Abstract
Background
General practice in the UK is undergoing a period of rapid and profound change. Traditionally, research into the effects of change on general practice has tended to regard GPs as individuals or as members of a professional group. To understand the impact of change, general practices should also be considered as organisations.
Aim
To use the organisational studies literature to build a conceptual framework of general practice organisations, and to test and develop this empirically using case studies of change in practice. This study used the implementation of National Service Frameworks (NSFs) and the new General Medical Services (GMS) contract as incidents of change.
Design of study
In-depth, qualitative case studies. The design was iterative: each case study was followed by a review of the theoretical ideas. The final conceptual framework was the result of the dynamic interplay between theory and empirical evidence.
Setting
Five general practices in England, selected using purposeful sampling.
Method
Semi-structured interviews with all clinical and managerial personnel in each practice, participant and non-participant observation, and examination of documents.
Results
A conceptual framework was developed that can be used to understand how and why practices respond to change. This framework enabled understanding of observed reactions to the introduction of NSFs and the new GMS contract. Important factors for generating responses to change included the story that the practice members told about their practice, beliefs about what counted as legitimate work, the role played by the manager, and previous experiences of change.
Conclusion
Viewing general practices as small organisations has generated insights into factors that influence responses to change. Change tends to occur from the bottom up and is determined by beliefs about organisational reality. The conceptual framework suggests some questions that can be asked of practices to explain this internal reality.
Keywords: change, conceptual framework, general practice, organisations
INTRODUCTION
Activity in general practice accounts for a significant proportion of overall activity in the UK NHS. However, little is understood about why practitioners behave as they do. In the past 10 or more years there have been frequent attempts by governments to modify behaviour, using contractual mechanisms (for example, the new GP contracts in 1991 and 2004), peer pressure (clinical governance and appraisal), and normative guidelines (for example, National Service Frameworks [NSFs] and National Institute for Health and Clinical Excellence guidelines).
Some of these initiatives have had limited success,1 while others have generated apparently perverse consequences, in the sense that distribution of rewards moved away from areas of greatest deprivation.2 As the NHS undergoes continuing rapid change, understanding how such change is perceived and responded to by general practices should be an important goal for research.
Traditionally, research into the effect of new initiatives on practices has seen GPs as individuals or as members of a professional group. Research has sought to explain the impact of change with reference to the beliefs, attitudes, and behaviours of GPs as individuals,3 or in terms of the effects on the standing of the professional group.4,5 There are areas of practice in which this approach is entirely appropriate. However, collective practice behaviour cannot solely be explained in terms of the individual. The context in which these individuals work — the practice — also needs to be understood.6
Research into the behaviour of doctors in primary care has begun to perceive practices as organisations, and to use aspects of the organisational studies literature to inform research. The metaphor of ‘organisational culture’ as a research tool, and as a management tool to improve performance, has been adopted.7–9 Despite the development of sophisticated measuring tools, no consensus exists as to what culture is or how it might be manipulated.10
It has been argued that ‘organisational culture’ is a ‘residual category’ that is used by policy makers (and researchers) to make sense of the difficulties that they encounter in trying to change practice.11 However, it is a useful concept that can help to inform research.
The use of complex adaptive systems is another strand of organisational thinking that has been referred to in the primary care literature. It is argued that general practices should be thought of as systems of interacting agents that act to maintain an internal equilibrium in response to external change. These interactions are complex, and responses to change cannot necessarily be predicted.12–16
The strength of the complex adaptive systems approach to practice organisations is that it acknowledges that it is unlikely that organisations will assess new initiatives according to a set of clear goals and will implement them in a linear fashion. The application of complexity theory to the behaviour of human beings has been criticised because it extrapolates from pure mathematics (where complexity and chaos theory have their origins).17 Much of the literature on the use of complexity theory in human contexts fails to address how this theory can be applied in practical settings. Although much of the language used will be familiar to those who are involved in general practice, the practical applications for research and development are less clear.
This article outlines a conceptual framework, relevant to general practice in the UK, which can be used to understand how practices work and how they may develop and respond to change in the future. The conceptual framework is based on organisational studies literature, and has been developed and tested in empirical studies. The framework is intended to provide researchers, practices, and primary care trusts (PCTs) with a practical tool to support their work.
The study aims were to:
design a conceptual framework to explore the nature of general practice organisations; and
to use the conceptual framework for investigation of responses to change, in particular, responses to the introduction of the NSFs and the new General Medical Services (GMS) contract.
How this fits in
Understanding the impact of change in general practice is important for developing strategies to meet new demands. This article uses organisational studies literature and evidence from empirical studies to generate a conceptual framework to provide information about the nature of general practice organisations and the factors that affect response to change.
The impact of these new initiatives have been reported elsewhere.18–20 This article describes the development of the conceptual framework. It begins with a description of the initial theoretical framework. The methods used are outlined and the final conceptual framework is presented and illustrated using examples from the case studies. A case is described to illustrate the use of the framework in understanding responses to change, and implications of the study are discussed.
Theoretical background
This study was based on the work of Weick,21–23 and complementary studies informed the design and method.24–28 Weick argues that the central activity in all organisations is what he calls ‘sensemaking’:
‘To talk about sensemaking is to talk about reality as an ongoing accomplishment that takes form when people make retrospective sense of the situations in which they find themselves and their creations.’21
According to Weick, members of organisations extract cues to action from the changing environment in which the organisation finds itself. What is seen as significant will vary, and is influenced by previous experiences and underlying values. The action that occurs as a result of these cues will in turn change the environment within the organisation and will play a part in determining which cues are noticed in future. For example, if a group of GPs in a practice make sense of their role as being predominantly concerned with the physical health of their patients (as opposed to psycho-social aspects of care), then the care of patients with diabetes in their practice will focus on physical parameters, such as HbA1c or blood pressure. They are less likely to pay attention to patients' psychological adjustment to the disease. In adjusting their care they will collect data which informs them how they are doing in terms of these physical parameters, and service improvements will also focus on these issues. They are likely to concentrate on changing medication or developing better computer templates rather than organising self-help groups for newly diagnosed patients. Thus, the fundamental beliefs that the group of doctors hold about the nature of their role will influence how they deliver care to patients, how they audit that care, and how they respond to any deficiencies that they find. Because they are not looking for psychological issues, they are less likely to notice if they are failing to deliver high quality psychological support. This process is circular (Weick21 calls it ‘ongoing’). In other words, the beliefs that people hold about what their role is, will determine which cues they notice in the world around them; this in turn will determine how they behave. How they behave will change the environment in which they are working, and will affect which cues they notice in the future as well as their beliefs about their role.
In relation to research, the GPs in the example above are more likely to notice research evidence that concentrates on technical diabetic control, and less likely to notice evidence that concentrates on psychological issues. They will alter their practice according to evidence that is congruent with their beliefs, and this will then reinforce their belief in the importance of technical control. In reality, most GPs recognise the importance of both aspects of diabetic care; however, this example illustrates how the ongoing feedback that Weick describes might work in practice. Weick states that the process of sensemaking in this context is rooted in identity construction.21 How a GP cares for a patient with diabetes is not only a technical question, but also one of identity, for example: ‘What kind of a doctor am I?’. Weick argues that sensemaking is also tied up with collective identity: ‘What kind of a practice are we?’. This is not necessarily a shared identity, as complete consensus is unlikely in any organisation, but it does represent an identity which members of the organisation feel they they can accept.
This study examines the notion of sensemaking in general practice. It investigates the usefulness of the concept and how, if practices ‘make sense’ differently, this is manifest. This study also examines factors that inform the sensemaking process.
METHOD
A fuller explanation of the methods used in this study is available.18,19 Case studies of five general practices (case studies 1–5 of Practices A–E) were undertaken between April 2002 and June 2004 in practices across areas covered by two PCTs. Interviews were undertaken with all doctors, nurses, managers, and senior administrative staff at each practice (38 interviews in all). Meetings and informal practice activity were also observed in each practice. All fieldwork was undertaken by the author who, as a qualified GP, was accepted by the practices and enjoyed a degree of ‘insider status’.29
Interviews were transcribed and analysed alongside detailed field notes from observation. Recurrent themes were identified with reference to the theoretical ideas described above. These themes were used to develop large diagrams or ‘causal networks’30 that linked observed behaviours with expressed attitudes and beliefs. The research was iterative. Weick's ideas were used to develop an initial theoretical framework, which was applied to the first case study to investigate the way in which NSFs had affected and been implemented by the practice.
Following application of the framework to the first case study, the framework was revisited and revised. The resulting modified framework was used in the second study. Further cycles of use and modification were undertaken until, after the fourth case study, the conceptual framework was developed. The framework was then tested in the final case study. Figure 1 illustrates the cycle of theory development and testing.
Figure 1.
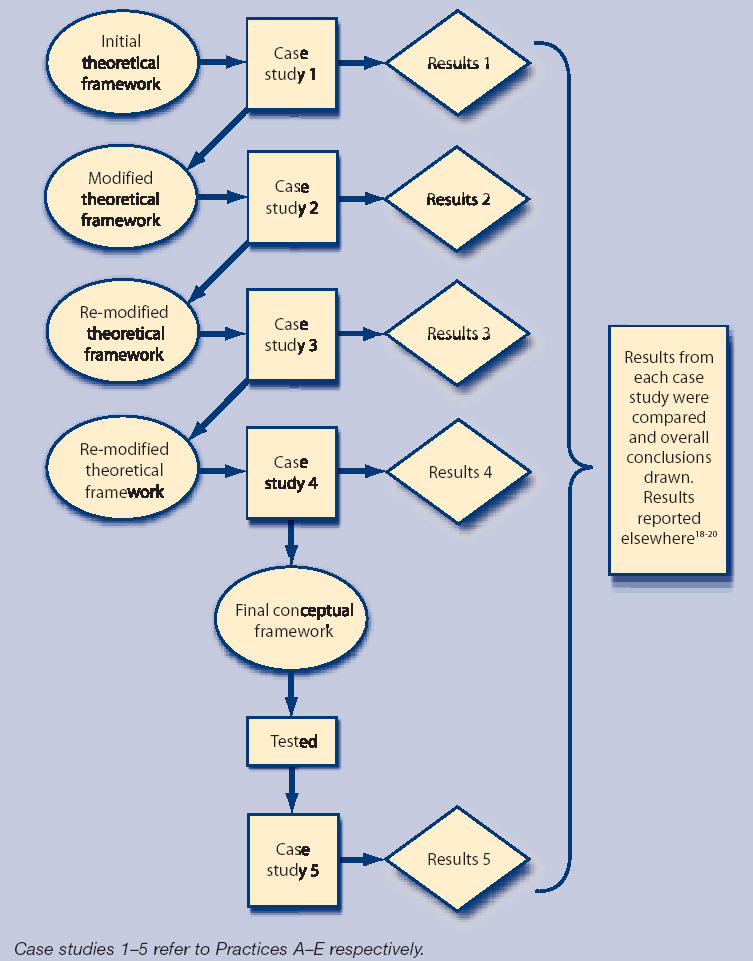
Development and testing of the conceptual framework.
To ensure validity, different data collection methods were triangulated. Findings from interviews were compared with findings from observation and from analysis of selected documents, such as memos, job descriptions, and records of meetings. Feedback visits were made to the practices, allowing a degree of responder validation of the findings.31
The conceptual framework
As the phrase ‘conceptual framework’ can be confusing, it is important to define the sense in which the term is being used. In this article it is used in the same way that some authors use the alternative phrase ‘conceptual model’. Conceptual framework here is defined as:
‘a simplified representation of selected aspects of a phenomenon aiming to conceptualise it and allow explanations of relationships to be framed and tested.32 [Author's emphasis added]
A conceptual framework can be viewed as a core conceptualisation of the problem situation, rather than a description of it. The elements in the conceptual framework are not assumed to be literally present in the world, but to be social constructs that are useful in thinking about the situation.
The conceptual framework presented in this article is designed to provide a structured approach to researching factors that may be important in understanding general practice. The conceptual framework can be used to illustrate the way that different elements of general practices are linked. It is provisional and developmental, designed to be interrogated and, possibly, improved as it is used in more cases (Figure 2).
Figure 2.
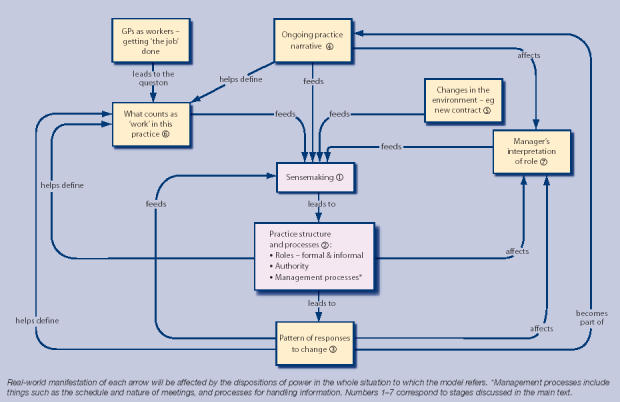
Conceptual framework for understanding the response of GP practices to change.
This conceptual framework assumes that the central activity taking place in the management and development of general practices is ‘sensemaking’ (Figure 2, stage 1). This was illustrated during the fieldwork when two of the practices aimed to appoint a new doctor. Practice A was overstretched, having recently had an influx of new patients. In discussing the appointment of a new partner their only consideration was the impact that this would have on workload. Practical issues, such as who would cover the infant clinic, dominated the meeting. More obscure questions, such as how practice dynamics might alter with the shift from three to four partners, were not considered.
In contrast, Practice C had a strong sense of identity as a small and close-knit practice. Discussion of the appointment of a new salaried doctor focused on the effect that this would have on their ideal of ‘smallness’. How to integrate the new doctor, how to remain close as a group, and how to avoid problems that they associated with larger practices were all discussed. However, they did not discuss more practical issues, such as how the salaried doctor would divide his or her time, and how much autonomy he or she would have.
Thus, Practices A and C ‘made sense’ of a similar issue, the appointment of a new doctor, in different ways. This sensemaking was informed by their previous experiences (for example, of overwork or work dynamics) and by their values and shared sense of identity.
The sensemaking process contributes to the structure and processes of the organisation (Figure 2, stage 2). For example, doctors in Practice C believed that the identity ‘GP’ must include a ‘hands-on’ approach to managing the practice. With their commitment to smallness, this resulted in a practice structure that included a manager who occupied a purely administrative role. Management meetings between the partners excluded the practice nurse and the manager, ensuring that they were excluded from decision making.
Sensemaking in Practice D emphasised meticulous organisation and proactive management. A manager was appointed who worked strategically, organising and presiding over management, clinical, and primary care team meetings. The manager was involved in planning for the new contract, making decisions, and coordinating all of the activity needed to gain maximum Quality and Outcomes Framework points. Sensemaking underpins organisation of the practice and influences how practices respond to new initiatives (Figure 2, stage 3).
During research, it became apparent that common factors could be identified to explain the pattern of sensemaking in each practice. Practices develop a narrative about themselves (Figure 2, stage 4). This is more than a ‘history’. It is an ongoing process in which past events are reinterpreted and integrated. The resulting narrative defines ‘who we are’ and ‘how we got here’, and it underpins sensemaking.
For example, doctors in Practice C had taken over a run-down practice years ago. They worked together to develop the premises and services. This experience could be seen to influence the development of their belief in the value of a close working partnership, the need for doctors to be fully ‘in control’ of the practice, and the importance of a commitment to the local population.
Previous changes to the environment and the way practices react to change are incorporated into the ongoing narrative and have a direct effect on sensemaking (Figure 2, stage 5). For example, staff members of Practice B were active participants in the fundholding scheme, using it to develop innovative services for their patients. They developed a sense of themselves as ‘entrepreneurs’, which conditioned their response to later initiatives. When faced with change, their first question was whether it would allow them to develop the practice.
Perceptions of ‘legitimate work’ by practice members were found to influence responses to change (Figure 2, stage 6). Thinking of doctors as workers who were trying to ‘get the job done’ was useful in understanding these responses.18,33 Asking the question: ‘What counts as work in this practice?’ yielded useful insights. Although ‘seeing patients’ is viewed as work in all practices, there is variation in the relative importance afforded to other aspects of the practice, for example, variation in the type of patients doctors are expected to see. In Practice C, it was regarded as essential for doctors to be doing management work, whereas in Practice A, management work was regarded as a nuisance. When faced with new initiatives, these beliefs played an important part in determining simple things, such as who read the relevant documents and who attended the relevant meetings. Understanding what practice members believe their ‘work’ entails can provide insight into how they respond to change.
It was found that the way managers interpret and perform their role can have a profound impact on the sensemaking process (Figure 2, stage 7). Doctors in Practice C had no experience of working with a high-level manager. They believed that such a manager was not needed in their practice and that it is not possible for any general practice to work successfully with a professional manager. In contrast, doctors in Practice D were used to working with a highly-skilled manager and found it hard to believe that any practice could manage without.
The effect of this factor depends, to a large extent, on the distribution of power in the situation. Contrary to the common perception of GPs as powerful professionals and practice ‘owners’, analysis of the case studies shows that power can be distributed in different ways in a practice. It is this distribution of power that determines the magnitude of the effect of the other elements in the conceptual framework. A powerful manager (as in Practice D) is likely to have a major effect on a practice's sensemaking process.
In individual practices the pattern of responses to change (Figure 2, stage 3) will feed back and inform other elements in the conceptual framework. Sensemaking is altered by the experience of acting in the world. Experiences are incorporated into the organisation's narrative which is a source of collective identity. Beliefs about legitimate roles evolve and change; thus, practices are dynamic organisations, constantly defined and redefined by their experiences.
RESULTS
Practice B is provided as an example of how the conceptual framework can be used to interpret responses to change (the introduction of NSFs and the GMS contract). Practice B had a long and complicated history, which included a number of partnership changes and disputes. The current partners have been together for a few years and have a good professional relationship. Thus, the ‘narrative’ that was offered by the practice members was that, after some turbulence, they were now able to provide a good service to their patients as a result of their good interpersonal relationships.
In this organisation, the partners held a belief in themselves as entrepreneurs providing a ‘good service’ which is well-organised. This formed part of the practice members’ definition of the legitimate work of GPs. The nurses were encouraged to play their part in this, developing new clinics for patients with chronic diseases. Success was defined by the range of services provided. (This contrasts with Practice A, whose definition of the legitimate role of GPs was as individual patient advocates, and for whom ‘success’ was defined by the quality of the relationships they developed with their patients.)
The manager's role in practice B was unclear. When the fundholding scheme ended, the fundholding manager became the practice manager, working reduced hours as income from the scheme was lost. In spite of the existence of a written job description, administrative staff and doctors were not in agreement about how this new role should be performed. The importance placed on harmonious relationships meant that this conflict was suppressed and the underlying issues were not addressed.
Internal sensemaking arose from these interacting factors and determined, and was determined by, the ongoing actions of practice members. Thus, activity by the members of this practice was directed at maintaining ‘organised’ patient care and the current good relationship between the partners, and seizing new opportunities that arose. It is important to note that these were implicit rather than explicit motivators of activity. These ideas are embedded in the belief system of the organisation and form the context within which activity occurs, rather than being followed as conscious ‘goals’. Out of the sensemaking process arose a structure that involved frequent meetings (which were often chaotic because of unresolved issues relating to the role of the manager), a leading role for nurses in developing organised care, and vying for position between the manager and the senior administrator.
When NSFs were introduced, they were welcomed by Practice B as fitting in with the ethos of providing organised care. However, working from the assumption that organised care was already provided, there was no formal plan to implement the frameworks. The confusion over the exact role of the manager meant that they did not take this kind of lead, and did not challenge these assumptions. The new GMS contract was also welcomed by the practice on the basis that ‘organised care’ was to be rewarded. They were interested in the opportunities for providing enhanced services, and were keen for nurses to play a leading role in developing the care for patients with chronic diseases.
The conceptual framework can be used to understand the finding that a practice which seemed to be in agreement with the philosophy behind NSFs had not made any explicit efforts to implement them. The manager's failure to fulfil the coordinating role specified in the job description meant that these assumptions were not challenged.
Engaging with this particular practice to facilitate change would involve being aware of the ambiguous role of the manager, engaging the nurses, and emphasising aspects of the desired innovation that would enhance the ‘organised care’ that the practice provided. In addition, practice members would be receptive to innovative ideas and would welcome the chance to develop their services proactively.
DISCUSSION
Summary of main findings
This article presents a conceptual framework that provides insight into the way general practices function in response to change. Its value is in generating a series of practical questions that can be used to understand how practices ‘work’. Asking questions, such as ‘What stories do these people tell about their practice?’, ‘What roles are occupied in this practice?’, ‘What is considered as legitimate work?’, and ‘How has this practice responded to initiatives in the past?’, allows conclusions to be drawn about the internal assumptions that drive the organisation and determine how new initiatives are perceived and acted on.
Strengths and limitations of the study
This conceptual framework was derived by an iterative process, moving from the literature to empirical evidence and back to the literature again. The resulting conceptual framework is practical and based on relevant theory. There is a tendency for research either to be seen by practitioners as irrelevant to their practical concerns, or to be seen by theorists as atheoretical and, therefore, suspect. This research aims to link this divide.
There are risks associated with starting from a strong theoretical base. Aspects of a situation that do not correspond with predetermined theory can be missed or ignored. Examination of these case studies aimed to guard against in this by looking for issue that did not fit with the conceptual framework or that seemed incongruous.
The study was conducted in two areas so the study was relatively small. None of the practices studied was large (the largest practice had five partners). However, it is likely that the factors identified will have relevance in larger organisations. Further research is required to explore this.
The practices studied had at least three partners, so the results may not have relevance to smaller practices. However, the dynamic interplay between theory and practice means that the conceptual framework can be applied to smaller practices. It provides an developing conceptualisation that changes as it is used.
Statistical claims to generalisability cannot be made, as only five practices were studied. However, results demonstrate that ideas developed in one practice were not refuted by the experience in subsequent practices. It seems likely that the core elements identified in this study (practice narrative, how individuals view their legitimate roles, and the experience of external events) will be important elsewhere.
Comparison with existing literature
There is limited research on the development of theoretical ideas about the nature of general practice organisations. The most well-known work of this kind relates to complexity theory.12,13 The issues raised in this study are compatible with complexity theory. In particular, both conceptual frameworks emphasise emergent properties, circularity and internal ‘drivers,’ and arise out of a tradition of organisational theory that emphasises the importance of interactions in determining outcomes.
Complexity theory can be criticised for being too vague and general in its approach. For example, proponents of this theory discuss identifying ‘attractors’ that drive activity,12 without specifying how such things can be identified or how they arise. The conceptual framework presented in this study was developed through practical research. It offers concrete questions that can be asked in practices and suggests the mechanisms by which internal drivers arise and develop.
The other strand of research that has sought to elucidate internal features of practices that drive activity is research into organisational culture.7–9 Proponents of this view of organisations seek to define the culture or cultures of organisations and to use this to drive change. The research presented in this study is not incompatible with this approach. Different ‘cultures’ could be identified in the practices studied; for example, one of the practices had a hierarchical culture, with the manager firmly at the top. However, research indicated that this culture was an emergent property of the underlying features of the organisation. The conceptual framework offers researchers interested in culture a mechanism to examine the determinants of organisational culture rather than its external manifestations.
Although other studies of primary care have not explicitly viewed general practices as organisations, similar issues have been raised to those described here. Riley and Hawe34 argue that practice narratives are an important tool in understanding attitudes to health promotion, and Bateman et al35 conclude that lack of clarity about legitimate roles impedes the development of interprofessional teams. Williams and Calnan36 found that differing views about the role of GPs contributed to the degree of emphasis practices placed on preventative services. The current study links underlying concepts related to sensemaking in general practice to form a more general explanatory conceptual framework.
Implications for future research and policy
This article describes a conceptual framework that can be used to understand responses to change in general practice. The framework has the potential to inform research as it has been developed empirically. Researchers can investigate beyond the activities of individuals by perceiving practices as organisations which can inform design, data collection, and analysis. For example, this conceptual framework suggests that research on the impact of different incentives on behaviour in general practice should differentiate between the impact on individuals and the impact on the practice as an organisation. It suggests useful questions to ask when examining responses to change, such as: ‘How do perceptions of legitimate work affect approaches to change?’, and ‘How are roles changing in the practice?’.
The conceptual framework has potential as a development tool, by suggesting questions that practices should consider to understand the underlying drivers that affect behaviour. It could also be of value to those working in PCTs who work directly with practices, by providing practical tools to assist with change. For example, during the research, one of the two local PCTs introduced an incentive scheme designed to save money. The scheme aimed to alter prescribing and referral patterns by offering a payment if practices signed up to it. One of the practices valued its independence from the PCT, and the scheme was rejected by one of the partners without any discussion. In another practice there was agreement to sign up to the scheme, but it seemed unlikely to bring about any meaningful change.
The conceptual framework helps to understand this limited impact and can assist with the development of strategies to implement change. For example, PCTs wishing to change referral practice should consider engaging with each practice individually. Considering different managerial roles (for example, is the manager empowered to negotiate?) and understanding the previous history of the practice and other drivers that influence behaviour may enable the development of a specific set of targets for each practice. This approach could be open to accusations of inconsistency or unnecessary expense; however, it may be more cost-effective than a scheme that is ignored or one that generates no meaningful change.
The conceptual framework described in this article could help policy makers to develop an understanding of the nature of organisations whose behaviour they are trying to influence. The conclusion that change can only realistically occur from the bottom up, taking into account underlying local realities, is one that many practitioners may recognise as congruent with their own experience.
Acknowledgments
Thanks are due to the practice participants, who were generous with their time and tolerated the intrusion with patience. Professor Stephen Harrison and Professor Martin Marshall also provided invaluable help and support throughout the project.
Funding body
This research was funded by a Training Fellowship from the National Primary Care Research and Development Centre, University of Manchester.
Ethics committee
Ethical approval was obtained from the relevant research ethics committees (Manchester MREC)
Competing interests
The author has stated that there are none
REFERENCES
- 1.Glendinning C. GPs and contracts: bringing general practice into primary care. Social Policy and Administration. 1999;33(2):115–131. [Google Scholar]
- 2.Langham S, Gillam S, Thorogood M. The carrot, the stick and the general practitioner: how have changes in financial incentives affected health promotion activity in general practice? Br J Gen Pract. 1995;45:665–668. [PMC free article] [PubMed] [Google Scholar]
- 3.Freeman AC, Sweeney K. Why general practitioners do not implement evidence: qualitative study. BMJ. 2001;323:1100–1102. doi: 10.1136/bmj.323.7321.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calnan M, Gabe J. Recent developments in general practice: a sociological analysis. In: Gabe J, Calnan M, Bury M, editors. The sociology of the health service. London: Routledge; 1991. pp. 140–161. [Google Scholar]
- 5.Elston MA. The politics of professional power: medicine in a changing health service. In: Gabe J, Calnan M, Bury M, editors. The sociology of the health service. London: Routledge; 1991. pp. 58–88. [Google Scholar]
- 6.University of York. Getting evidence into practice. Effective health care. York: University of York Centre for Reviews and Dissemination; 1999. [Google Scholar]
- 7.Scott T, Mannion R, Davies HT, et al. Implementing culture change in health care: theory and practice. Int J Qual Health Care. 2003;15(2):111–118. doi: 10.1093/intqhc/mzg021. [DOI] [PubMed] [Google Scholar]
- 8.Scott T, Mannion R, Marshall M, et al. Does organisational culture influence health care performance? A review of the evidence. J Health Serv Res Policy. 2003;8(2):105–117. doi: 10.1258/135581903321466085. [DOI] [PubMed] [Google Scholar]
- 9.Kralewski JE, Wingert TD, Barbouche MH. Assessing the culture of medical group practices. Med Care. 1996;34(5):377–388. doi: 10.1097/00005650-199605000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Mannion R, Davies HTO, Marshall MN. Cultures for performance in healthcare: evidence on the relationships between organisational culture and organisational performance in the NHS. York: Centre for Health Economics; 2003. [Google Scholar]
- 11.Ormrod S. Organisational culture in health service policy and research: ‘third way’ political fad or policy development? Policy Polit. 2003;31(2):227–237. [Google Scholar]
- 12.Plsek PE, Greenhalgh T. Complexity science: the challenge of complexity in health care. BMJ. 2001;323:625–628. doi: 10.1136/bmj.323.7313.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plsek PE, Wilson T. Complexity, leadership, and management in healthcare organisations. BMJ. 2001;323:746–749. doi: 10.1136/bmj.323.7315.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller WL, Crabtree BF, McDaniel R, et al. Understanding change in primary care practice using complexity theory. J Fam Pract. 1998;46(5):369–376. [PubMed] [Google Scholar]
- 15.Miller WL, McDaniel RR Jr, Crabtree BF, et al. Practice jazz: understanding variation in family practices using complexity science. J Fam Pract. 2001;50(10):872–878. [PubMed] [Google Scholar]
- 16.Kernick D. Wanted — new methodologies for health service research. Is complexity theory the answer? Fam Pract. 2006;23(3):385–390. doi: 10.1093/fampra/cml011. [DOI] [PubMed] [Google Scholar]
- 17.Reid I. Let them eat complexity: the emperor's new conceptual toolkit. (BMJ rapid response 23 September 2001). http://bmj.bmjjournals.com/cgi/eletters/323/7313/625#16696 (accessed 18 Nov 2006) [PMC free article] [PubMed]
- 18.Checkland K. National Service Frameworks and UK general practitioners: street-level bureaucrats at work? Sociol Health Illn. 2004;26(7):951–975. doi: 10.1111/j.0141-9889.2004.00424.x. [DOI] [PubMed] [Google Scholar]
- 19.Checkland K. Management in general practice: the challenge of the new General Medical Services contract. Br J Gen Pract. 2004;54:734–739. [PMC free article] [PubMed] [Google Scholar]
- 20.Checkland K, Harrison S. Policy implementation in practice: the case of National Service Frameworks in primary care. J Tissue Viability. 2004;14(4):133–136. doi: 10.1016/s0965-206x(04)44003-0. [DOI] [PubMed] [Google Scholar]
- 21.Weick KE. Sensemaking in organizations. Thousand Oaks: Sage; 1995. [Google Scholar]
- 22.Weick KE. The social psychology of organizing. Reading: Addison-Wesley Publishing Company; 1979. [Google Scholar]
- 23.Weick KE. Making sense of the organisation. Malden: Blackwell; 2001. [Google Scholar]
- 24.Vickers G. The art of judgement: A study of policy making. Thousand Oaks: Sage; 1995. [Google Scholar]
- 25.Checkland PB. Systems thinking, systems practice. Chichester: Wiley; 1999. [Google Scholar]
- 26.Checkland PB, Casar A. Vickers' concept of an appreciative system: a systemic account. J Applied Systems Analysis. 1986;13:4–7. [Google Scholar]
- 27.Checkland PB, Holwell S. Information, systems and information systems. Chichester: John Wiley; 1998. [Google Scholar]
- 28.Katz D, Kahn RL. The social psychology of organizations. 2nd (edn) New York: John Wiley and Sons; 1978. [Google Scholar]
- 29.Adler PA, Adler P. Observational techniques. In: Denzin NK, Lincoln YS, editors. Collecting and interpreting qualitative materials. Thousand Oaks: Sage; 1998. pp. 79–109. [Google Scholar]
- 30.Miles M, Huberman A. Qualitative data analysis: an expanded sourcebook. 2nd edition. Thousand Oaks: Sage; 1994. [Google Scholar]
- 31.Seale C. The quality of qualitative research. Thousand Oaks: Sage; 1999. [Google Scholar]
- 32.Miller PMC, Wilson MJ. A dictionary of social science methods. Chichester: Wiley; 1983. [Google Scholar]
- 33.Checkland K. Changing the lens: widening the approach to primary care research. J Health Serv Res Policy. 2003;8(4):248–250. doi: 10.1258/135581903322403335. [DOI] [PubMed] [Google Scholar]
- 34.Riley T, Hawe P. Researching practice: the methodological case for narrative inquiry. Health Educ Res. 2005;20(2):226–236. doi: 10.1093/her/cyg122. [DOI] [PubMed] [Google Scholar]
- 35.Bateman H, Bailey P, McLellan H. Of rocks and safe channels: learning to navigate as an interprofessional team. J Interprof Care. 2003;17(2):141–150. doi: 10.1080/1356182031000081740. [DOI] [PubMed] [Google Scholar]
- 36.Williams SJ, Calnan M. Perspectives on prevention: the views of general practitioners. Sociol Health Illn. 1994;16(3):372–393. [Google Scholar]


