Abstract
Introduction
To date, there is no evidence showing a benefit from any advanced cardiac life support (ACLS) medication in out-of-hospital cardiac arrest (OOHCA), despite animal data to the contrary. One explanation may be a difference in the time to first drug administration. Our previous work has shown the mean time to first drug administration in clinical trials is 19.4 minutes. We hypothesized that the average time to drug administration in large animal experiments occurs earlier than in OOHCA clinical trials.
Methods
We conducted a literature review between 1990 and 2006 in MEDLINE using the following MeSH headings: swine, dogs, resuscitation, heart arrest, EMS, EMT, ambulance, ventricular fibrillation, drug therapy, epinephrine, vasopressin, amiodarone, lidocaine, magnesium, and sodium bicarbonate. We reviewed the abstracts of 331 studies and 197 full manuscripts. Exclusion criteria included: non-peer reviewed, all without primary animal data, and traumatic models. From these, we identified 119 papers that contained unique information on time to medication administration. The data are reported as mean, ranges, and 95% confidence intervals. Mean time to first drug administration in animal laboratory studies and clinical trials was compared with a t-test. Regression analysis was performed to determine if time to drug predicted ROSC.
Results
Mean time to first drug administration in 2378 animals was 9.5 minutes (range 3.0–28.0; 95% CI around mean 2.78, 16.22). This is less than the time reported in clinical trials (19.4 min, p<0.001). Time to drug predicted ROSC (Odds Ratio 0.844; 95% CI 0.738, 0.966).
Conclusion
Shorter drug delivery time in animal models of cardiac arrest may be one reason for the failure of animal studies to translate successfully into the clinical arena.
Keywords: cardiopulmonary resuscitation (CPR), cardiac arrest, resuscitation, drug therapy
1. Introduction
Despite numerous clinical trials, survival rates in out-of-hospital cardiac arrest (OOHCA) remain low. To date, there is no evidence that supports the use of ACLS drugs in this setting. [1–3] Animal studies, in contrast, have demonstrated superior survival rates with drug use. [4–13] One reason for failure of animal studies to translate to clinical practice may be the time at which the first drug is delivered. Previous work has demonstrated the average time to first drug administration in clinical trials is 19.4 minutes (range 13.3–25.0; 95% CI around the mean 12.8, 25.9). [14, Appendix] Thus, clinically, these drugs are administered during the late metabolic phase of cardiac arrest. Consequently, it is not surprising they are ineffective. Based on our laboratory and clinical experience, we hypothesized that the average time to drug administration in large animal experiments occurs earlier than in OOHCA clinical trials.
2. Methods
We conducted a comprehensive literature review between 1990 and 2006 in MEDLINE using the following MeSH headings: swine, dogs, resuscitation, heart arrest, EMS, EMT, ambulance, ventricular fibrillation, drug therapy, epinephrine, vasopressin, amiodarone, lidocaine, magnesium, and sodium bicarbonate. We used no language restriction. We used OVID to search MEDLINE and obtain the abstracts. All abstracts were printed and two reviewers (JCR & JCR) jointly reviewed all abstracts. We eliminated the following from further review: small animal; non-peer reviewed; all without primary animal data (editorials, case reports, review articles, letters, practice guidelines); studies modeling trauma, sepsis, or burns; studies performed in vitro; and those studies were no exogenous medications were given. We then reviewed independently the full manuscripts of all remaining papers for data describing the time to first medication administration. Both reviewers then compared the articles captured.
The type of animal, number of animals, time to first drug administration, route of medication administration, type of medication, method of delivery (bolus vs. infusion), return of spontaneous circulation (ROSC) and short-term survival were abstracted from the articles. Unlike most meta-analyses where we compare the effect size as a function of treatment compared to control across the studies, our analysis compares the mean response time to the ‘minimally acceptable’ time. Consequently, our effect size is the sample mean and our goal is to combine the study results, derive a confidence interval for mean response time and compare that range to what the guidelines define as appropriate. Given that variances were not available for all studies, we used the weighted study sample sizes relative to the entire sample size across the 119 studies to estimate the effect size variance: [15]
weighti = Ni Where Ni is the sample size for each study
And which is the total sample size across all the studies.
Due to the large differences in sample sizes across the studies (and obvious heterogeneity), we chose to analyze the results using the random effects model as recommended by Hunter and Smith. [16] This approach accounts for the variability between studies and is a more conservative method to estimate the confidence interval around the mean. We used Microsoft Excel XP 2002 (Redmond, WA) and STATA 9.0 (College Station, TX) to record and analyze the data. We report the mean times, ranges, and the respective 95% confidence intervals around the mean. We next compared the data from this review with that of our previous study in clinical trials to determine if time to drug predicted ROSC. A t-test was completed to determine if the mean time to drug administration was different between the clinical trial data and the animal trial data. Multivariate logistic regression was used to determine predictors of ROSC in the animal studies. Predictor variables included: time to drug, route of delivery (IV or ET), induction of hypothermia, and type of drug. Time to drug was analyzed as a continuous variable in this regression model. The Hosmer-Lemeshow test was used to assess goodness of fit.
3. Results
Our literature review yielded 332 abstracts. Of these, 197 were selected for review of the full manuscript. The reason for exclusion is presented in Figure 1. Of the 197 manuscripts, 119 contained unique data on time to first drug administration. There was 100% agreement between both reviewers on which studies to include in our analysis. The average time to first medication administration in these 2378 animals was 9.5 minutes (range 3.0–28.0; 95% CI around mean 2.78, 16.22). This was less than our previously reported clinical trial data (19.4 minutes; p < 0.001). In the regression analysis, time to drug was the lone predictor of ROSC (Odds Ratio 0.844; 95% CI 0.738, 0.966). This regression model had acceptable fit (Hosmer-Lemeshow value 0.195).
Figure 1.
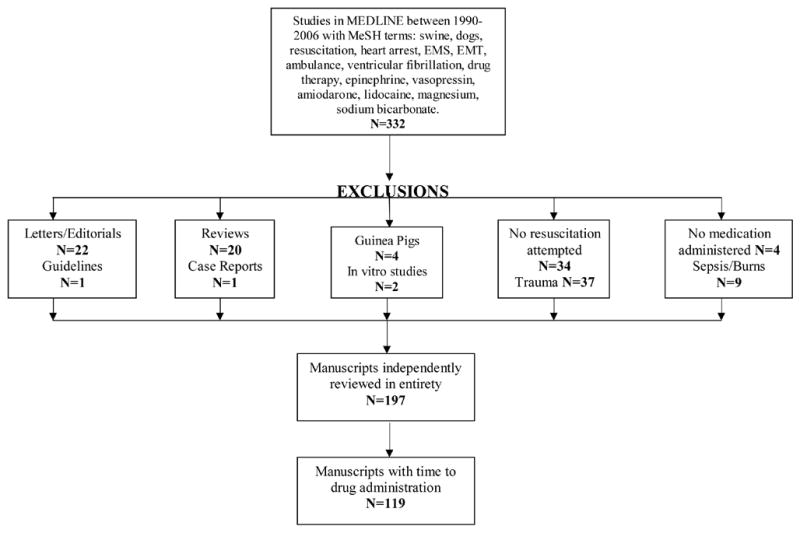
Results of decision algorithm used.
4. Discussion
Drugs are administered approximately 10 minutes earlier in animal studies than in clinical trials. Specifically, animal studies administer drugs during the circulatory phase while clinical trials administer drugs during the metabolic phase. This delay may be one reason animal studies have failed to translate to clinical practice.
Weisfeldt and Becker have proposed a three phase model of cardiac arrest. [17] The first phase is electrical and lasts from 0–4 minutes. During this initial phase, ventricular fibrillation responds well to countershock. The second phase, from 4–10 minutes, is the circulatory phase. Both animal and human data support the initiation of CPR before attempting defibrillation to ensure adequate tissue oxygenation and perfusion. Data in this phase also supports supplementary administration of vasopressors with CPR. Immediate rescue shock alone has been ineffective during this phase. [13, 18, 19] The third phase of cardiac arrest occurs beyond 10 minutes. Little research has been conducted in this metabolic phase, even though it is usually during this phase that advanced life support is initiated and patients receive their first dose of medication. One study has suggested that cardiopulmonary bypass may be effective and result in neurologically intact survivors. [20] Using a swine model, we demonstrated recently that these phases may be extended through the use of an optimal resuscitation incorporating CPR and a drug cocktail prior to rescue countershock. [21] This model would predict a 21% probability of ROSC with drug administration at 19.4 minutes, and an 83% probability of ROSC with drug administration at 9.5 minutes.
The 2005 ILCOR guidelines downplay the import of medication administration. [22] In light of this literature review and our own experience with animal models, we believe that these drugs are not inert, but only effective when administered during the circulatory phase of cardiac arrest. These data suggest a shift in resuscitation care to improve drug delivery in the out-of-hospital setting. One method employed to decrease time to drug is system-wide changes in dispatch protocols. These changes have been shown to decrease time to medication administration by 3.5 minutes. [23] A second method to improve drug delivery time is to provide first responders with the ability to establish intraosseus access and provide drugs. We have demonstrated previously that the use of an intraosseus needle by prehospital basic life support providers is feasible and compares favorably with prior studies of advanced life support intravenous catheter placement. [24, 25] If drug delivery continues to occur late during resuscitative efforts, we are unlikely to find a benefit from any drug or cocktail of drugs in the clinical setting.
Our study has several limitations. First, it is limited to a retrospective review of the literature. There is the possibility that studies have been missed, but we believe this to have been minimized by our inclusive search criteria and extensive review. Second, the animals used are young, healthy animals. The cardiovascular physiology of these animals may be different than that of many people who experience OOHCA. Third, time to drug delivery is reliably and consistently recorded in animal studies. However, in clinical settings this data is limited due to being self-reported. The time from collapse to EMS activation is rarely known. Finally, the outcomes assessed are ROSC and short-term survival. Most animal studies do not provide information on neurologically-intact survival, which is the most relevant outcome from the perspective of the patient. We note that previous studies showing short-term benefits have failed to translate to long-term survival. [26]
5. Conclusions
Time to first drug delivery in animal resuscitation studies occurs approximately 10 minutes earlier than in clinical trials. In animal trials, time to drug predicts ROSC. These data suggest that one reason for animal studies to translate into clinical practice may be delay to drug delivery. We suggest that an emphasis on gaining vascular access may improve drug effectiveness.
Supplementary Material
Table 1.
Time to drug administration (minutes) by study. Subject group given for studies comparing interventions.
| Study | Number of subjects | Time to drug Administration | First Medication Received |
|---|---|---|---|
| Krieter H, et al. [27] | 10 | 8 | Epinephrine |
| Loeckinger A, et al. [28] | 8 | 7 | Vasopressin |
| 10 | 7 | Epinephrine | |
| Krismer AC, et al. [29] | 7 | 7 | Vasopressin |
| 6 | 7 | Epinephrine | |
| Little CM, et al. [30] | 13 | 13 | Angiotensin II |
| 11 | 13 | Epinephrine | |
| 13 | 13 | Angiotensin II + epinephrine | |
| Johansson J, et al. [31] | 24 | 7 | Epinephrine |
| Bahlmann L, et al. [32] | 14 | 18 | Vasopressin |
| Behringer W, et al. [33] | 11 | 9 | Epinephrine |
| Voelckel WG, et al. [34] | 12 | 16 | Vasopressin |
| 6 | 16 | Vasopressin + epinephrine | |
| Holzer M, et al. [35] | 19 | 10 | Endothelin-1 |
| 6 | 10 | Epinephrine | |
| Johansson J, et al. [36] | 12 | 7 | Vasopressin |
| 12 | 7 | Epinephrine | |
| Prengel AW, et al. [37] | 7 | 7 | Epinephrine |
| 7 | 7 | Vasopressin | |
| 7 | 7 | Vasopressin + epinephrine | |
| Amann A, et al. [38] | 16 | 7 | Vasopressin |
| 9 | 7 | Epinephrine | |
| 11 | 7 | Novel vasopressor | |
| 12 | 4 | Epinephrine | |
| 11 | 4 | Vasopressin | |
| 2 | 10 | Vasopressin | |
| 3 | 10 | Epinephrine | |
| Adams JA, et al. [39] | 12 | 18 | Vasopressin |
| Schwarz B, et al. [40] | 7 | 18 | Vasopressin |
| 7 | 28 | Amiodarone | |
| Vukmir RB, et al. [41] | 12 | 5 | Epinephrine |
| 20 | 15 | Epinephrine | |
| Manning JE, et al. [42] | 5 | 10.5 | Epinephrine |
| 5 | 10.5 | Aortic occlusion + epinephrine | |
| 5 | 10.5 | Aortic occlusion + Intraaortic epinephrine | |
| Strohmenger HU, et al. [43] | 7 | 7 | Epinephrine |
| 7 | 7 | Vasopressin | |
| Ayoub IM, et al. [44] | 8 | 10 | Cariporide |
| 8 | 10 | Epinephrine | |
| 8 | 10 | Cariporide + epinephrine | |
| Stadlbauer KH, et al. [45] | 6 | 7 | Epinephrine |
| 6 | 7 | Epinephrine + vasopressin | |
| Mayr VD, et al. [46] | 6 | 12 | Epinephrine |
| 6 | 12 | Vasopressin | |
| 6 | 12 | High-dose epinephrine + vasopressin | |
| 6 | 12 | Standard-dose epinephrine + vasopressin | |
| Amann A, et al. [47] | 11 | 7 | Vasopressin |
| 5 | 7 | Epinephrine | |
| 5 | 12 | Vasopressin | |
| 4 | 12 | Epinephrine | |
| Hilwig RW, et al. [48] | 12 | 8 | Standard-dose epinephrine |
| 12 | 8 | Standard-dose epinephrine + β blocker | |
| 10 | 8 | High-dose epinephrine + β blocker | |
| 10 | 8 | Phenylephrine + β blocker | |
| Nozari A, et al. [49] | 11 | 7 | Aortic occlusion + epinephrine |
| 12 | 7 | Epinephrine IV | |
| Seaberg DC et al. [9] | 7 | 9 | Combination therapy including epinephrine + novel cardiocerebral-protective agent |
| 9 | 9 | Magnesium | |
| 8 | 10 | Epinephrine | |
| Menegazzi JJ, et al. [13] | 9 | 9 | Standard-dose epinephrine |
| 9 | 12 | Standard-dose epinephrine | |
| 9 | 15 | Standard-dose epinephrine | |
| 9 | 12 | Standard-dose epinephrine | |
| 7 | 15 | Standard-dose epinephrine | |
| 9 | 8 | High-dose epinephrine | |
| 8 | 11 | High-dose epinephrine | |
| Prengel AW, et al. [50] | 8 | 5 | Epinephrine |
| 8 | 5 | Vasopressin | |
| Wenzel V, et al. [51] | 8 | 18 | Vasopressin |
| 8 | 18 | Vasopressin + epinephrine | |
| Wenzel V, et al. [52] | 7 | 7 | Vasopressin |
| 7 | 7 | Vasopressin + nitroglycerin | |
| Lurie KG, et al. [53] | 12 | 8 | Epinephrine + vasopressin |
| 12 | 8 | Epinephrine | |
| Berg RA, et al. [54] | 12 | 11 | Epinephrine |
| Holzer M, et al. [55] | 21 | 10 | Endothelin-1 |
| 6 | 10 | Epinephrine | |
| Prengel AW, et al. [56] | 6 | 6 | Epinephrine |
| Bleske BE, et al. [57] | 7 | 5 | Intra-nasal epinephrine |
| 6 | 5 | Epinephrine IV | |
| Tang W, et al. [58] | 10 | 9 | Epinephrine |
| Lindner KH, et al. [59] | 14 | 5.5 | High-dose epinephrine |
| Lindner KH, et al. [60] | 7 | 7 | Epinephrine |
| 21 | 7 | Vasopressin | |
| Idris AH, et al. [61] | 24 | 17 | Epinephrine |
| Bar-Joseph G, et al. [62] | 36 | 17 | Epinephrine |
| Paradis NA, et al. [63] | 13 | 8 | Epinephrine |
| Bleske BE, et al. [64] | 26 | 6 | Epinephrine |
| Lindner KH, et al. [65] | 28 | 8 | Epinephrine |
| Wolf CF, et al. [66] | 7 | 7 | Epinephrine |
| 7 | 7 | Norepinephrine | |
| 7 | 7 | Vasopressin | |
| Blecic S, et al. [67] | 6 | 9 | Atropine |
| 6 | 9 | Atropine | |
| Prengel AW, et al. [68] | 8 | 5 | Epinephrine |
| 8 | 5 | Vasopressin | |
| Berg RA, et al. [69] | 15 | 11 | Standard-dose epinephrine |
| 15 | 11 | High-dose epinephrine | |
| Strohmenger HU, et al. [70] | 21 | 7 | Vasopressin |
| Bleske BE, et al. [71] | 9 | 12 | Bicarbonate |
| 9 | 13 | Epinephrine | |
| Menegazzi JJ, et al. [5] | 9 | 8 | Epinephrine |
| 9 | 9 | Epinephrine | |
| Manning JE, et al. [72] | 16 | 12 | Epinephrine |
| Wenzel V, et al. [73] | 9 | 18 | Epinephrine |
| 9 | 18 | Vasopressin | |
| Mayr VD, et al. [74] | 7 | 3 | Epinephrine |
| 7 | 3 | Vasopressin | |
| 7 | 3 | Epinephrine + vasopressin | |
| Gervais HW, et al. [75] | 7 | 8 | Epinephrine |
| 7 | 8 | Phenylephrine | |
| 7 | 8 | Epinephrine + β blocker | |
| Nejman GD, et al. [76] | 6 | 13 | Novel vasopressor |
| Achleitner U, et al. [77] | 5 | 7 | Vasopressin |
| 5 | 7 | Epinephrine | |
| 5 | 12 | Vasopressin | |
| 6 | 12 | Epinephrine | |
| Neimann JT, et al. [78] | 14 | 8 | Epinephrine |
| 14 | 7.5 | Epinephrine | |
| Voelckel WG, et al. [79] | 12 | 7 | Vasopressin |
| Lindner KH, et al. [80] | 7 | 7 | Epinephrine |
| 7 | 7 | Vasopressin | |
| Gazmuri RH, et al. [81] | 8 | 8 | Bicarbonate |
| 8 | 8 | Carbicarb | |
| Bleske BE, et al. [82] | 7 | 6 | Intra-nasal epinephrine |
| Jameson SJ, et al. [83] | 19 | 18 | Epinephrine |
| Wenzel V, et al. [84] | 7 | 7 | Vasopressin IV |
| 9 | 7 | Endobronchial Vasopressin | |
| Lindner KH, et al. [85] | 7 | 5 | Epinephrine |
| 7 | 5 | Norepinephrine | |
| Angelos MG, et al. [86] | 8 | 15 | Standard-dose epinephrine |
| 8 | 15 | High-dose epinephrine | |
| Prengel AW, et al. [87] | 7 | 7 | Vasopressin |
| 7 | 7 | Epinephrine | |
| Littmann L, et al. [88] | 20 | 6.5 | Epinephrine |
| 20 | 6 | Epinephrine | |
| DeBehnke DJ, et al. [89] | 8 | 15 | High-dose epinephrine |
| 8 | 15 | Standard-dose epinephrine | |
| Manning JE, et al. [90] | 8 | 10 | Epinephrine |
| Schleien CL, et al. [91] | 16 | 8 | Epinephrine |
| Strohmenger HU, et al. [92] | 21 | 7 | Epinephrine |
| Lindberg L, et al. [93] | 6 | 6 | Epinephrine |
| 6 | 6 | Norepinephrine | |
| Wenzel V, et al. [94] | 6 | 7 | Vasopressin |
| 6 | 7 | Epinephrine | |
| Menegazzi JJ, et al. [6] | 8 | 9 | Combination therapy including epinephrine + novel cardiocerebral-protective agent |
| 8 | 9 | Epinephrine | |
| 8 | 9 | Lidocaine + Bretylium | |
| 8 | 9 | Propanolol | |
| 8 | 9 | Novel cardiocerebral-protective agent | |
| 8 | 10 | Epinephrine | |
| Suddath WO, et al. [95] | 10 | 10 | Epinephrine |
| Nozari A, et al. [96] | 11 | 13 | Epinephrine |
| 11 | 13 | Vasopressin | |
| Krismer AC, et al. [97] | 14 | 4 | Epinephrine |
| 14 | 4 | Vasopressin | |
| Idris AH, et al. [98] | 24 | 17 | Epinephrine |
| Barton C, et al. [99] | 4 | 12 | Aortic occlusion + epinephrine |
| 4 | 12 | Epinephrine | |
| Berg RA, et al. [100] | 15 | 16 | High-dose epinephrine |
| 15 | 16 | Standard-dose epinephrine | |
| Killingsworth CR, et al. [101] | 8 | 9 | Β blocker |
| Cairns CB, et al. [102] | 14 | 8 | Epinephrine |
| Rubertsson S, et al. [103] | 8 | 11 | Aortic occlusion + epinephrine |
| 8 | 11 | Epinephrine IV | |
| Wenzel V, et al. [104] | 6 | 7 | Vasopressin IV |
| 6 | 7 | Intraosseous vasopressin | |
| Jasani MS, et al. [105] | 36 | 9 | Epinephrine |
| Rubertsson S, et al. [106] | 22 | 9 | Epinephrine |
| Wenzel V, et al. [107] | 12 | 7 | Epinephrine |
| Wenzel V, et al. [108] | 8 | 18 | Vasopressin |
| Voelckel WG, et al. [109] | 6 | 7 | Vasopressin |
| 6 | 7 | Epinephrine | |
| Hoekstra JW, et al. [110] | 7 | 13 | Norepinephrine |
| 7 | 13 | Epinephrine | |
| Leong EC, et al. [111] | 11 | 11 | Epinephrine |
| 12 | 10 | Epinephrine | |
| Kornberger E, et al. [112] | 6 | 7 | Epinephrine |
| Schwarz B, et al. [113] | 8 | 18 | Vasopressin |
| Krismer AC, et al. [114] | 6 | 9 | Epinephrine |
| 6 | 9 | Epinephrine + novel K+ channel blocker | |
| Nozari A, et al. [115] | 10 | 7 | Aortic occlusion + vasopressin |
| 10 | 7 | Vasopressin | |
| Voelckel WG, et al. [116] | 6 | 16 | Epinephrine |
| 6 | 16 | Vasopressin | |
| 6 | 16 | Vasopressin + epinephrine | |
| Roberts D, et al. [117] | 6 | 3 | Novel α1-agonist |
| 6 | 3 | Standard-dose epinephrine | |
| 6 | 3 | High-dose epinephrine | |
| Prengel AW, et al. [118] | 7 | 7 | Epinephrine |
| 7 | 7 | Vasopressin | |
| Brunette DD, et al. [119] | 10 | 15 | Standard-dose epinephrine |
| 10 | 15 | High-dose epinephrine | |
| Klouche K, et al. [120] | 7 | 9 | Novel α2-agonist |
| 7 | 9 | Epinephrine | |
| Hornchen U, et al. [121] | 8 | 3 | Standard-dose epinephrine |
| 8 | 3 | High-dose epinephrine | |
| Wenzel V, et al. [122] | 6 | 7 | Epinephrine |
| 6 | 7 | Vasopressin | |
| 6 | 12 | Epinephrine | |
| 6 | 12 | Vasopressin | |
| Bar-Joseph G, et al. [123] | 38 | 17 | Epinephrine |
| Hoekstra JW, et al. [124] | 10 | 13 | Epinephrine |
| Angelos MG, et al. [125] | 8 | 10 | Epinephrine |
| Hilwig RW, et al. [126] | 10 | 8 | Endothelin-1 + epinephrine |
| 17 | 8 | Epinephrine | |
| DeBehnke DJ, et al. [127] | 5 | 13 | Endothelin-1 |
| 6 | 13 | Epinephrine | |
| Kornberger E, et al. [128] | 7 | 7 | Epinephrine |
| 7 | 7 | Vasopressin | |
| Mulligan KA, et al. [129] | 11 | 8 | Epinephrine |
| 7 | 8 | Vasopressin | |
| 11 | 8 | Epinephrine + vasopressin | |
| Gedeborg R, et al. [130] | 13 | 10 | Aortic occlusion + epinephrine |
| 13 | 10 | Epinephrine | |
| Babar SI, et al. [131] | 17 | 8 | Epinephrine |
| 18 | 8 | Vasopressin | |
| Hornchen U, et al. [132] | 8 | 3 | Epinephrine |
| 8 | 3 | Endobronchial epinephrine | |
| Lindner KH, et al. [133] | 7 | 7 | Angiotensin II |
| Kern KB, et al. [134] | 16 | 12.5 | Epinephrine |
| 16 | 12.5 | Vasopressin | |
| 16 | 12.5 | Vasopressin | |
| Hornchen, U, et al. [135] | 8 | 3 | Epinephrine IV |
| 8 | 3 | Endobronchial epinephrine | |
| Schindler I, et al. [136] | 26 | 10 | Epinephrine |
| Hornchen U, et al. [137] | 16 | 3 | Epinephrine |
| Hornchen U, et al. [138] | 10 | 3 | Norepinephrine IV |
| 10 | 3 | Endotracheal norepinephrine | |
| Hornchen U, et al. [139] | 26 | 3 | Epinephrine IV |
| 18 | 3 | Endotracheal epinephrine | |
| Liu XL, et al. [140] | 10 | 10 | Aortic occlusion + Vasopressin |
| 10 | 10 | Aortic occlusion + epinephrine | |
| 10 | 10 | Epinephrine | |
| Manning JE, et al. [141] | 12 | 12 | Epinephrine |
Acknowledgments
Drs. Rittenberger and Menegazzi are supported by the Clinical Research Skills Development Core of the Resuscitation Outcomes Consortium through the National Heart, Lung and Blood Institute 5U01 HL077871-02. Dr. Menegazzi is also supported by the National Heart, Lung and Blood institute 5R01 HL080483-2.
Appendix
Time to medication administration (minutes) in clinical studies of cardiac arrest. Subject group given for studies comparing interventions. Grey shading indicates studies specifically evaluating time to study drug administration.
| Study | Number of Subjects | Time to Medication Administration | Subject Group |
|---|---|---|---|
| Nolan J, et al. | 309 | 14.7 | Standard CPR |
| Nolan J, et al. | 267 | 15.8 | Active compression-decompression CPR |
| Eisenburger P, et al. | 114 | 18.0 | |
| Allegra J, et al. | 58 | 13.3 | Magnesium sulfate |
| Allegra J, et al. | 58 | 14.7 | Placebo |
| Mauer D, et al. | 83 | 14.2 | Active compression- decompression CPR |
| Mauer D, et al. | 90 | 13.4 | Standard CPR |
| Mader TJ, et al. | 66 | 12.5 | Aminophylline |
| Mader TJ, et al. | 45 | 12.9 | Control |
| Callaham M, et al. | 286 | 16.0 | High-dose epinephrine |
| Callaham M, et al. | 260 | 17.0 | Standard-dose epinephrine |
| Callaham M, et al. | 270 | 16.0 | Norepinephrine |
| Gueugniaud P, et al. | 153 | 20.7 | Standard-dose epinephrine |
| Gueugniaud P, et al. | 173 | 20.6 | High-dose epinephrine |
| Persse DE, et al. | 24 | 18.8 | Uniform response |
| Persse DE, et al. | 181 | 15.2 | Targeted response |
| Rudner R, et al. | 171 | 10.0 | Resuscitation not successful |
| Rudner R, et al. | 17 | 10.0 | Resuscitation successful |
| Martin DR, et al. | 16 | 16.7 | Countershock group |
| Martin DR, et al. | 31 | 18.5 | No countershock group |
| Schneider T, et al. | 72 | 13.8 | |
| Van der Hoeven JG, et al. | 261 | 11.8 | Before physician supervision |
| Van der Hoeven JG, et al. | 218 | 13.9 | After physician supervision |
| Kudenchuk PJ, et al. | 123 | 21.4 | Amiodarone |
| Kudenchuk PJ, et al. | 179 | 20.5 | Placebo |
| Dorian P, et al. | 162 | 25.0 | Amiodarone |
| Dorian P, et al. | 148 | 24.0 | Lidocaine |
| Wenzel V, et al. | 589 | 17.5 | Vasopressin |
| Wenzel V, et al. | 597 | 18.1 | Epinephrine |
| Brown CG, et al. | 244 | 24.8 | Standard-dose epinephrine |
| Brown CG, et al. | 230 | 24.0 | High-dose epinephrine |
| Bar-Joseph G, et al. | 65 | 18.7 | Escalating Dose Epinephrine BRCT III Site 1 |
| Bar-Joseph G, et al. | 144 | 18.6 | BRCT III Site 2 |
| Bar-Joseph G, et al. | 114 | 20.1 | BRCT III Site 3 |
| Bar-Joseph G, et al. | 136 | 21.6 | BRCT III Site 4 |
| Bar-Joseph G, et al. | 173 | 17.1 | BRCT III Site 5 |
| Bar-Joseph G, et al. | 156 | 20.7 | BRCT III Site 6 |
| Bar-Joseph G, et al. | 96 | 23.2 | BRCT III Site 7 |
| Bar-Joseph G, et al. | 153 | 20.3 | BRCT III Site 8 |
| Bar-Joseph G, et al. | 60 | 19.7 | BRCT III Site 9 |
| Bar-Joseph G, et al. | 290 | 19.4 | BRCT III Site 10 |
| Bar-Joseph G, et al. | 77 | 20.5 | BRCT III Site 11 |
| Bar-Joseph G, et al. | 275 | 14.8 | BRCT III Site 12 |
| Bar-Joseph G, et al. | 37 | 21.2 | BRCT III Site 13 |
| Bar-Joseph G, et al. | 213 | 10.7 | BRCT III Site 14 |
| Bar-Joseph G, et al. | 77 | 24.7 | BRCT III Site 15 |
| Bar-Joseph G, et al. | 56 | 18.3 | BRCT III Site 16 |
Footnotes
Conflict of Interest Statement
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stiell IG, Wells GA, Field B, Spaite DW, Nesbitt LP, De Maio VJ, Nichol G, Cousineau D, Blackburn J, Munkley D, Lunistra-Toohey L, Campeau T, Dagnone Lyver M. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med. 2004;351:647–656. doi: 10.1056/NEJMoa040325. [DOI] [PubMed] [Google Scholar]
- 2.Fatovich DM, Prentice DA, Dobb GJ. Magnesium in cardiac arrest (the magic trial) Resuscitation. 1997;35:237–241. doi: 10.1016/s0300-9572(97)00062-2. [DOI] [PubMed] [Google Scholar]
- 3.Wang HE, Min A, Hostler D, Chang CH, Callaway CW. Differential effects of out-of-hospital interventions on short- and long-term survival after cardiopulmonary arrest. Resuscitation. 2005;67:69–74. doi: 10.1016/j.resuscitation.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 4.Niemann JT, Cairns CB, Sharma J, Lewis RJ. Treatment of prolonged ventricular fibrillation. Immediate countershock versus high-dose epinephrine and CPR preceding countershock. Circulation. 1992;85:281–287. doi: 10.1161/01.cir.85.1.281. [DOI] [PubMed] [Google Scholar]
- 5.Menegazzi JJ, Davis EA, Yealy DM, Molner RL, Nicklas KA, Hosack GM, Honingford EA, Klain MM. An experimental algorithm versus standard advanced cardiac life support in a swine model of out-of-hospital cardiac arrest. Ann Emerg Med. 1993;22:235–239. doi: 10.1016/s0196-0644(05)80211-2. [DOI] [PubMed] [Google Scholar]
- 6.Menegazzi JJ, Seaberg DC, Yealy DM, Davis EA, MacLeod BA. Combination pharmacotherapy with delayed countershock vs. standard advanced cardiac life support after prolonged ventricular fibrillation. Prehosp Emerg Care. 2000;4:31–47. doi: 10.1080/10903120090941614. [DOI] [PubMed] [Google Scholar]
- 7.Prengel AW, Linstedt U, Zenz M, Wenzel V. Effects of combined administration of vasopressin, epinephrine, and norepinephrine during cardiopulmonary resuscitation in pigs. Crit Care Med. 2005;33:2587–2591. doi: 10.1097/01.ccm.0000186774.30674.15. [DOI] [PubMed] [Google Scholar]
- 8.Cammarata G, Weil MH, Sun S, Tang W, Wang J, Huang L. B1-adrenergic blockade during cardiopulmonary resuscitation improves survival. Crit Care Med. 2004;32:S440–S443. doi: 10.1097/01.ccm.0000134263.32657.34. [DOI] [PubMed] [Google Scholar]
- 9.Seaberg DC, Menegazzi JJ, Check B, MacLeod BA, Yealy DM. Use of a cardiocerebral-protective drug cocktail prior to countershock in a porcine model of prolonged ventricular fibrillation. Resuscitation. 2001;51:301–308. doi: 10.1016/s0300-9572(01)00426-9. [DOI] [PubMed] [Google Scholar]
- 10.Prengel AW, Linder KH, Wenzel V, Tugtekin I, Anhaupl T. Splanchnic and renal blood flow after cardiopulmonary resuscitation with epinephrine and vasopressin in pigs. Resuscitation. 1998;38:19–24. doi: 10.1016/s0300-9572(98)00078-1. [DOI] [PubMed] [Google Scholar]
- 11.Wenzel V, Lindner KH, Augenstein S, Prengel A, Strohmenger HU. Vasopressin combined with epinephrine decreases cerebral perfusion compared with vasopressin alone during cardiopulmonary resuscitation in pigs. Stroke. 1998;29:1462–1468. doi: 10.1161/01.str.29.7.1462. [DOI] [PubMed] [Google Scholar]
- 12.Mulligan KA, McKnite SH, Lindner KH, Lindstrom PJ, Detloff B, Lurie KG. Synergistic effects of a vasopressin plus epinephrine during cardiopulmonary resuscitation. Resuscitation. 1997;35:265–271. doi: 10.1016/s0300-9572(97)00060-9. [DOI] [PubMed] [Google Scholar]
- 13.Menegazzi JJ, Wang HE, Lightfoot CB, Fertig KC, Chengelis NL, Sherman LD, Callaway CW. Immediate defibrillation versus interventions first in a swine model of prolonged ventricular fibrillation. Resuscitation. 2003;59:261–270. doi: 10.1016/s0300-9572(03)00212-0. [DOI] [PubMed] [Google Scholar]
- 14.Rittenberger JC, Bost JM, Menegazzi JJ. Time to give the first medication during resuscitation in out-of-hospital cardiac arrest. Resuscitation. 2006;70:201–206. doi: 10.1016/j.resuscitation.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Pititti DB. Meta Analysis, Decision Analysis, and Cost-Effectiveness Analysis. Oxford University Press; 1994. [Google Scholar]
- 16.Hunter JE, Schmidt FL. Methods of meta-analysis: Correcting error and bias in research findings. Newbury Park, CA: Sage; 1990. pp. 110–112. [Google Scholar]
- 17.Weisfeldt ML, Becker LB. Resuscitation after cardiac arrest. JAMA. 2002;288:3035–3038. doi: 10.1001/jama.288.23.3035. [DOI] [PubMed] [Google Scholar]
- 18.Menegazzi JJ, Callaway CW, Sherman LD, Hostler DP, Wang HE, Fertig KC, Logue ES. Ventricular fibrillation scaling exponent can guide timing of defibrillation and other therapies. Circulation. 2004;109:926–931. doi: 10.1161/01.CIR.0000112606.41127.D2. [DOI] [PubMed] [Google Scholar]
- 19.Wang HE, Menegazzi JJ, Lightfoot CB, Callaway CW, Fertig KC, Sherman LD, Hsieh M. Effects of biphasic vs. monophasic defibrillation on the scaling exponent in a swine model of prolonged ventricular fibrillation. Acad Emerg Med. 2001;8:771–780. doi: 10.1111/j.1553-2712.2001.tb00206.x. [DOI] [PubMed] [Google Scholar]
- 20.Beyersdorf F, Kirsch M, Buckberg GG, Allen BS. Warm glutamate/aspartate-enriched blood cardioplegic solution for perioperative sudden death. J Thorac Cardiovasc Surg. 1992;104:1141–1147. [PubMed] [Google Scholar]
- 21.Rittenberger JC, Menegazzi JJ, Callaway CW. Association of delay to first intervention with return of spontaneous circulation in a swine model of cardiac arrest. Resuscitation. 2006 doi: 10.1016/j.resuscitation.2006.07.029. in press. [DOI] [PubMed] [Google Scholar]
- 22.International Liaison Committee on Resuscitation. Part 4: Advanced life support. Resuscitation. 2005;67:213–247. doi: 10.1016/j.resuscitation.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 23.Persse DE, Key CB, Bradley RN, Miller CC, Dhingra A. Cardiac arrest survival as a function of ambulance deployment strategy in a large urban emergency medical services system. Resuscitation. 2003;59:97–104. doi: 10.1016/s0300-9572(03)00178-3. [DOI] [PubMed] [Google Scholar]
- 24.Guyette FX, Rittenberger JC, Platt TE, Suffoletto BS, Hostler DP, Wang HE. Feasibility of basic emergency medical technicians to perform selected advanced life support interventions. Prehosp Emerg Care. 2006:4. doi: 10.1080/10903120600726015. in press. [DOI] [PubMed] [Google Scholar]
- 25.Miller DD, Guimond G, Hostler DP, Platt T, Wang HE. Feasibility of sternal intraosseus access by emergency medical technician students. Prehosp Emerg Care. 2005;9(1):73–78. doi: 10.1080/10903120590891967. [DOI] [PubMed] [Google Scholar]
- 26.Callaham M, Madsen CD, Barton CW, Saunders CE, Pointer J. A randomized clinical trial of high-dose epinephrine and norepinephrine vs. standard-dose epinephrine in prehospital cardiac arrest. JAMA. 1992;268(19):2667–72. [PubMed] [Google Scholar]
- 27.Krieter H, Denz C, Janke C, Bertsch T, Luiz T, Ellinger K, Van Ackern K. Hypertonic-hyperonocotic solutions reduce the release of cardiac troponin I and S-100 after successful cardiopulmonary resuscitation in pigs. Anesthesia & Analgesia. 2002;95:1031–6. doi: 10.1097/00000539-200210000-00044. [DOI] [PubMed] [Google Scholar]
- 28.Loeckinger A, Kleinsasser A, Wenzel V, Mair V, Keller C, Kolbitsch C, Recheis W, Schuster A, Lindner KH. Pulmonary gas exchange after cardiopulmonary resuscitation with either vasopressin or epinephrine. Crit Care Med. 2002;30:2059–62. doi: 10.1097/00003246-200209000-00018. [DOI] [PubMed] [Google Scholar]
- 29.Krismer AC, Wenzel V, Voelckel WG, Stadlbauer KH, Wagner-Berger H, Schaefer A, Lindner KH. Effects of vasopressin on adrenal gland regional perfusion during experimental cardiopulmonary resuscitation. Resuscitation. 2003;56:223–8. doi: 10.1016/s0300-9572(02)00341-6. [DOI] [PubMed] [Google Scholar]
- 30.Little CM, Angelos MG, Paradis NA. Compared to angiotensin II, epinephrine is associated with high myocardial blood flow following return of spontaneous circulation after cardiac arrest. Resuscitation. 2003;59:353–9. doi: 10.1016/s0300-9572(03)00239-9. [DOI] [PubMed] [Google Scholar]
- 31.Johansson J, Gedeborg R, Basu S, Rubertsson S. Increased cortical cerebral blood flow by continuous infusion of adrenaline (epinephrine) during experimental cardiopulmonary resuscitation. Resuscitaiton. 2003;57:299–307. doi: 10.1016/s0300-9572(03)00031-5. [DOI] [PubMed] [Google Scholar]
- 32.Bahlmann L, Klaus S, Baumeier W, Schmucker P, Raedler C, Schmittinger CA, Wenzel V, Voelckel W, Lindner KH. Brain metabolism during cardiopulmonary resuscitation assessed with microdialysis. Resuscitation. 2003;59:255–260. doi: 10.1016/s0300-9572(03)00211-9. [DOI] [PubMed] [Google Scholar]
- 33.Behringer W, Sterz F, Domanovits H, Hohenberger B, Schorkhuber W, Frass M, Losert U, Laggner AN. Effects of manual high-impulse CPR on myocardial perfusion during cardiac arrest in pigs. Resuscitation. 1997;34:271–279. doi: 10.1016/s0300-9572(96)01090-8. [DOI] [PubMed] [Google Scholar]
- 34.Voelckel WG, Lurie KG, McKnite S, Zielinski T, Lindstrom P, Peterson C, Wenzel V, Lindner KH, Benditt D. Effects of epinephrine and vasopressin in a piglet model of prolonged ventricular fibrillation and cardiopulmonary resuscitation. Crit Care Med. 2002;30:957–62. doi: 10.1097/00003246-200205000-00001. [DOI] [PubMed] [Google Scholar]
- 35.Holzer M, Behringer W, Sterz F, Kofler J, Oschatz E, Schuster E, Laggner AN. Ventricular fibrillation median frequency may not be useful for monitoring during cardiac arrest treated with endothelin-1 or epinephrine. Anesthesia & Analgesia. 2004;99:1787–1793. doi: 10.1213/01.ANE.0000138421.74434.E3. [DOI] [PubMed] [Google Scholar]
- 36.Johansson J, Gedeborg R, Rubertsson S. Vasopressin versus continuous adrenaline during experimental cardiopulmonary resuscitation. Resuscitation. 2004;62:61–9. doi: 10.1016/j.resuscitation.2004.01.034. [DOI] [PubMed] [Google Scholar]
- 37.Prengel AW, Linstedt U, Zenz M, Wenzel V. Effects of combined administration of vasopressin, epinephrine, and norepinephrine during cardiopulmonary resuscitation in pigs. Crit Care Med. 2005;33:2587–91. doi: 10.1097/01.ccm.0000186774.30674.15. [DOI] [PubMed] [Google Scholar]
- 38.Amann A, Rheinberger K, Achleitner U, Krismer AC, Lingnau W, Lindner KH, Wenzel V. The prediction of defibrillation outcome using a new combination of mean frequency and amplitude in porcine models of cardiac arrest. Anesthesia & Analgesia. 2002;95:716–22. doi: 10.1097/00000539-200209000-00034. [DOI] [PubMed] [Google Scholar]
- 39.Adams JA, Bassuk J, Wu D, Kurlansky P. Survival and normal neurological outcome after CPR with periodic Gz acceleration and vasopressin. Resuscitation. 2003;56:215–21. doi: 10.1016/s0300-9572(02)00319-2. [DOI] [PubMed] [Google Scholar]
- 40.Schwarz B, Mair P, Wagner-Berger H, Stadlbauer KH, Girg S, Wenzel V, Lindner KH. Neither vasopressin nor amiodarone improve CPR outcome in an animal model of hypothermic cardiac arrest. Acta Anaesth Scan. 2003;47:1114–8. doi: 10.1034/j.1399-6576.2003.00214.x. [DOI] [PubMed] [Google Scholar]
- 41.Vukmir RB, Bircher NG, Radovsky A, Safar P. Sodium bicarbonate may improve outcome in dogs with brief or prolonged cardiac arrest. Crit Care Med. 1995;23:515–22. doi: 10.1097/00003246-199503000-00017. [DOI] [PubMed] [Google Scholar]
- 42.Manning JE, Batson DN, Payne FB, Adam N, Murphy CA, Peretta SG, Norfleet EA. Selective aortic arch perfusion during cardiac arrest: enhanced resuscitation using oxygenated perflubron emulsion, with and without aortic arch epinephrine. Ann Emerg Med. 1997;29:580–7. doi: 10.1016/s0196-0644(97)70244-0. [DOI] [PubMed] [Google Scholar]
- 43.Strohmenger HU, Lindner KH, Prengel AW, Pfenninger EG, Bothner U, Lurie KG. Effects of epinephrine and vasopressin on median fibrillation frequency and defibrillation success in a porcine model of cardiopulmonary resuscitation. Resuscitation. 1996;31:65–73. doi: 10.1016/0300-9572(95)00899-3. [DOI] [PubMed] [Google Scholar]
- 44.Ayoub IM, Kolarova J, Kantola RL, Sanders R, Gazmuri RJ. Cariporide minimizes adverse myocardial effects of epinephrine during resuscitation from ventricular fibrillation. Crit Care Med. 2005;33:2599–605. doi: 10.1097/01.ccm.0000186773.88576.83. [DOI] [PubMed] [Google Scholar]
- 45.Stadlbauer KH, Wagner-Berger HG, Wenzel V, Voelckel WG, Krismer AC, Klima G, Rheinberger K, Pechlander S, Mayr VD, Lindner KH. Survival with full neurologic recover after prolonged cardiopulmonary resuscitation with a combination of vasopressin and epinephrine in pigs. Anesthesia & Analgesia. 2003;96:1743–9. doi: 10.1213/01.ANE.0000066017.66951.7F. [DOI] [PubMed] [Google Scholar]
- 46.Mayr VD, Wenzel V, Voelckel WG, Krismer AC, Mueller T, Lurie KG, Lindner KH. Developing a vasopressor combination in a pig model of asphyxial cardiac arrest. Circulation. 2001;104:1651–6. doi: 10.1161/hc3901.095896. [DOI] [PubMed] [Google Scholar]
- 47.Amann A, Achleitner U, Antretter H, Bonatti JO, Krismer AC, Lindner KH, Reider J, Wenzel V, Voelckel WG, Strohmenger HU. Analyzing ventricular fibrillation ECG-signals and predicting defibrillation success during cardiopulmonary resuscitation employing N(alpha)-histograms. Resuscitation. 2001;50:77–85. doi: 10.1016/s0300-9572(01)00322-7. [DOI] [PubMed] [Google Scholar]
- 48.Hilwig RW, Kern KB, Berg RA, Sanders AB, Otto CW, Ewy GA. Catecholamines in cardiac arrest: role of alpha agonists, beta-adrenergic blockers and high-dose epinephrine. Resuscitation. 2000;47:203–8. doi: 10.1016/s0300-9572(00)00261-6. [DOI] [PubMed] [Google Scholar]
- 49.Nozari A, Rubertsson S, Wiklund L. Intra-aortic administration of epinephrine above an aortic balloon occlusion during experimental CPR does not further improve cerebral blood flow and oxygenation. Resuscitation. 2000;44:119–27. doi: 10.1016/s0300-9572(00)00132-5. [DOI] [PubMed] [Google Scholar]
- 50.Prengel AW, Lindner KH, Wenzel V, Tugtekin I, Anhaupl T. Splanchnic and renal blood flow after cardiopulmonary resuscitation with epinephrine and vasopressin in pigs. Resuscitation. 1998;38:19–24. doi: 10.1016/s0300-9572(98)00078-1. [DOI] [PubMed] [Google Scholar]
- 51.Wenzel V, Linder KH, Augenstein S, Prengel AW, Strohmenger HU. Vasopressin combined with epinephrine decreases cerebral perfusion compared with vasopressin alone during cardiopulmonary resuscitation in pigs. Stroke. 1998;29:1462–7. doi: 10.1161/01.str.29.7.1462. [DOI] [PubMed] [Google Scholar]
- 52.Wenzel V, Lindner KH, Mayer H, Lurie KG, Prengel AW. Vasopressin combined with nitroglycerin increases endocardial perfusion during cardiopulmonary resuscitation in pigs. Resuscitation. 1998;38:13–7. doi: 10.1016/s0300-9572(98)00063-x. [DOI] [PubMed] [Google Scholar]
- 53.Lurie KG, Voelckel WG, Iskos DN, McKnite SH, Zielinski TM, Sugiyama A, Wenzel V, Benditt D, Lindner KH. Combination drug therapy with vasopressin, adrenaline (epinephrine) and nitroglycerin improves vital organ blood flow in a porcine model of ventricular fibrillation. Resuscitation. 2002;54:187–94. doi: 10.1016/s0300-9572(02)00096-5. [DOI] [PubMed] [Google Scholar]
- 54.Berg RA, Hilwig RW, Kern KB, Ewy GA. Precountershock cardiopulmonary resuscitation improves ventricular fibrillation median frequency and myocardial readiness for successful defibrillation from prolonged ventricular fibrillation: a randomized, controlled swine study. Ann Emerg Med. 2002;40:563–70. doi: 10.1067/mem.2002.129866. [DOI] [PubMed] [Google Scholar]
- 55.Holzer M, Sterz F, Behringer W, Oschatz E, Kofler J, Eisenburger P, Kittler H, Konschitzky R, Laggner AN. Endothelin-1 elevates regional cerebral perfusion during prolonged ventricular fibrillation cardiac arrest in pigs. Resuscitation. 200;55:317–27. doi: 10.1016/s0300-9572(02)00211-3. [DOI] [PubMed] [Google Scholar]
- 56.Prengel AW, Lindner KH, Anhaupl T, Vogt J, Lurie KG. Regulation of right atrial beta-adrenoreceptors after cardiopulmonary resuscitation in pigs. Resuscitation. 1996;31:271–8. doi: 10.1016/0300-9572(95)00930-2. [DOI] [PubMed] [Google Scholar]
- 57.Bleske BE, Warren EW, Rice TL, Shea MJ, Amidon G, Knight P. Comparison of intravenous and intranasal administration of epinephrine during CPR in a canine model. Ann Emerg Med. 1992;21:1125–30. doi: 10.1016/s0196-0644(05)80657-2. [DOI] [PubMed] [Google Scholar]
- 58.Tang W, Weil MH, Schock RB, Sato Y, Lucas J, Sun S, Bisera J. Phased chest and abdominal compression-decompression. A new option for cardiopulmonary resuscitation. Circulation. 1997;95:1335–40. doi: 10.1161/01.cir.95.5.1335. [DOI] [PubMed] [Google Scholar]
- 59.Lindner KH, Pfenninger EG, Lurie KG, Schurmann W, Lindner IM, Ahnfeld FW. Effects of active compression-decompression resuscitation on myocardial and cerebral blood flow in pigs. Circulation. 1993;88:1254–63. doi: 10.1161/01.cir.88.3.1254. [DOI] [PubMed] [Google Scholar]
- 60.Lindner KH, Prengel AW, Pfenninger EG, Lindner IM, Strohmenger HU, Georgieff M, Lurie KG. Vasopressin improves vital organ blood flow during closed-chest cardiopulmonary resuscitation in pigs. Circulation. 1995;91:215–21. doi: 10.1161/01.cir.91.1.215. [DOI] [PubMed] [Google Scholar]
- 61.Idris AH, Becker LB, Fuerst RS, Wenzel V, Rush WJ, Melker RJ, Orban DJ. Effect of ventilation on resuscitation in an animal model of cardiac arrest. Circulation. 1994;90:3063–9. doi: 10.1161/01.cir.90.6.3063. [DOI] [PubMed] [Google Scholar]
- 62.Bar-Joseph G, Weinberger T, Ben-Haim S. Response to repeated equal doses of epinephrine during cardiopulmonary resuscitation in dogs. Ann Emerg Med. 2000;35:3–10. doi: 10.1016/s0196-0644(00)70098-9. [DOI] [PubMed] [Google Scholar]
- 63.Paradis NA. Is a pressor necessary during aortic perfusion and oxygenation therapy of cardiac arrest? Ann Emerg Med. 1999;34:697–702. doi: 10.1016/s0196-0644(99)70093-4. [DOI] [PubMed] [Google Scholar]
- 64.Bleske BE, Rice TL, Warren EW, Giacherio DA, Gilligan LJ, Massey KD, Tait AR. Effect of dose on the nasal absorption of epinephrine during cardiopulmonary resuscitation. Am J Emerg Med. 1996;14:133–8. doi: 10.1016/S0735-6757(96)90119-9. [DOI] [PubMed] [Google Scholar]
- 65.Lindner KH, Ahnefeld FW, Bowdler IM. Comparison of different doses of epinephrine on myocardial perfusion and resuscitation success during cardiopulmonary resuscitation in a pig model. Am J Emerg Med. 1991;9:27–31. doi: 10.1016/0735-6757(91)90008-8. [DOI] [PubMed] [Google Scholar]
- 66.Wolf CF, Keck FS, Brinkmann A, Rigos D, Lindner KH, Grunert A. Unchanged 5′-deiodinating activity during the induction of a nonthyroidal illness. Hormone and Metabolic Research. 1995;27:126–30. doi: 10.1055/s-2007-979923. [DOI] [PubMed] [Google Scholar]
- 67.Blecic S, Chaskis C, Vincent JL. Atropine administration in experimental electromechanical dissociation. Am J Emerg Med. 1992;10:515–8. doi: 10.1016/0735-6757(92)90174-v. [DOI] [PubMed] [Google Scholar]
- 68.Prengel AW, Lindner KH, Keller A, Lurie KG. Cardiovascilar function during the postressucitaiton phase after cardiac arrest in pigs: a comparison of epinephrine versus vasopressin. Crit Care Med. 1996;24:2014–9. doi: 10.1097/00003246-199612000-00014. [DOI] [PubMed] [Google Scholar]
- 69.Berg RA, Otto CW, Kern KB, Hilwig RW, Sanders AB, Henry CP, Ewy GA. A randomized blinded trial of high-dose epinephrine versus standard-dose epinephrine in a swine model of pediatric asphyxial cardiac arrest. Crit Care Med. 1996;24:1695–700. doi: 10.1097/00003246-199610000-00016. [DOI] [PubMed] [Google Scholar]
- 70.Strohmenger HU, Lindner KH, Keller A, Lindner IM, Pfenninger E, Bothner U. Effects of graded doses of vasopressin on median fibrillation frequency in a porcine model of cardiopulmonary resuscitation: results of a prospective, randomized, controlled trial. Crit Care Med. 1996;24:1360–5. doi: 10.1097/00003246-199608000-00015. [DOI] [PubMed] [Google Scholar]
- 71.Bleske BE, Rice TL, Warren EW, De Las Alvas VR, Tait AR, Knight PR. The effect of sodium bicarbonate administration on the vasopressor effect of high-dose epinephrine during cardiopulmonary resuscitation in swine. Am J Emerg Med. 1993;11:439–43. doi: 10.1016/0735-6757(93)90078-p. [DOI] [PubMed] [Google Scholar]
- 72.Manning JE, Murphy CA, Batson DN, Perretta SG, Mueller RA, Norfleet EA. Aortic arch versus central venous epinephrine during CPR. Ann Emerg Med. 1993;22:703–8. doi: 10.1016/s0196-0644(05)81852-9. [DOI] [PubMed] [Google Scholar]
- 73.Wenzel V, Lindner KH, Prengel AW, Maier C, Voelckel W, Lurie KG, Strohmenger HU. Vasopressin improves vital organ blood flow after prolonged cardiac arrest with postcountershock pulseless electrical activity in pigs. Crit Care Med. 1999;27:486–92. doi: 10.1097/00003246-199903000-00022. [DOI] [PubMed] [Google Scholar]
- 74.Mayr VD, Raedler C, Wenzel V, Lindner KH, Strohmenger HU. A comparison of epinephrine and vasopressin in a porcine model of cardiac arrest after rapid intravenous injection of bupivicaine. Anesthesia and Analgesia. 2004;98:1426–31. doi: 10.1213/01.ane.0000108488.05900.a8. [DOI] [PubMed] [Google Scholar]
- 75.Gervais HW, Schleien CL, Koehler RC, Berkowitz ID, Shaffner DH, Traystman RJ. Effect of adrenergic drugs on cerebral blood flow, metabolism, and evoked potentials after delayed cardiopulmonary resuscitation in dogs. Stroke. 1991;22:1554–61. doi: 10.1161/01.str.22.12.1554. [DOI] [PubMed] [Google Scholar]
- 76.Nejman GD, Griffith R, Van Ligten P, Hoekstra J, Casto L, Miller DD, Brown CG. Hemodynamic effects of 1-[3,4-dihydroxyphenyl]-1,2-diaminoethane versus norepinephrine during ventricular fibrillation and cardiopulmonary resuscitation. Resuscitation. 1990;20:243–52. doi: 10.1016/0300-9572(90)90007-2. [DOI] [PubMed] [Google Scholar]
- 77.Achleitner U, Wenzel V, Strohmenger HU, Krismer AC, Lurie KG, Lindner KH, Amann A. The effects of repeated doses of vasopressin or norepinephrine on ventricular fibrillation in a porcine model of prolonged cardiopulmonary resuscitation. Anesthesia & Analgesia. 200;90:1067–75. doi: 10.1097/00000539-200005000-00012. [DOI] [PubMed] [Google Scholar]
- 78.Niemann JT, Cairns CB, Sharma J, Lewis RJ. Treatment of prolonged ventricular fibrillation. Immediate countershock versus high-dose epinephrine and CPR preceding countershock. Circulation. 1992;85:281–7. doi: 10.1161/01.cir.85.1.281. [DOI] [PubMed] [Google Scholar]
- 79.Voelckel WG, Lindner KH, Wenzel V, Bonatti JO, Krismer AC, Miller EA, Lurie KG. Effect of small-dose dopamine on mesenteric blood flow and renal function in a pig model of cardiopulmonary resuscitation with vasopressin. Anesthesia and Analgesia. 1999;80:1430–6. doi: 10.1097/00000539-199912000-00020. [DOI] [PubMed] [Google Scholar]
- 80.Lindner KH, Brinkmann A, Pfenninger EG, Lurie KG, Goertz A, Lindner IM. Effect of vasopressin in hemodynamic variables, organ blood flow, and acid-base status in a pig model of cardiopulmonary resuscitation. Anesthesia & Analgesia. 1993;77:427–35. doi: 10.1213/00000539-199309000-00003. [DOI] [PubMed] [Google Scholar]
- 81.Gazmuri RJ, von Planta M, Weil MH, Rackow EC. Cardiac effects of carbon dioxide-consuming and carbon dioxide-generating buffers during cardiopulmonary resuscitation. J Am Col Card. 1990;15:482–90. doi: 10.1016/s0735-1097(10)80080-4. [DOI] [PubMed] [Google Scholar]
- 82.Bleske BE, Rice TL, Warren EW, Giacherio DA, Gilligan LJ, Massey KD, Chrisp CE, Tait AR. Effect of vehicle on the nasal absorption of epinephrine during cardiopulmonary resuscitation. Pharmacotherapy. 1996;16:1039–45. [PubMed] [Google Scholar]
- 83.Jameson SJ, Mateer JR, DeBehnke DJ. Early volume expansion during cardiopulmonary resuscitation. Resuscitation. 1993;26:243–50. doi: 10.1016/0300-9572(93)90145-g. [DOI] [PubMed] [Google Scholar]
- 84.Wenzel V, Lindner KH, Prengel AW, Lurie KG, Strohmenger HU. Endobronchial vasopressine improves survival during cardiopulmonary resuscitation in pigs. Anesthesiology. 1997;86:1375–81. doi: 10.1097/00000542-199706000-00020. [DOI] [PubMed] [Google Scholar]
- 85.Lindner KH, Ahnefeld FW, Schuermann W, Bowdler IM. Epinephrine and norepinephrine in cardiopulmonary resuscitation. Effects on myocardial oxygen delivery and consumption. Chest. 1990;97:1458–62. doi: 10.1378/chest.97.6.1458. [DOI] [PubMed] [Google Scholar]
- 86.Angelos MG, DeBehnke DJ, Leasure JE. Arterial blood gases during cardiac arrest: markers of blood flow in a canine model. Resuscitation. 1992;23:101–11. doi: 10.1016/0300-9572(92)90195-i. [DOI] [PubMed] [Google Scholar]
- 87.Prengel AW, Lindner KH, Keller A. Cerebral oxygenation during cardiopulmonary resuscitation with epinephrine and vasopressin in pigs. Stroke. 1996;27:1241–8. doi: 10.1161/01.str.27.7.1241. [DOI] [PubMed] [Google Scholar]
- 88.Littmann L, Ashline PT, Hayes WJ, Kempler P, Raymond RM, Norton HJ, Svenson RH, Tuntelder JR, Tatsis GP. Aminophylline fails to improve the outcome of cardiopulmonary resuscitation from prolonged ventricular fibrillation: a placebo-controlled, randomized, blinded experimental study. J Am Coll Cardiol. 1994;23:1708–14. doi: 10.1016/0735-1097(94)90679-3. [DOI] [PubMed] [Google Scholar]
- 89.DeBehnke DJ, Angelos MG, Leasure JE. Use of cardiopulmonary bypass, high-dose epinephrine, and standard-dose epinephrine in resuscitation from post-countershock electromechanical dissociation. Ann Emerg Med. 1992;21:1051–7. doi: 10.1016/s0196-0644(05)80644-4. [DOI] [PubMed] [Google Scholar]
- 90.Manning JE, Murphy CA, Hertz CM, Perretta SG, Mueller RA, Norfleet EA. Selective aortic arch perfusion during cardiac arrest: a new resuscitation technique. Ann Emerg Med. 1992;21:1058–65. doi: 10.1016/s0196-0644(05)80645-6. [DOI] [PubMed] [Google Scholar]
- 91.Schleien CL, Eberle B, Shaffner DH, Koehler RC, Traystman RJ. Reduced blood-brain barrier permeability after cardiac arrest by conjugated superoxide dismutase and catalase in piglets. Stroke. 1994;25:1830–4. doi: 10.1161/01.str.25.9.1830. [DOI] [PubMed] [Google Scholar]
- 92.Strohmenger HU, Wenzel V, Eberhard R, Guth BD, Lurie KG, Lindner KH. Effects of the specific bradycardic agent zatebradine on hemodynamic variables and myocardial blood flow during the early postresuscitation phase in pigs. Resuscitation. 1999;42:211–20. doi: 10.1016/s0300-9572(99)00093-3. [DOI] [PubMed] [Google Scholar]
- 93.Lindberg L, Liao Q, Steen S. The effects of epinephrine/norepinephrine on end-tidal carbon dioxide concentration, coronary perfusion pressure and pulmonary arterial blood flow during cardiopulmonary resuscitation. Resuscitation. 2000;43:129–40. doi: 10.1016/s0300-9572(99)00129-x. [DOI] [PubMed] [Google Scholar]
- 94.Wenzel V, Lindner KH, Krismer AC, Voelckel WG, Schocke MF, Hund W, Witkiewicz M, Miller EA, Klima G, Wissel J, Lingnau W, Aichner FT. Survival with full neurologic recovery and no cerebral pathology after prolonged cardiopulmonary resuscitation with vasopressin in pigs. J Am Col Cardiol. 2000;35:527–33. doi: 10.1016/s0735-1097(99)00562-8. [DOI] [PubMed] [Google Scholar]
- 95.Suddath WO, Deychak Y, Varghese PJ. Electrophysiologic basis by which epinephrine facilitates defibrillation after prolonged episodes of ventricular fibrillation. Ann Emerg Med. 2001;38:201–6. doi: 10.1067/mem.2001.115540. [DOI] [PubMed] [Google Scholar]
- 96.Nozari A, Rubertsson S, Wiklund L. Differences in the pharmacodynamics of epinephrine during and after experimental cardiopulmonary resuscitation. Resuscitation. 2001;49:59–72. doi: 10.1016/s0300-9572(00)00267-7. [DOI] [PubMed] [Google Scholar]
- 97.Krismer AC, Hogan QH, Wenzel V, Lindner KH, Achleitner U, Oroszy S, Rainer B, Wihaidi A, Mayr VD, Spencker P, Amann A. The efficacy of epinephrine or vasopressin for resuscitation during epidural anesthesia. Anesthesia & Analgesia. 2001;93:734–42. doi: 10.1097/00000539-200109000-00038. [DOI] [PubMed] [Google Scholar]
- 98.Idris AH, Wenzel V, Becker LB, Bannner MJ, Orban DJ. Does hypoxia or hypercarbia independently affect resuscitation from cardiac arrest? Chest. 1995;108:522–8. doi: 10.1378/chest.108.2.522. [DOI] [PubMed] [Google Scholar]
- 99.Barton C, Manning JE, Batson N. Effect of selective aortic arch perfusion on median frequency and peak amplitude of ventricular fibrillation in a canine model. Ann Emerg Med. 1996;27:610–6. doi: 10.1016/s0196-0644(96)70165-8. [DOI] [PubMed] [Google Scholar]
- 100.Berg RA, Otto CW, Kern KB, Sanders AB, Hilwig RW, Hansen KK, Ewy GA. High-dose epinephrine results in greater early mortality after resuscitation from prolonged cardiac arrest in pigs: a prospective, randomized study. Crit Care Med. 1994;22:282–90. doi: 10.1097/00003246-199402000-00020. [DOI] [PubMed] [Google Scholar]
- 101.Killingsworth CR, Wei CC, Dell’Italia LJ, Ardell JL, Kingsley MA, Smith WM, Ideker RE, Walcott GP. Short-acting beta-adrenergic antagonist esmolol given at reperfusion improves survival after prolonged ventricular fibrillation. Circulation. 2004;109:2469–74. doi: 10.1161/01.CIR.0000128040.43933.D3. [DOI] [PubMed] [Google Scholar]
- 102.Cairns CB, Niemann JT. Hemodynamic effects of repeated doses of epinephrine after prolonged cardiac arrest and CPR: preliminary observations in an animal model. Resuscitation. 1998;36:181–5. doi: 10.1016/s0300-9572(98)00018-5. [DOI] [PubMed] [Google Scholar]
- 103.Rubertsson S, Bircher NG, Smarik SD, Young MC, Alexander H, Grenvik A. Intra-aortic administration of epinephrine above aortic occlusion does not alter outcome of experimental cardiopulmonary resuscitation. Resuscitation. 1999;42:57–63. doi: 10.1016/s0300-9572(99)00075-1. [DOI] [PubMed] [Google Scholar]
- 104.Wenzel V, Lindner KH, Augenstein S, Voelckel W, Strohmenger HU, Prengel AW, Steinbach G. Intraosseous vasopressin improves coronary perfusion pressure rapidly during cardiopulmonary resuscitation in pigs. Crit Care Med. 1999;27:1565–9. doi: 10.1097/00003246-199908000-00027. [DOI] [PubMed] [Google Scholar]
- 105.Jasani MS, Nadkarni VM, Finkelstein MS, Mandell GA, Salzman SK, Norman ME. Effects of different techniques of endotracheal epinephrine administration in pediatric porcine hypoxic-hypercarbic cardiopulmonary arrest. Crit Care Med. 1994;22:1174–80. doi: 10.1097/00003246-199407000-00021. [DOI] [PubMed] [Google Scholar]
- 106.Rubertsson S, Grenvik A, Zemgulis V, Wiklund L. Systemic perfusion pressure and blood flow before and after administration of epinephrine during experimental cardiopulmonary resuscitation. Crit Care Med. 1995;23:1984–96. doi: 10.1097/00003246-199512000-00007. [DOI] [PubMed] [Google Scholar]
- 107.Wenzel V, Lindner KH, Prengel AW, Strohmenger HU. Effect of phased chest and abdominal compression-decompression cardiopulmonary resuscitation on myocardial and cerebral blood flow in pigs. Crit Care Med. 2000;28:1107–12. doi: 10.1097/00003246-200004000-00033. [DOI] [PubMed] [Google Scholar]
- 108.Wenzel V, Lindner KH, Baubin MA, Voelckel WG. Vasopressin decreases endogenous catecholamine plasma concentrations during cardiopulmonary resuscitation in pigs. Crit Care Med. 2000;28:1096–100. doi: 10.1097/00003246-200004000-00031. [DOI] [PubMed] [Google Scholar]
- 109.Voelckel WG, Lindner KH, Wenzel V, Bonatti J, Hangler H, Frimmel C, Kunszberg E, Lingnau W. Effects of vasopressin and epinephrine on splanchnic blood flow and renal function during and after cardiopulmonary resuscitation in pigs. Crit Care Med. 2000;28:1083–8. doi: 10.1097/00003246-200004000-00029. [DOI] [PubMed] [Google Scholar]
- 110.Hoekstra JW, Van Ligten P, Neumar R, Werman HA, Anderson J, Brown CG. Effect of high dose norepinephrine versus epinephrine on cerebral and myocardial blood flow during CPR. Resuscitation. 1990;19:227–40. doi: 10.1016/0300-9572(90)90104-m. [DOI] [PubMed] [Google Scholar]
- 111.Leong EC, Bendall JC, Boyd AC, Einstein R. Sodium bicarbonate improves the chance of resuscitation after 10 minutes of cardiac arrest in dogs. Resuscitation. 2001;51:309–15. doi: 10.1016/s0300-9572(01)00421-x. [DOI] [PubMed] [Google Scholar]
- 112.Kornberger E, Lindner KH, Mayr VD, Schwarz B, Rackwitz KS, Wenzel V, Krismer AC, Mair P. Effects of epinephrine in a pig model of hypothermic cardiac arrest and closed-chest cardiopulmonary resuscitation combined with active rewarming. Resuscitation. 2001;50:301–8. doi: 10.1016/s0300-9572(01)00353-7. [DOI] [PubMed] [Google Scholar]
- 113.Schwarz B, Mair P, Raedler C, Deckert D, Wenzel V, Lindner KH. Vasopressin improves survival in a pig model of hypothermic cardiopulmonary resuscitation. Crit Care Med. 2002;30:1311–4. doi: 10.1097/00003246-200206000-00027. [DOI] [PubMed] [Google Scholar]
- 114.Krismer AC, Wenzel V, Voelckel W, Witkiewicz M, Strohmenger HU, Raedler C, Lindner KH. Effect of the cardioselective ATP-sensitive potassium channel inhibitor HMR 1883 in a porcine model of cardiopulmonary resuscitation. Resuscitation. 2002;53:299–306. doi: 10.1016/s0300-9572(02)00038-2. [DOI] [PubMed] [Google Scholar]
- 115.Nozari A, Rubertsson S, Wiklund L. Improved cerebral blood supply and oxygenation by aortic balloon occlusion combined with intra-aortic vasopressin administration during experimental cardiopulmonary resuscitation. Acta Anaesthesiologica Scandinavica. 2000;44:1209–19. doi: 10.1034/j.1399-6576.2000.441005.x. [DOI] [PubMed] [Google Scholar]
- 116.Voelckel WG, Lurie KG, McKnite S, Zielinski T, Lindstrom P, Peterson C, Krismer AC, Lindner KH, Wenzel V. Comparison of epinephrine and vasopressin in a pediatric porcine model of asphyxial cardiac arrest. Crit Care Med. 2000;28:3777–83. doi: 10.1097/00003246-200012000-00001. [DOI] [PubMed] [Google Scholar]
- 117.Roberts D, Landolfo K, Dobson K, Light RB. The effects of methoxamine and epinephrine on survival and regional distribution of cardiac output in dogs with prolonged ventricular fibrillation. Chest. 1990;98:999–1005. doi: 10.1378/chest.98.4.999. [DOI] [PubMed] [Google Scholar]
- 118.Prengel AW, Lindner KH, Keller A. Cerebral oxygenation during cardiopulmonary resuscitation with epinephrine and vasopressin in pigs. Stroke. 1996;27:1241–8. doi: 10.1161/01.str.27.7.1241. [DOI] [PubMed] [Google Scholar]
- 119.Brunette DD, Jameson SJ. Comparison of standard versus high-dose epinephrine in the resuscitation of cardiac arrest in dogs. Ann Emerg Med. 1990;19:8–11. doi: 10.1016/s0196-0644(05)82130-4. [DOI] [PubMed] [Google Scholar]
- 120.Klouche K, Weil MH, Tang W, Povoas H, Kamohara T, Bisera J. A selective alpha(2)-adrenergic agonist for cardiac resuscitation. J Laboratory & Clinical Medicine. 2002;140:27–34. doi: 10.1067/mlc.2002.125177. [DOI] [PubMed] [Google Scholar]
- 121.Hornchen U, Lussi C, Schuttler J. Potential risks of high-dose epinephrine for resuscitation from ventricular fibrillation in a porcine model. J Cardiothoracic & Vascular Anesthesia. 1993;7:184–7. doi: 10.1016/1053-0770(93)90214-6. [DOI] [PubMed] [Google Scholar]
- 122.Wenzel V, Lindner KH, Krismer AC, Miller EA, Voelckel WG, Lingnau W. Repeated administration of vasopressin but not epinephrine maintains coronary perfusion pressure after early and late administration during prolonged cardiopulmonary resuscitation in pigs. Circulation. 1999;99:1379–84. doi: 10.1161/01.cir.99.10.1379. [DOI] [PubMed] [Google Scholar]
- 123.Bar-Joseph G, Weinberger T, Castel T, Bar-Joseph N, Laor A, Bursztein S, Ben Haim S. Comparison of sodium bicarbonate, Carbicarb, and THAM during cardiopulmonary resuscitation in dogs. Crit Care Med. 1998;26:1397–408. doi: 10.1097/00003246-199808000-00027. [DOI] [PubMed] [Google Scholar]
- 124.Hoekstra JW, Rinnert K, Van Ligten P, Neumar R, Werman HA, Brown CG. The effectiveness of bystander CPR in an animal model. Ann Emerg Med. 1990;19:881–6. doi: 10.1016/s0196-0644(05)81561-6. [DOI] [PubMed] [Google Scholar]
- 125.Angelos MG, Gaddis ML, Gaddis GM, Leasure JE. Improved survival and reduced myocardial necrosis with cardiopulmonary bypass reperfusion in a canine model of coronary occlusion and cardiac arrest. Ann Emerg Med. 1990;19:1122–8. doi: 10.1016/s0196-0644(05)81515-x. [DOI] [PubMed] [Google Scholar]
- 126.Hilwig RW, Berg RA, Kern KB, Ewy GA. Endothelin-1 vasoconstriction during swine cardiopulmonary resuscitation improves coronary perfusion pressures but worsens postresuscitation outcome. Circulation. 2000;101:2097–102. doi: 10.1161/01.cir.101.17.2097. [DOI] [PubMed] [Google Scholar]
- 127.DeBehnke DJ, Benson L. Effects of endothelin-1 on resuscitation rate during cardiac arrest. Resuscitation. 2000;47:185–9. doi: 10.1016/s0300-9572(00)00218-5. [DOI] [PubMed] [Google Scholar]
- 128.Kornberger E, Prengel AW, Krismer A, Schwarz B, Wenzel V, Lindner KH, Mair P. Vasopressin-mediated adrenocorticotropin release increases plasma cortisol concentrations during cardiopulmonary resuscitation. Crit Care Med. 2000;28:3517–21. doi: 10.1097/00003246-200010000-00028. [DOI] [PubMed] [Google Scholar]
- 129.Mulligan KA, McKnite SH, Lindner KH, Lindstrom PJ, Detloff B, Lurie KG. Synergistic effects of vasopressin plus epinephrine during cardiopulmonary resuscitation. Resuscitation. 1997;35:265–71. doi: 10.1016/s0300-9572(97)00060-9. [DOI] [PubMed] [Google Scholar]
- 130.Gedeborg R, Rubertsson S, Wiklund L. Improved haemodynamics and restoration of spontaneous circulation with constant aortic occlusion during experimental cardiopulmonary resuscitation. Resuscitation. 1999;40:171–80. doi: 10.1016/s0300-9572(99)00021-0. [DOI] [PubMed] [Google Scholar]
- 131.Babar SI, Berg RA, Hilwig RW, Kern KB, Ewy GA. Vasopressin versus epinephrine during cardiopulmonary resuscitation: a randomized swine outcome study. Resuscitation. 1999;41:185–92. doi: 10.1016/s0300-9572(99)00071-4. [DOI] [PubMed] [Google Scholar]
- 132.Hornchen U, Lauven PM, Schuttler J, Dorer A, Stoeckel H. The pharmacokinetics of lidocaine in resuscitation conditions. Results of experimental studies on swine. Anaesthesist. 1990;39:107–12. [PubMed] [Google Scholar]
- 133.Lindner KH, Prengel AW, Pfenninger EG, Lindner IM. Angiotensin II augments reflex activity of the sympathetic nervous system during cardiopulmonary resuscitation in pigs. Circulation. 1995;92:1020–5. doi: 10.1161/01.cir.92.4.1020. [DOI] [PubMed] [Google Scholar]
- 134.Kern KB, Heidenreich JH, Higdon TA, Berg RA, Hilwig RW, Sanders AB, Anavy N, Ewy GA. Effect of vasopressin on postresuscitation ventricular function: unknown consequences of the recent Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Crit Care Med. 2004;32:S393–7. doi: 10.1097/01.ccm.0000139459.39372.71. [DOI] [PubMed] [Google Scholar]
- 135.Hornchen U, Schuttler J, Stoeckel H. Influence of the pulmonary circulation on adrenaline pharmacokinetics during cardiopulmonary resuscitation. Eur J Anesth. 1992;9:85–91. [PubMed] [Google Scholar]
- 136.Schindler I, Steltzer H, Weindlmayr-Goettel M, Steinbereithner K. Nimodipine after circulatory arrest: effects on oxygen delivery and consumption. J Crit Care. 1994;9:18–24. doi: 10.1016/0883-9441(94)90029-9. [DOI] [PubMed] [Google Scholar]
- 137.Hornchen U, Berg PW, Schuttler J. Potential risks of high-dose adrenaline for resuscitation following short-term heart arrest in animal experiments. Anasthesiologie, Intensivmedizin, Notfallmedizin, Schmerztherapie. 1992;27:274–8. doi: 10.1055/s-2007-1000296. [DOI] [PubMed] [Google Scholar]
- 138.Hornchen U, Lussi C, Thomas M, Schuttler J. The pulmonary first pass effect of noradrenaline following intravenous and endobronchial administration for resuscitation. Anasthesiologie, Intensivmedizin, Notfallmedizin, Schmerztherapie. 1992;7:160–5. doi: 10.1055/s-2007-1000272. [DOI] [PubMed] [Google Scholar]
- 139.Hornchen U, Lussi C, Schuttler J. New standards for catecholamine therapy in cardiopulmonary resuscitation? Results of a modified application in a resuscitation model. Anasthesiologie, Intensivmedizin, Notfallmedizin, Schmerztherapie. 1992;7:225–9. doi: 10.1055/s-2007-1000285. [DOI] [PubMed] [Google Scholar]
- 140.Liu XL, Nozari A, Basu S, Ronquist G, Ruertsson S, Wiklund L. Neurological outcome after experimental cardiopulmonary resuscitation: a result of delayed and potentially treatable neuronal injury? Acta Anaes Scand. 2002;46:537–46. doi: 10.1034/j.1399-6576.2002.460511.x. [DOI] [PubMed] [Google Scholar]
- 141.Manning JE, Batson DN, Gansman TW, Murphy CA, Jr, Perretta SG, Norfleet EA. Selective aortic arch perfusion using serial infusions of perflubron emulsion. Academic Emergency Medicine. 1997;4:883–90. doi: 10.1111/j.1553-2712.1997.tb03814.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


