Abstract
Few prospective studies have examined the relation between early adolescent conduct disorder symptoms and the development of alcohol use disorders (AUD) by young adulthood. The relative contribution of other forms of adolescent psychopathology (i.e., attention-deficit hyperactivity disorder, depression, anxiety/withdrawal) to the development of AUD also remains poorly understood. There is some suggestion that the co-occurrence of conduct disorder symptoms with other forms of psychopathology may interact synergistically in predicting later alcohol use problems. The current study explores these issues using data on 506 boys from the oldest sample of the Pittsburgh Youth Study. Consistent with prior research, early conduct disorder symptoms emerged as a consistent predictor of increased AUD symptoms and an alcohol dependence diagnosis by young adulthood. In contrast, adolescent boys with high levels of anxiety/withdrawal had lower levels of AUD symptoms and were less likely to develop alcohol dependence by young adulthood. Increased depression in early adolescence was associated with higher AUD symptoms and alcohol abuse and dependence diagnoses by young adulthood, but only for boys with high levels of conduct disorder symptoms. No evidence was found for a relation between attention-deficit hyperactivity disorder symptoms and AUD symptoms or diagnoses after controlling for co-occurring psychopathology.
Keywords: alcohol use disorders, anxiety, depression, conduct disorder, ADHD
1. Introduction
There has been an increased interest in examining the relation between early adolescent psychopathology and the development of alcohol use disorders in adulthood. Longitudinal research indicates that behaviors consistent with conduct disorder (CD) symptoms (e.g., aggression, deceitfulness/theft, destruction of property, serious rule violations) are associated with more frequent and intense alcohol use across time (Henry et al., 1993; Miller-Johnson et al., 1998; White et al., 1999), as well as early-onset substance use disorders (for a review see Weinberg et al., 1998). Given the robustness of this relation, some investigators have postulated that early CD symptoms represent the phenotypic expression of a genetically inherited liability for substance use disorders (Tarter et al., 1999). However, there remains substantial heterogeneity among youth with elevated CD symptoms, and evidence indicates that early internalizing problems (e.g., depression, anxiety/withdrawal) and attention-deficit/hyperactivity disorder (ADHD) symptoms may also predict later alcohol use outcomes (Henry et al., 1993; Kaplow et al., 2001; Molina & Pelham, 2003; Pardini et al., 2004). In addition, the cooccurrence of CD symptoms with other forms of early psychopathology may actually identify those adolescents who are at highest risk for later substance use problems (Flory et al., 2003; Miller-Johnson et al., 1998). The goal of the current study will be to examine the relative contribution of different forms of early adolescent psychopathology in predicting AUD by young adulthood. We will also examine the potential interactive effects between early conduct problems and other forms of adolescent psychopathology in identifying boys who are most at risk for later AUD.
1.1 CD Symptoms and Alcohol Use Disorders
There is a substantial amount of evidence indicating that symptoms of CD and substance use disorders tend to co-occur across adolescence (Weinberg et al., 1998). In fact, early substance use is often included as an additional indicator of conduct problems in childhood and adolescence rather than treating the two as separate, yet related, problems (Angold & Costello, 2001). Despite this overlap, longitudinal evidence suggests that adolescent CD symptoms and substance using behaviors represent two distinct dimensions of behavior (Mason & Windle, 2002) that have some unique predictive factors (White et al., 1987). Behaviors consistent with CD symptoms in boys also predict the onset of alcohol use (Clark et al., 1999), escalations in substance using behaviors (Mason & Windle, 2002), and the development of substance use disorders in adolescence (Sung et al., 2004). However, many longitudinal studies in this area have followed boys across relatively brief periods in adolescence and do not account for the influence of other forms of psychopathology that tend to co-occur with both disorders. There is also a dearth of studies examining the interaction between early adolescent conduct disorder symptoms and other forms of externalizing and internalizing psychopathology in predicting the development of alcohol use disorders by young adulthood.
1.2 ADHD and Alcohol Use Disorders
There is ongoing debate about the relation between early ADHD symptoms and later substance use outcomes. Investigations have found that ADHD symptoms are more prevalent in adolescents and adults with substance use disorders than in the general population (for a review see Wilens, 2004). Longitudinal studies have found that children and adolescents exhibiting behaviors consistent with ADHD have high levels of later alcohol use, including more problem use, in comparison to normal control children (Barkley et al., 1990; Molina & Pelham, 2003; Pulkkinen & Pitkänen, 1994). However, many longitudinal studies have found that the relation between ADHD symptoms and later substance use is primarily driven by co-occurring conduct problems (Barkley et al., 1990; Biederman et al., 1997; Clark et al., 1999; Loeber et al., 1999; Pulkkinen & Pitkänen, 1994). While recent investigations with clinic-referred youth suggest that childhood inattentive symptoms may predict adolescent substance use outcomes above and beyond conduct disorder symptoms (Molina & Pelham, 2003), this finding may only be relevant for cigarette use (Burke et al., 2001). In addition, prospective investigations exploring the relation between early adolescent ADHD symptoms and the development of alcohol use disorders remain rare.
Some investigators have suggested that ADHD symptoms may escalate the risk for negative substance use outcomes only in youth with high levels of CD symptoms (Flory & Lynam, 2003; Molina et al., 1999). Much of this conjecture comes from longitudinal studies indicating that children with high levels of both ADHD and CD symptoms are more likely to exhibit severe and persistent forms of antisocial behavior in comparison to youth with ADHD or CD symptoms alone (for a review see Flory & Lynam, 2003). The relatively few studies examining the interactive effects between ADHD and CD symptoms in predicting substance use outcomes have provided mixed results. Molina et al. (1999) found that children with a comorbid ADHD and CD diagnosis were more likely to report using several substances in comparison to children with either disorder alone. However, many of these findings became non-significant after accounting for the severity of conduct disorder symptoms in the comorbid group. Flory et al. (2003) found that ADHD symptoms were related to increased levels of marijuana and hard drug dependence symptoms only for young adults with a history of significant CD symptoms, but this effect was not observed for alcohol use disorders. Both of these studies were limited by the use of cross-sectional data, making it impossible to determine if CD and ADHD symptoms preceded the onset of the substance use outcomes. The relatively few longitudinal studies that have examined the interaction between ADHD and CD symptoms in predicting later substance use, including problem use, have failed to produce significant findings (Fergusson et al., 1993; Taylor et al., 1996).
1.3 Internalizing Problems and Alcohol Use Disorders
There has also been substantial interest in examining the relation between early internalizing problems and later alcohol using behaviors. Much of this research has focused on depressive disorders, which commonly co-occur with substance use problems during adolescence and adulthood (Grant et al., 2004). While exceptions do exist (Hussong & Hicks, 2003), several longitudinal studies have found evidence indicating that childhood depressive symptoms in boys are associated with increased alcohol use (Costello et al., 1999; Henry et al., 1993; Kaplow et al., 2001; Pardini et al., 2004), and a higher rate of substance use disorders (Sung et al., 2004) during adolescence. In addition, depression and dysphoria among male adolescents have been related to increased alcohol involvement in early adulthood, even after controlling for initial levels of substance using behaviors (Locke & Newcomb, 2001). A potential confound in some of these studies is that commonly used measures of childhood depression often include items related to conduct problems (Weiss et al., 1991), which may account for the positive relation between depression and substance use (Kumpulainen & Roine, 2002). However, longitudinal evidence suggests that depression in boys may predict later adolescent alcohol use and substance use disorders, even after controlling for co-occurring conduct problems (Henry et al., 1993; Sung et al., 2004). An important area of future research is examining whether early adolescent depression is associated with the development of alcohol use disorders by early adulthood after accounting for co-occurring CD symptoms.
In contrast to research on depression, higher levels of anxiety/withdrawal in youth tend to be associated with a decreased risk for later substance use problems (Shedler & Block, 1990). While definitions vary across studies, adolescents high in anxiety/withdrawal are often characterized as apprehensive, shy, and timid individuals who are extremely cautious in novel or potentially threatening situations, similar to conceptualizations of behavioral inhibition (Gray, 1991) and harm avoidance (Cloninger et al., 1988). Longitudinal studies have found that characteristics consistent with anxiety/withdrawal are associated with a lower risk of initiating alcohol use in early adolescence (Kaplow et al., 2001; Masse & Tremblay, 1997; Pardini et al., 2004) as well as a lower risk of developing early-onset alcohol abuse (Cloninger et al., 1988). An anxious interpersonal style in adolescence has also been associated with lower problem drinking in adulthood, even after controlling for the influence of conduct problems (Pulkkinen & Pitkänen, 1994). Two primary explanations for this inverse relationship have been proposed. The first suggests that anxious teens are more concerned about the potential negative consequences associated with drinking and illicit drug use, which inhibits them from engaging in these behaviors (Wills et al., 1998, 1999). Second, anxious/withdrawn children may shy away from peer-related social activities where the initiation of problematic substance use typically takes place (Kaplow et al., 2001).
An important area of research that has received little attention is the potential interaction between adolescent internalizing and CD symptoms in predicting later alcohol use problems. Cross-sectional evidence suggests that conduct disorder and major depression may interact to predict substance use disorder symptoms in late adolescence, with comorbid youth exhibiting particularly high levels of dependence symptoms (Marmorstein & Iacono, 2003). Longitudinal evidence indicates that depressive symptoms in early adolescent boys may only be related to later alcohol use among individuals with significant conduct problems (Miller-Johnson et al., 1998). While other studies have failed to replicate this finding (Capaldi & Stoolmiller, 1999), adolescents with elevated depression and conduct problems seem to have particularly poor outcomes. For example, depression among clinic-referred adolescents with conduct disorder has been shown to be a particularly robust predictor of later antisocial personality disorder (Loeber et al., 2002). On the other hand, high levels of anxiety/withdrawal may actually buffer adolescents with significant conduct problems from experiencing long term negative outcomes. Children with CD and an anxiety disorder have been shown to have fewer police contacts, fewer school suspensions, and lower levels of physical aggression than youth with CD alone (Walker et al., 1991). In addition, low fearfulness is associated with a severe form of adolescent antisocial behavior characterized by a callous interpersonal style (Pardini et al., 2003; Pardini, in press). However, prospective studies assessing the interaction between early CD symptoms and internalizing difficulties in predicting later alcohol use disorders are still needed.
1.4 Current Study
The current study will expand the existing literature by examining the independent relations between several forms of early adolescent psychopathology (i.e., CD symptoms, ADHD symptoms, depression, anxiety/withdrawal) and the development of alcohol use disorders by young adulthood in a longitudinal sample of boys. The possibility that CD symptoms interact with depression and ADHD symptoms to create a multiplicative risk for alcohol use problems will also be explored. Conversely, we will examine whether anxiety/withdrawal can protect children with high CD symptoms from developing alcohol use disorders by young adulthood. This investigation will advance the existing literature in several ways. First, previous longitudinal studies, including those conducted with the current dataset, have not accounted for the co-occurrence between disruptive behaviors and internalizing problems when predicting later alcohol use outcomes (White et al., 2001). Similarly, previous studies have failed to differentiate between internalizing problems related to depression and anxiety/withdrawal when investigating substance use outcomes (Capaldi & Stoolmiller, 1999; Loeber et al., 1999). Research suggests that failing to control for the overlap between these internalizing symptoms can suppress the unique relation between each emotional state and substance use outcomes (Pardini et al., 2004; Wills et al., 1998, 1999). Lastly, studies in this area often focused on early psychopathology as a predictor of frequency or intensity of alcohol use, rather than targeting alcohol use disorders (e.g., White et al., 2001).
2. Methods
2.1 Design and Sample
This investigation used data collected as part of the Pittsburgh Youth Study (PYS), a longitudinal study aimed at understanding the development of delinquency, substance use, and mental health problems in boys (Loeber et al., 1998). While the PYS consists of three separate grade-based samples (commonly referred to as youngest, middle, and oldest samples), only data from the oldest sample was used because they received intensive alcohol use disorder assessments in young adulthood. The oldest sample was originally selected from a list of names and addresses of all seventh grade boys in participating Pittsburgh public schools during 1987-1988. A total of 1,165 families were randomly selected from this list for participation in a screening assessment. Most families agreed to participate once contacted (84.6%). As part of the screening assessment, information was collected on the boy's delinquent behavior using forms completed by mothers, teachers, and the boys themselves. Boys who were rated in the top 30% on the screening assessment (n = 256), as well as a relatively equal number of boys randomly selected from the remainder (n = 247), were selected for longitudinal follow-up. Most boys in the follow-up sample were either African American (56%) or Caucasian (41%). Nearly all were living with their biological mother (94%), and approximately half of the boys lived in a household with no biological or acting father (45.3%). Further details of the sample selection, study characteristics, and participants can be found in Loeber et al. (1998).
2.2 Procedures
Nearly all measures of early adolescent psychopathology, as well as control variables, were collected during the first follow-up assessment of the oldest cohort, which took place six months after the screening assessment. The only exception is the boys' self-report of conduct disorder symptoms, which included information collected during the screening assessment and the first follow-up (see details below). At the first follow-up, the boys had just entered the 8th grade and most were in their early teens (mean age = 13.9). Data collection at this phase consisted of an interview with each boy, an interview with his primary caregiver, and questionnaires completed by the boy's primary caregiver and teacher. Families were paid for their participation, and informed written consent was obtained from the boys and their legal guardians prior to the assessment. Information on the boys' alcohol use disorder symptoms were gathered on two separate occasions in early adulthood. The first took place when most participants were in their early 20s (mean age = 20.4), and the second was conducted when boys were in their mid 20s (mean age = 25.4). All participants were paid for completing the assessments in young adulthood, and informed written consent was obtained prior to the interviews. Most interviews were conducted within the participants' homes. Further information regarding the data collection procedures have been described in detail elsewhere (Loeber et al., 1998).
2.3 Measures
2.3.1 CD Symptoms
CD symptoms were assessed using instruments administered to boys and their primary caretaker (primarily mothers). The caretaker completed the Revised Diagnostic Interview Schedule for Children, Parent Version (DISC-P; Costello, 1987), a structured interview designed to assess several domains of child psychopathology found in the Diagnostic and Statistical Manual of Mental Disorders - 3rd Edition - Revised (DSM-III-R; American Psychiatric Association, 1987). Parents provided information on whether or not their child had exhibited 13 separate DSM-III-R CD symptoms such as lying, starting physical fights, and destruction of property.
Information gathered from the boys at the screening and the first 6-month follow-up assessment was also used to assess the presence or absence of the 13 DSM-III-R CD symptoms. This information was gathered using selected items from the 40-item Self-Reported Delinquency Scale (SRD; Loeber et al., 1998), and the 112-item Youth Self-Report (YSR; Achenbach & Edelbrock, 1987). The SRD assesses how many times in the past 6-months the child has engaged in several delinquent behaviors, including status offenses, stealing, destruction of property, and violence. The YSR assesses internalizing and externalizing behavior problems over the past 6-months by asking the child to rate the truthfulness of certain statements about their behavior on a 3-point scale (0 = “not true,” 1 = “sometimes true”, 2 = “very true”). For the YSR, a CD symptom was considered present if the boy endorsed the behavior as being “very true” at both the screening and six month follow-up assessment. For the SRD, a CD symptom was considered present if the boy reported the behavior occurred one or more times in the past 6 months at both the screening and follow-up assessments. In total, 17 items from the SRD and 4 items form the YSR were used. The YSR was used to gather information on the CD symptoms of lying (1 item), cruelty to animals (1 item), cruelty to people (1 item), and initiating fights (1 item). The SRD was used to assess the CD symptoms of stealing without confrontation (7 items), running away over night (1 item), fire-setting (1 item), truancy (1 item), breaking and entering (1 item), vandalism (1 item), sexual aggression (2 items), attacking someone with a weapon (1 item), and stealing with confrontation (2 items).
Parent and child reports of DSM-III-R CD symptoms were combined by treating a symptom as present if it was endorsed by either informant. This method of combining information avoids under-reporting by a specific informant and has been shown to be as effective as more complex procedures for combining information across informants (Piacentini et al., 1992). The 13 CD symptoms (coded as 1 if the symptom was present, 0 if the symptom was absent) were then summed to create a total symptom score. A previous study with the oldest cohort of the PYS found a significant association between this CD symptom scale and alcohol use during adolescence (White et al., 2001). The internal consistency for the combined parent and child symptom scale is .61.
2.3.2 ADHD Symptoms
The DISC-P was also used to assess the boys' ADHD symptoms in early adolescence. The instrument assesses the presence or absence of 14 different symptoms associated with a DSM-III-R diagnosis of ADHD. The behaviors fall under the broad categories of attentional difficulties (e.g., easily distracted), hyperactivity (e.g., talks excessively), and impulsivity (e.g., interrupts, difficulty waiting turn). All positively endorsed symptoms were added together, with higher scores indicating a greater number of ADHD symptoms. The internal consistency for this measure was good (α = .85).
2.3.3 Depression
Depression was assessed using the self-report Recent Moods and Feeling Questionnaire completed by the child (Costello & Angold, 1988). The measure consists of 13 items associated with major depression in children and adolescents according to DSM-IIIR criteria. Specifically, participants are presented with a series of descriptive statements and are asked to rate how accurately the statement describes their own feelings and behaviors over the past two weeks (e.g., “You felt miserable or unhappy,” “You hated yourself,” “You felt lonely”). Each item is rated on a 3 point scale (0= “not true,” 1 = “sometimes true,” 2 = “always true”). Items were summed to form a composite score, with higher scores indicating increased levels of depression. The distribution of scale was somewhat skewed due to a few extremely high scores, so the scale was square root transformed. Following this modification, the dispersion of scores on the depression scale reasonably approximated a Gaussian distribution (skew = .32, kurtosis = -.51). The internal consistency of the scale was good (α = .84).
2.3.4 Anxiety/Withdrawal
The anxiety/withdrawal scale was created using a combination of child, parent, and teacher report. The scale consisted of 8 items that were identical across the Youth Self Report (YSR; Achenbach & Edelbrock, 1987), Teacher Report Form (TRF; Achenbach & Edelbrock, 1986), and parent-report Child Behavior Checklist (CBC; Achenbach, 1991). Each informant was asked to rate how often the participant exhibited behaviors associated with an anxious and fearful interpersonal style (e.g., “too dependent on adults,” “afraid of going to school,” “self-conscious or easily embarrassed,” “shy or timid,” “keeps from getting involved with others”). Informants rated each item on a three point scale (0 = “not true,” 1 = “sometimes true,” 2 = “very true”). The highest rating across the three informants was selected for each item and then the items were summed to form a total anxiety/withdrawal score. The alpha reliability for this multi-informant scale was modest (α = .62).
2.3.5 Alcohol Use Disorders
Alcohol use disorders were assessed using the Diagnostic Interview Schedule (DIS; Robins & Helzer, 1988), which was administered to participants in the oldest cohort on two separate occasions in early adulthood (i.e., age 20 and 25). The DIS is a fully structured interview developed for psychiatric epidemiology research that can be administered by either computer or lay interviewers (Erdman et al., 1992). This instrument uses a series of standardized probes and follow-up questions to elicit symptoms from the participant and determine whether diagnostic criteria are met. The DIS has demonstrated reliability and construct validity in previous investigations (for a review see Malgady et al., 1992), and remains one of the most commonly used diagnostic instruments in substance use disorder research (Forman et al., 2004).
In their early twenties (mean age = 20.4), participants were administered the paper version of Diagnostic Interview Schedule for DSM-III-R diagnoses (DIS-III-R; Robins & Heltzer, 1988) by a trained interviewer. During this interview, participants were asked to report whether they had ever experienced symptoms related to DSM-III-R diagnoses, including those related to alcohol abuse and dependence. The scoring of the DIS-III-R was modified slightly so that information regarding the presence or absence of alcohol abuse and dependence symptoms was consistent with revisions made in the DSM-IV classification system (American Psychiatric Association, 2000). Five years later (mean age = 25.4), participants were administered the computerized version of the Diagnostic Interview Schedule for DSM-IV diagnosis (DIS-IV; Erdman et al., 1992), The second DIS interview also collected information about the lifetime prevalence of DSM-IV symptoms related to alcohol abuse and dependence. To generate a single measure of alcohol use disorder symptoms for each participant, information from the age 20 and 25 DIS assessments were combined at the symptom level. Specifically, each alcohol use disorder symptom was considered present if it was endorsed as having occurred by either the age 20 or age 25 assessment. This was done for the four symptoms associated with alcohol abuse (use in risky or dangerous situations, continued use despite interpersonal problems, recurrent legal problems as the result of use, and use resulting in a failure to fulfill major role obligations) and the seven symptoms associated with alcohol dependence (tolerance, withdrawal, using more often or in larger amounts than intended, persistent desire or unsuccessful attempts to cut down/control use, extensive time spent using or recovering from use, important activities given up/reduced as a result of use, and continued use despite psychological/medical problems).
After combining information from the age 20 and 25 interviews at the symptom level, the primary outcomes measures were created using a dimensional and categorical approach. Specifically, a dimensionally-oriented scale was created representing the total number of lifetime abuse and dependence symptoms reported by participants (scores range from 0 – 11). The internal consistency of the AUD symptom scale was good (α = .84). In addition, a single categorical variable was created based on DSM-IV criteria for abuse and dependence. This variable consisted of three mutually exclusive and exhaustive nominal categories: lifetime alcohol dependence (3 or more dependence symptoms), lifetime alcohol abuse without dependence (dependence criteria not met, but 1 or more abuse symptoms), and no lifetime alcohol abuse or dependence.
2.4 Potential Confounds
2.4.1 Demographic Variables
A number of demographic variables were selected as potential confounds to the relation between early psychopathology and later alcohol use problems. The first set of control variables consists of the basic demographic characteristics of age, minority status (1 = African American, 0 = Caucasian), and socioeconomic status (SES), which have previously been associated with substance use outcomes in the Pittsburgh Youth Study (Loeber et al., 1998). SES was calculated for each caregiver in the household using the Hollingshead Index (Hollingshead, 1975). When multiple caregivers were present, family SES was indexed using the highest Hollingshead score.
2.4.2 Family History of Alcohol/Drug Problems
To control for a family history of alcohol/drug problems, information on the biological parents' mental health history was obtained from the Family History Questionnaire (FHQ; Loeber et al., 1998). The FHQ was administered at the first 6-month follow-up assessment and asked about the lifetime prevalence of help-seeking behaviors for various mental health problems by members of the immediate family. Questions pertaining to whether or not the child's biological mother or father had ever sought help for an alcohol or drug problem were used in the current study. A binary variable indicating whether the child's biological mother or father had ever sought help for an alcohol or drug problem was created.
2.4.3 Child's History of Alcohol Use and Problems
The last set of control variables were designed to assess the boys' history of alcohol use and alcohol-related problems at the time the psychopathology variables (i.e., CD, ADHD, depression, anxiety/withdrawal) were measured. This information was gathered using substance use questions from of the National Youth Survey at the first 6-month follow-up assessment (NYS; Elliott et al., 1985). Specifically, the boys were asked if they had ever used alcohol without their parents' permission. Those participants who endorsed “ever” using alcohol were then asked nine questions about problems that may have occurred as the result of their use (e.g., “Have you ever had problems with your family as the result of your alcohol use?,” “Have you ever gotten into physical fights as the result of your alcohol use?”). Participants who positively endorsed any of the nine items were categorized as having a positive history for alcohol use problems.
2.5 Management of Missing Data
In general, sample retention for the Pittsburgh Youth Study has been high across all waves. The proportion of participants with missing data on one or more of the variables included in the current study was relatively low (15.4%, n = 78). The largest number of participants were missing data on the AUD symptom and diagnosis variables (7.1%, n = 36). There were also low levels of missing data for the independent variables of CD symptoms (4.2%, n = 21), ADHD symptoms (5.9%, n = 30), depression (< 1%, n = 1), anxiety/withdrawal (< 1%, n = 1), history of alcohol use (< 1%, n = 1), history of alcohol use problems (< 1%, n = 3), and parental history of alcohol/drug problems (1.8%, n = 9). The most common reasons for missing data were an inability to locate participants during the follow-up, participants repeatedly failing to show up for assessment sessions, and administration errors. To determine if participants with missing data were systematically different from those with complete data, a series of statistical tests were performed. Results indicated that participants with missing data were not significantly different from those with complete data on all variables used in the current study. Details regarding these analyses are available from the first author upon request.
For the primary analyses, missing data were handled using maximum likelihood estimation (MLE) procedures for count and categorical outcomes within Mplus 4.1 (Muthén & Muthén, 1998-2006). MLE uses all available information to generate parameter estimates rather than resorting to listwise deletion (for details see Schafer & Graham, 2002). Simulation research suggests that MLE provides accurate and efficient parameter estimates in comparison to other ad hoc techniques (e.g., pairwise deletion, listwise deletion) when data are missing completely at random or missing at random (Enders & Bandalos, 2001; Enders, 2001). In addition, MLE yields results that are highly similar to multiple imputation procedures for handling missing data when the two techniques are implemented in a similar manner (Collins, Schafer, & Kam, 2001).
2.6 Data Analysis Plan
A zero-inflated Poisson (ZIP) regression in Mplus 4.1 was used to predict AUD symptom scores. ZIP regression is appropriate for modeling count data with excessive zeros (Muthén & Muthén, 1998-2006). A large positive Vuong test for nonnested models favored the use of a ZIP model over an ordinary Poisson regression, z = 6.79, p < .0001. Maximum likelihood estimation with robust standard errors using a Monte Carlo numerical integration algorithm was employed for this analysis (for details see Muthén, 2004; Muthén & Muthén, 1998-2006). With a ZIP model, two regressions are simultaneously estimated. Specifically, a Poisson regression estimates the relation between predictor variables and the count portion of the independent variable for individuals who are able to assume values of zero and above. The inflation portion of the model consists of a logistic regression that models the likelihood of being unable to assume any value besides zero. As a result, the model assumes that zeros are the result of two latent subpopulations. For the inflation portion of the model, the latent subpopulation is individuals who are unable to assume any AUD symptom score besides zero, such as individuals who have abstained from substantive alcohol use for a large portion of their life (Simons, Neal, & Gaher, 2006). In contrast, the count portion of the model estimates the probability of experiencing a certain number of AUD symptoms (including zero) for the latent subpopulation of participants who have engaged in risky behaviors that could potentially lead to alcohol problems (e.g., regular alcohol users). Further details regarding the technical aspects of ZIP modeling are addressed by Long (1997).
In the current study, the same predictors were used for the inflation and count portions of the ZIP regression predicting AUD symptoms. In the first step of the regression, the potential confounds of age, minority status, family SES, parental history of alcohol/drug problems, child's prior alcohol use, and child's prior alcohol problems were entered. Also entered in this step were the early adolescent psychopathology variables of CD symptoms, ADHD symptoms, depression, and anxiety/withdrawal.1 In the second step of the regression, three product terms representing the interaction between CD symptoms and the other forms of early adolescent psychopathology (i.e., ADHD symptoms, depression, anxiety/withdrawal) were entered. Significant interactions were probed following procedures outlined by Aiken and West (1991). Specifically, the relation between early psychopathology and alcohol use disorder symptoms was examined at low (1 SD below the mean), moderate (the mean), and high (1 SD above the mean) levels of conduct disorder symptoms. To eliminate scaling differences between the variables representing early psychopathology, and avoid problems with collinearity that can occur when examining interactions, the primary predictor variables were standardized prior to this analysis.
Multinomial logistic regression was used to predict the categorical dependent variable representing AUD diagnosis. MLE with robust standard errors using a Monte Carlo numerical integration algorithm was employed for this analysis (Muthén, 2004; Muthén & Muthén, 1998-2006). For this model, the contrast group consisted of participants who did not met lifetime criteria for alcohol abuse or dependence. The procedural steps for entering predictors into the model and probing significant interactions were identical to those described for the analyses involving AUD symptoms.
All descriptive statistics and analyses presented are based on weighted data. Sampling weights were used to account for the over-representation of high-risk boys selected for longitudinal follow-up from the initial screening sample. As a result, estimates are representative of the original screening sample of boys attending Pittsburgh public schools in 1987-88. Unweighted analyses are available upon request from the corresponding author.
4. Results
4.1 Descriptive Statistics
Descriptive statistics and bivariate correlations for observed predictor and control variables are presented in Table 1. While nearly half of the boys in the study endorsed a prior history of alcohol use at the initial assessment in early adolescence (46%), relatively few endorsed ever experiencing problems as the result of their use (5%). All measures of early adolescent psychopathology were positively intercorrelated. As expected, the highest correlations were between the externalizing variables of CD and ADHD symptoms, and the internalizing variables of depression and anxiety/withdrawal. Participants with higher CD symptoms were significantly more likely to report a prior history of alcohol use and alcohol use problems, as well as have a biological parent with a history of alcohol/drug problems. Higher levels of depression were also related to an increased probability of reporting prior alcohol use problems.
Table 1.
Descriptive Statistics and Correlations for Potential Confounds and Primary Predictor Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| M | 13.82 | 33.80 | .57 | .24 | .46 | .05 | .58 | 3.12 | 1.29 | 5.08 |
| SD | .80 | 14.17 | .50 | .43 | .50 | .22 | .99 | 3.20 | 1.05 | 2.49 |
| 1. Age | ||||||||||
| 2. Family Socioeconomic Status | −.32*** | |||||||||
| 3. Minority Status | .21*** | −.21*** | ||||||||
| 4. Parent Alcohol/Drug Problems | .08 | −.07 | .10* | |||||||
| 5. Prior Alcohol Use | .00 | .08* | −.06 | .10* | ||||||
| 6. Prior Alcohol Problems | .11* | −.01 | .02 | .05 | .22*** | |||||
| 7. CD Symptoms | .19*** | −.13** | −.04 | .11* | .17*** | .21*** | ||||
| 8. ADHD Symptoms | .15** | −.09 | .04 | .07 | .08 | .08 | .43*** | |||
| 9. Depression | .10* | .06 | .02 | .04 | .06 | .10* | .20*** | .28*** | ||
| 10. Anxiety/Withdrawal | .17*** | −.02 | −.02 | .04 | .02 | −.01 | .26*** | .31*** | .40*** |
p < .05;
p < .01;
p < .001
The proportion of boys who met criteria for a diagnosis of alcohol abuse without dependence and alcohol dependence by young adulthood was similar. Specifically, 21.3% of participants met criteria for alcohol abuse without dependence and 24.5% met criteria for lifetime alcohol dependence. The mean number of alcohol use disorder symptoms reported for the entire sample was relatively low (M = 2.19, SD = 2.56, Range 0 – 11), with the modal response being zero (35.6%).
4.2 Alcohol Use Disorders Symptoms
Results from the ZIP regression using early adolescent psychopathology to predict AUD symptoms are presented in Table 2. The significant predictors for the zero-inflated portion of the model included minority status and participant's prior alcohol use. Specifically, boys who reported prior alcohol use at the first follow-up and Caucasian participants were less likely to belong to the latent group of participants who were unable to assume non-zero symptoms scores (e.g., abstainers). Early adolescent psychopathology did not significantly predict the inflation portion of the AUD symptom model.
Table 2.
Zero-Inflated Poisson Regression Using Early Adolescent Psychopathology to Predict Lifetime Alcohol Use Disorder Symptoms by Young Adulthood.
| Alcohol Use Disorder Symptoms | ||||||||
|---|---|---|---|---|---|---|---|---|
| Zero Inflation | Symptom Count | |||||||
| OR | 95% CI | z | p | IRR | 95% CI | z | p | |
| Step 1 | ||||||||
| Age | 1.047 | .766 − 1.432 | .288 | .773 | .882 | .777 − 1.001 | −1.947 | .052 |
| Minority Status | 1.925 | 1.168 − 3.177 | 2.566 | .010 | 1.001 | .832 − 1.204 | .006 | .995 |
| Family Socioeconomic Status | .997 | .979 − 1.016 | −.280 | .779 | 1.001 | .995 − 1.008 | .386 | .699 |
| Parent Alcohol/Drug Problems | .616 | .358 − 1.061 | −1.748 | .080 | 1.006 | .829 − 1.221 | .061 | .951 |
| Child's Prior Alcohol Use | .615 | .380 − .996 | −1.978 | .048 | 1.045 | .866 − 1.260 | .456 | .648 |
| Child's Prior Alcohol Problems | .512 | .186 − 1.409 | −1.296 | .195 | 1.163 | .883 − 1.530 | 1.075 | .282 |
| CD Symptoms | 1.065 | .808 − 1.402 | .446 | .656 | 1.190 | 1.054 − 1.342 | 2.833 | .005 |
| ADHD Symptoms | .985 | .752 − 1.292 | −.106 | .916 | 1.034 | .934 − 1.145 | .644 | .520 |
| Depression | .956 | .736 − 1.241 | −.337 | .736 | 1.048 | .937 − 1.172 | .827 | .408 |
| Anxiety/Withdrawal | 1.079 | .806 − 1.445 | .510 | .610 | .858 | .774 − .952 | −2.885 | .004 |
| Step 2 | ||||||||
| CD X ADHD | .918 | .703 − 1.200 | −.629 | .529 | .946 | .872 − 1.025 | −1.355 | .175 |
| CD X Depression | .854 | .659 − 1.106 | −1.194 | .232 | 1.106 | 1.011 − 1.210 | 2.193 | .028 |
| CD X Anxiety/Withdrawal | .817 | .581 − 1.149 | −1.160 | .246 | .978 | .889 − 1.078 | −.439 | .661 |
Note. OR = odds ratio; IRR = incident rate ratio; CI = confidence interval. In this zero-inflated Poisson regression, the inflation portion of the model is a logistic regression predicting a latent subpopulation of individuals who are unable to assume AUD symptom scores besides zero (e.g., abstainers). The count portion of the model is a Poisson regression predicting the number of AUD symptoms accrued by the latent subpopulation of individuals who could assume AUD symptom scores of zero and above (e.g., regular drinkers).
In contrast, facets of early adolescent psychopathology were significantly related to an increased number of AUD symptoms for the count portion of the ZIP regression. After controlling for potential confounds and the overlap between measures of early adolescent psychopathology, higher levels of anxiety/withdrawal were inversely related to AUD symptoms. On the other hand, higher levels of CD symptoms were significantly related to higher levels of AUD symptoms. There were no main effects for ADHD symptoms or depression in predicting AUD symptoms.
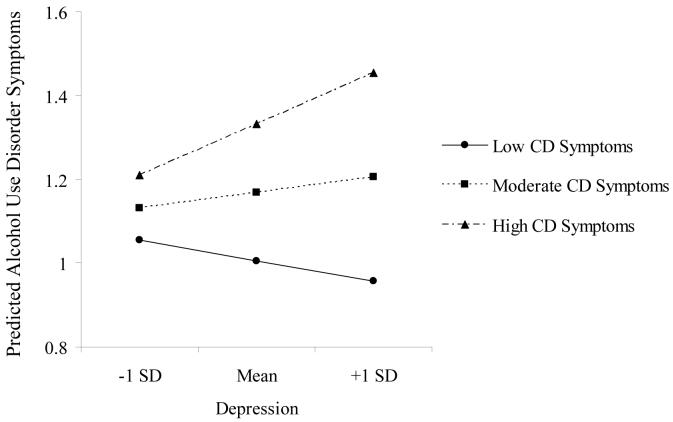
In the second step of the regression, there was a statistically significant interaction between conduct problems and depression in predicting the number of AUD symptoms by early adulthood. As previously mentioned, recommended procedures for probing continuous variable interactions at mean levels of all other covariates in the model were used to elucidate the nature of this relation (Aiken & West, 1991). The results from these analyses are visually depicted in Figure 1. Depressive symptoms were not significantly related to AUD symptoms for participants with low (incident rate ratio (IRR) = .952, 95% confidence interval (CI) = .826 − 1.10, z = −.671, p = .502) and moderate (IRR = 1.038, 95% CI = .931 − 1.156, z = .664, p =.507) levels of CD symptoms. However, increased depression was associated with a greater number of AUD symptoms for individuals with high levels of CD symptoms at a marginal level of statistical significance (IRR = 1.131, 95% CI = .996 − 1.284, z = 1.898, p = .058). Overall, the results suggest that the co-occurrence of high levels of depression and CD symptoms seems to place adolescents at particular risk of developing increased AUD symptoms by young adulthood.
Figure 1.
Interaction between conduct disorder symptoms and depression in predicting alcohol use disorder symptoms by young adulthood. Predicted values are based on the log of the incident rate ratio.
4.3 Alcohol Use Disorder Diagnoses
Multinomial regression results predicting AUD diagnoses from early adolescent psychopathology are presented in Table 4. Results indicated that early adolescent psychopathology did not significantly differentiate individuals with a lifetime diagnosis of alcohol abuse without dependence from those who never developed an AUD. In contrast, participants with higher levels of CD symptoms and lower levels of anxiety/withdrawal in early adolescence were more likely to develop a lifetime diagnosis of alcohol dependence in comparison to individuals who never developed an AUD.
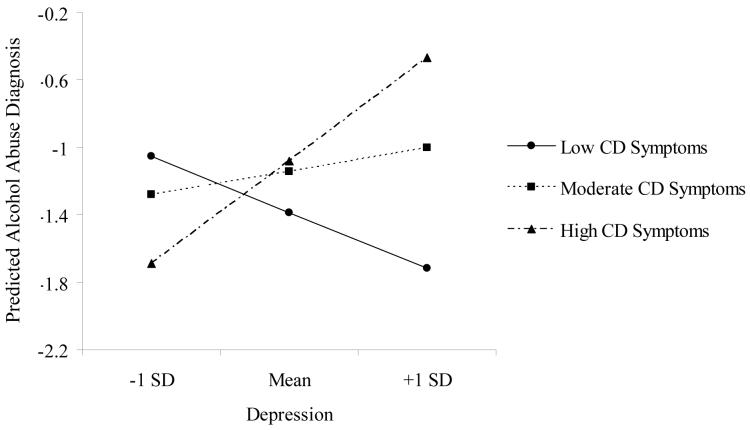
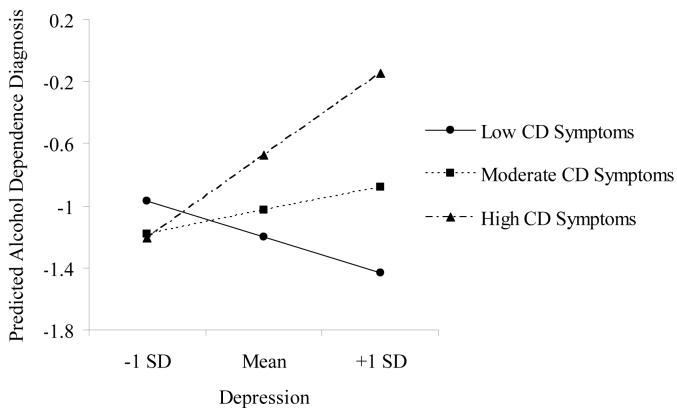
In the second step of the regression, a significant interaction emerged between early adolescent CD symptoms and depression in predicting both alcohol abuse and alcohol dependence. Post hoc probing of the interactions revealed a similar pattern of findings for alcohol abuse (see Figure 2) and alcohol dependence (see Figure 3). Depressive symptoms did not significantly differentiate non-AUD participants from those who developed alcohol abuse at low (relative risk ratio (RRR) = .717, 95% CI = .484 − 1.061, z = −1.664, p = .096) and moderate (RRR = 1.151, 95% CI = .846 − 1.565, z = .897, p = .370) levels of CD symptoms. However, increased depression was associated with a greater risk for developing alcohol abuse for individuals with high levels of CD symptoms (RRR = 1.842, 95% CI = 1.140 − 2.974, z = 2.496, p = .013). Similarly, depressive symptoms did not significantly differentiate non-AUD participants from those who developed alcohol dependence at low (RRR = .793, 95% CI = .541 − 1.164, z = −1.185, p = .236) and moderate (RRR = 1.163, 95% CI = .880 − 1.537, z = 1.061, p = .289) levels of CD symptoms. In contrast, higher levels of depressive symptoms were significantly associated with a greater risk for developing alcohol dependence for those participants with high levels of CD symptoms (RRR = 1.701, 95% CI = 1.174 − 2.465, z = 2.805, p = .005).
Figure 2.
Interaction between conduct disorder symptoms and depression in predicting alcohol abuse by young adulthood. Predicted values are based on the log of the relative risk ratio.
Figure 3.
Interaction between conduct disorder symptoms and depression in predicting alcohol dependence by young adulthood. Predicted values are based on the log of the relative risk ratio.
4.4 Post Hoc Analyses
Because no a priori hypotheses were made about interactions between early adolescent ADHD symptoms, depression, and anxiety in predicting AUD symptoms and diagnoses by young adulthood, two-way interactions between these facets of early adolescent psychopathology were not included in the primary analyses. However, exploratory analyses were conducted with the two-way interaction terms representing ADHD symptoms by depression, ADHD symptoms by anxiety/withdrawal, and depression by anxiety/withdrawal. These interaction terms were added to models predicting both AUD symptoms and diagnoses, after controlling for all potential confounds and the significant CD symptom by depression interaction. None of the parameter estimates for these interaction terms were statistically significant. These analyses are available upon request from the primary author.
5. Discussion
A primary goal of the current study was to examine the independent relation between measures of early adolescent psychopathology and the development of alcohol use disorder symptoms and diagnoses by young adulthood. Consistent with prior research, problems related to CD symptoms, ADHD symptoms, depression, and anxiety/withdrawal tended to co-occur in early adolescence. However, after controlling for the co-occurrence between these facets of psychopathology, several unique relations with AUD outcomes by early adulthood emerged. As expected, early adolescent CD symptoms emerged as a risk factor for developing increased AUD symptoms and alcohol dependence by early adulthood. There was also consistent evidence indicating that increased levels of depressive symptoms in conjunction high CD symptoms placed early adolescent boys at particular risk for developing AUD symptoms and diagnoses. In contrast, higher levels of anxiety/withdrawal in early adolescence seemed to protect boys from developing significant AUD symptoms and alcohol dependence. There was no evidence that early adolescent ADHD symptoms were related later AUD outcomes after controlling for cooccurring forms of psychopathology and potential confounds. In general, early adolescent psychopathology did not predict which boys would refrain from developing any AUD symptoms by early adulthood (i.e., zero-inflation), and early adolescent psychopathology was only modestly related to alcohol abuse in the absence of dependence. This is congruent with research suggesting that severe forms of psychopathology are consistently associated with alcohol dependence, but inconsistently related to alcohol abuse (Hasin et al., 2003).
5.1 CD Symptoms and Alcohol Use Disorders
The current results support research linking CD symptoms to early-onset alcohol use problems (Weinberg et al., 1998). Specifically, boys who exhibited higher levels of CD symptoms at the initial assessment were more likely to have initiated alcohol use and experienced problems as the result of alcohol use in the past. However, even after controlling for the co-occurrence of CD symptoms and alcohol use in early adolescence, elevated CD symptoms placed boys at risk for developing serious alcohol use problems by young adulthood. Moreover, the relation between CD symptoms and the development of AUD symptoms does not seem to be due to its overlap with other forms of early adolescent psychopathology (i.e., ADHD symptoms, depression, anxiety/withdrawal). An important area for future research will be to examine the processes that explain the robust relation between CD symptoms and later alcohol use problems. For example, more genetically informed studies are needed to determine the extent to which the co-occurrence between early CD symptoms and alcohol use disorders can be accounted for by genetic factors (Tarter et al., 1999), including the examination of specific candidate genes (for example see Hill et al., 2002). In addition, peer contagion models that suggest adolescents with significant CD symptoms are more likely to associate with deviant peers, who in turn promote problematic drinking habits, need to be tested further using longitudinal data (Dishion et al., 1995).
5.2 ADHD Symptoms and Alcohol Use Disorders
After controlling for other forms of early adolescent psychopathology, there was no evidence linking ADHD symptoms to alcohol use disorders by early adulthood. While the current measure of ADHD symptoms was limited by its reliance on one informant (i.e., parent), the findings are consistent with a growing body of literature. In a recent review of longitudinal studies, Flory and Lynam (2003) found no significant evidence for an independent relation between ADHD symptoms and substance use problems (except possibly tobacco use), after accounting for co-occurring conduct problems. While some cross-sectional evidence has suggested that problems with ADHD and CD may interact to increase an individual's risk for substance use problems (Flory et al., 2003; Molina et al., 1999), longitudinal studies have failed to find direct evidence for such an interaction (Fergusson, et al., 1993; Loeber et al., 1999; Taylor et al., 1996). Consistent with this longitudinal work, the current study found no evidence for an interaction between ADHD and CD symptoms in predicting alcohol use disorders by young adulthood.
5.3 Anxiety/Withdrawal and Alcohol Use Disorders
Findings suggested that boys who experienced significant levels of anxiety/withdrawal in early adolescence were less likely to develop AUD symptoms and alcohol dependence by young adulthood. This inverse relationship between measures of interpersonal anxiety and substance use outcomes has been observed in other longitudinal investigations (Kaplow et al., 2001; Masse & Tremblay, 1997; Pardini et al., 2004). As a result, investigators have warned against aggregating facets of negative affect into composite scales during childhood and adolescence (Pardini et al., 2004). In substance use studies, it seems particularly important to separate negative emotions that tend to be inversely related to substance use outcomes (e.g., social anxiety, fearfulness), from those shown to be positively associated with substance using behaviors (e.g., depression, anger). An important area of future research involves elucidating the mechanisms behind the inverse relation between anxiety/withdrawal and the development of substance use problems. Cross-sectional studies have suggested that children with high levels of anxiety/withdrawal are less likely to engage in risk-taking behaviors with deviant peers, thereby protecting them from engaging in significant substance using behaviors during adolescence (Wills et al., 1999). However, longitudinal investigations exploring this hypothesis in further detail are needed before firm conclusions can be drawn.
5.4 Interactive Effects of CD and Depression
There was consistent evidence indicating that early adolescent depression interacts with CD symptoms to predict alcohol use disorders. Specifically, higher levels of depression were related to the development of alcohol use disorder symptoms and diagnoses in young adulthood only for participants with high levels of early CD symptoms. Miller-Johnson et al. (1998) described a similar finding in which sixth graders with comorbid conduct and depressive problems had higher levels of 8th grade alcohol and marijuana use in comparison to those with either problem in isolation. Importantly, the authors determined that this interactive effect was not the result of more severe conduct problems in the comorbid group. While the explanatory mechanisms behind this interaction are unknown, hypotheses have been proposed. For example, Marmorstein and Iacono (2003) noted that adolescents with conduct disorder and elevated depressive symptoms may repeatedly use substances to manage their negative affective states because they are relatively unconcerned about violating social norms. Interestingly, longitudinal evidence also suggests that high levels of depression are associated with the progression from childhood conduct disorder to antisocial personality disorder in young adulthood (Loeber et al., 2002). As a result, young adolescents with co-occurring depression and conduct problem symptoms may be at particular risk for developing a severe form of alcoholism with antisocial features by young adulthood.
5.5 Limitations
A limitation of the current study was that participants reported on the lifetime prevalence of alcohol use disorder symptoms in young adulthood. However, the primary relations observed in this study were significant after controlling for the boys' prior history of alcohol use and history of alcohol use problems at the initial assessment. In addition, a relatively small proportion of boys reported any prior experience with alcohol use problems at the time that the psychopathology variables were assessed (i.e., 5%). This suggests that psychopathology symptoms preceded the development of AUD symptoms for most boys in the current study.
The current investigation did not examine the potential mediational processes linking early adolescent psychopathology to alcohol use disorders. Investigators have emphasized mediation analysis as an important next step in research on the development of substance use disorders (Cicchetti & Luthar, 1999). Cross-sectional and longitudinal studies suggest that factors such as poor self-control and coping skills, deviant peer group affiliation, and increased life stress are potential mediators worthy of future investigation (Wills et al., 1998, 1999; Wills & Stoolmiller, 2002). It will also be important to ensure that the association between early psychopathology and alcohol use disorders cannot be accounted for by a common third factor (e.g., poor parenting practices). While the current study did attempt to account for parental history of alcohol/drug problems, this variable was derived from a measure asking parents if they had ever sought help for these problems. As a result, it did not account for substance abusing parents who had never sought treatment for their problems.
Future studies should also determine if the effects observed in the current investigation hold for other substance use disorders. Unfortunately, the low prevalence rates of other substance use disorders at either assessment in early adulthood in the Pittsburgh Youth Study limits our ability to accurately estimate interaction effects with adequate statistical power (e.g., cannabis abuse/dependence = 11.9%). It is possible that the mechanisms underlying the development of substance use disorders involving illicit drugs are different from those involving alcohol.
There are also several limitations resulting from the nature of the sample. Because all participants in the Pittsburgh Youth Study are male, potential gender differences in the observed relations could not be examined. While the Pittsburgh Youth Study over-sampled boys with high levels of conduct problems, weighted analyses were used to account for this sampling scheme. However, all participants were selected from Pittsburgh city schools, limiting our ability to generalize these findings outside of this geographical area. Lastly, the boys in the oldest sample were already in early adolescence at the beginning of the investigation. Future studies with younger children are needed to determine if childhood measures of psychopathology are related to later alcohol use disorders in a manner similar to those described here.
5.6 Conclusions
The current study used prospective data to examine the relation between early adolescent psychopathology and the development of alcohol use disorders by early adulthood. CD symptoms emerged as a robust predictor of future alcohol use disorders, suggesting that substance abuse prevention programs are best targeted toward youth exhibiting significant antisocial behavior. However, adolescents with co-occurring depressive symptoms and CD symptoms were are at highest risk for developing alcohol use disorders by young adulthood. Along similar lines, a recently developed cognitive-behavioral intervention for adolescents with co-occurring depression and substance use disorders found that nearly all participants also met criteria for conduct disorder (Curry et al., 2003). Pilot testing of this program showed reductions in both depressive symptoms and substance using behaviors, suggesting that it could be adapted to help prevent the development of substance use disorders among children with comorbid conduct disorder and depression. On the other hand, adolescents with internalizing problems related to anxiety/withdrawal seem to have a lower risk for developing alcohol use disorders, which supports recent warnings about aggregating different facets of negative emotions in substance use research. Consistent with a growing body of longitudinal research, ADHD symptoms had little or no impact on the development of alcohol use disorders after controlling for co-occurring forms of psychopathology.
Table 3.
Multinomial Logistic Regression Using Early Adolescent Psychopathology to Predict Lifetime Alcohol Abuse and Alcohol Dependence Diagnoses by Young Adulthood.
| Alcohol Abuse Only | Alcohol Dependence | |||||||
|---|---|---|---|---|---|---|---|---|
| RRR | 95% CI | z | p | RRR | 95% CI | z | p | |
| Step 1 | ||||||||
| Age | .763 | .547 − 1.066 | −1.584 | .113 | .676 | .468 − .977 | −2.083 | .037 |
| Minority Status | .702 | .425 − 1.160 | −1.384 | .166 | .674 | .393 − 1.156 | −1.433 | .152 |
| Family Socioeconomic Status | .998 | .977 − 1.018 | −.236 | .813 | .997 | .977 − 1.016 | −.313 | .754 |
| Parent Alcohol/Drug Problems | 1.273 | .708 − 2.289 | .805 | .421 | 1.212 | .687 − 2.136 | .663 | .507 |
| Child's Prior Alcohol Use | 1.578 | .940 − 2.649 | 1.724 | .085 | 1.377 | .829 − 2.289 | 1.236 | .216 |
| Child's Prior Alcohol Problems | .639 | .225 − 1.817 | −.841 | .400 | 1.257 | .507 − 3.117 | .494 | .621 |
| CD Symptoms | 1.147 | .831 − 1.581 | .834 | .404 | 1.448 | 1.045 − 2.004 | 2.223 | .026 |
| ADHD Symptoms | 1.053 | .782 − 1.419 | .340 | .734 | 1.108 | .846 − 1.454 | .748 | .454 |
| Depression | 1.057 | .786 − 1.422 | .366 | .714 | 1.121 | .846 − 1.486 | .798 | .425 |
| Anxiety/Withdrawal | .814 | .610 − 1.085 | −1.402 | .161 | .674 | .512 − .890 | −2.793 | .005 |
| Step 2 | ||||||||
| CD X ADHD | .898 | .662 − 1.218 | −.696 | .486 | 1.021 | .763 − 1.368 | .145 | .885 |
| CD X Depression | 1.536 | 1.076 − 2.192 | 2.359 | .018 | 1.419 | 1.100 − 1.831 | 2.688 | .007 |
| CD X Anxiety/Withdrawal | 1.138 | .826 − 1.567 | .789 | .430 | 1.048 | .795 − 1.384 | .335 | .738 |
Note. The contrast group is participants without a lifetime diagnosis of alcohol abuse or dependence. RRR = Relative risk ratio; CI = confidence interval.
Acknowledgements
This study was supported by grants from the National Institute on Drug Abuse (DA411018, DA017482, DA017552), National Institute on Mental Health (MH 48890, MH 50778), and the Office of Juvenile Justice and Delinquency Prevention (96-MU-FX-0012). Additional support was provided to the first author through a National Institute on Mental Health training grant (T32 MH015169). Special thanks to Rebecca Stallings, Ernesta Pardini, Evelyn Wei, and Jamie Stump.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Longitudinal research with clinic samples has suggested that the inattentive symptoms of ADHD are more strongly associated with substance use outcomes, particularly tobacco use, than the symptoms of hyperactivity/impulsivity (Burke et al., 2001; Molina & Pelham, 2003). In the current study, we found no differences between early adolescent inattention and hyperactivity/impulsivity in predicting alcohol use disorders in young adulthood. As a result, we have chosen to present results for the aggregate ADHD symptom score.
Contributor Information
Dustin Pardini, University of Pittsburgh Medical Center Pittsburgh, PA 15213 USA.
Helene Raskin White, Center of Alcohol Studies Rutgers University Piscataway, NJ 08854 USA.
Magda Stouthamer-Loeber, Western Psychiatric Institute and Clinic University of Pittsburgh Medical Center Pittsburgh, PA 15213 USA.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 profiles. University of Vermont, Department of Psychiatry; Burlington: 1991. [Google Scholar]
- Achenbach TM, Edelbrock C. Manual for the Teacher's Report Form and teacher version of the Child Behavior Profile. University of Vermont, Department of Psychiatry; Burlington: 1986. [Google Scholar]
- Achenbach TM, Edelbrock CS. Manual for the Youth Self-Report and Profile. University of Vermont, Department of Psychiatry; Burlington: 1987. [Google Scholar]
- Aiken LS, West SG. Multiple regression. Sage Publications Inc; Newbury Park, CA: 1991. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 3rd ed. Author; Washington, DC: 1987. revision. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. text revision. [Google Scholar]
- Angold A, Costello EJ. The epidemiology of disorders of conduct: Nosological issues and comorbidity. In: Hill J, Maughan B, editors. Conduct disorders in childhood and adolescence. Cambridge University Press; Cambridge, UK: 2001. pp. 126–168. [Google Scholar]
- Barkley RA, Fischer M, Edelbrock CG, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]
- Biederman J, Wilens T, Mick E, Faraone SV, Weber W, Curtis S, Thornell A, Pfister K, Jetton JG, Soriano J. Is ADHD a risk factor for psychoactive substance use disorders? Findings from a four-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1997;29:546–557. doi: 10.1097/00004583-199701000-00013. [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Lahey BB. Which aspects of ADHD are associated with tobacco use in early adolescence? J Child Psychol Psychiatry. 2001;42:493–502. [PubMed] [Google Scholar]
- Capaldi D, Stoolmiller M. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: III. Prediction to young-adult adjustment. Dev Psychopathol. 1999;11:59–84. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Luthar SS. Developmental approaches to substance use and abuse. Dev Psychopathol. 1999;11:655–656. doi: 10.1017/s0954579499002254. [DOI] [PubMed] [Google Scholar]
- Clark DB, Parker AM, Lynch KG. Psychopathology and substance-related problems during early adolescence: A survival analysis. J Clin Child Psychol. 1999;28:333–341. doi: 10.1207/S15374424jccp280305. [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Sigvardsson S, Bohman M. Childhood personality predicts alcohol abuse in young adults. Alcohol Clin Exp Res. 1988;12:494–505. doi: 10.1111/j.1530-0277.1988.tb00232.x. [DOI] [PubMed] [Google Scholar]
- Collins LM, Schafer JL, Kam C. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychological Methods. 2001;6:330–351. [PubMed] [Google Scholar]
- Costello A. The Diagnostic Interview Schedule for Children, Parent Version (rev.) University of Massachusetts Medical Center; Worcester, MA: 1987. [Google Scholar]
- Costello EJ, Angold A. Scales to assess child and adolescent depression: Checklists, screens, and nets. J Am Acad Child Adolesc Psychiatry. 1988;27:726–737. doi: 10.1097/00004583-198811000-00011. [DOI] [PubMed] [Google Scholar]
- Costello JE, Erkanli A, Federman E, Angold A. Development of psychiatric comorbidity with substance abuse in adolescence: Effects of timing and sex. J Clin Child Psychol. 1999;28:298–311. doi: 10.1207/S15374424jccp280302. [DOI] [PubMed] [Google Scholar]
- Curry JF, Wells KC, Lochman JE, Craighead WE, Nagy PD. Cognitive-behavioral intervention for depressed, substance-abusing adolescents: Development and pilot testing. J Am Acad Child Adolesc Psychiatry. 2003;42:656–665. doi: 10.1097/01.CHI.0000046861.56865.6C. [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Capaldi DM, Spracklen KM, Li F. Peer ecology of male adolescent drug use. Dev Psychopathol. 1995;7:803–824. [Google Scholar]
- Elliott DZ, Huizinga D, Ageton SS. Explaining delinquency and drug-use. Sage; Beverly Hills, CA: 1985. [Google Scholar]
- Enders CK. The performance of full information maximum likelihood estimator in multiple regression models with missing data. Educational Psychol Measurement. 2001;5:713–740. [Google Scholar]
- Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8:430–457. [PubMed] [Google Scholar]
- Erdman HP, Klein MH, Greist JH, Skare SS, Justead JJ, Robins LN, Helzer JE, Goldring E, Hamburger M, Miller JP. A comparison of two computer-administered versions of the NIMH Diagnostic Interview Schedule. J Psychiatr Res. 1992;26:85–95. doi: 10.1016/0022-3956(92)90019-k. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Lynskey MT, Horwood LJ. Conduct problems and attention deficit behavior in middle childhood and cannabis use by age 15. Aust N Z J Psychiatry. 1993;27:673–682. doi: 10.3109/00048679309075830. [DOI] [PubMed] [Google Scholar]
- Flory K, Lynam D. The relation between attention deficit hyperactivity disorder and substance abuse: What role does conduct disorder play? Clin Child Fam Psychol Rev. 2003;6:1–16. doi: 10.1023/a:1022260221570. [DOI] [PubMed] [Google Scholar]
- Flory K, Milich R, Lynam DR, Leukefeld C, Clayton R. Relation between childhood disruptive behavior disorders and substance use and dependence symptoms in young adulthood: Individuals with symptoms of attention-deficit hyperactivity disorder and conduct disorder are uniquely at risk. Psychol Addict Behav. 2003;17:151–158. doi: 10.1037/0893-164x.17.2.151. [DOI] [PubMed] [Google Scholar]
- Forman RF, Svikis D, Montoya ID, Blaine J. Selection of a substance use disorder diagnostic instrument by the National Drug Abuse Treatment Clinical Trails Network. J Subst Abuse Treat. 2004;27:1–8. doi: 10.1016/j.jsat.2004.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Arch Gen Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Gray JA. The neuropsychology of temperament. In: Strelau J, Angleitner A, editors. Explorations in temperament: Perspectives on theory and measurement. Plenum Press; New York, NY: 1991. pp. 105–128. [Google Scholar]
- Hasin DS, Schuckit MA, Martin CS, Grant BF, Buckolz KK, Helzer JE. The validity of DSM-IV alcohol dependence: What do we know and what do we need to know? Alcohol Clin Exp Res. 2003;27:244–252. doi: 10.1097/01.ALC.0000060878.61384.ED. [DOI] [PubMed] [Google Scholar]
- Henry B, Feehan M, McGee R, Stanton W, Moffitt TE, Silva P. The importance of conduct problems and depressive symptoms in predicting adolescent substance use. J Abnorm Child Psychol. 1993;21:469–480. doi: 10.1007/BF00916314. [DOI] [PubMed] [Google Scholar]
- Hill EM, Stoltenberg SF, Bullard KH, Li S, Zucker RA, Burmeister M. Antisocial alcoholism and serotonin-related polymorphisms: Association tests. Psychiatr Genet. 2002;12:143–153. doi: 10.1097/00041444-200209000-00005. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. New Haven, CT: 1975. Unpublished manuscript. [Google Scholar]
- Hussong AM, Hicks RE. Affect and peer context interactively impact adolescent substance use. J Abnorm Child Psychol. 2003;31:413–426. doi: 10.1023/a:1023843618887. [DOI] [PubMed] [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. J Clin Child Psychol. 2001;30:316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- Kumpulainen K, Roine S. Depressive symptoms at the age of 12 years and future heavy alcohol use. Addict Behav. 2002;27:425–436. doi: 10.1016/s0306-4603(01)00182-4. [DOI] [PubMed] [Google Scholar]
- Locke TF, Newcomb MD. Alcohol involvement and dysphoria: A longitudinal examination of gender differences from late adolescence to adulthood. Psychol Addict Behav. 2001;15:227–236. [PubMed] [Google Scholar]
- Loeber R, Burke JD, Lahey BB. What are adolescent antecedents to antisocial personality disorder. Crim Behav Ment Health. 2002;12:24–36. doi: 10.1002/cbm.484. [DOI] [PubMed] [Google Scholar]
- Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB. Antisocial behavior and mental health problems: Explanatory factors in childhood and adolescence. Lawrence Erlbaum Associates; Mahwah, New Jersey: 1998. [Google Scholar]
- Loeber R, Stouthamer-Loeber M, White HR. Developmental aspects of delinquency and internalizing problems and their association with persistent juvenile substance use between ages 7 and 18. J Clin Child Psychol. 1999;28:322–332. doi: 10.1207/S15374424jccp280304. [DOI] [PubMed] [Google Scholar]
- Long S. Regression models for categorical and limited dependent variables. Sage Publications; Thousand Oaks, CA: 1997. [Google Scholar]
- Malgady RG, Rogler LH, Tyron WW. Issues of validity in the diagnostic interview. J Psychiatr Res. 1992;26:59–67. doi: 10.1016/0022-3956(92)90016-h. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG. Major depression and conduct disorder in a twin sample: Gender, functioning, and risk for future psychopathology. J Am Acad Child Adolesc Psychiatry. 2003;42:225–233. doi: 10.1097/00004583-200302000-00017. [DOI] [PubMed] [Google Scholar]
- Mason WA, Windle M. Reciprocal relations between adolescent substance use and delinquency: A longitudinal latent variable analysis. J Abnorm Psychol. 2002;111:63–76. doi: 10.1037//0021-843x.111.1.63. [DOI] [PubMed] [Google Scholar]
- Masse LC, Tremblay RE. Behavior of boys in kindergarten and the onset of substance use during adolescence. Arch Gen Psychiatry. 1997;54:62–68. doi: 10.1001/archpsyc.1997.01830130068014. [DOI] [PubMed] [Google Scholar]
- Miller-Johnson S, Lochman JE, Coie JD, Terry R, Hyman C. Comorbidity of conduct and depressive problems at sixth grade: Substance use outcomes across adolescence. J Abnorm Child Psychol. 1998;26:221–232. doi: 10.1023/a:1022676302865. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE. Childhood predictors of adolescent substance use in a longitudinal study. J Abnorm Psychol. 2003;112:497–507. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Smith BH, Pelham WE. Interactive effects of attention deficit hyperactivity disorder and conduct disorder on early adolescent substance use. Psychol Addict Behav. 1999;13:348–358. [Google Scholar]
- Muthén BO. Latent variable analysis: Growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. The sage handbook of quantitative methodology for the social sciences. Sage Publications; Thousand Oaks, CA: 2004. pp. 345–370. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 4th Edition Muthén & Muthén; Los Angeles, CA: 19882006. [Google Scholar]
- Pardini DA. The callousness pathway to severe violent delinquency. Aggressive Behavior. in press. [Google Scholar]
- Pardini DA, Lochman JE, Frick PJ. Callous-unemotional traits and social cognitive processes among adjudicated youths. J Am Acad Child Adolesc Psychiatry. 2003;42:364–371. doi: 10.1097/00004583-200303000-00018. [DOI] [PubMed] [Google Scholar]
- Pardini D, Lochman J, Wells K. Negative emotions and alcohol use initiation in high-risk boys: The moderating effect of good inhibitory control. J Abnorm Child Psychol. 2004;32:519–533. doi: 10.1023/b:jacp.0000037780.22849.23. [DOI] [PubMed] [Google Scholar]
- Piacentini JC, Cohen P, Cohen C. Combining discrepant diagnostic information from multiple sources: Are complex algorithms better than simple ones? J Abnorm Child Psychol. 1992;20:51–63. doi: 10.1007/BF00927116. [DOI] [PubMed] [Google Scholar]
- Pulkkinen L, Pitkänen T. A prospective study of the precursors to problem drinking in young adulthood. J Stud Alcohol. 1994;55:578–587. doi: 10.15288/jsa.1994.55.578. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE. The Diagnostic Interview Schedule: its development, evaluation, and use. Social Psychiatry Psychiatr Epidemiol. 1988;23:6–16. doi: 10.1007/BF01788437. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychol Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Shedler J, Block J. Adolescent drug use and psychological health: A longitudinal inquiry. Am Psychol. 1990;5:612–630. doi: 10.1037//0003-066x.45.5.612. [DOI] [PubMed] [Google Scholar]
- Simons JS, Neal DJ, Gaher RM. Risk for marijuana-related problems among college students: An application of zero-inflated negative binomial regression. Am J Drug Alcohol Abuse. 2006;32:41–53. doi: 10.1080/00952990500328539. [DOI] [PubMed] [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello EJ. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug Alcohol Depend. 2004;75:287–299. doi: 10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Tarter R, Vanyuko M, Giancola P, Dawes M, Blackson T, Mezzich A, Clark D. Etiology of early age onset of substance use disorder: A maturational perspective. Dev Psychopathol. 1999;11:657–683. doi: 10.1017/s0954579499002266. [DOI] [PubMed] [Google Scholar]
- Taylor E, Chadwick O, Heptinstall E, Danckaerts M. Hyperactivity and conduct problems as risk factors for adolescent development. J Am Acad Child Adolesc Psychiatry. 1996;35:1213–1226. doi: 10.1097/00004583-199609000-00019. [DOI] [PubMed] [Google Scholar]
- Walker JL, Lahey BB, Russo MF, Frick PJ, Christ MAG, McBurnett K, Loeber R, Stouthamer-Loeber M, Green SM. Anxiety, inhibition, and conduct disorder in children: I. Relation to social impairment. J Am Acad Child Adolesc Psychiatry. 1991;30:187–191. doi: 10.1097/00004583-199103000-00004. [DOI] [PubMed] [Google Scholar]
- Weinberg NZ, Rahdert E, Colliver JD, Myer GD. Adolescent substance abuse: A review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 1998;37:252–261. doi: 10.1097/00004583-199803000-00009. [DOI] [PubMed] [Google Scholar]
- Weiss B, Weisz JR, Politano M, Carey M, Nelson WM, Finch AJ. Developmental differences in the factor structure of the Children's Depression Inventory. Psychol Assess. 1991;3:38–45. [Google Scholar]
- White HR, Loeber R, Stouthamer-Loeber M, Farrington D. Developmental associations between substance use and violence. Dev Psychopathol. 1999;11:785–803. doi: 10.1017/s0954579499002321. [DOI] [PubMed] [Google Scholar]
- White HR, Pandina RJ, LaGrange RL. Longitudinal predictors of serious substance use and delinquency. Criminol. 1987;25:715–739. [Google Scholar]
- White HR, Xie M, Thompson W, Loeber R, Stouthamer-Loeber M. Psychopathology as a predictor of adolescent drug use trajectories. Psychol Addict Behav. 2001;15:210–218. [PubMed] [Google Scholar]
- Wilens TE. Attention-deficit/hyperactivity disorder and the substance use disorders: The nature of the relationship, subtypes at risk, and treatment issues. Psychiatr Clin North Am. 2004;27:283–301. doi: 10.1016/S0193-953X(03)00113-8. [DOI] [PubMed] [Google Scholar]
- Wills TA, Sandy JM, Shinar O. Cloninger's constructs related to substance use level and problems in late adolescence: A mediational model based on self-control and coping motives. Exp Clin Psychopharmacol. 1999;7:122–134. doi: 10.1037//1064-1297.7.2.122. [DOI] [PubMed] [Google Scholar]
- Wills TA, Stoolmiller M. The role of self-control in early escalation of substance use: A time-varying analysis. J Consult Clin Psychol. 2002;4:986–997. doi: 10.1037//0022-006x.70.4.986. [DOI] [PubMed] [Google Scholar]
- Wills TA, Windle M, Cleary SD. Temperament and novelty seeking in adolescent substance use: An application of Cloninger's theory. J Sub Abuse. 1998;6:1–20. doi: 10.1037//0022-3514.74.2.387. [DOI] [PubMed] [Google Scholar]