Abstract
Background: Primary care is a potential setting for implementation of depression prevention interventions using cognitive behavioral therapy (CBT) and interpersonal psychotherapy (IPT). The purpose of this study was to develop and conduct a process evaluation of a primary care/ Internet-based intervention that addresses key dissemination barriers in a community setting.
Method: We used an interdisciplinary team of investigators in a multistep intervention development process among a sample of primary care patients (aged 18 to 24 years). The intervention included an initial primary care motivational interview to engage the participant, 11 Internet-based modules based on CBT (to counter pessimistic thinking) and IPT (to activate social networks and strengthen relationship skills), and a follow-up motivational interview in primary care to enhance behavior change. Each component of the intervention was rated with regard to dissemination barriers of (1) fidelity, (2) motivation, (3) dose, (4) perceived helpfulness (rated on a Likert scale), and (5) potential costs. The study was conducted from April through June of 2004.
Results: Fidelity checklist and serial reviews were satisfactory (100% core concepts translated into intervention). Key motivations for participation included (1) risk reduction, (2) intervention effectiveness, (3) “resiliency,” and (4) altruism. In terms of dose, 13 of 14 participants engaged the Internet-based components, completing a mean of 7.2 modules (SD = 3.9). The 2 primary care interviews and the self-assessment and resiliency modules received the highest helpfulness ratings. The duration of the 2 motivational interviews was approximately 17–18 minutes, which is similar to a typical primary care visit.
Conclusions: By using multidisciplinary teams and incorporating the opinions of potential users, complex preventive mental health interventions can be translated into primary care settings with adequate fidelity, motivation, dose, and perceived helpfulness, and at a reasonably low cost.
Emerging adults (aged 18 to 25 years) have a higher incidence and cumulative prevalence of depressive disorders than any other age group.1–3 Emerging adults experience developmental challenges and adverse events that may make these individuals uniquely vulnerable to depressive disorders.4,5 While primary care chronic disease management models have demonstrated improvements in process and depression outcomes for youth,6 depression remains an important cause of educational impairment, lost productivity, tobacco abuse, relationship problems, and mortality (suicide) in adolescence.1,7–10 Preventive approaches offer the promise of reducing the morbidity associated with depressive disorders during the transition to adulthood. A targeted depression prevention intervention using a group psychotherapy model based on cognitive behavioral therapy (CBT) in adolescents has demonstrated reductions in the incidence of depression in 2 studies.11,12 Unfortunately, many face-to-face preventive interventions (group or individual) are not easily disseminated into primary care settings. The costs of training personnel and staffing programs, the limited supply of mental health specialists in many areas (e.g., rural settings), and low cultural acceptability of face-to-face counseling are barriers to implementation of such interventions in communities.13–16
The role of depression prevention in primary care is a natural combination of mental health and preventive services already provided by primary care physicians. Primary care physicians currently play a critical role in the identification, treatment, and referral of adolescents and emerging adults with depression.17 For example, pediatricians and family practitioners evaluate children and adolescents for risk of future cardiovascular disease using blood pressure measurements and total cholesterol levels. Preventive mental health care is a natural extension of this role.18 The American Psychological Association has recommended the integration of preventive interventions for mental disorders into medical settings.19 The American Academy of Pediatrics encourages physicians to assume a more active role in identifying risk factors for future mental disorders and in helping families modify their beliefs and behaviors.20 There is also an increasing recognition of the need to find ways to engender resiliency and protective factors in youth in multiple community settings.21
The primary care setting also offers several advantages in overcoming key feasibility and acceptability barriers for the implementation of depression prevention interventions in community settings. Most adolescents see their primary care physicians at least once per year and are receptive to counseling and advice from their physicians about their health and behavior.22 Primary care physicians currently provide counseling services for psychological problems in as many as 24% of patient encounters.23 As many as 61% of primary care counseling sessions include elements of CBT.24 Primary care physicians have been successfully taught and have implemented motivational interviewing techniques to reduce problem behaviors.25 For example, a primary care intervention that included 2 short motivational visits and a workbook completed by the patient continued to have an impact on reduced problem drinking up to 4 years later.26
Self-directed treatment programs may have effectiveness levels similar to one-on-one counseling and are acceptable to patients.27–29 However, without supervision, few emerging adults or adolescents complete free-standing Internet-based programs.30,31 Coupling self-directed programs with limited face-to-face contact may increase the efficacy of such interventions. A randomized trial of an Internet-based depression self-management intervention coupled with 6 follow-up telephone calls demonstrated significant reductions in depressed mood in adults.32 In an adult sample, Dutch investigators who used a similar self-directed primary care workbook preventive intervention demonstrated a 33% reduction in the incidence of major depression.16 Because more than half of all adolescents already use the Internet to seek health information, the Internet is ideally suited for delivery of a behavior change intervention for youth.33–36 While there are strong theoretical and empirical rationales for a self-directed combined primary care Internet-based intervention, there is currently no such intervention available for emerging adults.
For this study, we developed an intervention to explore the potential feasibility of a primary care Internet-based depression prevention program. We incorporated and considered common known barriers to community implementation. Little is known on how individuals use and experience Internet-based interventions intended to reduce depression symptoms. The purpose of this study is to develop and conduct a process evaluation of the combined primary care Internet-based depression prevention intervention that addresses key community implementation barriers of (1) fidelity, (2) motivation, (3) dose, (4) perceived helpfulness, and (5) potential cost.37–39
METHOD
Overview
We used a 2-stage approach for the development and assessment of this program. First, development of the combined primary care Internet-based intervention and second, a process evaluation by 14 emerging adults recruited from 2 urban primary care settings.40 The intervention development took place at Johns Hopkins University and the University of Chicago and was approved by the institutional review boards of both universities. The process evaluation took place in the city of Chicago at a university student health clinic and an urban primary care clinic. The study was conducted from April through June of 2004. In this section we describe (1) the formative research and intervention development, (2) the intervention description and evidence for efficacy, and (3) the formative (fidelity) and process evaluation (including statistical and qualitative methods).40
Formative Research and Intervention Development
Development process
We used a community-centered approach for the intervention development and for the process of translating manuals. This approach included (1) selection of a best practice approach, (2) tailoring and adaptation of technologies, (3) practitioner and patient control (allowing both some discretion in the implementation of the intervention), and (4) self-evaluation incorporated into the process evaluation.37 In terms of choice of a best practice model, we selected manuals with demonstrated efficacy.
Primary care component
We selected the motivational interview approach because of its demonstrated efficacy in the treatment of substance use and in the reduction of at-risk behaviors in adolescents and emerging adults.41 With regard to tailoring and adaptation of new technologies, we found that the Internet is a widely accepted source of health information for adolescents and emerging adults; 75% to 80% of this group have Internet access and use the Internet to search for health information.33–36 We emphasized control by the emerging adult and local evaluation through the use of a community motivational encounter that emphasizes the emerging adult's role in choosing healthy behaviors, and also by using goal-setting and choice-making throughout the Internet-based intervention. The integration of the intervention into the primary care environment allowed for local evaluation.
Internet component
We used The Adolescent Coping With Stress Course,42 Interpersonal Psychotherapy: A Clinician's Guide,43 and Interpersonal Psychotherapy for Depression44 to develop the Internet-based components. The Adolescent Coping With Stress Course has demonstrated a reduction in the incidence of depression in 2 randomized trials using a group psychotherapy approach.11,12 We used a process of initial translation followed by serial reviews for fidelity conducted by a health psychologist, authors of the original manuals, a practicing psychologist, and a youth editor. Before translating the manuals, the texts were outlined with regard to key concepts in order to create a fidelity checklist. The translation principles were to maintain a high degree of fidelity to source content while also achieving high degrees of readability, ease of understanding, and perceived helpfulness. To increase perceived helpfulness, we avoided technical psychological terminology and jargon in lieu of everyday examples. We addressed common concerns with regard to depression interventions identified in our prior surveys.45,46
Intervention Description and Evidence of Efficacy
Primary care component
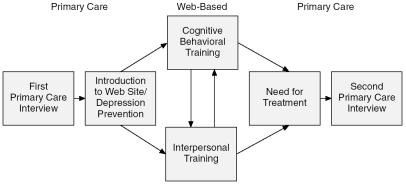
The community-level engagement of the at-risk adolescent uses a manual-based motivational interview.41 Figure 1 describes the intervention sequence and structure, and Table 1 provides an overview of the content of the intervention. We adapted this approach for the purpose of motivating emerging adults to engage in a resiliency-based depression prevention program. The physician helps the emerging adult to identify his or her personal goals and to understand how depression poses risks to these goals and promotes self-efficacy to boost the motivation needed to change behavioral risk factors (e.g., GUARDS: Goals, Understanding, Adolescent, Risk, Depression, Self-efficacy).
Figure 1.
Sequence of Primary Care Internet-Based Intervention to Prevent Depression in Emerging Adults
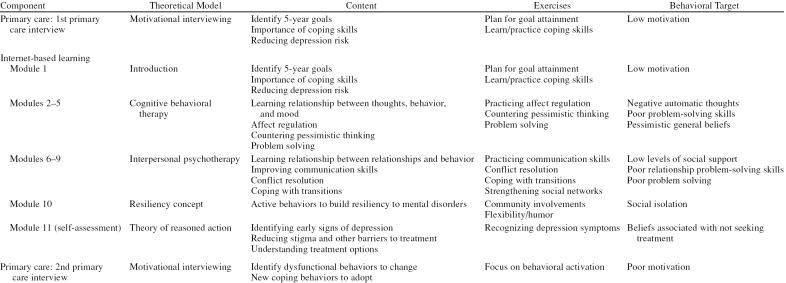
Table 1.
Components of Primary Care, Internet-Based Intervention to Prevent Depression in Emerging Adults
The physician asks open-ended questions that enable the emerging adult to evaluate the costs/benefits of participation in the intervention. In this way, the emerging adult develops his or her own rationale for engagement with the preventive intervention. The purpose of the follow-up interview is to review the exercises and to encourage the adolescent to further practice and develop the protective behaviors. The principal investigator, a primary care physician, received approximately 3 hours of instruction on the motivational interview technique from an experienced practitioner and investigator. The trainer worked closely with the principal investigator in the development of the manual for this intervention.
Internet component
Table 1 describes the components, theoretical conceptualization, content exercises, and behavioral risk factors targeted for each module. Participants submit their personal life goals in the first module to establish personal relevance. Subsequent modules focus on teaching emerging adults to identify the behavior, thought, or interpersonal situation causing their depressed mood and how they may change their responses and reduce their depressed moods. In the CBT modules, participants learn to identify and counter pessimistic and irrational thoughts (both automatic thoughts and general beliefs), regulate affect, and solve personal problems. In the interpersonal psychotherapy (IPT) modules, participants learn to problem-solve relationship problems, cope with transitions, and engage and increase their means of social support. The tenth module encourages participants to build “resiliency” by engaging in the wider community (such as performing altruistic activities), adopting flexible strategies to deal with new situations, and using humor and hope to overcome obstacles.21 In the final module, participants learn how to recognize the symptoms of depression, what the current treatment options are, and how to overcome stigma. Each module has exercises that participants can complete online and print for review at their leisure.
Evidence for intervention efficacy
We completed a pilot study to evaluate changes in depression risk factors among completers of the intervention. We evaluated depressive symptoms (Center for Epidemiologic Studies Depression Scale47), dysfunctional thinking (Automatic Thoughts Questionnaire Revised48), and social support (Social Support Questionnaire-Short Form49) to evaluate changes in established risk factors for depressive disorders during the study (measures compared before and after intervention). Participants who completed the intervention showed favorable trends for certain risk factors, including reduced depressive symptoms, reduced dysfunctional thinking, and increased social support.50
Intervention Formative (Fidelity) and Process Evaluation
Fidelity evaluation
A research assistant (J.M.E.) was trained to review and identify key content items from the original manuals in the translated text and create a fidelity checklist. A health psychologist (J.F.) trained in several psychotherapy approaches conducted the initial fidelity review for overall fidelity models (CBT, IPT). Subsequently, either the original authors (for IPT)43,44 or a trained research coordinator (for CBT) with knowledge of the original manuals and content reviewed the intervention to ensure that each key component from the original intervention was present and correctly described in the final intervention.
Sample recruitment
For the process evaluation, we recruited 14 emerging adults (aged 18 to 24 years) from 2 primary care settings (an urban primary care clinic and a university student health clinic) who were at risk for developing major depression. Participants were recruited by fliers posted in and around the clinics and by physician or nurse recommendation. Eligibility criteria included having at least 1 of the following risk factors for developing depression: (1) a family history of clinical depression or (2) a personal history of depression. We excluded those who had a moderate probability of having major depression (Center for Epidemiologic Studies Depression Scale score > 16),51 suicidal ideation, or active substance abuse. After acquiring informed consent and completing enrollment and an initial interview, we provided each participant with instructions on how to use the Internet site. Participants completed pre/post participation surveys that assessed motivation and perceived helpfulness. Participants also maintained a diary of usage that included the times the participant logged on and off the Internet site, ratings, and comments with regard to each component. Thirteen of the 14 participants completed either an in-person or telephone follow-up interview (and 1 participant who dropped out declined telephone follow-up).
Process evaluation
For motivation, we adapted the standard approach for measuring motivation as described by Miller and Rollnick41 (1 = not important; 10 = very important) to evaluate importance, self-efficacy, and readiness to complete the intervention. After each module or component, we asked each participant if that section “made [him or her] want to change” (the targeted behavior). Each participant was asked to identify his or her motivations for participation.
We assessed dose received, perceived helpfulness, and costs with a variety of measures. To assess dose received, we asked participants to record start and stop times for each module and to complete knowledge tests in a diary. The primary care interviewer recorded the total duration of the interview and techniques used. Additionally, participants rated the ease of reading and understanding for each component using a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). For perceived helpfulness, participants rated each component of the intervention, again on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree), in terms of adverse effects (e.g., “brought up sad or angry feelings”) and helpfulness (e.g., “exercises were helpful”) and provided answers to open-ended questions (e.g., “What did you like?” “What did you dislike?” “What would you change?”). We evaluated costs to participants and primary care physicians in 4 ways: time, ranking of participation in the intervention relative to other activities, willingness to pay for the intervention (e.g., “What is the most you would be willing to pay for this program?”), and themes.
Statistical methods
We report descriptive results with means and standard deviations. We calculated the Spearman correlation coefficient between measures of intention at baseline (importance, self-efficacy, and readiness) and performance of the intervention components (total time, number of modules) using diaries maintained by the participants. We conducted a subgroup analysis to understand how community-dwelling urban and university-affiliated emerging adults may have responded differently to the intervention. The Fisher exact test or t test was used as appropriate.
Qualitative methods
Grounded theory was utilized to identify major themes in individuals' experiences with the program in postintervention interviews and diaries maintained while participating.52 We used extensive probing of participants to elicit key concerns in interviews. In reviewing both the diary entries and the interview responses, the principal investigator and a research assistant in the same age group as the participants analyzed results independently to reduce the probability of bias. Conflicting interpretations were resolved by consensus. The principal investigator and research assistant had prior training in qualitative research methods.
RESULTS
Sample
Almost all of the individuals qualified to enter the study were enrolled (14/16; 2 chose not to enroll after the phone screen because of lack of interest in the study). It was a diverse group of participants (8/14 male, 6/14 African American, 1/14 Hispanic). All 14 participants had completed high school, 10 were full-time college students, and 4 were not currently employed.
Most participants had some level of current depressed mood and had favorable or somewhat favorable attitudes toward treatment. The mean Center for Epidemiologic Studies Depression Scale score was 13, a score indicative of a mild depressed mood. In terms of prior treatment experience, 7 of 14 participants had personal prior treatment (counseling, N = 7; medication, N = 5) and 4 of 14 reported that a family member had been treated. In terms of attitudes toward treatment, 13 of 14 agreed with one of these statements: “Some medications are effective in treating depression” or “Medications are effective in treating depression,” and 9 of 14 agreed with the statement, “For most people, counseling is as effective as medication in treating depression.”
Formative (Fidelity) Evaluation
Fidelity checklist and serial reviews were satisfactory for the primary care and Internet components. Eighty-seven core content items and exercises were identified in the original texts and present in the final intervention. Where the authors of the original non–Internet-based intervention recommended a change in content or wording to enhance clarity, those changes were made. The Flesch-Kincaid grade level was 7.1.
Process Evaluation
Motivation
Participants reported a strong intention to participate in the depression prevention intervention (1–10 scale; higher scores indicate greater importance); sample comments include “depression prevention is important” (mean = 8.4, SD = 1.5), “am able to change behavior to reduce my risk of depression” (mean = 8.0, SD = 1.8) (self-efficacy), and “I am ready to change behavior” (mean = 8.2, SD = 1.8). Two individuals noted that they had difficulty motivating themselves to complete the intervention because they were not currently depressed. There was a significant negative correlation between self-efficacy at baseline and total number of modules completed (r = –0.59, p = .02), a nonsignificant negative correlation with regard to readiness (r = –0.24, p = .48), and a nonsignificant positive correlation between importance and modules completed (r = 0.40, p = .15). The most common motivations for participation were a desire to prevent a recurrence (N = 7), relief from current symptoms/life stress (N = 3), recommendation by a parent or friend (N = 3), self-improvement (N = 2), to avoid an episode similar to that of a relative (N = 2), and/or altruism (N = 1).
With regard to sustaining motivation, the predominant theme reported was that the intervention required ongoing motivation to complete the intervention and actually change behavior (N = 10). Two participants dropped out on the basis of recommendations of others related to concerns about anxiety. One participant stated that he wished to continue and felt comfortable doing so, but did not wish to contradict his family's recommendation. The other participant preferred to continue; however, the participant's psychotherapist preferred that the participant address issues of behavior change within a traditional face-to-face therapeutic relationship. The Internet components that participants rated most strongly for increasing their desire to change behavior were CBT and resiliency (Table 2).
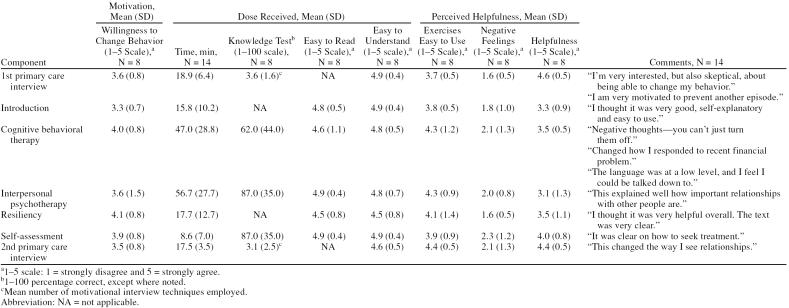
Table 2.
Process Evaluation of Intervention Component
Dose
All participants completed the first motivational interview, and 8 completed the second motivational interview (Figure 2). In both the first and second interviews, the mean time was less than 20 minutes with a mean number of 3 techniques delivered (Table 2). Reflective listening was the most commonly used technique (22 of 25 interviews). Several other techniques were used, including looking forward (19/25), reframing (7/25), exaggeration (4/25), accepting personal responsibility (2/25), and shifting the focus (1/25). “Strongly agree” ratings were achieved for ease of understanding (Table 2) and for the feeling that “the physician listened to [the participant]” (data not shown).
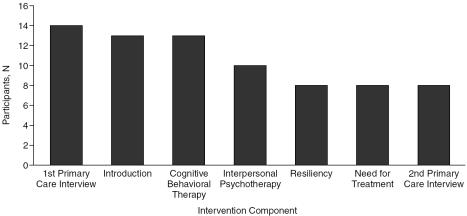
Figure 2.
Number of Participants Engaging Each Component of the Primary Care Internet-Based Intervention to Prevent Depression in Emerging Adults
Thirteen participants engaged the Internet site, 13 of 14 completed at least 3 modules, and 8 of 14 completed the entire intervention (Figure 2). Mean number of modules completed was 7.2 (SD = 3.9). Participants spent approximately 45 to 60 minutes on each of the 2 major components (CBT and IPT, Table 2). To assess pattern of use, we calculated mean time per module (mean = 15.0 minutes, SD = 4.8), mean time per session (mean = 40.1 minutes, SD = 32.1), mean time between sessions (mean = 3.5 days, SD = 3.4), and mean time from start to completion of the Internet-based modules (mean = 10.8 days, SD = 6.1). On a scale of 1–5, all Internet components of the intervention received ratings in the agree range (4 or 5) for ease of reading and understanding. In terms of participant knowledge of the intervention concepts, satisfactory scores were obtained for all components except for CBT.
Important themes from comments with regard to dose included clarity/simplicity and length/burden. Participants often reported different opinions of various portions of the intervention. With regard to clarity/simplicity, subthemes included “helpfulness” (e.g., “It was clear and made me really consider how negative thoughts have impacted my life”) and “patronizing” (e.g., “[The] language was at a low level, and I feel I could be talked down to” [i.e., felt condescended to]). In terms of length/burden, we identified 2 subthemes: “repetitive” (e.g., “It was kind of redundant” and “too long”) and “comforting” (e.g., “Very soothing and encouraging” and “I thought it was very good, self-exploratory, and easy to use”).
Perceived helpfulness
The 2 primary care interviews and the self-assessment and resiliency modules received the highest helpfulness ratings (Table 2). With regard to perceived helpfulness, the predominant themes in comments received from participants were “personal utility” with subthemes of “resonance” (e.g., “I liked the relationship issue information––really resonated with me”) and “resistance” (e.g., “I do not believe I have social relationship issues so it was not relevant.”).
Costs
Participants reported that a “fair price to pay for the program” was a mean of $21.43 (SD = $15.99) versus $28.63 that they would pay for a rare, out-of-print CD. In comparison to other activities, participating in the intervention ranked ahead of studying and working at a job, behind reading a book or going to the movies with a friend, and at nearly the same level as working out. The mean duration of each individual motivational interview was 17 to 18 minutes, roughly equivalent to a typical primary care visit (15.4 minutes).53
Subgroup analysis comparing urban clinic and university participants
Urban clinic participants were more likely than university participants to be African American (7/7 vs. 0/7, p = .001), less likely to have received past treatment for depressive disorders (0/6 vs. 6/8, p = .01), and were more depressed at baseline (Center for Epidemiologic Studies Depression Scale mean score = 17.3 vs. 9.8, p = .03). However, both groups had similar mean levels of education (14.3 for urban clinic participants vs. 14.0 for university participants, p = .82), were of similar age (mean = 19.8 vs. 20.3 years, p = .68), had similar proportions of men (4/6 vs. 2/8, p = .28) and of mothers who were college graduates (3/6 vs. 8/8, p = .06), and had similar mean levels of baseline motivation (stage of change level 3.5 vs. 3.8 [indicates both were at the “action” stage of the trans-theoretical model of change], p = .84). Those recruited from the urban site were more likely to drop out (5/6 vs. 1/8, p = .03), complete fewer modules, (mean = 4.2 vs. 10.4, p = .002), and spend less time online working on the intervention (mean = 64.8 minutes vs. 137.2 minutes, p = .04).
DISCUSSION
We developed a combined primary care Internet-based depression prevention intervention for emerging adults using a community-based model to address known barriers to the implementation of psychosocial interventions, such as fidelity, motivation, adequate dose, perceived helpfulness, and cost. The resulting intervention maintained a high degree of fidelity to the original theoretical models and specific behavioral change components while using a low reading level and achieving high ratings for ease of reading, understanding, use, and helpfulness. At baseline, participants were very motivated to participate in the depression prevention intervention. The most important motivations appeared to be the beliefs that the intervention could either prevent depression in the future or ameliorate current depressed mood. Nearly all the participants engaged the intervention, and most completed some portion of the Internet-based training. While the intervention received satisfactory ratings for ease of reading, understanding, and helpfulness and a large predominance of favorable comments with regard to usefulness, many reported that the intervention's length and repetition remained an important barrier. We have previously reported that completers of this intervention demonstrated favorable trends (not statistically significant) in depressed mood, automatic negative thoughts, and social support in pre/post study comparisons.50
The unique contribution of this study is to provide a description of the development and use of a primary care Internet-based depression prevention intervention for emerging adults. We are not aware of any other similar intervention. This alternative model builds on the existing, inherent relationships between communities, emerging adults, and the Internet. The model capitalizes on the therapeutic alliance between primary care physicians and emerging adults; on the desire of many primary care patients to reduce depression symptoms “naturally,” without face-to-face contact with a mental health specialist; and also on the low-cost delivery, privacy, and accessibility of the Internet. Additionally, this study provides a structured approach for translating mental health interventions developed in mental health specialty settings into primary care and community settings while conducting a process evaluation to determine the effectiveness of the translation.
This study also provides a deeper understanding of the barriers that may prevent many individuals in primary care settings from completing self-directed interventions.30,31,54 Our observation that beliefs about potential value of participation, likelihood of benefit (efficacy), and social norms (recommendations of others) are the key motivations for most individuals is consistent with prior studies of both mental health care seeking and adoption of physical exercise.15,55 The inverse relationship between the number of modules completed and self-efficacy may be explained by participants either feeling that their coping skills were already adequate or underestimating the difficulty of completing the intervention. Comments regarding the length of the intervention and the difficulty in changing behaviors support the latter inference.
Ensuring high perceived helpfulness and low cost needed for dissemination proved challenging. Decreasing the reading complexity level and removing technical terminology increased accessibility but diminished the perceived helpfulness and efficacy of the intervention from the perspective of some of the participants. Furthermore, interventions may require further adaptation to address specific needs of urban emerging adults and to enhance participation and completion rates. Similarly, while some participants were motivated by a desire to reduce their risk of depression, others preferred the more positive concept of “building resiliency” or moving toward valued goals.21 The participants' willingness to pay ($21.43) is approximately equivalent to typical copayment for the 2 primary visits required for the intervention. In actual practice, participation in a sustainable Internet-based intervention might require an additional $10 to $25 payment.
The principal limitations of the intervention design were (1) a lack of scheduled telephone follow-ups to problem-solve barriers, (2) a lack of Internet-based responses to concerns (such as anxiety), and (3) the absence of behavioral activation as an alternative strategy for reducing the risk of depression. Individuals who either found the cognitive-intensive approaches too abstract for current problems or developed excessive anxiety with cognitive approaches might have responded to the behavioral activation approach, which focuses on reestablishment of regular, pleasant, meaningful activities. A revised version of the intervention currently under construction addresses both of these limitations. Although the sample size was small, the participants included men and ethnic minorities, who are often underrepresented in depression studies. The study reliance on diary entries may have overestimated participation. However, diary entries were accompanied by specific comments with regard to each timed component.
Given cost constraints, the limited supply of mental health specialists, and the need to reduce the burden of depressive disorders in emerging adults, preventive interventions in primary care are needed.14,56,57 The results of this study suggest that primary care Internet-based depression prevention interventions may be feasible, acceptable, and effective. Multidisciplinary teams may be an effective approach to translating complex mental health interventions into primary care and community settings. However, considerable research will be needed to address several key issues of (1) maintaining motivation for completion and managing negative emotions while on the Internet program, (2) effective identification and referral of those at risk for depressive disorders, (3) enhancing perceived helpfulness to ethnic minority participants through sociocultural adaptation, (4) understanding moderators and mediators of intervention participation and efficacy, and (5) feasibility and implementation in non-academic primary care practices. To address these barriers, we have revised this intervention on the basis of this evaluation, and are currently fielding 2 studies in community and primary care settings (the revised intervention can be viewed at http://catchit.bsd.uchicago.edu using user name “guest” and password “test”). Primary care physicians may want to consider recommending Internet-based cognitive behavioral psychotherapy interventions for emerging adults who are at risk for developing major depression.
Footnotes
This work was supported by the Centers for Disease Control, Prevention Research Centers, Grant #U48/CCU309674; National Association for Research on Schizophrenia and Affective Disorders (NARSAD) Young Investigators Award (2004); Project CATCH-IT Primary Care Based Depression Prevention for Adolescents; and Robert Wood Johnson Foundation Depression in Primary Care Linking Clinical and System Strategies, #051780.
The authors report no additional financial interests relating to this article and have no conflicts of interest.
REFERENCES
- Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety. 1998;7:3–14. doi: 10.1002/(sici)1520-6394(1998)7:1<3::aid-da2>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Klerman GL. The current age of youthful melancholia: evidence for increase in depression among adolescents and young adults. Br J Psychiatry. 1988;152:4–14. doi: 10.1192/bjp.152.1.4. [DOI] [PubMed] [Google Scholar]
- Klerman GL, Weissman MM. Increasing rates of depression. JAMA. 1989;261:2229–2235. [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. The development of depression in children and adolescents. Am Psychol. 1998;53:221–241. doi: 10.1037//0003-066x.53.2.221. [DOI] [PubMed] [Google Scholar]
- Berry D. The relationship between depression and emerging adulthood: theory generation. ANS Adv Nurs Sci. 2004;27:53–69. doi: 10.1097/00012272-200401000-00007. [DOI] [PubMed] [Google Scholar]
- Asarnow JR, Jaycox LH, and Duan N. et al. Effectiveness of a quality improvement intervention for adolescent depression in primary care clinics: a randomized controlled trial. JAMA. 2005 293:311–319. [DOI] [PubMed] [Google Scholar]
- Reinherz HZ, Giaconia RM, and Hauf AM. et al. General and specific childhood risk factors for depression and drug disorders by early adulthood. J Am Acad Child Adolesc Psychiatry. 2000 39:223–231. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Schwartz S, and Dohrenwend BP. et al. Minor depression in a cohort of young adults in Israel. Arch Gen Psychiatry. 1994 51:542–551. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kilbey MM, Andreski P. DSM-III-R nicotine dependence in young adults: prevalence, correlates and associated psychiatric disorders. Addiction. 1994;89:743–754. doi: 10.1111/j.1360-0443.1994.tb00960.x. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wolk S, and Goldstein RB. et al. Depressed adolescents grown up. JAMA. 1999 281:1707–1713. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hawkins W, and Murphy M. et al. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention. J Am Acad Child Adolesc Psychiatry. 1995 34:312–321. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hornbrook M, and Lynch F. et al. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Arch Gen Psychiatry. 2001 58:1127–1134. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Gonzales JJ, and Gallo JJ. et al. The acceptability of treatment for depression among African-American, Hispanic, and white primary care patients. Med Care. 2003 41:479–489. [DOI] [PubMed] [Google Scholar]
- Van Voorhees BW, Cooper LA, and Rost KM. et al. Primary care patients with depression are less accepting of treatment than those seen by mental health specialists. J Gen Intern Med. 2003 18:991–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Voorhees BW, Fogel J, and Houston TK. et al. Beliefs and attitudes associated with the intention to not accept the diagnosis of depression among young adults. Ann Fam Med. 2005 3:38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willemse GR, Smit F, and Cuijpers P. et al. Minimal-contact psychotherapy for sub-threshold depression in primary care: randomized trial. Br J Psychiatry. 2004 185:416–421. [DOI] [PubMed] [Google Scholar]
- Richardson LP, Katzenellenbogen R. Childhood and adolescent depression: the role of primary care providers in diagnosis and treatment. Curr Probl Pediatr Adolesc Health Care. 2005;35:6–24. doi: 10.1016/j.cppeds.2004.09.001. [DOI] [PubMed] [Google Scholar]
- Kronn DF, Sapru A, Satou GM. Management of hypercholesterolemia in childhood and adolescence. Heart Dis. 2000;2:348–353. [PubMed] [Google Scholar]
- Johnson SB, Millstein SG. Prevention opportunities in health care settings. Am Psychol. 2003;58:475–481. doi: 10.1037/0003-066X.58.6-7.475. [DOI] [PubMed] [Google Scholar]
- Schor E. Report of the task force on the family. Pediatrics. 2003;111:1541–1571. [PubMed] [Google Scholar]
- Bell CC. Cultivating resiliency in youth. J Adolesc Health. 2001;29:375–381. doi: 10.1016/s1054-139x(01)00306-8. [DOI] [PubMed] [Google Scholar]
- Joffe A, Radius S, Gall M. Health counseling for adolescents: what they want, what they get, and who gives it. Pediatrics. 1988;82:481–485. [PubMed] [Google Scholar]
- Olfson M, Weissman MM, and Leon AC. et al. Psychological management by family physicians. J Fam Pract. 1995 41:543–550. [PubMed] [Google Scholar]
- Robinson P, Bush T, and Von Korff M. et al. Primary care physician use of cognitive behavioral techniques with depressed patients. J Fam Pract. 1995 40:352–357. [PubMed] [Google Scholar]
- Emmons KM, Rollnick S. Motivational interviewing in health care settings: opportunities and limitations. Am J Prev Med. 2001;20:68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Mundt MP, and French MT. et al. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res. 2002 26:36–43. [PubMed] [Google Scholar]
- Scogin F, Bynum J, and Stephens G. et al. Efficacy of self-administered treatment programs: meta-analytic review. Prof Psychol Res Pr. 1990 21:42–47. [Google Scholar]
- Cuijpers P. Bibliotherapy in unipolar depression: a meta-analysis. J Behav Ther Exp Psychiatry. 1997;28:139–147. doi: 10.1016/s0005-7916(97)00005-0. [DOI] [PubMed] [Google Scholar]
- Kaltenthaler E, Shackley P, and Stevens K. et al. A systematic review and economic evaluation of computerized cognitive behavior therapy for depression and anxiety. Health Technol Assess. 2002 6:1–89. [DOI] [PubMed] [Google Scholar]
- Clarke GN, Hornbrook M, and Lynch F. et al. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Arch Gen Psychiatry. 2001 58:1127–1134. [DOI] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Korten A. Web-based cognitive behavior therapy: analysis of site usage and changes in depression and anxiety scores. J Med Internet Res. 2002;4:e3. doi: 10.2196/jmir.4.1.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the Internet: randomized controlled trial. BMJ. 2004;328:265. doi: 10.1136/bmj.37945.566632.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanauer D, Dibble E, and Fortin J. et al. Internet use among community college students: implications in designing healthcare interventions. J Am Coll Health. 2004 52:197–202. [DOI] [PubMed] [Google Scholar]
- Borzekowski DL, Rickert VI. Adolescent cybersurfing for health information: a new resource that crosses barriers. Arch Pediatr Adolesc Med. 2001;155:813–817. doi: 10.1001/archpedi.155.7.813. [DOI] [PubMed] [Google Scholar]
- Gould MS, Munfakh JL, and Lubell K. et al. Seeking help from the Internet during adolescence. J Am Acad Child Adolesc Psychiatry. 2002 41:1182–1189. [DOI] [PubMed] [Google Scholar]
- Skinner H, Biscope S, and Poland B. et al. How adolescents use technology for health information: implications for health professionals from focus group studies. J Med Internet Res. 2003 5:e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wandersman A. Community science: bridging the gap between science and practice with community-centered models. Am J Community Psychol. 2003;31:227–242. doi: 10.1023/a:1023954503247. [DOI] [PubMed] [Google Scholar]
- Wandersman A, Florin P. Community interventions and effective prevention. Am Psychol. 2003;58:441–448. doi: 10.1037/0003-066x.58.6-7.441. [DOI] [PubMed] [Google Scholar]
- Nation M, Crusto C, and Wandersman A. et al. What works in prevention: principles of effective prevention programs. Am Psychol. 2003 58:449–456. [DOI] [PubMed] [Google Scholar]
- Escoffery C, McCormick L, Bateman K. Development and process evaluation of a web-based smoking cessation program for college smokers: innovative tool for education. Patient Educ Couns. 2004;53:217–225. doi: 10.1016/S0738-3991(03)00163-0. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. New York, NY: The Guilford Press. 2002 [Google Scholar]
- Clarke GN. The Coping With Stress Course: Adolescent Workbook. Portland, Ore: Kaiser Permanente Center for Health Research. 1994 [Google Scholar]
- Stuart S, Robertson M. Interpersonal Psychotherapy: A Clinician's Guide. New York, NY: Oxford University Press. 2003 [Google Scholar]
- Klerman GL, Weissman MM, and Rounsaville BJ. et al. Interpersonal Psychotherapy for Depression. New York, NY: Basic Books. 1984 [Google Scholar]
- Van Voorhees BW, Clarke G, and Stuart S. et al. Project CATCH-IT: a primary care/web based depression prevention intervention development project for adolescents and young adults [poster]. Presented at the National Research Service Award Trainees Conference. 26June2003 Nashville, Tenn. [Google Scholar]
- Van Voorhees BW, Fogel J, and Houston TK. et al. Attitudes and illness factors associated with low perceived need for depression treatment among young adults. Soc Psychiatry Psychiatr Epidemiol. 2006 41:746–754. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Hays RC. Self-referent speech and psychopathology: the balance of positive and negative thinking. Cognit Ther Res. 1989;13:583–598. [Google Scholar]
- Sarason IG, Sarason BR, Shearin EN. A brief measure of social support: practical and theoretical implications. J Soc Pers Relat. 1987;4:497–510. [Google Scholar]
- Van Voorhees BW, Ellis J, and Stuart S. et al. Pilot study of a primary care Internet-based depression prevention intervention for late adolescents. Can Child Adolesc Psychiatry Rev. 2005 14:40–43. [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. App Psychol Meas. 1977;1:385–401. [Google Scholar]
- Strauss CJ. Basics of Qualitative Research. Grounded Theory Procedures and Techniques. Newbury Park, Calif: Sage. 1990 [Google Scholar]
- Bensing JM, Roter DL, Hulsman RL. Communication patterns of primary care physicians in the United States and the Netherlands. J Gen Intern Med. 2003;18:335–342. doi: 10.1046/j.1525-1497.2003.10735.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patten SB. Prevention of depressive symptoms through the use of distance technologies. Psychiatr Serv. 2003;54:396–398. doi: 10.1176/appi.ps.54.3.396. [DOI] [PubMed] [Google Scholar]
- Hagger MS, Chatzisarantis NL, Biddle SJH. The influence of autonomous and controlling motives on physical activity intentions within the Theory of Planned Behavior. Br J Health Psychol. 2002;7:283–297. doi: 10.1348/135910702760213689. [DOI] [PubMed] [Google Scholar]
- Weissman E, Pettigrew K, and Sotsky S. et al. The cost of access to mental health services in managed care. Psychiatr Serv. 2000 51:664–666. [DOI] [PubMed] [Google Scholar]
- Van Voorhees BW, Wang NY, Ford DE. Managed care organizational complexity and access to high-quality mental health services: perspective of US primary care physicians. Gen Hosp Psychiatry. 2003;25:149–157. doi: 10.1016/s0163-8343(03)00017-3. [DOI] [PubMed] [Google Scholar]