Abstract
Background: Despite increasing psychotropic drug prescriptions worldwide, little is known about utilization of these medications in the general population in Israel. We examined psychotropic drug use in the general population of Israel and the patterns of use among individuals with different DSM-IV diagnoses of 12-month mental disorders.
Method: A representative sample was derived from the National Population Register of noninstitutionalized residents aged 21 and older. Face-to-face interviews were conducted from May 2003 to April 2004. Individuals were asked about any psychotropic drug use in the past 12 months. DSM-IV disorders were assessed using a revised version of the World Health Organization's Composite International Diagnostic Interview.
Results: Psychotropic drug utilization was observed in 6.9% of the general population and in 19.6% of individuals with any 12-month psychiatric disorder. The extent of use varied according to sociodemographic variables and the specific DSM-IV diagnostic categories. Among individuals with a 12-month diagnosis of pure major depression, only 13.6% received any antidepressants within the same period; exclusive use of antidepressants was 5.7%, while 3.3% of the individuals used only anxiolytics.
Conclusion: Similar to findings in other European countries, our findings suggest that the majority of individuals diagnosed with a common mental disorder are not being treated with psychotropic drugs or are being inappropriately treated.
During the past thirty years, psychotropic medication use became common and is increasing in all industrialized countries. The information on prevalence and patterns of drug use in the general population comes from pharmacoepidemiology investigating the interactions between drugs and populations.1 This knowledge about the utilization and impact (benefits and risks) of pharmaceutical products at the level of population actually treated is necessary to inform mental health polices and service developments.2 Several studies in Europe have explored the utilization of psychotropic drugs in representative samples from the general population, but most have been conducted at the national level.3–8 Only 2 large, recent, international surveys provided data for cross-national comparisons: the telephone-based, cross-national survey of the general populations of France, Germany, Italy, and the United Kingdom9 and the European Study of the Epidemiology of Mental Disorders/Mental Health Disability: a European Assessment (ESEMeD/MHEDEA 2000), including the general populations of Belgium, France, Germany, Italy, the Netherlands, and Spain.10 The study reported here supplements the European findings with pharmacoepidemiologic data from Israel.
The Israel National Health Survey (INHS) is the first country-wide study designed to estimate the prevalence rates of common mental disorders and mental health services use, including psychotropic drug utilization in the adult population. Previous surveys were limited to population subgroups11 or to populations in psychiatric treatment.12,13 None investigated the psychotropic medication utilization in the general population and its relationship to the common mental disorders.
The objectives of this report were (1) to evaluate a 12-month prevalence rate of psychotropic drug use in the general population of Israel; and (2) to assess the pattern of use in individuals with different Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnoses of 12-month psychiatric disorders.
METHOD
Sampling and Subjects
The INHS, as a component of the World Mental Health Survey conducted in 27 countries, followed the uniform procedures established.14 The sample was extracted from the National Population Register and comprised nonin-stitutionalized de jure residents aged 21 and older. The sample was designed to reflect the distribution of selected gender-age-population groups in the general population (Arabs and Jews: Israel-born and immigrants from the former Soviet Union or other countries since 1990). The sample was weighted back to the total population to compensate for unequal selection probabilities resulting from disproportionate stratification, clustering effects, and nonresponse. The weights were adjusted to make weighted sample totals conform to known population totals taken from reliable Central Bureau of Statistics (CBS) sources. Face-to-face interviews at the homes of respondents were conducted from May 2003 to April 2004 in Arabic, Hebrew, or Russian. The survey was administered using laptop computer-assisted personal interview methods by professional survey interviewers trained and supervised by the CBS. A letter signed by the Government Statistician, explaining the purpose of the survey and the rights of respondents, was sent to each potential respondent a few days prior to the first contact attempt. Upon making in-person contact with the sampled respondent, the interviewer explained the survey again and obtained verbal informed consent. Interviews took, on average, 60 minutes. The overall response rate was 73% (88% among Arab Israelis and 71% among Jewish Israelis), totaling 4859 completed interviews. There were no replacements. The Experimentation on Human Subjects Committee of the Ministry of Health (Jerusalem, Israel) approved the study.
Assessment of Psychotropic Drug Use
All respondents were asked about the use of any psychotropic medications during the 12 months preceding the survey, even if this occurred only once. Questions probing drug utilization were included in each diagnostic section dealing with specific psychiatric disorders. In addition, a section including 191 items specifically inquired about detailed characteristics of drug use, characteristics of the prescribing clinician(s), duration and frequency of use, reasons for discontinuation, and related issues. The analyses presented in this report refer to any episode of use in the 12 months preceding the interview and do not distinguish between occasional use (a single episode over the year) and a regular or systematic utilization of psychotropic drugs. To overcome recall bias that had often hampered drug utilization studies (especially in the case of prior, short-term use), a standard booklet including a show-card listing psychotropic drugs commonly used in Israel to treat mental health problems and psychiatric disorders was provided. Psychotropic drugs were recorded in the interviews using national brand names and then converted in a drug coding system based on the Anatomical Therapeutic Chemical classification system.15 Although data were collected regarding the specific compounds in each category of medication used, data presented in this report are limited to 5 main drug categories. These were (1) antidepressants (including tricyclics and new-generation antidepressants); (2) anxiolytics (including benzodiazepines and non-benzodiazepine anxiolytic agents, such as buspirone); (3) hypnotics of any pharmacologic class; (4) drugs used for the treatment of psychotic disorders, including antipsychotics (conventional and atypical antipsychotic agents, such as clozapine, olanzapine, quetiapine, ziprasidone, and risperidone), antipsychotic depot injections; and (5) mood stabilizers (including lithium, carbamazepine, valproate, gabapentin, topiramate, and lamotrigine). We expect that the estimate of mood stabilizer use may be higher as some of the drugs included are commonly used for other indications, e.g., chronic pain treatment.
Diagnostic Assessment
The diagnostic instrument used in the INHS was a revised version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI),14 a structured diagnostic interview for assessing the lifetime and recent prevalence of selected psychiatric disorders according to both the International Classification of Diseases, 10th Edition (ICD-10), and the DSM-IV classification systems. In our survey we assessed the following disorders: anxiety disorders (panic disorder, generalized anxiety disorder, agoraphobia without panic disorder, and posttraumatic stress disorder), mood disorders (major depressive disorder, dysthymia, and bipolar disorder I and II), and substance abuse disorders (alcohol abuse, alcohol dependence, drug abuse, and drug dependence). The anxiety disorders excluded specific phobias or social phobia. Prevalence estimates of mental disorders were determined using respondents' reports of past or current symptoms that met the 12-month diagnostic criteria for a DSM-IV disorder. For each disorder, a screening sub-questionnaire was administered to each respondent. All participants responding positively to a specific screening item were asked the questions in the respective diagnostic section of the main questionnaire. All of the CIDI interviews were performed concurrently with the assessments of psychotropic drug utilization.
Statistical Analysis
The proportion of respondents in the general population who reported using psychotropic drugs in the 12 months preceding the interview was computed. Cross-tabulations were used to calculate bivariate odds ratios (ORs) and 95% confidence intervals (CIs) to assess the strength of reported drug use and gender differences. The association of sociodemographic and clinical-diagnostic characteristics with psychotropic drug use was analyzed using univariate logistic regression analysis. All analyses on weighted data were performed using the SAS-9.1 software package (SAS Institute Inc., Cary, N.C.).
RESULTS
Sociodemographic Characteristics
Table 1 presents the characteristics of the study sample (the left 2 columns) alongside with 12-month prevalence of psychotropic drug use distributed according to these characteristics. Mean age was 47.0 years (95% CI = 46.7 to 47.4), with the plurality of the respondents (23%) being between 21 and 29 years old. Men represented 48% of the sample. Nearly 68% were married, and 44% lived in urban areas. The plurality were more highly educated (47%) and in paid employment at the time of the interview (56%). Nearly 82% of the sample identified themselves as Jews and the remaining as belonging to non-Jewish confessions; 15.8% of respondents were recent (since 1990) immigrants from the former Soviet Union, and 2.3% immigrated from elsewhere.
Table 1.
Study Sample Characteristics (raw numbers and weighted proportions) and 12-Month Prevalence of Psychotropic Drug Usea in the General Population
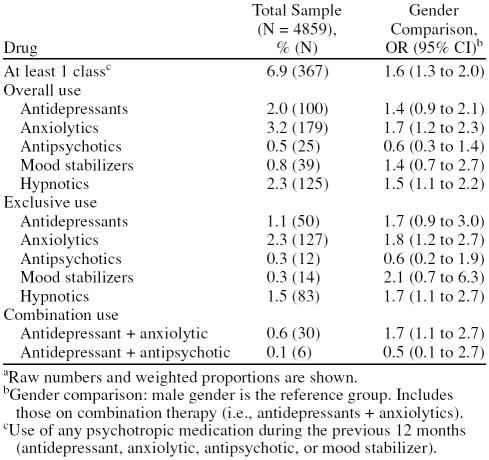
Psychotropic Drug Use
Overall, 6.9% of the general population reported receiving at least 1 psychotropic drug in the 12 months preceding the survey. Use was approximately one and a half times as common in women as in men (OR = 1.6; 95% CI = 1.3 to 2.0). Anxiolytics were the medications most commonly used (3.2%), with a percentage of exclusive users of 2.3%. Hypnotics were the second most common psychotropics used, 2.3% of the sample reporting use in the previous year (OR for women = 1.5, 95% CI = 1.1 to 2.2); the percentage of exclusive hypnotics users was 1.5%. Antidepressants followed in third place, with 2.0% (OR = 1.4, 95% CI = 0.9 to 2.1). Further were mood stabilizers at 0.8% (OR = 1.4, 95% CI = 0.7 to 2.7) (recall, this estimate may be artificially higher as some drugs of this group could be used for other indications). Antipsychotic agents were much less commonly used (0.5%), with 0.3% of individuals using exclusively one of these medications in the previous year. The most frequent drug combination (albeit not necessarily simultaneous) included the use of antidepressants and anxiolytics (0.6%), being more likely used by women compared with men (OR = 1.7, 95% CI = 1.1 to 2.7) (Table 2).
Table 2.
12-Month Psychotropic Drug Use by Gender According to Psychotropic Therapeutic Classa
The prevalence rates of psychotropic drug use in the general population according to sociodemographic characteristics are presented in Table 1 (the right 2 columns). In both genders, the probability of drug use consistently enhanced with age, reaching its maximum in the group older than 70 years old (OR = 15.9, 95% CI = 9.4 to 26.9). Compared with the married, the highest proportion of users was among the previously married (OR = 3.2, 95% CI = 2.5 to 4.2) and the least proportion was among never married (OR = 0.6, 95% CI = 0.4 to 0.9) subjects. The use of psychotropic drugs was somewhat higher among those with low education (primary and secondary school graduates), and a trend was found of lower drug use as years of education increased. Likewise, we found a substantial difference in use patterns depending on employment status, in which the highest use rates were seen among the combined category including disabled, people on illness leave, and retired individuals (OR = 3.8, 95% CI = 3.0 to 4.8). With regard to use patterns in people with different religious observance status, atheists and traditionalists showed a similar, 3.5-fold prevalence rate compared with Orthodox subjects. Finally, compared with Israel-born respondents, immigrants from elsewhere but particularly from the former Soviet Union showed a 2-fold prevalence use pattern (OR = 2.0, 95% CI = 1.5 to 2.5).
Psychotropic Drug Use by Gender, Therapeutic Class, and 12-Month DSM-IV Diagnosis
Table 3 shows drug use for individuals with a 12-month psychiatric disorder according to 4 of the 5 therapeutic classes (i.e., antidepressants, anxiolytics, antipsychotics, and hypnotics), and Table 4 displays the percentage of exclusive use of antidepressants and anxiolytics. Antidepressants were the medications most commonly used, with 11.0% of individuals with any 12-month psychiatric disorder reporting use of one of these drugs during the same period; 4.3% had exclusively used antidepressants. Anxiolytics were the second most commonly used drugs, with 9.2% of individuals with a 12-month diagnosis of a psychiatric disorder reporting prior use (4.2% were exclusive users) within the year before interview. Both antidepressant use and anxiolytic use were only slightly higher in women compared to men (OR = 1.2, 95% CI = 0.6 to 2.2 and OR = 1.3, 95% CI = 0.7 to 2.5, respectively). Hypnotics and antipsychotics were used less frequently among people meeting criteria for any disorders (4.4% and 2.9%, respectively).
Table 3.
12-Month Psychotropic Drug Use by Gender According to 12-Month Mental Disorders
Table 4.
12-Month Exclusive Antidepressant and Anxiolytic Drug Use by Gender, According to 12-Month Mental Disordersa
Among individuals with a 12-month diagnosis of pure major depression, 21.3% took a psychotropic medication, 13.6% took an antidepressant, and 8.8% took an anxiolytic during the same period. Twice as many women than men with this diagnosis took an anxiolytic in the same period (OR = 2.0, 95% CI = 0.8 to 5.3), while no gender differences in antidepressant use were noted (OR = 0.9, 95% CI = 0.5 to 2.0). The proportions of subjects with a diagnosis of pure major depression who received hypnotics and antipsychotics were substantially lower (5.0% and 2.9%, respectively), also without gender differences.
The exclusive use of antidepressants was substantially lower; only 5.7% of individuals with a 12-month diagnosis of pure major depression used exclusively antidepressants and 3.3% used only anxiolytics. The exclusive use of antipsychotics or mood stabilizers was negligible in individuals with this diagnosis.
Among people who had a 12-month diagnosis of pure anxiety disorder, 18.6% of individuals took any psychotropic drug in the same period and 12.8% had used an anxiolytic medication, with no gender differences in both cases. Compared with respondents diagnosed with major depression, a lower percentage (5.9%) used antidepressants, with a higher frequency in women (OR = 2.0, 95% CI = 0.2 to 18.4); only one of the subjects diagnosed with pure anxiety disorder took an antipsychotic medication.
The exclusive use of anxiolytic medications was generally lower, with 4.8% of subjects with a 12-month diagnosis of pure anxiety disorders using only anxiolytics in the same period. None of those having this diagnosis used exclusively antidepressants within the year before the survey. The exclusive use of antipsychotics or mood stabilizers was negligible (data not shown).
Regarding 12-month exclusive antidepressant and exclusive anxiolytic drug use according to DSM-IV disorder status (Table 4), among people with any disorder, 4.3% used antidepressants exclusively. Individuals with pure major depression (5.7%) and with pure mood disorder (6.4%) showed higher proportions of use, but there were also substantial levels of drug usage among those with any anxiety disorder (3.8%). No gender differences in utilization were found, although a trend is suggested of a higher probability of use among women if a mood disorder was present and a lower probability of use among men if an anxiety disorder was the case.
Anxiolytic drugs were taken in an exclusive way by 2.0% of individuals with no disorder and by 4.2% of those with any disorder, with women having a nearly 2-fold probability of use compared to men. There were no great differences in anxiolytic use between specific disorders, with only one exception for any anxiety disorder (6.5%).
DISCUSSION
The INHS is the first study in Israel that directly examined the prevalence and patterns of psychotropic drug use in a representative sample of subjects from the general population. Apart from this, it is the first study to bind psychotropic drug utilization to the 12-month prevalence of common mental disorders. The study findings substantially supplement the picture of psychotropic drug utilization in Europe.
Sociodemographic Characteristics of Drug Users
In the present study, 5.4% of men and 8.4% of women received at least 1 psychotropic medication within the year before the survey. Other studies carried out in Europe4,5 have reported 1- or 2-week point prevalence estimates ranging from a low of 1.6% for men and 2.9% for women to a high of 9% and 18%, respectively. In the ESEMeD/MHEDEA 2000 study,10 12-month prevalence rates were 8.2% for men and 16% for women. Studies that also provided gender aggregated data3,4,6,9 reported prevalence rates of psychotropic drug use ranging from 6% to 15%.
For both genders, psychotropic drug use substantially increased with age, approaching the maximum in the oldest age group (70 years and older), in which nearly 23% of subjects had used any drugs in the past 12 months, with an OR of 15.9 in female favor. Use of psychotropic drugs was higher among the previously married versus married individuals and among unemployed, disabled, and retired people compared with those employed. The rates were also higher in subjects with lower schooling and among those living in an urban environment.
Most of our findings are consistent with data of the relevant literature on European countries. For example, gender and age differences, with females and older people reporting higher rates of psychotropic drug utilization, have consistently been pointed out in previous studies.10,16 Several plausible explanations have been suggested for gender differences in drug pattern use17,18: (1) higher psychiatric morbidity among women, particularly in relation to common mental disorders4,17,19; (2) a greater proneness of females than males to experience psychological distress, complain of psychological symptoms, and seek professional help20; and, conversely, (3) a greater proneness of males than females to alcohol use in stressful situations that interferes with psychotropic drug use.21
Likewise, each of the above reasons, alone or in combination, may help to explain the increased use of psychotropic drugs with age. Compared with younger individuals, older people demonstrate more subclinical depression syndromes and organic mood disorders leading to erroneously high prevalence rates of major depression,22,23 elevated levels of distress related to social isolation and loneliness,24 and a decline in the prevalence of alcohol and other substance use disorders with age.25 Factors reflecting social isolation have been shown to be associated with somatization and increased rates of medical utilization. A plausible explanation is that older persons turn to health care providers as an auxiliary social support system in times of stress.26
Our findings indirectly confirm previous studies on the variation in mood disorders between rural and urban areas.27 Overall, urbanicity seems to be linked to a higher risk of mental health disorders, particularly depressive disorders, whereas the link to anxiety disorders is only moderate, and there is no link at all to alcohol disorders.28 The lowest prevalence of psychotropic drug use in the West Bank inhabitants found in this study may be explained by their younger age, greater social cohesion, and ideological commitment to Israel, which enhance resilience to stress.29,30
Indicators of social exclusion (unmarried status, unemployment, low education) as factors known to be associated with lower social support and elevated levels of psychological distress31–33 were also correlated with higher drug utilization. Apart from this, lower prevalence of psychotropic medicine use found among more educated subjects and subjects with high occupation skills could be explained by their positive attitudes toward a healthy lifestyle, leisure time and occupational physical activity,34,35 prevention efforts rather than treatment of diseases, and, linked to these attitudes, the preference in the use of alternative/complementary medicines and interventions rather than pharmaceuticals.36,37
Among variables most specific for Israel, immigration status and religious affiliation need to be considered. Regarding the first factor, we found that compared with native-born Israelis, the prevalence of psychotropic medicine utilization was higher among immigrants from the former Soviet Union, while newcomers from other countries have been placed in between. These findings could be explained by differences in adjustment efforts and related psychological distress between immigrants from different countries to Israel. As a rule, immigrants from the former Soviet Union must do their utmost to preserve or restore their former social and professional status in the host country,38 while professional adjustment of newcomers from Western Europe and the United States occurs meaningfully easier, sometimes almost automatically.39 Restoration of former social and professional statuses is not required from Ethiopian immigrants at all.40,41
Regarding the factor of religious affiliation, we found that the prevalence of psychotropic drug use was substantially higher among secular people or individuals identifying themselves as belonging to traditional Jewish religion compared with those of Orthodox Jewish communities. There are at least 2 reasons for explaining this difference: (1) both social cohesion and social support in the ultra-orthodox communities enable resilience to psychological stress,42 and (2) negative (stigmatizing) attitudes toward mental disorders and treatment are expressed and mental health service utilization is lowered among these communities.43,44 These reasons fit also to explain lower psychotropic drug use among Arabs45,46 and, probably, other religious minorities in Israel.47,48
Use Patterns in Different Countries
Since our survey is part of the World Mental Health (WMH) survey, comparisons with results from other countries are accessible. The overall prevalence rate of psychotropic drug use in Israel (6.9%) falls in between the 2 lowest estimates among European countries surveyed: Germany (5.9%) and the Netherlands (7.4%), whereas the highest rate was shown in France (19.2%).10 Among others, one possible explanation for the observed diversity is differences in prevalence rates of common mental disorders in these countries. However, when prevalence estimates of mood disorders are compared across countries, this explanation seems to be inconsistent. While both prevalence rates (of mood disorders and drug utilization) are similarly low in Germany (3.8% and 5.9%, respectively), the obvious discrepancy between the 2 occurs in France (3.6% vs. 19.2%).10 In Israel, both rates are almost equal in magnitude (6.4% and 6.9%). In other words, there may be other factors, e.g., administrative or legal rules influencing prescription practices of psychotropic drugs and utilization of mental health services. Therefore, additional analyses are needed to understand the reasons for the between-country differences in the utilization of psychotropic drugs in the general population.
Patterns of Drug Use
In consistence with other studies, anxiolytic drugs were the most often used, with 3.2% of subjects reporting use of one of these drugs in the year preceding the survey, with higher usage among women. Hypnotics (2.3%) and antidepressants (2.0%) had been used less often; mood stabilizers (0.8%) and antipsychotics (0.5%) were used only minimally. The latter finding reflects, perhaps, the fact that psychiatric services in Israel were traditionally adjusted to needs patients with chronic, severe mental disorders, and only 2% of individuals in the general population use these services.49 All of these findings are consistent with data of previous surveys.6,50,51
Use of Psychotropic Drugs Among People With Mental Disorders
Nearly one fifth of individuals fulfilling DSM-IV criteria for a 12-month diagnosis of any mental disorder reported using any psychotropic drug during the same period. The corresponding figures for subjects diagnosed with pure anxiety disorder, any mood disorder, pure major depression, and pure mood disorder were very similar, ranging from 18.6% to 21.3%. All of these figures are substantially less than those reported in the ESEMed survey (25.5%–45.6%).10
Limitations and Strengths
The first limitation is that we do not analyze data on nonmedication treatment of psychiatric disorders. The fact that the vast majority of our respondents (75%–80%) who were diagnosed as having a common mental disorder reported not receiving psychotropic treatment in the same time period suggests that some could be treated with psychotherapy or alternative/complimentary treatment devices. Given that a cognitive-behavioral therapy of common mental disorders is no less popular among patients and physicians than pharmacotherapy,52,53 it may be suggested that the extent of undertreatment is less than reported here.
Another limitation of the study is that we describe any drug and any dose taken during the previous year and we do not measure duration of medication treatment; hence, we cannot evaluate the appropriateness of treatment receiving for each of the specific psychiatric disorders. Further analyses we intend to conduct will evaluate these parameters of the study.
There are also methodological strengths of the study: (1) a relatively high response rate was achieved, (2) the interviews using the mother tongue (Hebrew, Arabic, and Russian) enabled the vast majority of the respondents to better understand the questions, (3) the interviews using computerized programs increased data quality by drastically reducing between-interviewer variation, and (4) the INHS as part of the WHO/WMH survey allowed an opportunity for cross-countries comparisons.
In conclusion, the INHS results suggest that the majority of individuals diagnosed with an identifiable, common mental disorder are not being treated with psychotropic drugs or are being inappropriately treated.
Drug names: buspirone (BuSpar and others), carbamazepine (Carbatrol, Equetro, and others), clozapine (Clozaril, FazaClo, and others), gabapentin (Neurontin and others), lamotrigine (Lamictal and others), lithium (Eskalith, Lithobid, and others), olanzapine (Zyprexa), quetiapine (Seroquel), risperidone (Risperdal), topiramate (Topamax and others), ziprasidone (Geodon).
Acknowledgments
We also thank Irena Radomislensky (Mental Health Services, Ministry of Health, Jerusalem, Israel) for her statistical assistance.
The Israel National Health Survey was carried out in conjunction with the World Health Organization/World Mental Health (WMH) Survey Initiative. We thank the staff of the WMH Data Collection and Data Analysis Coordination Centers for assistance with instrumentation, fieldwork, and consultation on data analysis. These activities were supported by the National Institute of Mental Health (R01-MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the U.S. Public Health Service (R13-MH066849, R01-MH069864, and R01-DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly, Ortho-McNeil, GlaxoSmithKline, and Bristol-Myers Squibb. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/.
Disclaimer: The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations or of the Israeli government.
Footnotes
The Israel National Health Survey was funded by the Ministry of Health, Jerusalem, Israel, with additional support from the Israel National Institute for Health Policy and Health Services Research and the National Insurance Institute of Israel.
Acknowledgment, additional support, and disclaimer appear at the end of the article.
Dr. Weizman has participated in speakers/advisory boards for Pfizer and Lilly. Drs. Grinshpoon and Ponizovsky and Mr. Marom report no additional financial or other relationships relevant to the subject of this article. All other acknowledged individuals report no conflict of interest.
REFERENCES
- Begaud B. Dictionary of Pharmacoepidemiology. Chichester, England: John Wiley & Sons. 2000 [Google Scholar]
- Verdoux H, Begaud B. Pharmacoepidemiology: what do (and don't) we know about utilisation and impact of psychotropic medications in real-life conditions? Br J Psychiatry. 2004;185:93–94. doi: 10.1192/bjp.185.2.93. [DOI] [PubMed] [Google Scholar]
- Cans C, Rotily M. Consumption of psychotropic drugs in the general population in the Isere District. Rev Epidemiol Sante Publique. 1991;39:515–522. [PubMed] [Google Scholar]
- Weyerer S, Dilling H. Psychiatric and physical illness, sociodemographic characteristics, and the use of psychotropic drugs in the community: results from the Upper Bavarian Field Study. J Clin Epidemiol. 1991;44:303–311. doi: 10.1016/0895-4356(91)90042-8. [DOI] [PubMed] [Google Scholar]
- Pariente P, Lepine JP, Lellouch J. Self-reported psychotropic drug use and associated factors in a French community sample. Psychol Med. 1992;22:181–190. doi: 10.1017/s0033291700032839. [DOI] [PubMed] [Google Scholar]
- Turrina C, Zimmermann-Tansella C, and Micciolo R. et al. A community survey of psychotropic drug consumption in South Verona: prevalence and associated variables. Soc Psychiatry Psychiatr Epidemiol. 1993 28:40–44. [DOI] [PubMed] [Google Scholar]
- Brugha TS, Bebbington PE, and Singleton N. et al. Trends in service use and treatment for mental disorders in adults throughout Great Britain. Br J Psychiatry. 2004 185:378–384. [DOI] [PubMed] [Google Scholar]
- Colman I, Wadsworth ME, and Croudace TJ. et al. Three decades of antidepressant, anxiolytic and hypnotic use in a national population birth cohort. Br J Psychiatry. 2006 189:156–160. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Lader MH. Use of psychotropic medication in the general population of France, Germany, Italy, and the United Kingdom. J Clin Psychiatry. 2002;63:817–825. doi: 10.4088/jcp.v63n0912. [DOI] [PubMed] [Google Scholar]
- Alonso J, Angermeyer MC, and Bernert S. et al. the ESEMed/MHEDEA 2000 Investigators, European Study of the Epidemiology of Mental Disorders. Psychotropic drug utilization in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004 55–64. [DOI] [PubMed] [Google Scholar]
- Levav I, Kohn R, and Dorenwend BP. et al. An epidemiological study of mental disorders in the ten-year cohort of young adults in Israel. Psychol Med. 1993 23:691–707. [DOI] [PubMed] [Google Scholar]
- Lerner Y. Psychiatric epidemiology in Israel. Isr J Psychiatry Relat Sci. 1992;29:218–228. [PubMed] [Google Scholar]
- Aviram U, Zilber N, and Lerner Y. et al. Chronically mentally ill persons in Israel: estimations of their number and characteristics. Social Security. 1998 53:92–105. [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC Classification and DDD Assignment. Oslo, Norway: WHO Collaborating Centre for Drug Statistics Methodology. 2006 [Google Scholar]
- Isacson D, Haglund B. Psychotropic drug use in a Swedish community: the importance of demographic and socioeconomic factors. Soc Sci Med. 1988;26:477–483. doi: 10.1016/0277-9536(88)90317-6. [DOI] [PubMed] [Google Scholar]
- Hohmann AA. Gender bias in psychotropic drug prescribing in primary care. Med Care. 1989;27:478–490. doi: 10.1097/00005650-198905000-00004. [DOI] [PubMed] [Google Scholar]
- Ashton H. Psychotropic-drug prescribing for women. Br J Psychiatry Suppl. 1991;10:30–35. [PubMed] [Google Scholar]
- Weich S, Sloggett A, Lewis G. Social roles and gender difference in the prevalence of common mental disorders. Br J Psychiatry. 1998;173:489–493. doi: 10.1192/bjp.173.6.489. [DOI] [PubMed] [Google Scholar]
- Levav I, Gilboa S, Ruiz F. Demoralization and gender differences in a kibbutz. Psychol Med. 1991;21:1019–1028. doi: 10.1017/s0033291700030014. [DOI] [PubMed] [Google Scholar]
- Mellinger GD, Balter MB, Manheimer DI. Patterns of psychotherapeutic drug use among adults in San Francisco. Arch Gen Psychiatry. 1971;25:385–394. doi: 10.1001/archpsyc.1971.01750170001001. [DOI] [PubMed] [Google Scholar]
- Schneider G, Kruse A, and Nehen HG. et al. The prevalence and differential diagnosis of subclinical depressive syndromes in inpatients 60 years and older. Psychother Psychosom. 2000 69:251–260. [DOI] [PubMed] [Google Scholar]
- Rauch SA, Morales KH, and Zubritsky C. et al. Posttraumatic stress, depression, and health among older adults in primary care. Am J Geriatr Psychiatry. 2006 14:316–324. [DOI] [PubMed] [Google Scholar]
- Osborn DP, Fletcher AE, and Smeeth L. et al. Factors associated with depression in a representative sample of 14,217 people aged 75 and over in the United Kingdom: results from the MRC trial of assessment and management of older people in the community. Int J Geriatr Psychiatry. 2003 18:623–630. [DOI] [PubMed] [Google Scholar]
- Lynskey MT, Day C, Hall W. Alcohol and other drug use disorders among older-aged people. Drug Alcohol Rev. 2003;22:125–133. doi: 10.1080/09595230100100552. [DOI] [PubMed] [Google Scholar]
- Fink P. Psychiatric illness in patients with persistent somatisation. Br J Psychiatry. 1995;166:93–99. doi: 10.1192/bjp.166.1.93. [DOI] [PubMed] [Google Scholar]
- Sundquist K, Frank G, Sundquist J. Urbanisation and incidence of psychosis and depression: follow-up study of 4.4 million women and men in Sweden. Br J Psychiatry. 2004;184:293–298. doi: 10.1192/bjp.184.4.293. [DOI] [PubMed] [Google Scholar]
- Kovess-Masfety V, Alonso J, and de Graaf R. et al. A European approach to rural-urban differences in mental health: the ESEMeD 2000 comparative study. Can J Psychiatry. 2005 50:926–936. [DOI] [PubMed] [Google Scholar]
- Kaplan Z, Matar MA, and Kamin R. et al. Stress-related responses after 3 years of exposure to terror in Israel: are ideological-religious factors associated with resilience? J Clin Psychiatry. 2005 66:1146–1154. [DOI] [PubMed] [Google Scholar]
- Shalev AY, Tuval R, and Frenkiel-Fishman S. et al. Psychological responses to continuous terror: a study of two communities in Israel. Am J Psychiatry. 2006 163:667–673. [DOI] [PubMed] [Google Scholar]
- Bjarnason T, Sigurdardottir TJ. Psychological distress during unemployment and beyond: social support and material deprivation among youth in six northern European countries. Soc Sci Med. 2003;56:973–985. doi: 10.1016/s0277-9536(02)00109-0. [DOI] [PubMed] [Google Scholar]
- Fryer D, Fagan R. Toward a critical community psychological perspective on unemployment and mental health research. Am J Community Psychol. 2003;32:89–96. doi: 10.1023/a:1025698924304. [DOI] [PubMed] [Google Scholar]
- Bleich A, Gelkopf M, and Melamed Y. et al. Mental health and resiliency following 44 months of terrorism: a survey of an Israeli national representative sample. BMC Med. 2006 4:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barengo NC, Hu G, and Lakka TA. et al. Low physical activity as a predictor for total and cardiovascular disease mortality in middle-aged men and women in Finland. Eur Heart J. 2004 25:2204–2211. [DOI] [PubMed] [Google Scholar]
- Pitsavos C, Panagiotakos DB, and Lentzas Y. et al. Epidemiology of leisure-time physical activity in sociodemographic, lifestyle and psychological characteristics of men and women in Greece: the ATTICA Study. BMC Public Health. 2005 5:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Outram S, Mishra GD, Schofield MJ. Sociodemographic and health related factors associated with poor mental health in midlife Australian women. Women Health. 2004;39:97–115. doi: 10.1300/J013v39n04_06. [DOI] [PubMed] [Google Scholar]
- Upchurch DM, Chyu L. Use of complementary and alternative medicine among American women. Womens Health Issues. 2005;15:5–13. doi: 10.1016/j.whi.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Ponizovsky A, Ginath Y, and Factourovich A. et al. The impact of professional adjustment on the psychological distress of immigrant physicians. Stress Med. 1996 12:247–251. [Google Scholar]
- Hasin D, Rahav G, and Meydan J. et al. The drinking of earlier and more recent Russian immigrants to Israel: comparison to other Israelis. J Subst Abuse. 1998 10:341–353. [DOI] [PubMed] [Google Scholar]
- Ponizovsky A, Ginath Y, and Durst R. et al. Psychological distress among Ethiopian and Russian Jewish immigrants to Israel: a cross-cultural study. Int J Soc Psychiatry. 1998 44:35–45. [DOI] [PubMed] [Google Scholar]
- BenEzer G. Group counseling and psychotherapy across the cultural divide: the case of Ethiopian Jewish immigrants in Israel. Transcult Psychiatry. 2006;43:205–234. doi: 10.1177/1363461506064849. [DOI] [PubMed] [Google Scholar]
- Goodman Y, Witztum E. Cross-cultural encounters between careproviders: rabbis' referral letters to a psychiatric clinic in Israel. Soc Sci Med. 2002;55:1309–1323. doi: 10.1016/s0277-9536(01)00278-7. [DOI] [PubMed] [Google Scholar]
- Cinnirella M, Loewenthal KM. Religious and ethnic group influences on beliefs about mental illness: a qualitative interview study. Br J Med Psychol. 1999;72:505–524. doi: 10.1348/000711299160202. [DOI] [PubMed] [Google Scholar]
- Feinberg SS. Issues in the psychopharmacologic assessment and treatment of the orthodox Jewish patient. CNS Spectr. 2005;10:954–965. doi: 10.1017/s109285290001052x. [DOI] [PubMed] [Google Scholar]
- Al-Krenawi A, Graham JR, and Dean YZ. et al. Cross-national study of attitudes towards seeking professional help: Jordan, United Arab Emirates (UAE) and Arabs in Israel. Int J Soc Psychiatry. 2004 50:102–114. [DOI] [PubMed] [Google Scholar]
- El-Islam MF. Some cultural aspects of the Arab patient-doctor relationship. Int Psychiatry. 2005;7:18–20. [PMC free article] [PubMed] [Google Scholar]
- Daie N, Witztum E, and Mark M. et al. The belief in the transmigration of souls: psychotherapy of a Druze patient with severe anxiety reaction. Br J Med Psychol. 1992 65:119–130. [DOI] [PubMed] [Google Scholar]
- Iancu I, Spivak B, and Mester R. et al. Belief in transmigration of the soul and psychopathology in Israeli Druze: a culture-sensitive psychotherapeutic approach. Psychopathology. 1998 31:52–58. [DOI] [PubMed] [Google Scholar]
- Levav I, Grinshpoon A. Mental health services in Israel. Int Psychiatry. 2004;4:10–14. [PMC free article] [PubMed] [Google Scholar]
- Pakesch G, Loimer N, and Rasinger E. et al. The prevalence of psychoactive drug intake in a metropolitan population. Pharmacopsychiatry. 1989 22:61–65. [DOI] [PubMed] [Google Scholar]
- Del Rio MC, Prada C, Alvarez FJ. The use of medication and alcohol among the Spanish population. Br J Clin Pharmacol. 1996;41:253–255. doi: 10.1111/j.1365-2125.1996.tb00193.x. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus SC, and Druss B. et al. National trends in the outpatient treatment of depression. JAMA. 2002 287:203–209. [DOI] [PubMed] [Google Scholar]
- Bebbington P, Brugha T, and Meltzer H. et al. Neurotic disorders and the receipt of psychiatric treatment. Int Rev Psychiatry. 2003 15:108–114. [DOI] [PubMed] [Google Scholar]