A previously healthy 12-year-old girl presented to her family doctor with a 4-day history of sore throat, fever and vomiting, preceded by an apparent cold sore on her right upper lip. Bacterial pharyngitis was diagnosed, and amoxicillin–clavulanate was prescribed, but the patient discontinued the medication after only 4 days because of gastrointestinal upset. On the eighth day of feeling unwell, the girl was brought to the local emergency department because of rigours, severe neck pain and an occipital headache. She was febrile (39.5°C) and had left-sided neck swelling and nuchal rigidity. A lumbar puncture was performed, and analysis of the cerebrospinal fluid (CSF) showed elevated leukocyte count (602 cells/mL [91% neutrophils]), 2 erythrocytes/mL and a slightly elevated protein level; glucose level and the results of gram staining were normal. Head CT revealed opacified left mastoid air cells. The patient was presumed to have partly treated meningitis. Blood samples were drawn for culture, and intravenous administration of vancomycin and cefotaxime was started.
The CSF culture results were all negative, but after 72 hours the blood samples grew penicillin-sensitive, filamentous, gram-negative bacilli identified as Fusobacterium necrophorum (Fig. 1). Both antibiotics were continued. After 48 hours of treatment (day 10 of the illness), drooling and left facial droop were noted. Neurologic examination confirmed palsies of the left fifth, seventh and eighth cranial nerves. MRI of the brain showed bilateral mastoiditis, worse on the left, as well as a “possible small early clot” in the left sigmoid sinus. A left tympanostomy tube was placed, and treatment with ciprofloxacin otic drops was initiated.
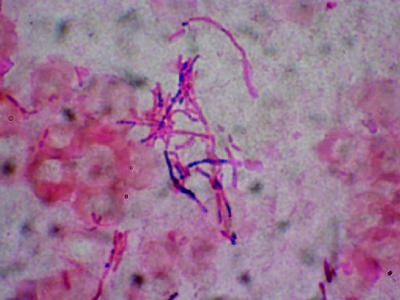
Figure 1. Photo: V. Boras, Department of Microbiology, Lethbridge Regional Hospital
Over the following week, the cranial nerve palsies resolved, the antibiotic therapy was discontinued, and the patient was discharged home. However, she continued to experience low-grade fatigue, anorexia and neck pain. Repeat MRI ordered as part of her 4-week follow-up and a subsequent magnetic resonance venogram (Fig. 2) demonstrated extensive thrombosis of the left transverse and sigmoid sinuses extending into the internal jugular vein and leading to a complete loss of venous blood flow. Lemierre syndrome was diagnosed on the basis of pharyngitis, confirmed F. necrophorum infection, mastoiditis and thrombophlebitis of the internal jugular vein. The patient underwent left mastoidectomy, during which only minimal residual inflammation was found. A 4-week course of intravenous piperacillin– tazomycin was initiated along with a 3-month course of subcutaneous low-molecular-weight heparin. The results of initial screening tests for systemic hyper- coagulability disorders were negative. Six weeks after the initial presentation, the patient was well, the results of a neurologic examination were normal, and follow-up MRI demonstrated no further clot extension.
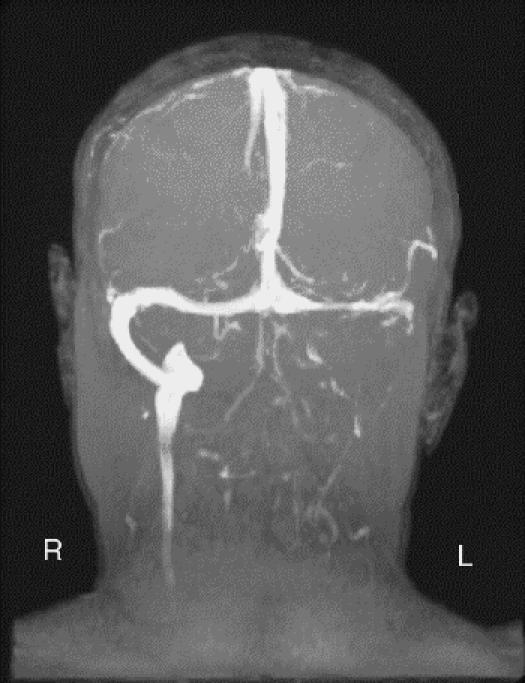
Figure 2. Photo: Department of Radiology, Alberta Children's Hospital.
Lemierre syndrome, or necrobacillosis, is a severe systemic infection with F. necrophorum. The first of the 3 classical stages is primary infection, usually of the throat or ear. Next, the tissue surrounding the lateral pharyngeal space is invaded, and thrombophlebitis of the internal jugular vein develops. Finally, there is metastatic spread of the bacteria, often associated with systemic coagulopathy.1 Lemierre originally described “pulmonary infarcts and arthritic manifestations,” which in the pre-antibiotic era resulted in a 90% mortality rate.2 F. necrophorum is ubiquitous in the normal oral flora, but these anaerobic gram-negative rods are sufficiently virulent to cause infection in immunocompetent hosts, and, worse, they produce an endotoxin that appears to promote coagulation.3 Although a recent literature review revealed 116 case reports of F. necrophorum infections, occurrence is likely underreported.1
In the patient described here, the “cold sore” may have provided the portal of entry, followed by the first stage of local infection, as evidenced by pharyngitis and fever. Swelling of the neck indicated the second stage, invasion of local tissue. The meningitis and venous thrombosis of the sigmoid sinus were most likely a result of migration of bacteria and bacterial endotoxin from the area of active infection into adjacent structures, as would be expected at the beginning of the third stage of the syndrome.
F. necrophorum infections may cause serious complications, including cranial nerve palsies, sinovenous thrombosis predisposing to venous infarction, sepsis and death.1,4,5 The complications experienced by this patient, mastoiditis and meningitis, have only rarely been reported in association with Lemierre syndrome.6,7 We felt that aggressive, long-term anaerobic antibiotic coverage was indicated in this patient, along with anticoagulation to treat the sinovenous thrombosis. Low-molecular-weight heparin has been used safely in children with sinovenous thrombosis and probably decreases the risk of clot extension, possibly shortening recovery times.8
This case of Lemierre syndrome highlights the perilous course of disease that can result from infection with F. necrophorum, a common oral anaerobe. F. necrophorum infection should be considered in any patient with a tender or swollen neck in association with pharyngitis. Management should include culture of blood and CSF for anaerobes, imaging to effectively diagnose the condition and appropriate anaerobic antibiotic coverage to prevent complications. A high index of suspicion is necessary to prevent morbidity and death from this serious infection in otherwise healthy patients.
Jacob L. Jaremko Radiology Resident University of Alberta Edmonton, Alta. Adam Kirton Pediatric Neurology Resident University of Calgary Calgary, Alta. Jennifer L. Brenner Clinical Assistant Professor and Pediatrician Alberta Children's Hospital Calgary, Alta.
References
- 1.Chirinos JA, Lichtstein DM, Garcia J, Tamariz LJ. The evolution of Lemierre syndrome: report of 2 cases and review of the literature. Medicine (Baltimore) 2002;81(6):458-65. [DOI] [PubMed]
- 2.Lemierre A. On certain septicemias due to anaerobic organisms. Lancet 1936;1:701-3.
- 3.Mandell G, Bennett J, Dolin R. Bacteroides, Prevotella, Porphyromonas, and Fusobacterium species. In: Principles and practice of infectious diseases. Philadelphia: Churchill Livingstone; 2000. p. 2561-8.
- 4.deVeber G, Andrew M. Cerebral sinovenous thrombosis in children. N Engl J Med 2001;345 (6): 417-23. [DOI] [PubMed]
- 5.Volturo GA, Repeta RJ Jr. Non-lower extremity deep vein thrombosis. Emerg Med Clin North Am 2001;19(4):877-93. [DOI] [PubMed]
- 6.Bader-Meunier B, Pinto G, Tardieu M, Pariente D, Bobin S, Dommergues JP. Mastoiditis, meningitis and venous sinus thrombosis caused by Fusobacterium necrophorum. Eur J Pediatr 1994; 153(5):339-41. [DOI] [PubMed]
- 7.Jones TH, Bergvall V, Bradshaw JP. Carotid artery stenoses and thrombosis secondary to cavernous sinus thromboses in Fusobacterium necrophorum meningitis. Postgrad Med J 1990;66 (779): 747-50. [DOI] [PMC free article] [PubMed]
- 8.deVeber G, Chan A, Monagle P, Marzinotto V, Armstrong D, Massicotte P, et al. Anticoagulation therapy in pediatric patients with sinovenous thrombosis: a cohort study. Arch Neurol 1998; 55 (12):1533-7. [DOI] [PubMed]


