constructed from 10 cm of an unstretched condom (London Rubber Industries Ltd, London, UK) and connected to the distal part of a 14F Nélaton catheter, was introduced into the rectum so that the proximal end of the condom lay 6 to 8 cm above the anal orifice. The vesical and urethral sphincteric pressures were recorded by means of a 2-channel microtip catheter (Wiest, Urocompact 2000, Los Altos, CA), which was connected to a strain gauge pressure transducer (Statham, 2306, Oxnard, CA). The rectal balloon was then inflated with air in increments of 50 mL to 300 mL, and the vesical and posterior urethral pressures were recorded.
Rectal and Urethral Anesthetization
Fifteen of the 22 studied subjects approved and consented to the anesthetization test after being informed of its details. The rectum was anesthetized by a lidocaine solution consisting of 20 mL of 2% lidocaine added to 100 mL of normal saline. The solution was introduced into the rectum by means of a 16F catheter, which was removed after administration of the anesthetic solution. The response of the vesical and posterior urethral pressures to rectal balloon distension in increments of 50 mL up to 300 mL was recorded 20 minutes after lidocaine administration, and 3 hours later when the anesthetic effect had waned. The test was repeated after rectal administration of normal saline instead of lidocaine.
Two days later, the urinary bladder was anesthetized by introducing into it a solution of 10 mL of 2% lidocaine in 100 mL of normal saline per urethra. The vesical and urethral pressure responses to rectal distension as aforementioned were then registered 20 minutes after lidocaine administration and 3 hours later. The test was repeated using saline instead of lidocaine. After 2 days, the urethra was anesthetized by 2% lidocaine gel fed into the urethra through a 16F catheter, and the response to rectal distension was recorded as above mentioned. In a repetition of the test, bland gel was used instead of lidocaine gel. To ensure reproducibility of the results, the measurements were repeated at least twice, and the mean value was calculated. The results were analyzed statistically using Student's t test, and values were given as the mean ± SD. Differences assumed significance at P < 0.05.
RESULTS
No adverse side effects were encountered during or after performing the tests, and all the subjects were evaluated. The mean basal vesical pressure was 7.2 ± 1.2 cmH2O and posterior urethral pressure 63.7 ± 4.8 cmH2O (Table 1); these figures agree with those of normal controls in our laboratory.
Table 1.
Vesical and Urethral Pressures in 22 Volunteers During Rectal Distension †
Vesicourethral pressure showed no response to 50-mL rectal balloon distension (P > 0.05, Table 1). At 100 mL and up to 300 mL of rectal distension, vesical pressure significantly decreased, while urethral pressure significantly increased (P < 0.05, P < 0.05, respectively; Figure 1, Table 1). From 100 mL to 300 mL of distension, the vesicourethral pressure response showed no significant difference (P > 0.05, Table 1).
Figure 1. (a) Urethral and (b) vesical pressure tracing on rectal balloon distension with 100 mL of air. The ↑ indicates distension.
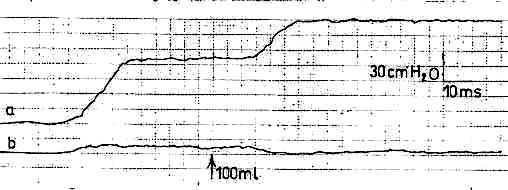
The latency or the time lapse from the start of rectal distension to the start of the vesicourethral pressure response recorded a mean of 16.8 ± 2.4 milliseconds (range 14–21 milliseconds). The mean response duration was 6.3 ± 1.1 milliseconds (range 5–8 milliseconds). The vesicourethral pressure measurements showed no significant difference between the old vs the young (P > 0.05) or the multiparous vs the nulliparous subjects (P > 0.05).
The vesicourethral pressure did not respond to the above-mentioned rectal distending volumes when the bladder, urethra, or rectum was individually anesthetized. However, vesicourethral pressure did respond 3 hours later when the anesthetic effect had disappeared; it also responded to rectal distension when saline was instilled in the rectum or bladder instead of lidocaine and when bland gel was administered into the urethra. These results were reproducible with no significant difference when the same test was repeated in the individual subject.
DISCUSSION
These results show that experimentally produced rectal distension, a condition simulating rectal distension induced by rectal inertia, was associated with diminished vesical and increased posterior urethral pressure. These results presumably denote that rectal distension dilates the urinary bladder, while it apparently increases the urethral sphincter tone. This effect did not occur with small-volume rectal distension. It seems that large-volume rectal distension stimulates stretch receptors located in the rectal wall with a resulting vesical dilatation and pressure decrease as well as posterior urethral pressure increase, which presumably results from augmentation of urethral sphincter tone.
We postulate that the rectal distension by the fecal mass occurring at defecation produces vesical dilatation and an increase in the urethral sphincter tone. Apparently any attempt to urinate, either voluntary or reflexly, is warded off by this effect until the fecal mass has left the rectum and the rectal distension has disappeared. These responses seem to point to the existence of a physiologic process that acts to prevent urination during defecation. The mechanism underlying this process needs to be discussed.
The vesicourethral response to rectal distension suggests a reflex relationship between the 2 actions. The constancy of this relationship was assured by reproducibility. Meanwhile, the reflex nature of this relationship is evidenced by the absence of the vesicourethral pressure response upon individual anesthetization of the assumed 2 arms of the reflex arc: the rectum and the bladder with urethra. We call this reflex relationship the “recto-vesicourethral reflex” (RVUR). It seems that rectal distension stimulates the mechanoreceptors in the rectal wall, and the impulses pass along the pelvic nerve to the sacral spinal cord, which eventually sends impulses to the bladder and urethra. Anesthetization of the rectal, vesical, or posterior urethral mucosa apparently blocks their innervation, so that nerve impulses cannot be transmitted from the rectum to the spinal cord or from the spinal cord to the bladder or urethra. Lidocaine blocks the sensory fibers (C and A α-fibers) responsible for pain and reflex activity (10,11).
It appears that the RVUR acts to harmonize the relation between the rectum and urinary bladder during evacuation. The reflex seems to regulate defecation and urination mechanisms, so that each act can be performed independently without fecal or urinary leak, respectively. Thus at defecation, the micturition mechanism seems to be inhibited as evidenced by vesical dilatation and the increased urethral sphincter tone; this action appears to be mediated through the RVUR, which presumably functions to keep the processes of defecation and micturition apart from each other and not synchronously occurring.
The rectum and urinary bladder share a common evacuation muscle, which is the levator ani (12–14). Contraction of the levator ani muscle leads to opening of both the rectal and vesical necks (12–14). However, defecation seems to evoke the RVUR, which presumably aborts micturition through reflex urethral sphincter contraction and the detrusor dilatory effect. Furthermore, while the puborectalis muscle acts as a common continence sphincter for both the rectum and for the urinary bladder, each organ also has its individual sphincter, which is controlled not only by the reflex, but also by voluntary control (15,16. The external anal and urethral sphincters are derived from the puborectalis muscle (15,16. During defecation, the tonic activity of the urethral sphincter appears to become reflexly increased; however, after defecation, the sphincter can relax voluntarily if urination is acceded to. Thus, the urethral sphincter is presumably under both reflex and voluntary control. The reflex action seems to act during defecation.
The RVUR differs from the anorectal excitatory reflex, which produces rectal contraction upon stimulation of the anal stretch receptors through anal dilatation (17). The latter reflex constitutes the mechanism by which anal stretch and stimulation effect bowel emptying in individuals with spinal cord injury.
CONCLUSION
This study suggests the existence of a relationship between the rectum on the one hand, and the urinary bladder with the urethral sphincter on the other hand. We postulate that rectal disorders may disturb the vesicourethral function. A normal reflex action depends on the integrity of the segmental pathways. Involvement of these pathways in a neurological pathology may lead to prolongation of the latency of the reflex or diminution of the amplitude of the motor unit action potentials. Detectable changes in the latency or amplitude would indicate a defect in the reflex pathway that could be caused by muscle or nerve damage from disease of the spinal cord, spinal nerve roots or peripheral nerves, or from a central lesion. The RVUR might thus prove to be of diagnostic significance in rectourinary disorders.
In conclusion, a diminished vesical and increased urethral sphincter pressure in response to rectal distension was demonstrated and appears to be mediated through a reflex that we call the “rectovesicourethral reflex.” The reflex seems to be evoked at defecation to inhibit simultaneous micturition. The clinical significance of this reflex needs to be established.
Acknowledgments
The authors thank Margot Yehia for assistance in the preparation of this manuscript.
REFERENCES
- Miyazato M, Sugaya K, Nishijima S, Ashitomi K, Ohyama C. Effect of glycerin enema for acute urinary retention in children and its mechanism. J Jpn Med Soc Spinal Cord Lesion. 2003;16:174–178. [Google Scholar]
- Bleday R, Pena JP, Rothenberger DA, et al. Symptomatic hemorrhoids: current incidence and complications of operative therapy. Dis Colon Rectum. 1992;35:477–480. doi: 10.1007/BF02049406. [DOI] [PubMed] [Google Scholar]
- Catalds PA, Senagore AJ. Does alpha sympathetic blockade prevent urinary retention following anorectal surgery? Dis Colon Rectum. 1991;34:1113–1116. doi: 10.1007/BF02050073. [DOI] [PubMed] [Google Scholar]
- Bilkey WJ, Awad EA, Smith AD. Clinical application of sacral reflex latency. J Urol. 1983;129:1187–1189. doi: 10.1016/s0022-5347(17)52632-4. [DOI] [PubMed] [Google Scholar]
- Pedersen E. The anal reflex. In: Henry M, Swash M, editors. Coloproctology and the Pelvic Floor: Pathophysiology and Management. London, UK: Butterworths; 1985. pp. 105–109. [Google Scholar]
- Shafik A, El-Sibai O. Rectal inhibition by inferior rectal nerve stimulation in dogs: recognition of a new reflex—the ‘voluntary anorectal inhibition reflex’. Eur J Gastroenterol Hepatol. 2001;13:413–418. doi: 10.1097/00042737-200104000-00019. [DOI] [PubMed] [Google Scholar]
- Wexner SD, Jorge MN. Anatomy and embryology of the anus, rectum and colon. In: Corman ML, editor. Colon and Rectal Surgery. 4th ed. New York, NY: Lippincott-Raven; 1998. pp. 1–26. [Google Scholar]
- Shafik A. Anovesical reflex: role in inducing micturition in paraplegic patients. Paraplegia. 1994;32:104–107. doi: 10.1038/sc.1994.18. [DOI] [PubMed] [Google Scholar]
- Buntzen S, Nordgren S, Delbro D, Hulten L. Anal and rectal motility responses to distension of the urinary bladder in man. Int J Colorect Dis. 1995;10:148–151. doi: 10.1007/BF00298537. [DOI] [PubMed] [Google Scholar]
- Yokoyami O, Komatso K, Kodama K, et al. Diagnostic value of intravesical lidocaine for overactive bladder. J Urol. 2000;164:340–343. [PubMed] [Google Scholar]
- Silva C, Ribeiro MI, Cruz F. The effect of intravesical resiniferatoxin in patients with idiopathic detrusor instability suggests that involuntary detrusor contractions are triggered by C-fiber input. J Urol. 2002;168:575–579. [PubMed] [Google Scholar]
- Shafik A, Asaad S, Doss S. The histomorphologic structure of the levator ani muscle and its functional significance. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:116–124. doi: 10.1007/s001920200026. [DOI] [PubMed] [Google Scholar]
- Shafik A, Asaad S, Doss S. Etiology of the resting myoelectric activity of the levator ani muscle: physioanatomic study with a new theory. World J Surg. 2003;27:309–314. doi: 10.1007/s00268-002-6584-1. [DOI] [PubMed] [Google Scholar]
- Shafik A, El-Sibai O. Effect of levator ani muscle contraction on urethrovesical and anorectal pressures and role of the muscle in urination and defecation. Urology. 2001;58:193–197. doi: 10.1016/s0090-4295(01)01196-7. [DOI] [PubMed] [Google Scholar]
- Shafik A. Study on the origin of the external anal, urethral, vaginal and prostatic sphincters. Int Urogynecol J Pelvic Floor Dysfunct. 1997;8:126–129. doi: 10.1007/BF02764842. [DOI] [PubMed] [Google Scholar]
- Shafik A. Pelvic double-sphincter control complex: theory of pelvic organ continence with clinical application. Urology. 1984;23:611–618. doi: 10.1016/0090-4295(84)90086-4. [DOI] [PubMed] [Google Scholar]
- Shafik A, Shafik AA, Ahmed I. Role of positive anorectal feedback in rectal evacuation: the concept of a second defecation reflex: the anorectal reflex. J Spinal Cord Med. 2003;26:380–383. doi: 10.1080/10790268.2003.11753709. [DOI] [PubMed] [Google Scholar]



