Abstract
Objective
To examine premature mortality in terms of years of potential life lost (YPLL) among a cohort of long-term heroin addicts.
Method
This longitudinal, prospective study followed a cohort of 581 male heroin addicts in California for more than 33 years. In the latest follow-up conducted in 1996/97, 282 subjects (48.5%) were confirmed as deceased by death certificates. YPLL before age 65 years were calculated by causes of death. Ethnic differences in YPLL were assessed among Whites, Hispanics, and African Americans.
Results
On average, addicts in this cohort lost 18.3 years (SD = 10.7) of potentiallife before age 65. Of the total YPLL for the cohort, 22.3% of the years lost was due to heroin overdose, 14.0% due to chronic liver disease, and 10.2% to accidents. The total YPLL and YPLL by death cause in addict cohort were significant higher than that of US population. The YPLL among African Americans was significantly lower than that among Whites or Hispanics.
Conclusion
The YPLL among addicts was much higher than that in the national population; within the cohort, premature mortality was higher among Whites and Hispanics compared to African American addicts.
Keywords: Premature mortality, Heroin, YPLL, Addiction
Introduction
Heroin abuse remains a major public health problem in the United States, with the burden of heroin-induced problems reaching a staggering height (Substance abuse and Mental Health Services Administration, 2004). Many studies have examined the consequences associated with heroin abuse, mostly in terms of criminal involvement, morbidity, and mortality (Booth et al., 1991; Hser et al., 1993; Hser et al., 1994; McGlothlin et al., 1977; Hser et al., 2001). Mortality statistics are one of the most commonly used and important measures of the health status of populations. However, it ignores the fact that death at a young age is generally considered to be a greater loss to the individual and society compared with death at an older age. This paper, therefore, considers premature death, weighing death at a young age more heavily than death at an older age, and compares that to traditional mortality statistics in a cohort of long-term heroin addicts.
Various formulas for measuring premature mortality have been proposed (Wise et al., 1988). The Centers for Disease Control and Prevention (CDC) has customarily assessed premature mortality with a simple definition of “years of potential life lost” (YPLL) before age 65 (Centers for Disease Control, 1986). The United States General Accounting Office (General Accounting Office, 1996) also accepts the concept of YPLL and reports that premature mortality, measured as YPLL, is the best single indicator for reflecting differences in the health status of populations and recommends that it be used to assist the distribution of federal funding for core public health functions.
The advantage of examining premature death using YPLL is that age at death and cause of death are taken into consideration. Causes of death generally may be classified as degenerative diseases, communicable diseases, or causes due to social pathologies (Rogers, 1995). Pathologies such as drug abuse, homicide, and cirrhosis of the liver are much more prevalent among younger persons, while degenerative diseases such as cancer, heart disease, or cerebrovascular disease have a much greater impact among the elderly (Rogers, 1995). From a public health perspective, deaths at younger ages warrant increased attention because they result in lost productivity, reduce the support young persons generally provide to dependent elderly persons and children, and are more likely to be preventable. YPLL is being utilized currently to assess the social and economic burdens of smoking, alcohol use, suicide, and HIV/AIDS (Centers for Disease Control, 2004; Selik and Chu, 1997; Rivara et al., 2004; John and Hanke, 2003; Obiri et al., 1998). Like substance abuse, HIV/AIDS is predominantly found in the 20- to 40-year-old group, a subset of the community that is generally economically and socially productive (Lai et al., 2006; Stewart, 1997; Obiri et al., 1998).
The number of longitudinal prospective studies of heroin addiction has grown steadily in recent years. In general, the death rates in these studies range from 1.24% to 3.3% per year for the period of the individual studies (Brugal et al., 2005; Rathod et al., 2005; Sorensen et al., 2005; Termorshuizen et al., 2005; Termorshuizen et al., 2005; De Angelis et al 2004; Vlahov et al., 2004; Oppenheimer et al., 1994; Barr et al., 1984; Haastrup and Jepsen, 1988; Joe et al., Joe and Simpson, 1987). Many such studies reported traditional mortality data, however, a few of them provided information on premature mortality because of small sample sizes, short observational periods, or failure to report adequate findings for deceased addicts. Based on a 33-year follow-up study, the present paper focuses on premature death among long-term heroin addicts with varied ethnic backgrounds. With such a long period of follow-up data on a sample in which half of the participants have died, our study is unique in amassing unparalleled data regarding mortality and YPLL among a cohort of heroin addicts.
Methods
Subjects
The sample was selected from men admitted to the California Civil Addict Program (CAP) during 1962-1964. CAP was a compulsory drug treatment program under the California Department of Corrections for heroin-dependent criminal offenders committed under court order. It was enacted in 1961 and was the only major publicly funded treatment available to California addicts in the 1960s. CAP consisted of an inpatient period followed by supervised community aftercare. From 1962-1964, 581 eligible subjects were selected for the present study under certain criteria including gender (male only), ethnicity (White, Hispanic, or Black), writ discharge, California resident for at least 5 years, and without previous civil commitments or dual felon and civil commitments at admission (McGlothlin et al., 1977). The sample was limited to male subjects because of the small number of female commitments to the CAP in the 1960s.
Subjects were face-to-face interviewed at three 10-year intervals since admission: 1974-75, 1985-86, and 1996-97. At the end of the 33-year follow-up period, 282 subjects had died. Using death certificates, all deaths were confirmed and the underlying cause of death was classified as coded by nosologists in accordance with the International Classification of Diseases, Ninth Revision (ICD-9; Division of Vital Statistics, 1999). The ICD-9 codes and associated causes of death are shown in Table 1.
Table 1.
Years of potential life lost (YPLL) and % YPLL ranked by cause of death for heroin addicts 33 year post treatment (Study from California, USA, 1962-1997)
| CAUSE OF DEATH | ICD-9 CODES | N | YPLL | %YPLL* | Annual mortality rate for specific cause |
|---|---|---|---|---|---|
| Heroin Overdose | E850.0 | 49 | 1153 | 22.3 | 0.26 |
| Chronic Liver Disease | 571 | 42 | 722 | 14.0 | 0.22 |
| Accidents | E800-E999(excluding E850- 858,E950-959,E980-989,E970);800- 950 |
23 | 527 | 10.2 | 0.12 |
| Cardiovascular Disease | 390-459 | 33 | 485 | 9.4 | 0.17 |
| Homicide | E960-E969 | 20 | 479 | 9.3 | 0.10 |
| Cancer | 140-208 | 32 | 281 | 5.4 | 0.16 |
| Poisoning or Injury | E980-E989 | 8 | 258 | 5.0 | 0.04 |
| Suicide | E950-E959 | 12 | 252 | 4.9 | 0.06 |
| Overdose - Misc. | E850-E858 (excluding E850.0) | 11 | 204 | 3.9 | 0.06 |
| Respiratory Disease | 460-519 | 11 | 184 | 3.6 | 0.06 |
| Drug Disorder | 304-305.9 | 9 | 179 | 3.5 | 0.05 |
| Stroke | 430-438 | 7 | 122 | 2.4 | 0.04 |
| Alcohol Disorder | 303 | 5 | 83 | 1.6 | 0.03 |
| Endocrine Disorders | 240-259 | 5 | 63 | 1.2 | 0.03 |
| Infectious Disease | 001-139 | 5 | 35 | 0.7 | 0.03 |
| Others | 520-579, E970, 345, 797-799,580- 629 |
10 | 145 | 2.8 | 0.05 |
%YPLL was calculated as cause specific YPLL divided by total YPLL
All study procedures were reviewed and approved by the UCLA Institutional Review Board. Eligible subjects signed informed consent forms to participate in the study.
Analysis
We calculated years of potential life lost (YPLL) before 65 years and the death age below which is considered premature, according to CDC's method. If the death age was greater than or equal to 65 years, YPLL was coded as 0 (Centers for Disease Control, 1993; 1989). The cause-specific YPLL in the sample was the sum of YPLL across individuals by their causes of death. YPLL per 1000 people (YPLL/1000) for each cause of death was the above number divided by the number of people 65 years or less in the cohort and the number of death in this cause group, and then times 1000. Addicts' death data were summarized at year 1996-1997, so national male data in 1997 were selected for the comparison (National Web-based Injury Statistics Query and Reporting System, 2005). In the U.S. population, the denominators for calculating YPLL/1000 were mid-year intercensal estimates provided by the U. S. Bureau of Census on magnetic tapes (Center for disease Control, 1986).
A series of one-sample t tests was carried out to test statistical differences in cause-specific YPLL/1000 between addict cohort to values from the U.S. general population. Analysis of variance (ANOVA) by GLM regression was used to test the YPLL differences among ethnic groups by SAS (version 8.1, SAS Institute Inc, Cary, NC).
Results
Heroin Addicts
At time of admission (1962-64), the original cohort had a mean age of 25.4 and consisted of 323 Hispanic (55.6%), 212 White (36.5%), and 46 African-American (7.9%) heroin abusers. More than 60% of the sample started using heroin before age 20 years. Before age 18 years, more than 80% of them had been arrested and 80% had tried marijuana.
At the first follow-up interview (1974-75), 80 subjects were deceased. The number of dead was 81 at 1984-85 and 121 at 1996-97. At the 33-year follow-up, the total number of deaths was 282 over 581 subjects (48.5%), and the annual mortality rate was 1.5%. Among the 282 deceased subjects, the mean age at death was 46.9 years (SD = 11.2), and 160 were Hispanic (56.7%), 98 were White (34.7%), and 24 African American (8.5%). On average, potential life lost before 65 in our cohort was 18.3 years per person (SD = 10.7). There were 13 cases (4.3%) with zero value because their death ages were beyond 65 years.
The leading cause of death was heroin overdose, with a total 49 deaths and YPLL value of 1153 (Tables 1). More than half of the death (n=29) from heroin overdose occurred within fifteen years from admission (data not shown), which indicated the early age of death and high YPLL. Chronic liver disease followed heroin overdose in YPLL rank (722, 14.0% of the total YPLL in this group) with 42 deaths. Accidents ranked third by YPLL (10.2%), though they ranked fifth by annual mortality rate (0.12%). Conversely, although cancer represented 32 deaths and ranked fourth by mortality (0.16%), it merited only sixth rank in YPLL (5.4%). Cardiovascular diseases held third place in mortality (0.17%) and fourth place (9.4%) in terms of YPLL. Homicide was ranked sixth in mortality ranking and fifth in YPLL. Gastrointestinal diseases, legal intervention, epilepsy, renal diseases, and ill-defined causes had less than 5 people for each; therefore, they were combined in the “others” category.
Ethnic Differences in YPLL
On average, Whites lost 19.5 years of potential life (SD = 10.7), Hispanics lost 19.0 years (SD = 10.3), and African Americans 9.2 years (SD = 9.5). The mean comparison of YPLL among the three ethnic groups was significant (p < 0.0001) from the ANOVA analysis. Further Tukey's post-hoc analysis revealed that African Americans had significantly less YPLL than Whites (diff = −10.3, 95% CI: −15.0, −5.7), and Hispanics (diff = −9.8, 95% CI: −14.3, −5.4). No notable disparity was found between Whites and Hispanics.
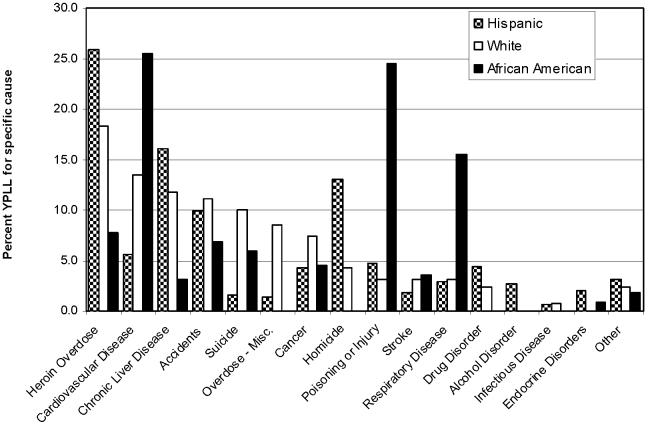
When the cause-specific YPLL was assessed, heroin overdose represented the greatest loss in years for both Whites (18.3% of YPLL) and Hispanics (25.8% of YPLL) (Figure 1). For African Americans, cardiovascular disease was listed as the first in terms of YPLL, followed by poisoning and respiratory diseases. Chronic liver disease was a close second for Hispanics, responsible for 16.1% of YPLL, but cardiovascular disease was second for Whites (13.5% of YPLL). Homicide figured prominently among Hispanics (13.1% of YPLL), ranking as the third leading cause of death, but only ranked ninth for Whites (4.3% of YPLL), and no African Americans died from homicide. Death from alcohol disorder was only found in Hispanics, not in Whites or African Americans.
Figure 1.
Ethnic Difference in %YPLL for Long-term Heroin Addicts (Study from California, USA, 1962-1997).
African Americans also showed no other drug-related deaths such as overdose from another drug (“overdose – miscellaneous”) or drug disorder.
Narcotics Addicts in Comparison with the U.S. Population
In the present study, heroin overdose, overdose-miscellaneous, poisoning, and accidents were combined to the category of “unintentional injuries” to conform to the national statistics. For the whole cohort, the highest discrepancy in YPLL/1000 between addict cohort and national population were unintentional injuries, homicide, and suicide (Table 2). Heart disease and cancer showed the least disparity. Cause-specific YPLL/1000 showed significant differences in all categories between abusers and US population with p values ranging from < 0.0001 to 0.007. In each ethnic group, all comparisons showed significant results except for African Americans, who had a marginal significant level (p=0.08). Whites exhibited the most discrepancy in suicide and liver disease, while Hispanics showed that in homicide and unintentional injuries. African Americans were a small group and each cause category contained no more than 6 deaths, so the total death was listed in the table.
Table 2.
Comparisons of YPLL per 1000 between narcotics addicts and U.S. population (Study from California, USA, 1962-1997)
|
CAUSE OF DEATH |
Narcotics | Addicts | US data (1997) |
Difference between Addicts and population |
||
|---|---|---|---|---|---|---|
| N | YPLL per 1000 |
YPLL per 1000 |
SD | P | ||
|
Total Males |
||||||
| Unintentional Injuries* | 91 | 42.64 | 11.95 | 30.69 | 18.51 | <0.0001 |
| Liver Disease | 42 | 31.14 | 1.32 | 29.82 | 13.96 | <0.0001 |
| Heart Disease | 33 | 26.62 | 8.29 | 18.33 | 17.08 | <0.0001 |
| Cancer | 32 | 15.91 | 7.75 | 8.16 | 12.16 | 0.0006 |
| Homicide | 21 | 43.22 | 4.38 | 38.84 | 18.81 | <0.0001 |
| Suicide | 12 | 38.04 | 4.56 | 33.48 | 20.10 | 0.0001 |
| Stroke | 7 | 31.57 | 1.17 | 30.40 | 20.11 | 0.007 |
| Total | 238 | 34.29 | 5.63 | 28.66 | 19.28 | <0.0001 |
|
Whites |
||||||
| Unintentional Injuries* | 36 | 39.60 | 11.47 | 28.13 | 18.78 | <0.0001 |
| Liver Disease | 11 | 37.22 | 1.50 | 35.72 | 16.33 | <0.0001 |
| Heart Disease | 15 | 31.16 | 8.43 | 22.73 | 17.09 | 0.0001 |
| Cancer | 13 | 19.65 | 8.12 | 11.53 | 10.32 | 0.002 |
| Homicide§ | 3 | 49.52 | 1.55 | - | - | - |
| Suicide | 8 | 43.48 | 5.11 | 38.37 | 20.40 | 0.001 |
| Stroke§ | 2 | 54.35 | 0.94 | - | - | - |
| Total | 88 | 35.90 | 5.30 | 30.60 | 19.11 | <0.0001 |
|
Hispanics |
||||||
| Unintentional Injuries* | 51 | 45.08 | 12.02 | 33.06 | 18.06 | <0.0001 |
| Liver Disease | 30 | 29.53 | 1.89 | 27.64 | 12.45 | <0.0001 |
| Heart Disease | 13 | 23.83 | 3.84 | 19.99 | 17.12 | 0.001 |
| Cancer | 13 | 18.11 | 4.01 | 14.10 | 12.94 | 0.002 |
| Homicide | 17 | 44.65 | 6.77 | 37.88 | 13.25 | <0.0001 |
| Suicide§ | 3 | 28.38 | 2.88 | - | - | - |
| Stroke§ | 4 | 24.46 | 0.92 | - | - | - |
| Total | 131 | 35.70 | 4.62 | 31.08 | 18.42 | <0.0001 |
|
African Americans |
||||||
| Total | 19 | 17 | 9.19 | 7.97 | 18.54 | 0.08 |
Unintentional Injuries included heroin overdose, overdose-miscellaneous, poisoning/injury and accidents
No comparison test was done for small group (N<5).
Discussion
The present study focused on premature mortality among a cohort of heroin addicts in California that have been followed for 33 years since their admission to the California Civil Addict Program. The major findings are that on average, the addict lost 18.3 years of potential life before age 65 and that the leading causes of premature death by YPLL measurement in this cohort were heroin overdose, chronic liver disease, and accidents. To our knowledge, while there are many studies investigating traditional mortality among heroin addicts (Brugal et al., 2005; Rathod et al., 2005; Sorensen et al., 2005; Termorshuizen et al., 2005; Termorshuizen et al., 2005; De Angelis et al 2004; Vlahov et al., 2004; Oppenheimer et al., 1994), only a limited number of studies have examined premature mortality with sufficient observational periods. The relationship between the average age at death and YPLL is central to understanding differences in premature mortality in our study. For example, accidents was ranked fifth in mortality rate and yet third in terms of YPLL, indicating that accidental deaths are more likely to occur at a younger age. The key to understanding the relationship between the absolute number of deaths for a given cause and the rank order of premature death as measured by YPLL is that the former ignores the age at death. In general, the younger the age at death among persons dying from a specific cause, the larger the disparity between the proportionate contribution to YPLL versus total mortality. Thus, by taking into consideration of the age at death, our study provides a useful supplement to the literature.
Several study limitations are noted before we discuss the study findings. First, the study sample is limited to male who started using heroin in the 1950s in California. Findings may not be generalizable to other drugs or user characteristics (women, recent heroin users, or those who lived outside California). In contrast to other studies showing high rates of mortality among heroin abusers due to HIV/AIDS (Sanchez-Carbonell and Seus, 2000; Obiri et al., 1998; Brugal et al., 2005; Galli and Musicco, 1994; Bartu et al., 2004), the present study only had three deaths from AIDS, and the cohort showed a low HIV infection rate (1.8%) among living subjects in 1997 (Hser et al., 2004). This finding, however, is consistent with the low HIV/AIDS death rate observed in the state of California. In California, the HIV death rate in 2004 was 3.9% (Kaiser Family Foundation, 2006) and HIV infection rates among injection drug users was stably low, around 2 to 6% (Carpenter et al, 1999; Longshore et al., 1994). Other possibilities for the low AIDS death in this cohort could be that subjects who were at high risk for HIV infection had died before the HIV/AIDS epidemic. AIDS was first recognized in 1981 in California, and the epidemic expanded and reached its peak in the early 1990s in the United States (MMWR, 2006). In the current study, 69% of the heroin overdose deaths happened before 1981, and 203 subjects (72%) were dead before the 1990s.
Another limitation of the study is that the comparison US population figures are based on cross-sectional data in 1997. Unfortunately comparable national YPLL data based on a representative longitudinal cohort do not exist. Nevertheless, the national YPLL data provide an important bench mark for the study findings.
Despite these study limitations, our study findings have important implications for studies of the premature mortality among heroin addicts. Consistent with previous literature (Hickman et al., 2003; Gossop et al., 2002; Digiusto et al., 2004; Galli & Musicco, 1994), heroin overdose is a leading cause of mortality for heroin addicts in our sample. Heroin overdose is also the leading cause of premature death since it occurred mostly at younger ages. This finding confirms previous studies reporting that fatal heroin overdoses typically occur when people are in their late 20s and early 30s (Darke and Zador, 1996). The second leading cause of premature death in this cohort is chronic liver disease, which should not be surprising given the high prevalence of hepatitis B and C and heavy drinking problems among heroin addicts (Hser et al., 2001; 2004). The death rate from accidents or injuries ranked as the third leading cause of premature death and the fifth for traditional mortality in this sample. Accidental deaths, including those from falls, firearms, motor vehicle accidents, and/or other injuries, happen more often in the younger age groups of the general population as well (Centers for Disease Control, 1991; Anderson et al., 2004; Mallonee, 2003). Other studies among heroin abusers also show a high death rate from accidents or injuries (Hickman et al, 2003; Sanchez-Carbonell & Seus, 2000; Gossop et al., 2002). Although longitudinal mortality data from general population are not available, the significantly higher YPLL among heroin addicts compared to the 1997 US population figures suggest that these social pathologies can be directly related to narcotics addiction and an associated lifestyle that includes crime and other addictions (e.g., heavy alcohol use) (Jarvik 1990).
Our study also revealed that African Americans showed lower premature mortality rates than did Whites or Hispanics, and their leading causes of death were different from the other two ethnic groups. The lower YPLL among African Americans in our sample conflict with national data which often showed that African Americans in general lost more potential life than other ethnic groups (Centers for Disease Control and Prevention, 1992) and African Americans were at a higher risk for death from homicide, fatal injury, and HIV/AIDS than other ethnic groups (Blumstein et al., 2000; Chu and Sorenson, 1996; Anderson et al., 2004; Center of Disease Control and Prevention, 1996). The rate of tobacco smoking among our sample has been reported to be up to 98% (Hser et al., 1993), which may partly explain the greater mortality due to heart diseases reported among African Americans and Whites. Galea and colleagues reported that in New York City, African Americans had a lower death rate from opiate overdose or alcohol overdose than did Whites and Latinos (Galea et al., 2003), which may corroborate why overdose was not the leading cause of death for African Americans in this California study. Since our study included only a small number of African Americans, further studies with larger samples of African Americans heroin addicts are needed to replicate the present findings as well as to provide an in-depth understanding of the nature and causes of the ethnic differences in premature death.
Addressing problems stemming from heroin addiction requires intervention programs that reduce unnecessary loss of life. The federal government's primary agency for drug abuse research, the National Institute on Drug Abuse (NIDA), has concluded that methadone is an effective method for treating heroin addiction. When patients are in methadone treatment, criminal behavior dramatically decreases and gainful employment increases (Harwood et al., 1992). Methadone maintenance treatment also has a significant effect on decreasing the spread of HIV/AIDS, hepatitis B and C, tuberculosis, and sexually transmitted diseases (Dolan et al., 2005). However, access to treatment remains extremely limited. Because of geographical constraints and limited treatment slots, current licensed and centralized methadone maintenance programs reach only an estimated 14% of patients with opioid dependence (Rounsaville and Kosten, 2000). Thus, deficient treatment capacity might be one of the factors responsible for increased premature deaths and YPLL, among the many other negative consequences to society and individuals.
This study provides unique and important information about the underlying nature of the premature mortality related to long-term heroin addiction. Future studies should replicate and extend these analyses by including more African Americans and women. By evaluating YPLL values, the burden of heroin-induced premature mortality can be revealed and considered in public health efforts. Resources may be prioritized to health education and treatment efforts for the populations most in need of public health interventions.
Precis
This study examined years of potential life lost (YPLL) and mortality among long-term narcotics addicts. YPLL differences among ethnic groups and between addicts and the U.S. population were investigated.
Acknowledgments
This research was supported by the National Institute on Drug Abuse Grants DA09169, K02DA00139, and DA016383-01A1 to Dr. Hser and DA07272 to Dr. Smyth. The authors thank Dr. Richard Selik at CDC for his valuable advice, and staff at the UCLA Integrated Substance Abuse Programs for their support in manuscript preparation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anderson RN, Minino AM, Fingerhut LA, Warner M, Heinen MA. Deaths: injuries, 2001. Natl Vital Stat Rep. 2004;52(21):1–86. [PubMed] [Google Scholar]
- Barr HL, Antes D, Ottenberg DJ, Rosen A. Mortality of treated alcoholics and drug addicts: The benefits of abstinence. J Stud Alcohol. 1984;45(5):440–452. doi: 10.15288/jsa.1984.45.440. [DOI] [PubMed] [Google Scholar]
- Bartu A, Freeman NC, Gawthorne GS, Codde JP, Holman CD. Mortality in a cohort of opiate and amphetamine users in Perth, Western Australia. Addiction. 2004;99(1):53–60. doi: 10.1111/j.1360-0443.2004.00602.x. [DOI] [PubMed] [Google Scholar]
- Blumstein A, Rivara FP, Rosenfeld R. The rise and decline of homicide--and why. Annu Rev Public Health. 2000;21:505–41. doi: 10.1146/annurev.publhealth.21.1.505. Review. [DOI] [PubMed] [Google Scholar]
- Booth MW, Castro RG, Anglin MD. What do we know about Hispanic substance abuse? A review of the literature. In: Glick R, Moore J, editors. Drugs in Hispanic Communities. Rutgers University Press; New Brunswick, NJ: 1991. pp. 21–43. [Google Scholar]
- Brugal MT, Domingo-Salvany A, Puig R, Barrio G, Garcia de Olalla de la Fuente L. Evaluating the impact of methadone maintenance programmes on mortality due to overdose and aids in a cohort of heroin users in Spain. Addiction. 2005;100:981–9. doi: 10.1111/j.1360-0443.2005.01089.x. [DOI] [PubMed] [Google Scholar]
- Carpenter CL, Longshore D, Annon K, Annon JJ, Anglin MD. Prevalence of HIV-1 among recent arrestees in Los Angeles County, California: serial cross-sectional study, 1991-1995. J Acquir Immune Defic Syndr. 1999;21(2):172–7. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Twenty-Five Years of HIV/AIDS --- United States, 1981—2006. MMWR. Morb Mortal Wkly Rep. 2006;55(21):589–92. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Suicide among Hispanics--United States, 1997-2001. MMWR. 2004;53(22):478–81. [PubMed] [Google Scholar]
- Centers for Disease Control Premature mortality in the United States: public health issues in the use of years of potential life lost. MMWR. 1986;35:1S–11S. [PubMed] [Google Scholar]
- Centers of Disease Control and Prevention Years of potential life lost before age 65 – Unites States, 1990 and 1991. MMWR. 1993;42:251–253. [PubMed] [Google Scholar]
- Centers of for Disease Control and Prevention Trend in years of potential life lost before age 65 among whites and blacks 1989. MMWR. 1992;41:889–891. [PubMed] [Google Scholar]
- Centers for Disease Control (CDC) Injury Mortality Atlas of the United States, 1979-1987. MMWR Morb Mortal Wkly Rep. 1991;40(49):846–8. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Trends in rates of homicide--United States, 1985-1994. MMWR Morb Mortal Wkly Rep. 1996;45(22):460–4. [PubMed] [Google Scholar]
- Chu LD, Sorenson SB. Trends in California homicide, 1970 to 1993. West J Med. 1996;165(3):119–25. [PMC free article] [PubMed] [Google Scholar]
- Copeland L, Budd J, Robertson JR, Elton RA. Changing patterns in causes of death in a cohort of injecting drug users, 1980-2001. Archives of Internal Medicine. 2004;164(11):1214–1220. doi: 10.1001/archinte.164.11.1214. [DOI] [PubMed] [Google Scholar]
- Darke S, Zabor D. Fatal heroin overdose: a review. Addiction. 1996;91:1765–1772. doi: 10.1046/j.1360-0443.1996.911217652.x. [DOI] [PubMed] [Google Scholar]
- De Angelis D, Hickman M, Yang SY. Estimating long-term trends in the incidence and prevalence of opiate use/injecting drug use and the number of former users: Back-calculation methods and opiate overdose deaths. Am J Epidemiology. 2004;160(10):994–1004. doi: 10.1093/aje/kwh306. [DOI] [PubMed] [Google Scholar]
- Desenclos JCA, Hahn RA. Years of potential life lost before age 65, by race, Hispanic origins and sex – United States, 1986-1988. MMWR. 1992;41:13–23. [PubMed] [Google Scholar]
- Division of Vital Statistics. National Center for Health Statistics. Centers for Disease Control and Prevention 1999 [Google Scholar]
- Digiusto E, Shakeshaft A, Ritter A, O'Brien S, Mattick RP, The NEPOD Research Group Serious adverse events in the Australian National Evaluation of Pharmacotherapies for Opioid Dependence (NEPOD) Addiction. 2004;99(4):450–60. doi: 10.1111/j.1360-0443.2004.00654.x. [DOI] [PubMed] [Google Scholar]
- Dolan KA, Shearer J, White B, Zhou J, Kaldor J, Wodak AD. Four-year follow-up of imprisoned male heroin users and methadone treatment: mortality, reincarceration and hepatitis C infection. Addiction. 2005;100(6):820–8. doi: 10.1111/j.1360-0443.2005.01050.x. [DOI] [PubMed] [Google Scholar]
- Galli M, Musicco M. Mortality of intravenous drug users living in Milan, Italy: role of HIV-1 infection. COMCAT Study Group. AIDS. 1994;8(10):1457–63. doi: 10.1097/00002030-199410000-00013. [DOI] [PubMed] [Google Scholar]
- Galea S, Ahern J, Tardiff K, Leon A, Coffin PO, Derr K, Vlahov D. Racial/ethnic disparities in overdose mortality trends in New York City, 1990-1998. J Urban Health. 2003;80(2):201–11. doi: 10.1093/jurban/jtg023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- General Accounting Office . A health status indicator for targeting federal aid to states (GAO report no. GAO/HEHS-97-13) General Accounting Office; Gaithersburg: 1996. [Google Scholar]
- Haastrup S, Jepsen PW. Seven year follow-up of 300 young opiod addicts. Acta Psychiatr Scand. 1988;77(1):503–509. [Google Scholar]
- Gossop M, Stewart D, Treacy S, Marsden J. A prospective study of mortality among drug misusers during a 4-year period after seeking treatment. Addiction. 2002;97(1):39–47. doi: 10.1046/j.1360-0443.2002.00079.x. [DOI] [PubMed] [Google Scholar]
- Harwood H, Fountain D, Livermore G. The economic costs of alcohol and drug abuse in the United States, 1992. National Institute on Drug Abuse & National Institute on Alcohol Abuse and Alcoholism. 1998 [Google Scholar]
- Hickman M, Carnwath Z, Madden P, Farrell M, Rooney C, Ashcroft R, Judd A, Stimson G. Drug-related mortality and fatal overdose risk: pilot cohort study of heroin users recruited from specialist drug treatment sites in London. J Urban Health. 2003;80(2):274–87. doi: 10.1093/jurban/jtg030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hser YI, Anglin MD, Powers K. A 24-Year follow-up of California Narcotics Addicts. Arch Gen Psychiatry. 1993;50:577–584. doi: 10.1001/archpsyc.1993.01820190079008. [DOI] [PubMed] [Google Scholar]
- Hser YI, McCarthy WJ, Anglin MD. Tobacco use as a distal predictor of Mortality among Long-Term Narcotics Addicts. Preventive Medicine. 1994;23:61–69. doi: 10.1006/pmed.1994.1009. [DOI] [PubMed] [Google Scholar]
- Hser YI, Grella CG, Hoffman V, Anglin MD. A 33-year follow-up of narcotics addicts. Archives of General Psychiatry. 2001;58:503–508. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- Hser YI, Gelberg L, Hoffman V, Grella CE, McCarthy W, Anglin MD. Health conditions among aging narcotics addicts: medical examination results. J Behav Med. 2004;27(6):607–22. doi: 10.1007/s10865-004-0005-x. [DOI] [PubMed] [Google Scholar]
- Jarvik ME. The Drug Dilemma: Manipulating the Demand. Science. 1990;250:387–391. doi: 10.1126/science.2218544. [DOI] [PubMed] [Google Scholar]
- Joe GW, Lehman W, Simpson DD. Addict death rates during a four-year posttreatment follow-up. Am J Pub Health. 1982;72(7):703–709. doi: 10.2105/ajph.72.7.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joe GW, Simpson DD. Mortality rates among opioid addicts in a longitudinal study. Am J Pub Health. 1987;77(3):347–348. doi: 10.2105/ajph.77.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John U, Hanke M. Tobacco- and alcohol-attributable mortality and years of potential life lost in Germany. European Journal of Public Health. 2003;13(3):275–277. doi: 10.1093/eurpub/13.3.275. [DOI] [PubMed] [Google Scholar]
- Jones JH, Weir WB. Cocaine-induced chest pain. Clin Lab Med. 2006;26(1):127–46. doi: 10.1016/j.cll.2006.01.010. viii. Review. [DOI] [PubMed] [Google Scholar]
- Lai DJ, Tarwater PM, Hardy RJ. Measuring the impact of HIV/AIDS, heart disease and malignant neoplasms on life expectancy in the USA from 1987 to 2000. Public Health. 2006;120(6):486–92. doi: 10.1016/j.puhe.2005.12.009. [DOI] [PubMed] [Google Scholar]
- Longshore D, Anglin MD. HIV prevalence and incidence among injection drug users in Los Angeles. J Acquir Immune Defic Syndr. 1994;7(7):738–9. [PubMed] [Google Scholar]
- Mallonee S. Injuries among Hispanics in the United States: implications for research. J Transcult Nurs. 2003;14(3):217–26. doi: 10.1177/1043659603014003008. Review. [DOI] [PubMed] [Google Scholar]
- McGlothlin WH, Anglin DM, Wilson BD. A Follow-up of Admissions to the California. Civil Addict Program. Am J Drug Alcohol Abuse. 1977;4(2):179–99. doi: 10.3109/00952997709002759. [DOI] [PubMed] [Google Scholar]
- National Web-based Injury Statistics Query and Reporting System (WISQARS) Center for Injury Prevention and Control 2005 http://webappa.cdc.gov/sasweb/ncipc/ypll9.html; accessed on 7/18/2005.
- Obiri UG, Fordyce EJ, Singh PT, Forlenza S. Effects of HIV/AIDS Versus Other Causes of Death on Premature Mortality in New York City, 1983-1994. Am J Epidemiol. 1998;147:840–45. doi: 10.1093/oxfordjournals.aje.a009537. [DOI] [PubMed] [Google Scholar]
- Ogborne AC, Stimson GV. Follow-up of a representative sample of heroin addicts. Int J Addict. 1975;10(6):1061–1071. doi: 10.3109/10826087509028361. [DOI] [PubMed] [Google Scholar]
- Oppenheimer E, Tobutt C, Taylor C, Andrew T. Death and survival in a cohort of heroin addicts from London clinics: a 22-year follow-up study. Addiction. 1994;89(10):1299–308. doi: 10.1111/j.1360-0443.1994.tb03309.x. [DOI] [PubMed] [Google Scholar]
- Pletcher MJ, Kiefe CI, Sidney S, Carr JJ, Lewis CE, Hulley SB. Cocaine and coronary calcification in young adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am Heart J. 2005;150(5):921–6. doi: 10.1016/j.ahj.2005.04.016. [DOI] [PubMed] [Google Scholar]
- Rathod NH, Addenbrooke WM, Rosenbach AF. Heroin dependence in an English town: 33-year follow-up. Br J Psychiatry. 2005;187:421–5. doi: 10.1192/bjp.187.5.421. [DOI] [PubMed] [Google Scholar]
- Rivara FP, Ebel BE, Garrison MM, Christakis DA, Wiehe SE, Levy DT. Prevention of Smoking-Related Deaths in the United States. Am J Prev Med. 2004;27(2):118–125. doi: 10.1016/j.amepre.2004.04.014. [DOI] [PubMed] [Google Scholar]
- Rogers RG. Sociodemographic characteristics of long-lived and healthy individuals. Popul Dev Rev. 1995;21:33–58. [Google Scholar]
- Rounsaville BJ, Kosten TR. Treatment for opioid dependence: quality and access. JAMA. 2000;283(10):1337–9. doi: 10.1001/jama.283.10.1337. [DOI] [PubMed] [Google Scholar]
- Sanchez-Carbonell X, Seus L. Ten-year survival analysis of a cohort of heroin addicts in Catalonia: the EMETYST project. Addiction. 2000;95(6):941–8. doi: 10.1046/j.1360-0443.2000.95694110.x. [DOI] [PubMed] [Google Scholar]
- Selik RM, Chu SY. Years of potential life lost due to HIV infection in the United States. AIDS. 1997;11:1635–1639. doi: 10.1097/00002030-199713000-00013. [DOI] [PubMed] [Google Scholar]
- Sorensen HJ, Jepsen PW, Haastrup S, Juel K. Drug-use pattern, comorbid psychosis and mortality in people with a history of opioid addiction. Acta Psychiatrica Scandinavica. 2005;111(3):244–249. doi: 10.1111/j.1600-0447.2004.00445.x. [DOI] [PubMed] [Google Scholar]
- Stewart SD. Effect of changing mortality on the working life of American men and women, 1970-1990. Soc Biol. 1997;44(12):153–8. doi: 10.1080/19485565.1997.9988942. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2003 National Survey on Drug Use and Health: National Findings. Office of Applied Studies; Rockville, MD: 2004. (NSDUH Series H–25, DHHS Publication No. SMA 04–3964). [Google Scholar]
- Termorshuizen F, Krol A, Prins M, Geskus R, van den Brink W, van Ameijden EJ. Long-term outcome of chronic drug use - The Amsterdam Cohort Study among Drug Users. Am J Epidemiology. 2005;161(3):271–279. doi: 10.1093/aje/kwi035. [DOI] [PubMed] [Google Scholar]
- The Kaiser Family Foundation . Data Source: The Centers for Disease Control and Prevention (CDC), National Center for Health Statistics, Division of Vital Statistics, National Vital Statistics Report. 13 Vol. 54. 2006. , Table 29, April 19, 2006. statehealthfacts.org, access at 7/3/2006.
- Vlahov D, Wang CL, Galai N, Bareta J, Mehta SH, Strathdee SA, Nelson KE. Mortality risk among new onset injection drug users. Addiction. 2004;99(8):946–954. doi: 10.1111/j.1360-0443.2004.00780.x. [DOI] [PubMed] [Google Scholar]
- Wise RP, Livengood JR, Berkelman RL, Goodman RA. Methodological alternatives for measuring premature mortality. Am J Prev Med. 1988;4:268–73. [PubMed] [Google Scholar]