Abstract
Background
The Vancouver Coastal Health Authority will initiate North America's first sanctioned safer injecting facility, as a pilot project, on Sept. 15, 2003. The analyses presented here were conducted to estimate the potential use of safer injecting facilities by local illicit injection drug users (IDUs) and to evaluate the potential impact of newly established Health Canada restrictions and current police activities on the use of the proposed facility.
Methods
During April and May 2003, we recruited active IDUs in Vancouver's Downtown Eastside to participate in a feasibility study. We used descriptive and univariate statistics to determine potential use of a safer injecting facility and to explore factors associated with willingness to use such a facility with and without federal restrictions and police presence.
Results
Overall, 458 street-recruited IDUs completed an interviewer-administered survey, of whom 422 (92%) reported a willingness to use a safer injecting facility. Those expressing willingness were more likely to inject in public (odds ratio [OR] 3.9, 95% confidence interval [CI] 1.9–8.0). When the restrictions in the Health Canada guidelines were considered, only 144 (31%) participants were willing to use a safer injecting facility. IDUs who inject alone were more likely (OR 1.8, 95% CI 1.0–3.1) and women were less likely (OR 0.6, 95% CI 0.4–0.9) to be willing to use a safer injecting facility operating under these restrictions. Only 103 (22%) of the participants said they would be willing to use a safer injecting facility if police were stationed near the entrance.
Interpretation
Most IDUs participating in this study expressed a willingness to use a safer injecting facility. However, willingness declined substantially when the IDUs were asked about using a facility operating under selected Health Canada restrictions and in the event that police were stationed near the entrance.
Many Canadian cities are experiencing an array of health and social harms as a result of illicit injection drug use, including epidemics of HIV, hepatitis C and overdose deaths.1,2,3 Health care costs due to injection-related bacterial infections also take a substantial toll on health care budgets.4,5 In other settings, where similar health crises have emerged, medically supervised safer injecting facilities, where injection drug users (IDUs) can inject previously obtained illicit drugs under the supervision of medical staff, have been implemented to reduce the community, public health and fiscal impacts of illicit drug use.6 Although safer injecting facilities vary considerably in design and function, evaluations conducted in Germany, Switzerland, Australia and the Netherlands indicate that such facilities have improved the health and social functioning of their clients,7 while reducing overdose deaths,8 HIV risk behaviours,7 improper disposal of syringes8 and use of drugs in public.9 In addition, improved access to medical care and drug treatment has been attributed to attendance at safer injecting facilities.6
In December 2002, following a federal task force's recommendation that safer injecting facility pilot projects proceed, Health Canada released guidelines for applying for a legal exemption to conduct such research studies.10 The Vancouver Coastal Health Authority recently received an exemption from Health Canada to conduct a sanctioned pilot study and intends to open a safer injecting facility on Sept. 15, 2003.11 The pilot facility will be open 18 hours a day, 7 days a week. It will have 12 private cubicles where IDUs can self-inject previously obtained drugs under the supervision of a registered nurse. Included in the Health Canada guidelines are a number of restrictions on the design and operation of safer injecting facility pilot sites, including prohibition of the sharing of drugs and prohibition of assisted injection. The guidelines also require that individuals register when using a safer injecting facility. These restrictions have been implemented primarily to limit the scope of the federal exemption to issues associated with the possession of illicit drugs in the facility and to reduce the risks associated with civil and criminal liability.
Previous studies have indicated that the use of safer injecting facilities may be limited when the service design includes many rules and restrictions.12,13 In addition, although the adverse effects of a police presence on access to health care services among IDUs has been well documented,14,15 the Vancouver Police Department is currently undertaking a controversial operation whereby police cruisers are at times parked outside local health services.16,17 Although willingness among Vancouver IDUs to use a safer injecting facility has been examined previously,18 the impacts of the newly established federal restrictions and current police activities have not been characterized. Therefore, we undertook a survey to estimate the potential use of a safer injecting facility by IDUs in Vancouver's Downtown Eastside and to evaluate how new federal restrictions and police activities might affect this potential use.
Methods
During April and May 2003, active IDUs were recruited for participation in a feasibility study of safer injecting facilities. The IDUs were informed of the study through street-based recruitment and “snowballing” methods and were eligible for inclusion if they reported being active IDUs (currently injecting illicit drugs), provided evidence of track marks and provided written informed consent. Participants completed an interviewer-administered survey in 1 of 3 Downtown Eastside locations: a rented storefront, a newly established Life Skills Centre and a large space that operates as a needle exchange site. A published definition of a medically supervised safer injecting facility18 was read to each participant, who was then shown 2 pictures of a facility similar to the model planned for Vancouver. Each study participant received $15 upon completion of the survey. The University of British Columbia/Providence Health Care Research Ethics Board approved the study.
Sociodemographic variables considered in these analyses included sex, age and housing status. In addition, because of the recent observation that Aboriginal IDUs in Vancouver are at heightened risk for HIV infection,1 ethnicity (Aboriginal or non-Aboriginal) was also examined. Unstable housing was defined as living in a single room occupancy hotel or shelters or having no fixed address. Drug use and behavioural variables were sex-trade work, number of previous overdoses, injecting in public spaces, requiring help injecting, injecting alone, and frequency of cocaine and heroin injection per day. Variables specific to safer injecting facilities included willingness to use such a facility and willingness to use a facility under 3 of the conditions stipulated by Health Canada's guidelines for a scientific pilot study: no sharing of drugs, no assisted injection and mandatory registration. More specifically, participants were told that a number of restrictions were being considered for safer injecting facilities and were then asked to indicate whether they would use a facility operating under each condition (e.g., “… if you were required to register to use the facility”). The survey further evaluated willingness to attend a safer injecting facility if police were stationed near the facility entrance.
We used descriptive and univariate statistics to determine potential use of safer injecting facilities and to explore factors associated with willingness to use a facility with and without the Health Canada restrictions. Categorical and explanatory variables were analyzed by means of Pearson χ2, normally distributed continuous variables were analyzed by means of t-tests for independent samples, and skewed continuous variables were analyzed with Mann–Whitney U-tests.
Results
In total, 458 active IDUs were recruited and completed questionnaires during April and May 2003. There were no refusals to participate in the study, although one IDU was unable to participate because of intoxication. The participants consisted of 197 women (43%) and 261 men (57%). Almost a third (149 or 32%) of the participants were of Aboriginal ancestry, the median age was 40 years, and 307 (67%) participants reported that they regularly injected in public places.
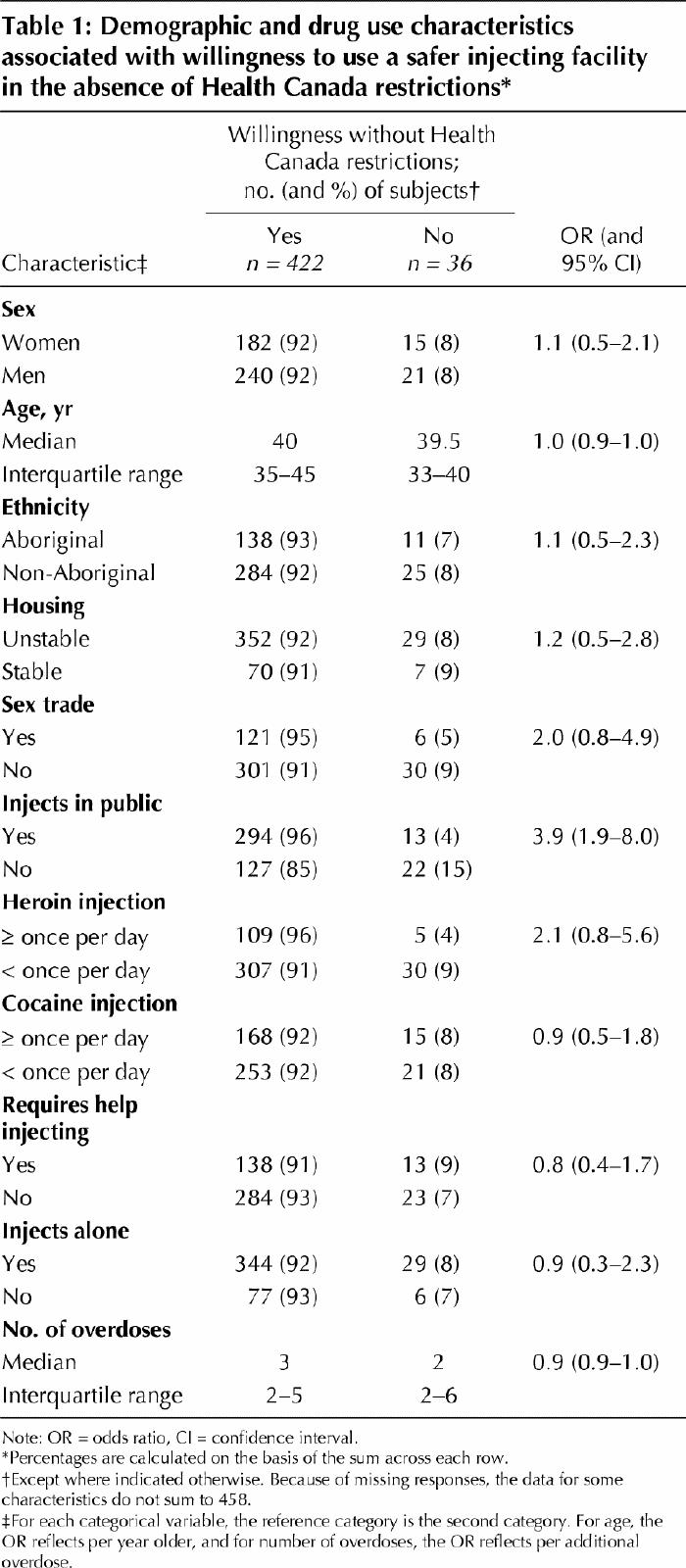
A total of 422 (92%) of the participants reported a willingness to use a safer injecting facility in the absence of Health Canada restrictions, and those expressing willingness were more likely to inject in public (odds ratio [OR] 3.9, 95% confidence interval [CI] 1.9–8.0) (Table 1). There were no differences in willingness to use a safer injecting facility with regard to any of the other characteristics examined (Table 1).
Table 1
Among the 422 participants (92%) who initially expressed willingness to use a safer injecting facility, 296 (64% of the total sample) were willing to use such a facility under a restriction prohibiting the sharing of drugs (Fig. 1). In bivariate analyses, injecting alone was associated with willingness under this restriction (OR 2.0, 95% CI 1.2–3.6), whereas female sex was associated with nonwillingness (OR 0.6, 95% CI 0.4–0.9).
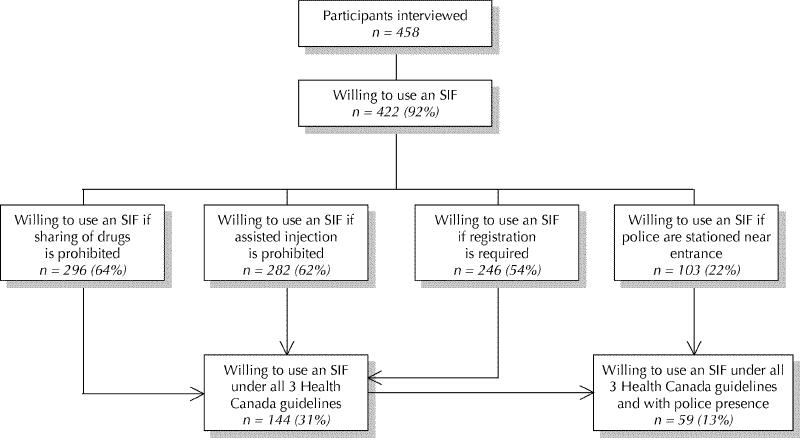
Fig. 1: Flow diagram illustrating initial willingness to use a safer injecting facility (SIF) and reductions in willingness related to Health Canada restrictions and police presence. All percentages are calculated on the basis of the complete sample of 458 survey participants.
Similarly, 282 participants (62% of the total sample) were willing to use a safer injecting facility under the restriction prohibiting assisted injection (Fig. 1). Injecting alone was also associated with willingness under this restriction (OR 1.8, 95% CI 1.1–2.9), whereas female sex (OR 0.4, 95% CI 0.3–0.7) and requiring help injecting (OR 0.4, 95% CI 0.2–0.6) were associated with nonwillingness.
Two hundred and forty-six participants (54% of the total sample) were willing to use a safer injecting facility under the restriction requiring client registration (Fig. 1). Aboriginal ethnicity (OR 1.6, 95% CI 1.0–2.4) and injecting in public (OR 1.6, 95% CI 1.0–2.3) were associated with willingness under this restriction.
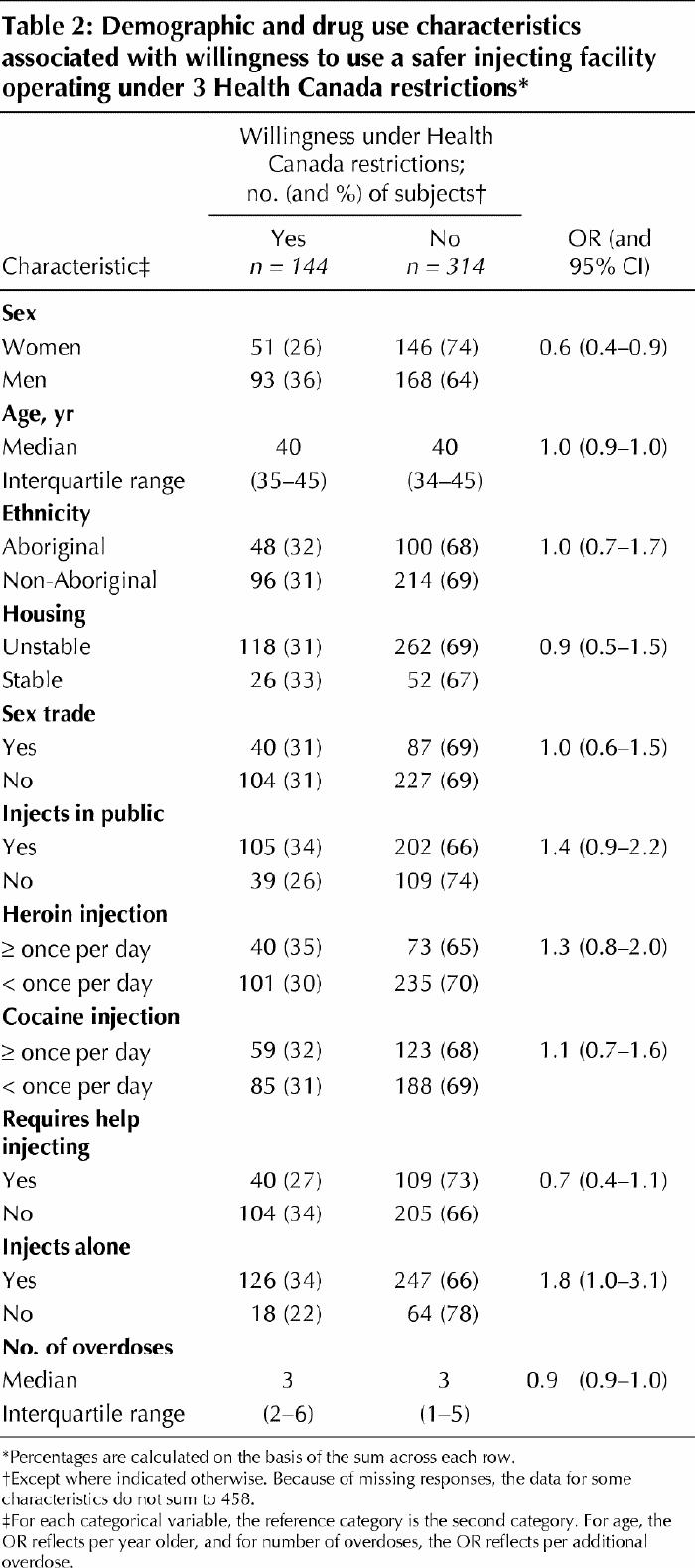
Finally, only 144 participants (31% of the total) were willing to use a safer injecting facility when the 3 Health Canada restrictions (no sharing of drugs, no assisted injection and mandatory registration) were considered together, on the basis of overlap for the 3 restrictions separately (Fig. 1, Table 2). Injecting alone was associated with willingness to use a facility under these restrictions (OR 1.8, 95% CI 1.0–3.1), whereas injecting in public was marginally associated with willingness (Table 2). Conversely, women were less likely to be willing to use a facility operating under these restrictions (OR 0.6, 95% CI 0.4–0.9) (Table 2).
Table 2
Only 103 (22%) of the participants said they would be willing to use a safer injecting facility if police were stationed near the entrance. About half of these (59 or 13% of the total) would be willing to use a safer injecting facility when all 3 Health Canada restrictions and police presence were considered together (on the basis of overlap). None of the variables under study were associated with willingness to use a safer injecting facility under the latter 2 scenarios.
Interpretation
In this study 92% of IDUs expressed willingness to use a medically supervised safer injecting facility, and injection of drugs in public was associated with willingness. However, willingness declined substantially when participants were asked if they would use a facility operating under 3 of the Health Canada restrictions. Study participants who inject alone were more likely and women were less likely to be willing to use a safer injecting facility operating under these restrictions. Only 22% of participants said they would use a safer injecting facility if police were stationed near the entrance.
The results of this study suggest that a safer injecting facility in Vancouver's Downtown Eastside could be well accepted by local IDUs, including those who inject in public. The latter finding, which is consistent with an earlier study involving Vancouver IDUs,18 is encouraging, given previous studies indicating that public injection is associated with an array of injection-related harms, including syringe-sharing, bacterial infection and overdose.19,20,21 However, our results differ from those of the earlier Vancouver study, in which only 36% of IDUs expressed willingness to use a safer injecting facility;18 the high rates of willingness observed here may be explained by the fact that, unlike IDUs in the earlier study, most participants in the current study were active street-based injectors and all were recruited from the heart of Vancouver's open drug scene in the Downtown Eastside. Our findings are consistent with an Australian study of IDU attitudes, which found that rules prohibiting the sharing of drugs and prohibiting assisted injection were associated with a substantial reduction in willingness to use a safer injecting facility.13 Although the overall decline in willingness is problematic, of particular concern was the finding that female sex was associated with unwillingness to use a safer injecting facility operating under specific restrictions, since the risk of HIV infection among female IDUs living in Vancouver is elevated.22 This negative impact of the restrictions on potential use of such facilities by women is not surprising, given that elevated rates of requiring help injecting have been associated with female sex.23 It should be noted that legal precedents indicate that operators of safer injecting facilities may be legally required to accommodate people with disabilities who are physically unable to self-inject by allowing them to obtain injection assistance from other IDUs in this supervised setting.24,25 The reduced willingness to use a safer injecting facility in the event of a police presence near the entrance is particularly worrisome. Previous studies in Vancouver have repeatedly indicated that police presence has had a negative impact on access to health care services,14,16,26 a finding that has also been demonstrated in the United States.15,27 For example, a recent Vancouver police operation was found to substantially reduce access to sterile syringes.14
Our study had several limitations. First, it offers evidence only of potential use of a safer injecting facility by IDUs; actual use can only be assessed once Vancouver's pilot study is under way. For instance, the adverse impact of Health Canada's restrictions may be overestimated in our study, as previous studies have indicated that IDUs will modify their behaviour in an effort to reduce harm to themselves and others.28 Nevertheless, the proposed single safer injecting facility in Vancouver might have difficulty meeting service needs, even in the event of restrictive guidelines and police presence.29 Second, this study relied on a convenience sample of IDUs recruited in Vancouver's Downtown Eastside, which might not be representative of IDU populations in other settings. Third, the study examined only a limited set of restrictions that might affect use of such a facility and may have neglected other restrictions that could limit use. Fourth, the age range of the active IDUs recruited in this study precluded an assessment of potential use of the safer injecting facility by youth. However, we feel that our sample is representative of the population targeted by the pilot project. Finally, the current study relies on self-reporting and therefore may be susceptible to socially desirable reporting.30
In summary, 92% of active IDUs in this study expressed an initial willingness to use a safer injecting facility. Those who expressed willingness were likely to be public injectors, suggesting the potential for immediate public health and public order benefits. However, willingness to use a safer injecting facility declined substantially when IDUs were asked if they would use a facility operating under Health Canada restrictions and in the event that police were stationed near its entrance. To maximize benefit, it is essential that safer injecting facilities be designed to address concerns regarding liability while making the service accessible to those at highest risk. In addition, the success of the safer injecting facility will probably require substantial modification of the potentially harmful law enforcement practices now in effect in Vancouver's Downtown Eastside.14,16,26
β See related articles pages 777 and 825
Acknowledgments
Anita Palepu is supported by a Canadian Institutes of Health Research New Investigator Award. Evan Wood is supported by the Michael Smith Foundation for Health Research.
Footnotes
Fast-tracked article. Published at www.cmaj.ca on Sept. 12, 2003.
This article has been peer reviewed.
Contributors: Thomas Kerr was the principal investigator of the study, and he coordinated the collection of the data, conducted the analyses and prepared the first draft of the manuscript. Thomas Kerr and Evan Wood designed the methodology for the paper. Evan Wood, Dan Small, Anita Palepu and Mark Tyndall provided input to the design of the survey questionnaire and the methodology and made critical comments and revisions to the content of the manuscript.
We acknowledge the contributions of Tomiye Ishida, Daniel Miles Kane, Dean Wilson, Calvin Lai and the Vancouver Area Network of Drug Users for their assistance with the study design and for administrative support.
We also acknowledge the assistance of Richard Elliot and Ruth Carey with the legal and policy analyses.
This research was funded by a Canadian Institutes of Health Research operating grant (Mark Tyndall, principal investigator).
Competing interests: None declared.
Correspondence to: Dr. Thomas Kerr, Canadian HIV/AIDS Legal Network, 417, rue Saint Pierre, Suite 408, Montréal QC H2Y 2M4; fax 514 397-8570; tkerr@aidslaw.ca
References
- 1.Craib KJP, Spittal PM, Wood E, Laliberte N, Hogg RS, Li K, et al. Risk factors for elevated HIV incidence among Aboriginal injection drug users in Vancouver. CMAJ 2003;168(1):19-24. [PMC free article] [PubMed]
- 2.Fischer B, Rehm J, Blitz-Miller T. Injection drug use and preventive measures: a comparison of Canadian and Western European jurisdictions over time. CMAJ 2000;162(12):1709-13. [PMC free article] [PubMed]
- 3.Wood E, Tyndall MW, Spittal PM, Li K, Kerr T, Hogg RS, et al. Unsafe injection practices in a cohort of injection drug users in Vancouver: Could safer injecting rooms help? CMAJ 2001;165(4):405-10. [PMC free article] [PubMed]
- 4.Palepu A, Tyndall MW, Leon H, Muller J, O'Shaughnessy MV, Schechter MT, et al. Hospital utilization and costs in a cohort of injection drug users. CMAJ 2001;165(4):415-20. [PMC free article] [PubMed]
- 5.Wood E, Kerr T, Spittal PM, Tyndall MW, O'Shaughnessy MV, Schechter MT. The healthcare and fiscal costs of the illicit drug use epidemic: the impact of conventional drug control strategies and the impact of a comprehensive approach. B C Med J 2003;45(3):130-6.
- 6.Broadhead RS, Kerr TH, Grund JP, Altice FL. Safer injection facilities in North America: their place in public policy and health initiatives. J Drug Issues 2002;32(1):329-55.
- 7.Ronco C, Spuhler G, Coda P, Schopfer R. Evaluation for street facilities I, II, and III in Basel [in German]. Soz Praventivmed 1996;41(Suppl 1):S58-68. [DOI] [PubMed]
- 8.Kemmesies UE. The open drug scene and the safe injection room offers in Frankfurt and Main 1995. Final report. Hamburg, Germany: European Cities on Drug Policy; 1999.
- 9.Dolan K, Kimber J, Fry C, Fitzgerald J, McDonald D, Frautmann F. Drug consumption facilities in Europe and the establishment of supervised injecting centres in Australia. Drug Alcohol Rev 2000;19:337-46.
- 10.Health Canada. Application for an exemption under section 56 of the Controlled Drugs and Substances Act for a scientific purpose for a pilot supervised injection site research project. Ottawa: Health Canada; 2002.
- 11.Injection site gets go-ahead: Health Canada approves three-year supervised injection trial in Downtown Eastside. Vancouver Sun 2003 June 25.
- 12.Fry C, Fox S, Rumbold G. Establishing safe injecting rooms in Australia: attitudes of injecting drug users. Aust N Z J Public Health 1999;23(5):501-4. [DOI] [PubMed]
- 13.Fry CL. Injecting drug user attitudes towards rules for supervised injecting rooms: implications for uptake. Int J Drug Pol 2002;13:471-6.
- 14.Wood E, Kerr T, Small W, Jones J, Schechter MT, Tyndall MW. The impact of police presence on access to needle exchange programs. J Acquir Immune Defic Syndr 2003;34(1):116-8. [DOI] [PubMed]
- 15.Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Med Anthropol 1997;18(1):61-83. [DOI] [PubMed]
- 16.Human Rights Watch. Canada: Abusing the user: police misconduct, harm reduction and HIV/AIDS in Vancouver [report online]. Hum Rights Watch Rep 2003;15(2B). Available: www.hrw.org/reports/2003/canada/canada0503.pdf (accessed 2003 Sep 6).
- 17.Human rights news. HRW letter to Mayor Larry Campbell. New York: Human Rights Watch; 2003 Jun 23. Available: www.hrw.org/press/2003/06/canada0623031-ltr.htm (accessed 2003 Sep 6).
- 18.Wood E, Kerr T, Spittal PM, Li K, Small W, Tyndall MW, et al. The potential public health and community impacts of safer injecting facilities: evidence from a cohort of injection drug users. J Acquir Immune Defic Syndr 2003; 32(1):2-8. [DOI] [PubMed]
- 19.Darke S, Kaye S, Ross J. Geographical injecting locations among injecting drug users in Sydney, Australia. Addiction 2001;96(2):241-6. [DOI] [PubMed]
- 20.Klee H, Morris J. Factors that characterize street injectors. Addiction 1995; 90 (6): 837-41. [DOI] [PubMed]
- 21.Latkin C, Mandell W, Vlahov D, Oziemkowska M, Knowlton A, Celentano D. My place, your place, and no place: behavior settings as a risk factor for HIV-related injection practices of drug users in Baltimore, Maryland. Am J Community Psychol 1994;22(3):415-30. [DOI] [PubMed]
- 22.Spittal PM, Craib KJ, Wood E, Laliberté N, Li K, Tyndall MW, et al. Risk factors for elevated HIV incidence rates among female injection drug users in Vancouver. CMAJ 2002;166(7):894-9. [PMC free article] [PubMed]
- 23.Wood E, Spittal P, Kerr T, Small W, O'Shaughnessy M, Schechter M. Requiring help injecting as a risk factor for HIV infection in the Vancouver epidemic: implications for HIV prevention. Can J Public Health. In press. [DOI] [PMC free article] [PubMed]
- 24.Eldridge v. Attorney General of British Columbia and the Medical Services Commission [1997] 3 S.C.R. 624.
- 25.Human Rights Code, R.S.O. 1990, c.H. 19 as amended. Available: 192.75.156.68/DBLaws/Statutes/English/90h19_e.htm (accessed 2003 Sep 9).
- 26.Wood E, Tyndall M, Spittal P, Li K, Hogg R, O'Shaughnessy M, Schechter M. Needle exchange and difficulty with needle access during an ongoing HIV epidemic. Int J Drug Pol 2002;13(2):95-102.
- 27.Rich JD, Strong L, Towe CW, McKenzie M. Obstacles to needle exchange participation in Rhode Island. J Acquir Immune Defic Syndr 1999;21(5):396-400. [PubMed]
- 28.Friedman SR, Des Jarlais DC, Sterk CE, Sotheran JL, Tross S, Woods J, et al. AIDS and the social relations of intravenous drug users [published erratum appears in Milbank Q 1990;68(1):142]. Milbank Q 1990;68(Suppl 1):85-110. [PubMed]
- 29.Kerr T, Wood E, Small D, Palepu A, Tyndall MW. Potential uptake and coverage of a safe injection site in Vancouver's Downtown Eastside [poster abstract]. In: 2nd International Conference on Urban Health; 2003 Oct 15–18; New York. In press.
- 30.Des Jarlais DC, Paone D, Milliken J, Turner CF, Miller H, Gribble J, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet 1999;353(9165):1657-61. [DOI] [PubMed]


