Abstract
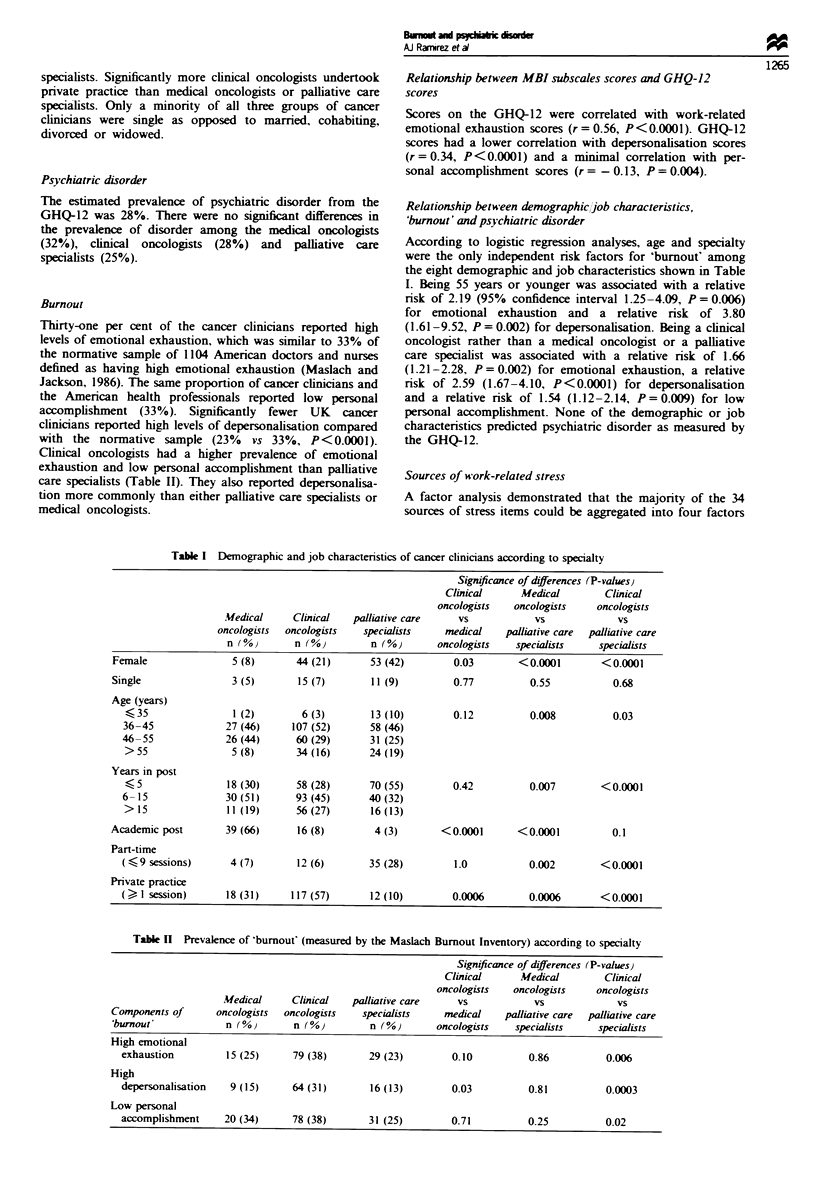
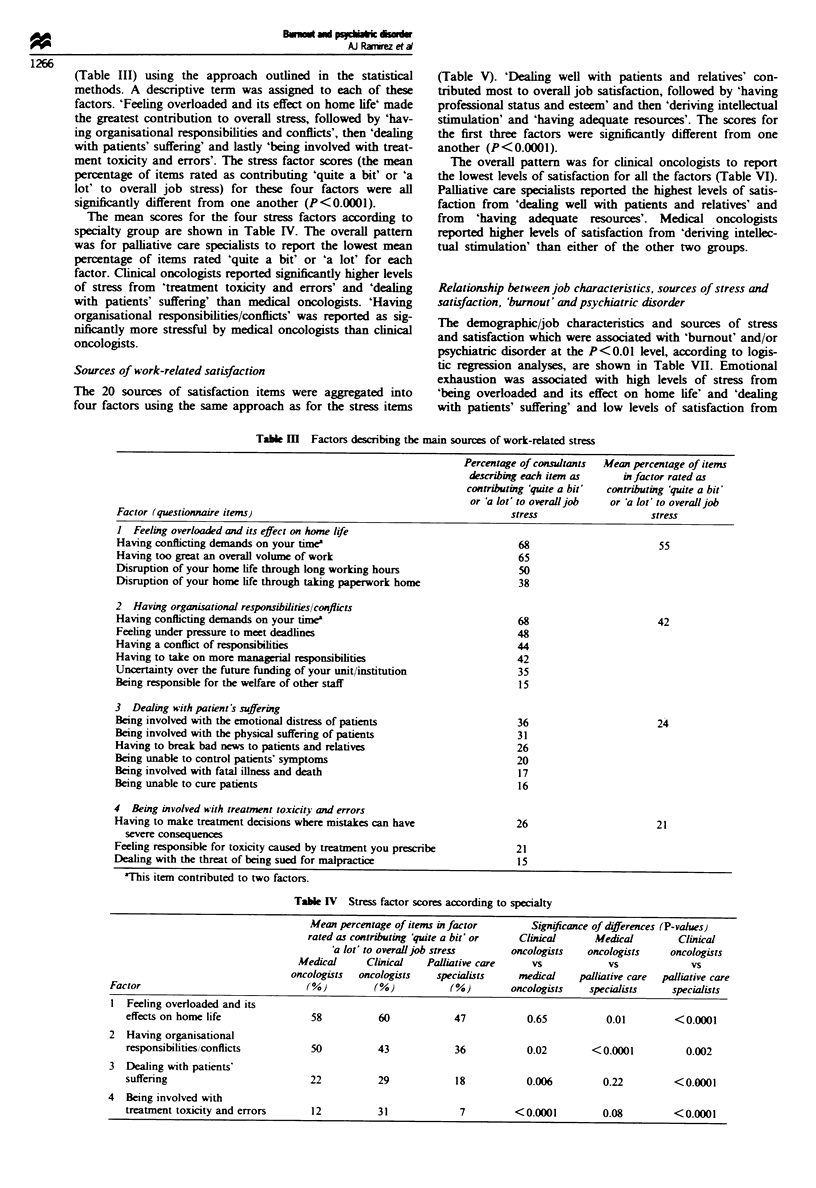
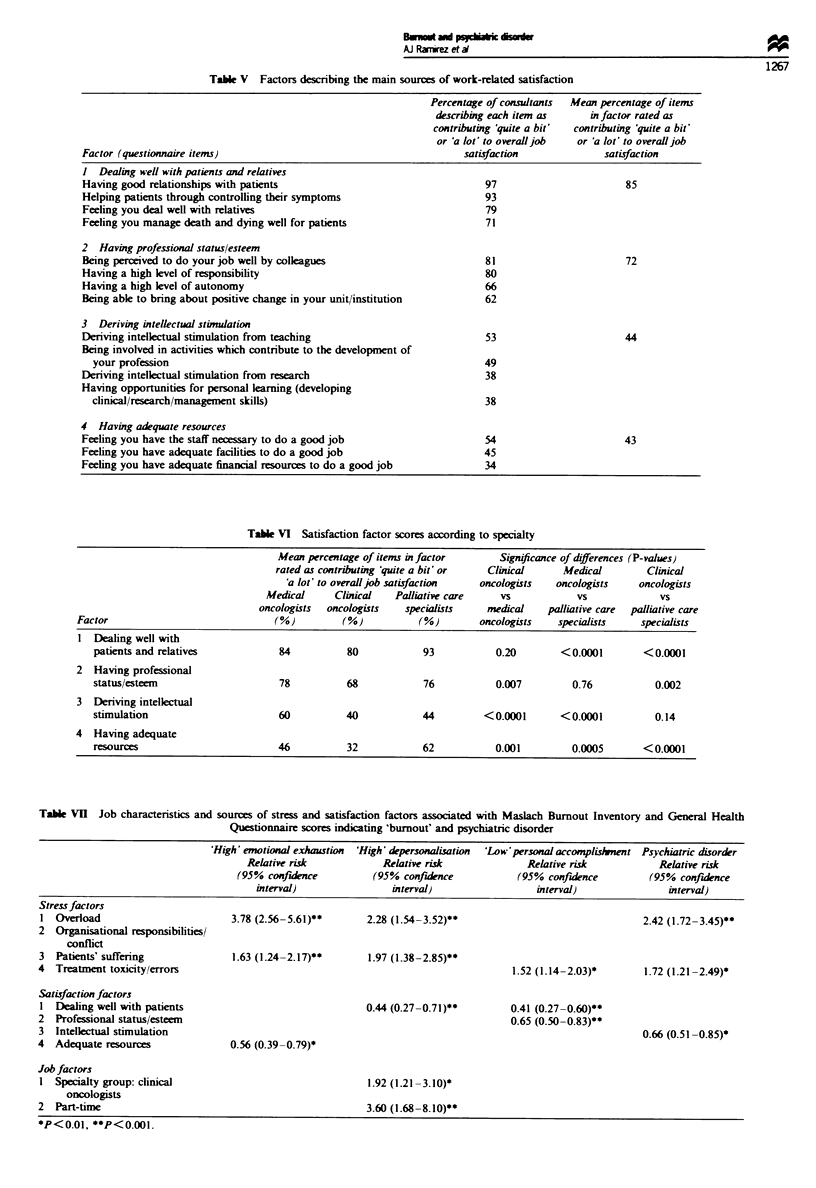
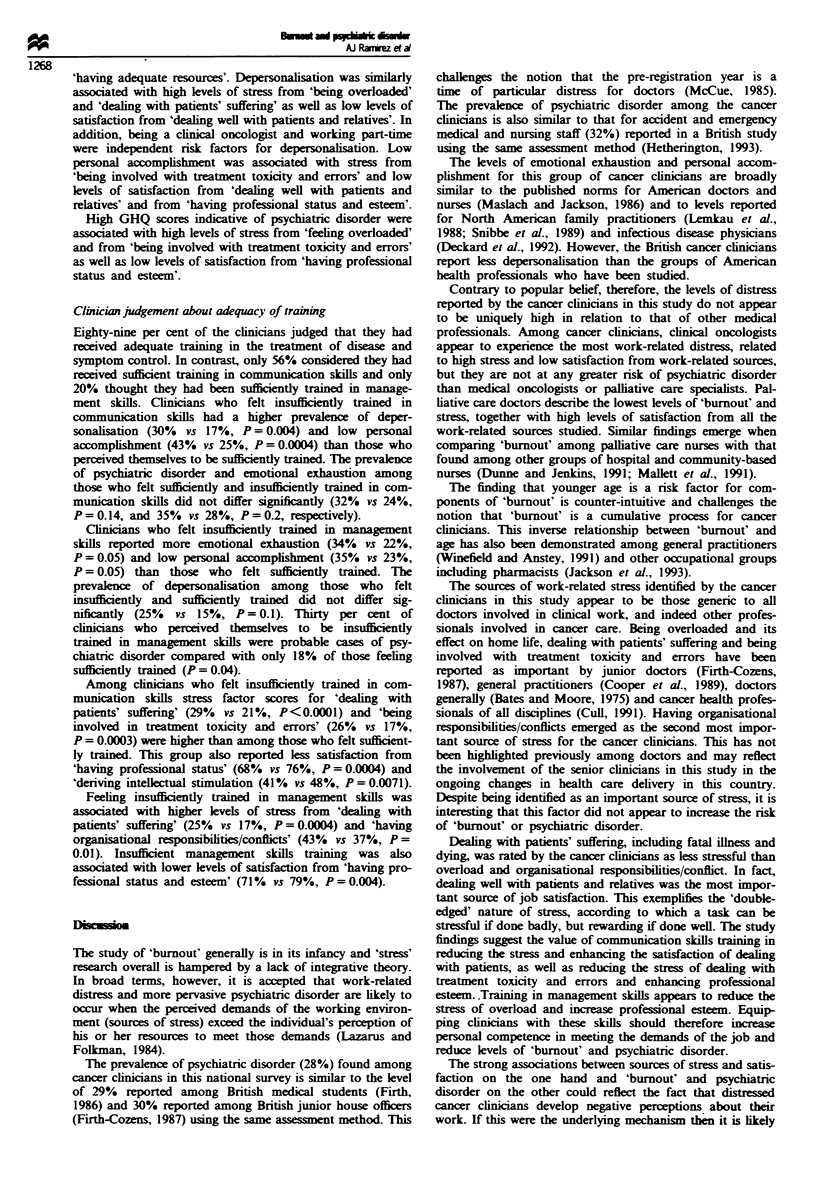
The prevalence and causes of 'burnout' and psychiatric disorder among senior oncologists and palliative care specialists have been measured in a national questionnaire-based survey. All consultant non-surgical oncologists in the UK were asked to participate. Sources of work-related stress and satisfaction were measured using study-specific questions which were aggregated into factors. Psychiatric disorder was estimated using the 12-item General Health Questionnaire. The three components of 'burnout'--emotional exhaustion, depersonalisation and low personal accomplishment--were assessed using the Maslach Burnout Inventory. Three hundred and ninety-three out of 476 (83%) consultants returned their questionnaires. The estimated prevalence of psychiatric disorder in cancer clinicians was 28%, and this is similar to the rate among British junior house officers. The study group had equivalent levels of emotional exhaustion and low personal accomplishment to those found in American doctors and nurses, but lower levels of depersonalisation. Among cancer clinicians, 'burnout' was more prevalent among clinical oncologists than among medical oncologists and palliative care specialists. Psychiatric disorder was independently associated with the stress of feeling overloaded (P < 0.0001), dealing with treatment toxicity/errors (P < 0.004) and deriving little satisfaction from professional status/esteem (P = 0.002). 'Burnout' was also related to these factors, and in addition was associated with high stress and low satisfaction from dealing with patients, and with low satisfaction from having adequate resources (each at a level of P < or = 0.002). Clinicians who felt insufficiently trained in communication and management skills had significantly higher levels of distress than those who felt sufficiently trained. If 'burnout' and psychiatric disorder among cancer clinicians are to be reduced, increased resources will be required to lessen overload and to improve training in communication and management skills.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bates E. M., Moore B. N. Stress in hospital personnel. Med J Aust. 1975 Nov 15;2(20):765–767. doi: 10.5694/j.1326-5377.1975.tb106276.x. [DOI] [PubMed] [Google Scholar]
- Cooper C. L., Rout U., Faragher B. Mental health, job satisfaction, and job stress among general practitioners. BMJ. 1989 Feb 11;298(6670):366–370. doi: 10.1136/bmj.298.6670.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cull A. M. Studying stress in care givers: art or science? Br J Cancer. 1991 Dec;64(6):981–984. doi: 10.1038/bjc.1991.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deckard G. J., Hicks L. L., Hamory B. H. The occurrence and distribution of burnout among infectious diseases physicians. J Infect Dis. 1992 Feb;165(2):224–228. doi: 10.1093/infdis/165.2.224. [DOI] [PubMed] [Google Scholar]
- Delvaux N., Razavi D., Farvacques C. Cancer care--a stress for health professionals. Soc Sci Med. 1988;27(2):159–166. doi: 10.1016/0277-9536(88)90324-3. [DOI] [PubMed] [Google Scholar]
- Firth-Cozens J. Emotional distress in junior house officers. Br Med J (Clin Res Ed) 1987 Aug 29;295(6597):533–536. doi: 10.1136/bmj.295.6597.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firth-Cozens J. Stress in medical undergraduates and house officers. Br J Hosp Med. 1989 Feb;41(2):161–164. [PubMed] [Google Scholar]
- Johnson W. D. Predisposition to emotional distress and psychiatric illness amongst doctors: the role of unconscious and experiential factors. Br J Med Psychol. 1991 Dec;64(Pt 4):317–329. doi: 10.1111/j.2044-8341.1991.tb01670.x. [DOI] [PubMed] [Google Scholar]
- Lemkau J. P., Purdy R. R., Rafferty J. P., Rudisill J. R. Correlates of burnout among family practice residents. J Med Educ. 1988 Sep;63(9):682–691. doi: 10.1097/00001888-198809000-00003. [DOI] [PubMed] [Google Scholar]
- Mallett K., Price J. H., Jurs S. G., Slenker S. Relationships among burnout, death anxiety, and social support in hospice and critical care nurses. Psychol Rep. 1991 Jun;68(3 Pt 2):1347–1359. doi: 10.2466/pr0.1991.68.3c.1347. [DOI] [PubMed] [Google Scholar]
- McCue J. D. The distress of internship. Causes and prevention. N Engl J Med. 1985 Feb 14;312(7):449–452. doi: 10.1056/NEJM198502143120725. [DOI] [PubMed] [Google Scholar]
- Rucinski J., Cybulska E. Mentally ill doctors. Br J Hosp Med. 1985 Feb;33(2):90–94. [PubMed] [Google Scholar]
- Snibbe J. R., Radcliffe T., Weisberger C., Richards M., Kelly J. Burnout among primary care physicians and mental health professionals in a managed health care setting. Psychol Rep. 1989 Dec;65(3 Pt 1):775–780. doi: 10.2466/pr0.1989.65.3.775. [DOI] [PubMed] [Google Scholar]
- Whippen D. A., Canellos G. P. Burnout syndrome in the practice of oncology: results of a random survey of 1,000 oncologists. J Clin Oncol. 1991 Oct;9(10):1916–1920. doi: 10.1200/JCO.1991.9.10.1916. [DOI] [PubMed] [Google Scholar]
- Winefield H. R., Anstey T. J. Job stress in general practice: practitioner age, sex and attitudes as predictors. Fam Pract. 1991 Jun;8(2):140–144. doi: 10.1093/fampra/8.2.140. [DOI] [PubMed] [Google Scholar]


