Abstract
OBJECTIVE
To systematically review the literature and to quantitatively compare outcomes and complications following retropubic versus transobturator approach to midurethral slings.
STUDY DESIGN
We searched PUBMED, OVID, EMBASE, CINAHL, POPLINE, Web of Science, Cochrane Collaboration resources, TRIP, Global Health databases and abstracts from relevant meetings from 1990–2006. We included all studies that compared retropubic and transobturator approaches to midurethral slings and defined outcomes. We used random effects models to estimate pooled odds ratios and 95% confidence intervals for objective and subjective failure, complications, and de novo irritative voiding symptoms.
RESULTS
Six randomized trials and eleven cohort studies compared transobturator and retropubic approaches to midurethral slings. There was insufficient evidence to support if one approach leads to better objective outcomes. We found no difference in subjective failure between the two approaches after pooling data from randomized trials (pooled OR 0.85 [95% CI, 0.38–1.92]). The transobturator approach was associated with a decreased risk of complications (pooled OR 0.40 [95% CI, 0.19 – 0.83]).
CONCLUSIONS
The transobturator approach to midurethral slings is associated with a lower risk of complications; however, it is still unclear if one approach results in superior objective or subjective outcomes.
Keywords: Midurethral sling, retropubic, transobturator, meta-analysis, systematic review
Introduction
Minimally invasive midurethral slings have changed the way many surgeons treat female stress urinary incontinence. Many of these midurethral slings are now performed under local anesthesia with short operative times, minimal dissection, and can be performed on an outpatient basis. The tension-free vaginal tape (TVT) was one of the first widely available retropubic (RP) midurethral slings and its ease of use has contributed to its popularity. Studies have reported an 80–85% cure rate following the RP approach at 2–5 years, comparable to the traditional bladder neck sling and Burch colposuspension.1, 2 Complication rates range from <1% to 7% and include bladder and other organ perforation, bleeding, voiding dysfunction and de novo irritative voiding symptoms.3 More recently, the transobturator (TO) approach was developed in an attempt to further minimize associated morbidity. Case series have demonstrated similar “cure” rates for the TO and the RP approach.4, 5 Although the TO approach has the advantage of avoiding the space of Retzius, with limited proximity to the peritoneal cavity and its contents, complications have been reported following this approach as well.6
Currently, there is limited data comparing complication rates or success rates between the two approaches. Current practice variation is often driven by local norms, experiences in training, influence of manufacturers, and individual surgeon preference instead of evidence based practice. The primary aims of this study were to systematically review the existing literature comparing RP and TO approaches to midurethral slings for stress urinary incontinence, and to compare objective outcomes, subjective outcomes and complications. The secondary aim was to evaluate differences in outcomes among subgroups of women with mixed incontinence, and those with intrinsic sphincter deficiency.
Material and Methods
A protocol was prospectively developed, detailing specific objectives, criteria for study selection, and approach to assessing study quality, outcomes and statistical methods, which is described below. This article was prepared in accordance with the QUOROM and MOOSE statements.7, 8 We used already published, de-identified data and thus this study was IRB exempt.
Sources
Searches were conducted in collaboration with two research librarians. We searched the literature from January 1, 1990, to April 26, 2006 using the following computerized databases: PUBMED, OVID, EMBASE, CINAHL, POPLINE, Web of Science, Cochrane Collaboration resources including the Cochrane Controlled Trials Registry, the Cochrane Database of Systematic Reviews, the Cochrane Incontinence Group’s registry, DARE, TRIP, Global Health, ClinicalTrials.gov, and CRISP. We used the MESH terms “urinary incontinence”, “surgical mesh” and “prosthesis” in combination. We also used the following search terms singly and in combination: sling, midurethral sling, retropubic, TVT, TOT, tension free tape, transobturator, transobturator tape, Monarc, ObTape, SPARC. Studies were also located by reviewing reference lists and bibliographies of selected articles. We hand-searched references of review articles and texts, and performed both web-based and hand searches of abstracts from relevant meetings (ICS 2001–2005, AUGS 2001–2005, SGS 2001–2006, IUGA 2004–2005), and consulted with experts in the field. Efforts were made to contact authors when additional information was needed. There were no language restrictions on our searches.
Study Selection
Abstracts of articles were assessed for relevance and those meeting eligibility criteria were included. The following criteria were used for study selection: (1) they were comparative studies (e.g. case-control, cohort, non-randomized controlled studies, or randomized controlled trials) of retropubic versus transobturator approach to midurethral polypropylene slings for stress urinary incontinence; (2) objective and/or subjective outcome measures were clearly defined; and (3) follow-up times were clearly defined. Studies were excluded if: (1) the report included duplicate cases, in which case the report containing the most complete data was included.
Data Extraction
Using a pre-specified data abstraction form, two reviewers (C.R.R. and R.M.W.) independently evaluated all articles and abstracted the following information: (1) study characteristics (year, design); (2) patient characteristics (number, demographics, clinical characteristics); (3) eligibility (definition of stress incontinence); (4) treatment (type of device and manufacturer); (5) duration of follow-up; (6) outcomes including: subjective and/or objective outcomes; perioperative complications (defined as hematoma, infection, vascular, bladder, or other organ injury); postoperative de novo irritative voiding symptoms (defined as new onset urinary urgency, frequency, or urge incontinence); and reoperation for voiding dysfunction; (7) odds ratios extracted or calculated from study data; (8) outcomes for women with intrinsic sphincter deficiency and mixed incontinence. A third author (V.W.S.) identified any discrepancies between the two reviewers, which were then reconciled among the three team members.
Statistical Analysis
We analyzed data from randomized trials and cohort studies separately to minimize methodological heterogeneity, and used the DerSimonian and Laird random-effects model to estimate odds ratios. We excluded studies that had dissimilar outcome measures from our pooled analyses. For zero-event data, we used 0.5 for computation of pooled odds ratios. We assessed statistical heterogeneity among studies using the Cochran Q statistic: P < .10 was considered to represent statistically significant heterogeneity. We assessed publication bias using funnel plots and Begg’s and Egger’s tests. Subgroup analyses planned a priori included: women with mixed incontinence and women with intrinsic sphincter deficiency.
We performed a series of sensitivity analyses to determine the robustness of our results. To determine if our results were driven by any single study we recalculated pooled results after systematically excluding each study individually. We repeated our analyses excluding studies with short term follow-up to determine if our results were temporally sensitive. To determine if our analyses were sensitive to the small size of included trials, we systematically changed event counts by one in each arm of each trial to see if this altered our findings. To quantify the potential effect of publication bias and the potential for our results to vary with future comparisons, we determined the characteristics needed for a hypothetical trial to qualitatively change our results. All analyses were performed using Microsoft Excel, 2002 and STATA 8.0 (Stata Corp, College Station, TX).
Results
Study Selection
Our search identified 303 reports, of which 280 were excluded on the basis of title/abstract due to lack of a comparative study design, missing control groups, or procedures other than RP or TO midurethral slings. Of the remaining 23 articles, 2 were excluded because “success”, either objective or subjective, was not clearly defined,9, 10 one article by de Tayrac et al was retracted by the journal11 and thus excluded from our analyses, and one had only one patient in the RP group12. When data was incomplete, we attempted to contact authors for further information. The remaining eligible studies included 6 randomized controlled trials 13–18 and 13 cohort studies.5, 19–30 Three of the cohort studies 21–23 reflected the same cohort of women, and thus only the study with the most updated and complete data was used.21 De novo irritative symptoms for this cohort of women were reported separately and this data was extracted from this paper.22 Therefore, data from a total of 18 studies was used in this review.
Overall, 492 women were randomized to receive either a TO or RP midurethral sling for stress urinary incontinence. Some trials included women with either stress or mixed incontinence.13, 14, 17, 18 Some trials specified which TO or RP device was used, but many did not. Follow-up times also varied, ranging from 1–15 months. Only one trial clearly stated that both patients and outcome assessors were blinded to treatment allocation; however, it is unclear how patients remained blinded to type of procedure.17 Study characteristics and outcomes are presented in Table I. When provided in the study, the name of the device used is listed in the table and includes Monarc and SPARC (American Medical Systems, Minnetonka, MN), TVT-O and TVT (Gynecare, Ethicon, USA), ISTOP (CL Medical, Lyon, France), Serasis-TO (Serag-Wiessner), SAFYRE (MedicService AG, Switzerland), Uratape (Porges), and ObTape (Mentor, USA).
Table I.
Characteristics of studies included in meta-analysis
| Source | Mean follow-up time | Objective Measure | Subjective Measure | No. participants included in analysis | Objective failure | Subjective outcome | Complications | De Novo urgency, frequency |
|---|---|---|---|---|---|---|---|---|
| Randomized Trials | ||||||||
| Porena,13 2005 | 13.4 months | Cough stress test | Dry, improved, failed | TO (42) | 1 | 33, 9, 0 | 2 | 1 |
| RP (47) | 3 | 33, 9, 5 | 5 | 5 | ||||
| Mansoor,14 2003 | 6.2 months | Not defined | Questionnaire: cured, failed | TO (48) | -- | 46, 2 | 0 | 1 |
| RP (54) | -- | 50, 4 | 6 | 10 | ||||
| Kim,15 2005 | “short term” | Negative cough stress test, pad test | Dry, improved, failed | TO-Monarc (21) | Not reported | 17, 4, 0 | 0 | Not reported |
| RP-SPARC (22) | Not reported | 17, 4, 0 | 1 | Not reported | ||||
| Enzelsberger,16 2005 | 15 months | Not defined | Cured, failed | TO (53) | -- | 45, 8 | 0 | 6 |
| RP (52) | -- | 45, 7 | 7 | 5 | ||||
| Wang,17 2005 | 6 months (median) | Improved pad weight | Not reported | TO-Monarc (31) | Pre pad weight: 31.8±31.0
Post pad weight: 8.6±21.4 |
-- | 0 | 8 |
| RP – SPARC (29) | Pre pad weight: 37.2±32.3
Post pad weight: 8.2±21.0 |
-- | 2 | 12 | ||||
| David-Montefiore,18 2005 | 1 month | Not defined | Dry, improved, failed | TO-Istop (46) | -- | 43, 1, 2 | 0 | 9 |
| RP -Istop (42) | -- | 39, 2, 1 | 9 | 10 | ||||
| Cohort Studies | ||||||||
| Kim,19 2005 | Short term | Not defined | Satisfied, failed | TO (12) | -- | 12, 0 | 0 | Not reported |
| RP (11) | -- | 10, 1 | 0 | Not reported | ||||
| Green,20 2005 | 8–10 months | Not defined | Dry, improved, failed | TO (35) | -- | 28, 3, 4 | 0 | 4 |
| RP (40) | -- | 32, 4, 3 | 3 | 5 | ||||
| Miller,21 2006 | 3.2 months | Urodynamics | Dry, failed | TO-Monarc (85) | 8 | 58, 11 | 0 | (based on Botros22, et al) 0/34 |
| RP-Gynecare (60) | 2 | 50, 7 | 1 | 10/39 | ||||
| Mellier,24 2004 | TOT – 12.8 months
TVT – 29.5 months |
Not reported | Dry, improved, failed | TO-Monarc (94) | -- | 89, 4, 1 | 2 | 4 |
| RP-Gynecare (99) | -- | 90, 7, 2 | 12 | 3 | ||||
| Fischer,25 2005 | >12 months | Success=pad test <2 grams | Not reported | TO-Monarc, Serasis (220) | 42 | -- | 1 | TOT – 3 |
| RP-Gynecare (220) | 53 | -- | 13 | 15 | ||||
| Palma,26 2005 | 14–18 months | Cough stress test | Dry, improved, failed | TO-SAFYRE (100) | 0 | 94, 2, 4 | 1 | 10 |
| RP-SAFYRE (126) | 0 | 116, 3, 7 | 9 | 26 | ||||
| Dietz,27 2005 | 9 months | Not reported | Dry or improved, or failed | TO-Monarc (58) | -- | 55, 3 | Not reported | Not reported |
| RP-Gynecare (56) | -- | 41,15 | Not reported | Not reported | ||||
| Ansquer,28 2004 | 1 month | Not reported | Dry, improved, failed | TO (variety of brands) (24) | -- | 20, 3, 1 | 3 | 1 |
| RP (25) | -- | 20, 5, 0 | 2 | 1 | ||||
| De Tayrac,29 2005 | 21–24 months | Cough stress test | Dry, failed | TO-Mentor Uratape (31) | 6 | 31, 0 | 0 | 4 |
| RP-Gynecare (18) | 3 | 18, 0 | 3 | 3 | ||||
| Neuman,30 2006 | 6 months | -- | Subjective outcomes, cough stress test, urodynamics: Cured, failed | TVT-O-Gynecare (75) | -- | 74, 1 | 0 | Not reported |
| RP-Gynecare (75) | -- | 73, 2 | 8 | Not reported | ||||
| Morey,5 2005 | 9–20 months | Not reported | Pad use=failed | TO – Monarc, ObTape (154) | -- | 36 | 0 | 2 |
| RP– Gynecare, SPARC (350) | -- | 70 | 5 | 21 |
TO = Transobturator approach RP = Retropubic approach
Outcomes may not add up to total participants due to loss to follow-up
There were a total of 2099 women who received either a TO or RP midurethral sling included in the 11 cohort studies. In a second article by deTayrac et al, which was not retracted, the authors specified inclusion of women with mixed incontinence. 29 Similar to the randomized trials, inclusion criteria, brand of device used, and follow-up times varied.
Objective outcomes
Only one randomized trial13 reported results for cough stress test; therefore, a pooled estimate was not obtained for objective outcomes for randomized trials. Four21, 25, 26, 29 of the eleven cohort studies reported objective outcomes with 56 failures out of 436 (12.8%) women who underwent TO and 58 failures out of 424 (13.7%) women who underwent the RP approach. Because these studies used different definitions of objective success, a pooled estimate was not obtained.
Subjective outcomes
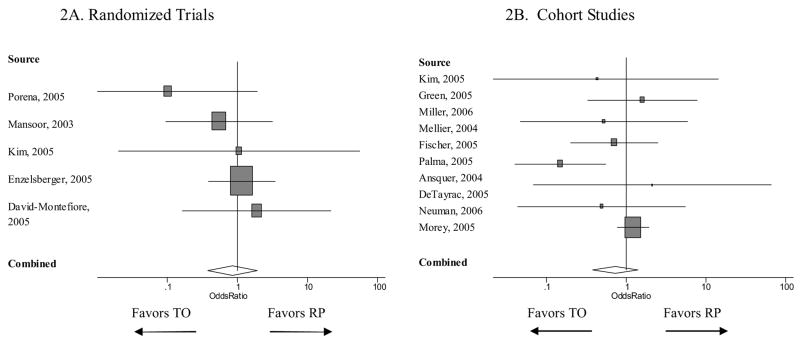
Subjective outcomes were reported in 5 of the 6 randomized trials and were defined by patient history and categorized by the authors as “dry”, “improved” and/or “failed”.13–16, 18 Using these categories, we defined subjective success as women who reported being either “dry” or “improved” and failures as women who were “unchanged or worse”. Overall, 12 women out of 210 (5.7%) who underwent TO and 17 women out of 217 (7.8%) who underwent the RP approach had subjective failures. The pooled OR for subjective failure in patients who underwent the TO compared to RP approach was 0.85 (95% CI, 0.38–1.92). See Figure 2A. These pooled results did not change when we defined subjective success as “dry” and failures as women who were “improved, unchanged or worse” (pooled OR 0.77, 95% CI, 0.37, 1.60). These results also did not change when we only included studies with greater than 1 year follow-up13, 16 (pooled OR 0.63, 95% CI 0.12–3.34). An additional randomized trial with a 5.7% TO and a 7.8% RP failure rate would require 1100 women in each arm for the pooled effect estimate to reach statistical significance favoring the TO approach.
Figure 2.
Risk of subjective failure after transobturator versus retropubic midurethral slings Abbreviations: TO, transobturator approach; RP, retropubic approach
Only 2 of the trials 13, 18 included validated quality of life measures (Incontinence Impact Questionnaire and Urogenital Distress Inventory) and there was insufficient data to perform pooled analyses for this outcome. Both of these studies reported improvement in quality of life scores post-operatively in both the TO and RP groups.
Subjective outcomes were reported in 10 of the 11 cohort studies and were defined in these studies by patient history and categorized by the authors as “dry”, “improved” and/or “failed”.5, 19–21, 24, 26–30 The method of obtaining subjective outcomes (face-to-face interview, telephone interview, survey) was inconsistent among these studies. We considered women categorized as being either “dry” or “improved” or “satisfied to very satisfied” as subjective successes and all others as failures. Neuman, et al reported outcomes that combined both symptoms and cough stress test and we decided to analyze this as a subjective outcome.30 Miller, et al and De Tayrac, et al dichotomized subjective outcomes into only dry or failed and therefore, these studies were excluded from this part of the analysis.21, 29 The remaining 8 studies were included in the pooled analysis. Overall, 86 out of 552 women (15.4%) who underwent TO and 100 out of 782 women (12.8%) who underwent the RP approach had subjective failures. The pooled OR for subjective failure in patients who underwent TO compared to RP approach was 0.73 (95% CI, 0.38–1.4). See Figure 2B. These findings did not change when we defined subjective cure as “dry”, and all others as failures, with a pooled OR of 0.83 (95% CI, 0.61–1.1). These results also did not change when we only included studies with greater than 1 year follow-up24, 26 (pooled OR 0.66, 95% CI 0.22–2.03). Finally, these findings also did not change when we compared TVT (Gynecare, Ethicon, USA) only to the TO approach and excluded studies that used SPARC or did not explicitly state type of RP device used,21, 24, 27, 29, 30 (pooled OR 0.52, 95% CI 0.21–1.29). Because of limited data, we were unable to perform analyses comparing SPARC alone to the TO approach.
Validated quality of life measures were reported in only 3 of the 11 cohort studies.25, 26, 29 Fischer et al utilized a German validated questionnaire31 and reported that 91% of women in the TO group and 88% in the RP group had improvement in their QOL scores.25 Palma et al utilized the International Consultation on Incontinence Questionnaire-short form and reported that 90% of all women in their study had improvement in all questions.26 De Tayrac et al utilized the Contilife Questionnaire and reported that improvement in scores were similar between the TO and RP groups.29 Because the 3 studies utilized different measures, pooled analyses were not performed for this outcome.
Finally, because our findings from both the randomized trials and cohort studies were almost identical for subjective failure, we performed a post-hoc sensitivity analysis, pooling the data from these studies. This did not change our findings and the pooled OR of subjective failure following the TO compared to the RP approach was 0.82 (95% CI 0.53, 1.27).
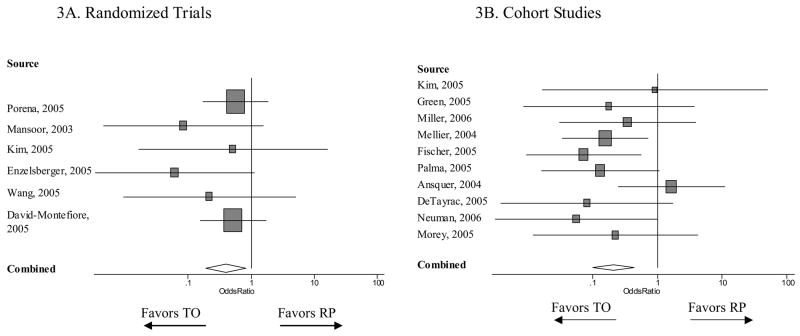
Perioperative complications
All six of the randomized trials provided data on perioperative complications. Overall, 2 out of 241 women (0.8%) who underwent TO and 30 out of 246 women (12.2%) who underwent the RP approach had complications. The pooled OR for complications in women who underwent TO compared to RP approach was 0.40 (95% CI, 0.19 – 0.83). See Figure 3A.
Figure 3.
Risk of complications after transobturator versus retropubic midurethral slings
Ten out of the eleven cohort studies reported data on complications.5, 19–21, 24–26, 28–30 Overall, 7 out of 830 women (0.8%) who underwent TO and 56 out of 1024 women (5.5%) who underwent the RP approach had complications. The pooled OR for complications in women who underwent TO compared to RP approach was 0.21 (95% CI, 0.10 – 0.44). See Figure 3B.
Among all studies, the most common complication was bladder perforation (3.5% in RP group, 0.2% TO group), followed by hematoma (1.6% RP group, 0.08% TO group), and infection (<1% both groups). There were no reports of other perforated organs. One study reported that 2 women returned to the operating room secondary to post-operative bleeding.25 Both women were in the RP group.
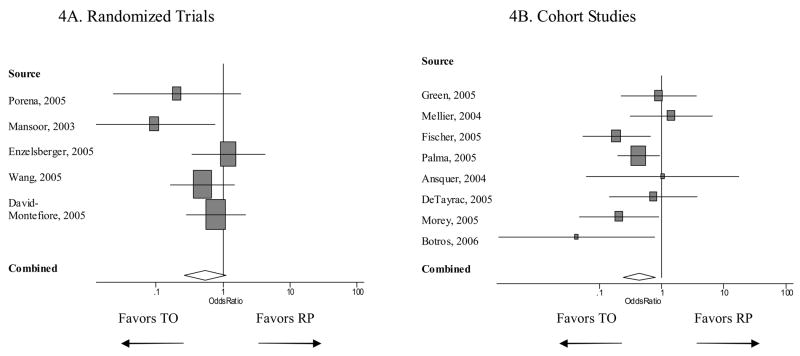
De novo irritative voiding symptoms
Five of the six randomized trials provided data on de novo irritative symptoms.13, 14, 16–18 Overall, 25 out of 220 women (11.4%) who underwent TO and 42 out of 224 women (18.8%) who underwent RP approach had de novo irritative symptoms. The pooled OR for de novo irritative voiding symptoms in patients who underwent TO compared to the RP approach was 0.54 (95% CI, 0.26–1.1). See Figure 4A. These results did not change when we only included those studies with >1 year follow-up (pooled OR 0.63, 95% CI 0.12–3.33).13, 16 An additional randomized trial with an 11.4% TO and 18.8% RP rate of de novo irritative symptoms would require 60 women in each arm for the pooled effect estimate to reach statistical significance favoring the TO approach.
Figure 4.
Risk of de novo irritative voiding symptoms after transobturator versus retropubic midurethral slings
Eight out of 11 cohort studies reported information on de novo irritative voiding symptoms.5, 20, 22, 24–26, 28, 29 Overall, 28 out of 692 women (4.1%) who underwent TO and 84 out of 917 women (9.2%) who underwent RP had de novo irritative symptoms. The pooled OR for de novo irritative voiding symptoms in patients who underwent TO compared to RP was 0.44 (95% CI 0.24–0.80). See Figure 4B. When we only included studies with > 1 year follow up, the pooled OR was 0.48 (95% CI 0.23 – 1.00).11, 24–26 29
Voiding dysfunction requiring reoperation
Only one randomized trial14 and six out of the eleven cohort studies5, 20, 25, 26, 29, 30 reported data on reoperation secondary to long-term voiding dysfunction. Overall this outcome was rare and therefore numbers were insufficient to pool results.
Mixed incontinence and intrinsic sphincter deficiency
Only two studies reported subgroup analyses and outcomes on women with preoperative mixed incontinence.13, 22 Similarly, only two studies reported subgroup analyses and outcomes on women with intrinsic sphincter deficiency.13, 21 These numbers were insufficient to pool results for either subgroup.
Sensitivity analyses and publication bias
Sensitivity analyses revealed that our findings were not driven by any single study and were not sensitive to small trial sizes. There was no evidence of statistical heterogeneity or publication bias for any of our analyses.
Comment
We found no difference in subjective failure between the transobturator and retropubic approaches to midurethral slings for female stress urinary incontinence. Some authors have hypothesized that the hammock nature of the TO approach decreases the risk of irritative voiding symptoms or voiding dysfunction;5, 27 however, we found that there is currently insufficient randomized trial evidence to support these claims. There is also not enough evidence to support that one approach leads to better outcomes in women with intrinsic sphincter deficiency or mixed incontinence.
We did find that women who undergo the TO approach are less likely to suffer from peri-operative hematoma, infection, vascular or bladder injury. However, the majority of peri-operative complications for the RP approach included bladder perforation, which often does not have long-term consequences. Therefore, these results should be treated with caution, especially given that there is no evidence to support if one approach has better objective or subjective outcomes. For both approaches, major peri-operative complications were rare. Although some studies reported on mesh erosion, we excluded this from the analysis because it was clear that not all studies included a pelvic exam at the time of outcome measurement, which sometimes were conducted by telephone interview, and were inconsistent in reporting this outcome. Mesh erosion is an important outcome that should be reported in long-term follow-up studies.
Our findings are consistent with most studies comparing these two approaches18, 25 in that most studies have not found a difference in subjective outcomes. However, this finding does not imply that outcomes of the two approaches are the same, only that the current data does not show these outcomes are different. This is an important distinction to be considered, as most studies have not been designed to demonstrate equivalence between the two approaches. Ultimately, current selection of operative technique is based on limited comparative data on the failure rates of the two techniques.
Using the information in this study, we calculated sample size estimates required for demonstrating equivalence between the TO and RP approaches. Assuming a subjective failure rate of 5.7% for the TO approach found in randomized trials and defining equivalence as an absolute difference of <0.5% between the two approaches, an additional randomized trial would require 15,000 women with 885 failures in each arm to demonstrate equivalence between these two approaches for subjective failure. Combined with the randomized trials in this study, the pooled OR would be 1.00 (95% CI 0.91, 1.08). We recognize that these assumptions are conservative. Using less strict definitions, assuming a subjective failure rate of 10% and defining equivalence as an absolute difference of <5% between the two approaches, an additional trial would require 250 women with 25 failures in each arm to demonstrate equivalence for subjective failure. Combining this hypothetical study with the randomized trials, the pooled OR would be 0.95 (95% CI 0.61, 1.52), demonstrating equivalence between the two approaches.
We found that the reporting of inclusion criteria, indications for surgery, and defined outcomes to be highly variable among the studies. Future studies should include manufacturer information, clear definitions and standardized measures of both objective and subjective outcomes as well as systematic postoperative assessments of complications, mesh erosion, de novo irritative voiding symptoms, and voiding dysfunction, and long term follow-up. Outcomes should be stratified by important clinical variables. Future studies should also report short and long term outcomes separately instead of combining these outcomes together.
There are potential weaknesses to our study. First, although we did establish predefined criteria for study selection, the quality of our study is dependent on the quality of the included studies. For example, retrospective cohort studies are subject to selection bias. Also, the quality of included trials was often unclear and at times we were unable to identify blinding of outcome assessors and randomization allocation methods. Additionally, because the randomized trials were all fairly small in size, authors were unable to adjust for potential confounders. Second, the studies included different brands of midurethral slings and although there is currently limited evidence to support one brand over another, this may contribute to clinical heterogeneity of the studies. Recent studies may suggest that outcomes following SPARC may be inferior to TVT.32, 33 Although the primary aim of this study was to compare different approaches and not different manufacturers, we did perform sensitivity analyses comparing TVT alone to the RP approach, excluding studies that used SPARC, which did not significantly alter our findings. Third, follow-up times were variable between the studies. However, sensitivity analyses demonstrated that our findings were fairly consistent when only studies with greater than 1 year follow-up were included. Finally, we were unable to obtain some of the missing data from all studies despite attempts at contacting authors, requiring exclusion of some studies in our analyses.
In conclusion, the transobturator approach to midurethral slings is associated with a decreased risk of complications; however, there is currently no evidence to suggest that one approach results in superior objective or subjective outcomes. Methodologically rigorous studies are needed comparing the transobturator and retropubic approaches to midurethral slings for the treatment of female stress urinary incontinence.
Figure 1.

Study selection flow chart
Acknowledgments
The authors would like to thank William Anger and Janet Crager for their assistance in the search and identification of articles used in this study.
Supported in part by grant 5-K12-HD050108-02; WIH/Brown Women’s Reproductive Health Research Career Development Award; National Institute of Child Health and Human Development.
Footnotes
Reprints are not available.
Condensation: The transobturator approach to midurethral slings is associated with a lower risk of complications; however, it is still unclear if one approach results in superior objective or subjective outcomes.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Nilsson CG, Kuuva N, Falconer C, Rezapour M, Ulmsten U. Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(Suppl 2):S5–8. doi: 10.1007/s001920170003. [DOI] [PubMed] [Google Scholar]
- 2.Ward KL, Hilton P. A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: two-year follow-up. Am J Obstet Gynecol. 2004;190:324–31. doi: 10.1016/j.ajog.2003.07.029. [DOI] [PubMed] [Google Scholar]
- 3.Karram MM, Segal JL, Vassallo BJ, Kleeman SD. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol. 2003;101:929–32. doi: 10.1016/s0029-7844(03)00122-4. [DOI] [PubMed] [Google Scholar]
- 4.Delorme E, Droupy S, de Tayrac R, Delmas V. Transobturator tape (Uratape): a new minimally-invasive procedure to treat female urinary incontinence. Eur Urol. 2004;45:203–7. doi: 10.1016/j.eururo.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Morey AF, Medendorp AR, Noller MW, et al. Transobturator versus transabdominal mid urethral slings: a multi-institutional comparison of obstructive voiding complications. J Urol. 2006;175:1014–7. doi: 10.1016/S0022-5347(05)00412-X. [DOI] [PubMed] [Google Scholar]
- 6.Boyles SH, Edwards R, Gregory W, Clark A. Complications associated with transobturator sling procedures. Int Urogynecol J Pelvic Floor Dysfunct. 2006 doi: 10.1007/s00192-006-0091-0. [DOI] [PubMed] [Google Scholar]
- 7.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354:1896–900. doi: 10.1016/s0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 8.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. Jama. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 9.Cotte B, Dumousset E, Boda C, Mansoor A. [Comparison of transobturator tape (TO) and tension-free vaginal tape (TVT) using perineal ultrasound] Gynecol Obstet Fertil. 2006;34:298–303. doi: 10.1016/j.gyobfe.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Palanca ABPF, Beltran Meseguer JF, Zaragoza Q, Claramunt JE, Sempere FP. [Comparison of different suburethral slings for the treatment of stress urinary incontinence] Actas urologicas Espanolas. 2005;29:757–763. doi: 10.1016/s0210-4806(05)73337-4. [DOI] [PubMed] [Google Scholar]
- 11.de Tayrac RDX, Droupy S, Chauveaud-Lambling A, Calvanese-Benamour L, Fernandez H. A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol. 2004;190:602–8. doi: 10.1016/j.ajog.2003.09.070. [DOI] [PubMed] [Google Scholar]
- 12.Oliveira LMGM, Sartori MGF, Castro RA, Fonseca ESM. Comparison of retropubic TVT, pre-pubic TVT and TVT transobturator in surgical treatment of women with stress urinary incontinence. Presented at IUGA; 2005. [Google Scholar]
- 13.Porena MKE, Costantini E, Cecchetti G, Bini V, Crivellaro S, Frea B. Tension free vaginal tape vs transobturator tape as surgery for stress urinary incontinence: Results of a multicentre randomised trial. As presented at ICS 2005 as a podium presentation abstract; 2005. [Google Scholar]
- 14.Mansoor AVN, Darcq C. Surgery of female urinary incontinence using transobturator tape (TO): A prospective randomised comparitive study with TVT. Neurourology and Urodynamics. 2003;22:88. [Google Scholar]
- 15.Kim Y-WNY, Sul CK. Randomized prospecive study between pubovaginal sling using SPARC sling system and MONARC sling system for the treatment of female stress urinary incontinence: Short term results. Korean Journal of Urology. 2005;46:1078–1082. [Google Scholar]
- 16.Enzelsberger HSJ, Heider R, Mayer G. TVT versus TO - A prospective randomized study for the treatment of female stress urinary incontinence at a follow-up of 1 year. Geburtshilfe und Frauenheilkunde. 2005;65:506–511. [Google Scholar]
- 17.Wang AC, Lin YH, Tseng LH, Chih SY, Lee CJ. Prospective randomized comparison of transobturator suburethral sling (Monarc) vs suprapubic arc (Sparc) sling procedures for female urodynamic stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2005:1–5. doi: 10.1007/s00192-005-0035-0. [DOI] [PubMed] [Google Scholar]
- 18.David-Montefiore E, Frobert JL, Grisard-Anaf M, et al. Peri-operative complications and pain after the suburethral sling procedure for urinary stress incontinence: a French prospective randomised multicentre study comparing the retropubic and transobturator routes. Eur Urol. 2006;49:133–8. doi: 10.1016/j.eururo.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 19.Kim YBJY, Jee BC, Park KH, Suh CS. The efficacy and safety of tension-free vaginal tape and transobturator suburethral tape in the surgical management of stress urinary incontinence. Presented at IUGA; 2005. [Google Scholar]
- 20.Green JBD, Herschorn S. A comparison of the transobturator tape and transabdominal tension free vaginal tape procedures for the surgical treatment of stress urinary incontinence. presented at ICS 2005 abstract. [Google Scholar]
- 21.Miller JBS, Akl MN, Goldberg RP, Sand PK. Is transobturator tape as effective as tension free vaginal tape in patients with a borderline maximal urethral closure pressure? J Pelvic Med and Surg. 2006;12:68. doi: 10.1016/j.ajog.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 22.Botros SMMJ, Akl M, Goldberg RP, Sand PK. Detrusor overactivity and urge incontinence in Monarc versus TVT and SPARC. J Pelvic Med and Surg. 2006;12:89. [Google Scholar]
- 23.Miller JBS, Akl MN, Beaumont JL, Goldberg RP, Abramov Y, Sand PK. Comparing stress urinary outcomes of tension free vaginal tape with transobturator tape sling: A retrospective cohort study. As presented at ICS 2005 abstract. [Google Scholar]
- 24.Mellier G, Benayed B, Bretones S, Pasquier JC. Suburethral tape via the obturator route: is the TO a simplification of the TVT? Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:227–32. doi: 10.1007/s00192-004-1162-8. [DOI] [PubMed] [Google Scholar]
- 25.Fischer A, Fink T, Zachmann S, Eickenbusch U. Comparison of retropubic and outside-in transoburator sling systems for the cure of female genuine stress urinary incontinence. Eur Urol. 2005;48:799–804. doi: 10.1016/j.eururo.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 26.Palma P, Riccetto C, Herrmann V, et al. Transobturator SAFYRE sling is as effective as the transvaginal procedure. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:487–91. doi: 10.1007/s00192-005-1309-2. [DOI] [PubMed] [Google Scholar]
- 27.Dietz HP, Barry C, Lim Y, Rane A. TVT vs Monarc: a comparative study. Int Urogynecol J Pelvic Floor Dysfunct. 2006 doi: 10.1007/s00192-006-0065-2. [DOI] [PubMed] [Google Scholar]
- 28.Ansquer Y, Marcollet A, Yazbeck C, et al. The suburethral sling for female stress urinary incontinence: a retropubic or obturator approach? J Am Assoc Gynecol Laparosc. 2004;11:353–8. doi: 10.1016/s1074-3804(05)60050-3. [DOI] [PubMed] [Google Scholar]
- 29.de Tayrac R, Deffieux X, Resten A, Doumerc S, Jouffroy C, Fernandez H. A transvaginal ultrasound study comparing transobturator tape and tension-free vaginal tape after surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2005:1–6. doi: 10.1007/s00192-005-0043-0. [DOI] [PubMed] [Google Scholar]
- 30.Neuman M. TVT and TVT-Obturator: Comparison of two operative procedures. Eur J Obstet Gynecol Reprod Biol. 2006 doi: 10.1016/j.ejogrb.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 31.Bong JdGG, Schuth W. Quality of Life-Fragebogen bei Patientinnen mit Harninkontinenz. Geburtsh u Frauenheilk. 1998;58:597–604. [Google Scholar]
- 32.Lord HE, Taylor JD, Finn JC, et al. A randomized controlled equivalence trial of short-term complications and efficacy of tension-free vaginal tape and suprapubic urethral support sling for treating stress incontinence. BJU Int. 2006;98:367–76. doi: 10.1111/j.1464-410X.2006.06333.x. [DOI] [PubMed] [Google Scholar]
- 33.Gandhi S, Abramov Y, Kwon C, et al. TVT versus SPARC: comparison of outcomes for two midurethral tape procedures. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:125–30. doi: 10.1007/s00192-005-1369-3. [DOI] [PubMed] [Google Scholar]