Abstract
Resilience may be an important component of prevention of neuropsychiatric disease. Resilience has proven to be quantifiable by scales such as the Connor-Davidson Resilience Scale (CD-RISC). Here, we introduce a 2-item version of this scale, the CD-RISC2. We hypothesize that this shortened version of the scale has internal consistency, test-retest reliability, convergent validity, and divergent validity as well as significant correlation with the full scale. Additionally, we hypothesize that the CD-RISC2 can be used to assess pharmacological modification of resilience. We test these hypotheses by utilizing data from treatment trials of post-traumatic stress disorder, major depression, and generalized anxiety disorder with setraline, mirtazapine, fluoxetine, paroxetine, venlafaxine XR, and kava as well as data from the general population, psychiatric outpatients, and family medicine clinic patients.
Keywords: Anxiety, treatment, hardiness
1. INTRODUCTION
The concept of resilience can be defined as the personal qualities that enable one to thrive in the face of adversity (Connor and Davidson, 2003). Resilience may also be viewed as a measure of successful stress-coping ability (Connor and Davidson, 2003). Resilience and related concepts such as ‘hardiness’ (Maddi and Khoshaba, 1994) have been noted to be an index of mental health (Maddi and Khoshaba, 1994, Ramaniah et al., 1999); in particular, hardiness and resilience have been shown to contribute to protection against developing chronic post-traumatic stress disorder (PTSD) after combat (King et al., 1998; Waysman et al., 2001). Indeed, increased resilience may be associated with improvements in both physical and mental health (Connor et al., 2003).
There is increasing evidence that the concept of resilience has biological validity. Indeed, resilience may be marked by high measures of dehydroepiandrosterone (DHEA), neuropeptide Y, galanin, and testerosterone, as well as increased 5-HT1A receptor and benzodiazepine receptor function (Charney, 2004). There is also a possible genetic correlation to resilience: the T.7 haplotype of the DRD4 dopamine gene may be correlated with decreased resilience (Gervai et al., 2005) as is also believed to be the case for a polymorphism of the serotonin transporter gene (Caspi et al., 2003).
There is also increasing evidence that childhood trauma can be associated with development of neuropsychiatric diseases such as PTSD and major depression later in life (Heim and Nemeroff, 2002). As such, understanding resilience may prove to be critical in developing preventative treatments for a wide assortment of neuropsychiatric disease, with a subsequent decrease in physical and economic burden on society.
As the concept of resilience proves to be increasingly important, the need to have valid scales to measure this quality becomes all the more important. We have introduced the Connor-Davidson Resilience Scale (CD-RISC) previously (Connor and Davidson, 2003). Here, we introduce an abbreviated form of this self-report scale consisting of two items (the CD-RISC2). A shortened version may be beneficial because of decreased time needed to administer the scale and subsequent possible increased usage. We hypothesize that: (1) the CD-RISC2 shows adequate internal consistency, test-retest reliability, convergent validity, and divergent validity, as well as correlation with the CD-RISC and (2) the CD-RISC2 can be used to assess pharmacological modification of resilience. We test these hypotheses by analyzing data from treatment trials of PTSD, major depressive disorder, and generalized anxiety disorder (GAD) with sertraline, mirtazapine, fluoxetine, paroxetine, venlafaxine XR, and kava as well as data from the general population, a general psychiatric outpatient population, and a family medicine clinic population.
2. METHODS
Two items from the CD-RISC were used (the CD-RISC2), namely items 1 (“Able to adapt to change”) and 8 (“Tend to bounce back after illness or hardship”). These items were selected by the originators of the scale as etymologically capturing the essence of resilience, i.e., the ability to spring back and successfully adapt to change. Patients’ data were drawn from the following outpatient pharmacological trials: general population subjects chosen by random digit dialing who took part in a national survey of trauma (Group 1, n=458), outpatients in a family medicine clinic (Group 2, n=138), psychiatric outpatients in private practice (Group 3, n=42), assessment of paroxetine and venlafaxine XR (Group 4, n=43) on heart rate variability in depressed patients, patients in trials of kava for treatment of Generalized Anxiety Disorder (GAD) (Group 5, n=24), and patients in trials of sertraline, mirtazapine, and fluoxetine for PTSD, Group 6 (n=75 for sertraline, n=20 for mirtazapine, and n=44 for fluoxetine). All these samples have been described in more detail elsewhere (Connor and Davidson, 2003). Each study protocol was approved by the Duke University Medical Center Institutional Review Board, and all patients provided informed consent.
The data were analyzed with the following objectives: (1) to assess the reliability and validity of the scale and (2) to assess the extent to which the CD-RISC2 scores can change with clinical improvement with treatment and over time.
The reliability and validity of the scale were assessed as follows (based on the groups for which data were available for analysis). Test-retest reliability was examined in patients from Groups 5 and the mirtazapine and fluoxetine patients of Group 6 in whom no clinical change was noted between two consecutive visits with the computing of intraclass correlations (“no clinical change” was quantified as a 1 or 2 on the CGI-I scale). Convergent validity was assessed in the various groups by correlating the CD-RISC2 with measures of hardiness (Kobasa Hardiness Scale; Kobasa et al., 1979), perceived stress (Perceived Stress Scale; Cohen et al., 1983), stress vulnerability (Stress Vulnerability Scale; Sheehan et al., 1990), measures of disability (Sheehan Disability Scale; Sheehan et al., 1983) and social support (Sheehan Social Support Scale; Sheehan, 1990). The same analyses were utilized to assess for convergent validity in the original CD-RISC study and were found to be significantly correlated (Connor and Davidson, 2003). Indeed, aspects of the above scales were utilized in making the original CD-RISC (Connor and Davidson, 2003) and thus significant correlation of the CD-RISC2 with these scales would provide evidence of convergent validity. The two items of the CD-RISC2 were thought by the authors to reflect resilience and thus were felt to likely overlap similar concepts such as “hardiness,” “stress vulnerability,” and “perceived stress.” Finally, item and subtotal correlations between the CD-RISC2 and the remaining 23 CD-RISC items were also utilized to assess convergent validity.
Divergent validity was assessed by correlating CD-RISC2 scores with the Arizona Sexual Experience Scale (ASEX; McGahuey et al., 2000) in patients from Group 5 (kava for GAD), as was done in the initial CD-RISC report (Connor and Davidson, 2003). Of note, nonparametric tests were used (Kruskal-Wallis Chi Square, Spearman correlation coefficient) throughout the various analyses because the data set was not normally distributed and nonparametric tests are statistically more conservative. Additionally, to account for multiple comparisons, the method of Siegel and Castellan (Siegel and Castellan, 1988) was followed; the test used was weighted for the number of comparisons and the sample size, comparing the adjusted rank score difference to a critical rank score difference.
The baseline CD-RISC2 scores were compared between each group (pairwise comparisons across Groups 1 to 6). As resilience may be particularly relevant to PTSD, the CD-RISC2 scores of responders as defined by CGI-I scores of 1 or 2 were compared in PTSD trials to non-responder scores (3, 4, or 5 on CGI-I).
The effect size of the treatment compared to placebo with respect to change in CD-RISC2 score from baseline to final visit was calculated for the one randomized, double-blind, placebo-controlled treatment trial represented (mirtazapine vs. placebo for PTSD).
3. RESULTS
CD-RISC2 scores over all the groups (n=844) were not affected by demographic factors (age: Spearman correlation coefficient=0.01, P=0.72; race: Kruskal-Wallis Chi Square(1)=0.69, P=0.41; gender: Kruskal-Wallis Chi Square(1)=2.04, P=0.15) except for marital status (Kruskal-Wallis Chi Square(1)=6.65, P=0.01).
The intraclass correlation between Group 5 and the mirtazapine and fluoxetine patients of Group 6 was 86.5%, p<0.0001, suggesting good test-retest reliability. Of note, the time between consecutive visits was generally 1 week for the group of 33 patients, but could be variable as the Last Observation Carried Forward (LOCF) data was used. Convergent validity data is described below. When CD-RISC2 scores of Group 4 patients were compared to the Kobasa Hardiness Scale, the two measures had an r of 0.30, p=0.047. There was also a significant correlation between the same measures with the Group 5 patients (r=0.73, P<0.0001).
When the CD-RISC2 was compared to the Perceived Stress Scale (PSS) utilizing all the patients in the PTSD trials (Group 6), the correlation was again significant (r= −0.51, P<0.0001
The CD-RISC2 in Groups 5 and 6 correlated significantly (r= −0.61, P<0.0001) with the Sheehan Stress Vulnerability Scale (SVS). When compared with the general population (Group 1), the coefficient was −0.18 (P=0.0001). Item-subtotal correlations were significant for the CDRISC-2 as compared to the remaining 23 CD-RISC items (r=0.78, P<0.001). Further, the CDRISC-2 showed significant correlations with each individual item (ranging from r=0.27 to r=0.66). See Table 1 for details.
Table 1.
Correlation Between CD-RISC2 (Items 1 and 8 from the CD-RISC) and the Other 23 Items of the CD-RISC
| CD-RISC Item Number | R | P |
|---|---|---|
| 2 | 0.35 | <0.0001 |
| 3 | 0.27 | <0.0001 |
| 4 | 0.66 | <0.0001 |
| 5 | 0.65 | <0.0001 |
| 6 | 0.57 | <0.0001 |
| 7 | 0.54 | <0.0001 |
| 9 | 0.33 | <0.0001 |
| 10 | 0.46 | <0.0001 |
| 11 | 0.57 | <0.0001 |
| 12 | 0.54 | <0.0001 |
| 13 | 0.50 | <0.0001 |
| 14 | 0.56 | <0.0001 |
| 15 | 0.44 | <0.0001 |
| 16 | 0.54 | <0.0001 |
| 17 | 0.62 | <0.0001 |
| 18 | 0.49 | <0.0001 |
| 19 | 0.59 | <0.0001 |
| 20 | 0.33 | <0.0001 |
| 21 | 0.51 | <0.0001 |
| 22 | 0.56 | <0.0001 |
| 23 | 0.49 | <0.0001 |
| 24 | 0.51 | <0.0001 |
| 25 | 0.48 | <0.0001 |
In the assessment of divergent validity, CD-RISC2 scores did not correlate significantly with the ASEX in Group 4 (r=0.21, P=0.33).
There was a significant difference across patient populations when an omnibus comparison was done (Kruskal-Wallis Chi Square(5)=206.74, P<0.0001). Pair-wise comparisons were then made, compensating for multiple comparisons as per the method of Siegel and Castellan (Siegel and Castellan, 1988). PTSD trial patients had significantly decreased CD-RISC2 scores at baseline compared to the general population, family medicine clinic patients, and psychiatric outpatients (P<0.05 for all comparisons). Also, depressed patients had significantly lower CD-RISC2 scores than family medicine clinic patients and the general population (P<0.05); similar findings occurred with GAD patients compared to family medicine clinic patients and the general population. Psychiatric outpatients had significantly lower CD-RISC2 scores than the general population, and family medicine patients had lowered scores than the general population (P<0.05). However, CD-RISC2 scores did not significantly vary by diagnosis of depression, GAD, or PTSD (Kruskal-Wallis Chi Square(2)=1.45, P=0.48). See Figure 1 for mean CD-RISC2 scores across all groups.
Figure 1.
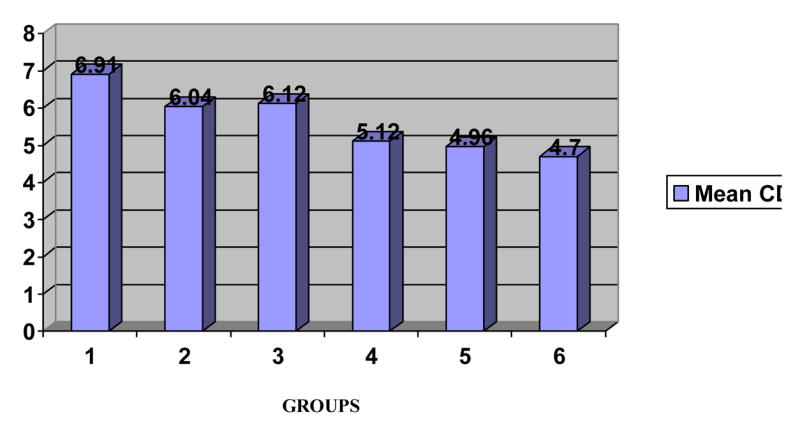
Mean CD-RISC2 scores at baseline across groups. (1=General population, 2=Family Medicine outpatients, 3=Psychiatric outpatients, 4=Depressed patients, 5=GAD patients, 6=PTSD patients)
There was a significant interaction between CD-RISC2 scores and CGI-I scores of 1 or 2 (responders) in PTSD trials (Wilcoxon Signed Rank Statistic=−64.5, P=0.018); that is, patients who improved (responded per CGI-I) also had improvement on CD-RISC2 scores. There was not a significant interaction between CD-RISC2 scores and CGI-I scores of 3, 4, or 5 (Wilcoxon Signed Rank Statistic=17.5, P=0.505), suggesting that patients who did not respond per CGI-I also did not significantly improve on the CD-RISC2.
In the the one double-blind, placebo-controlled trial in this data set, an effect size of 0.46 was found in favor of mirtazapine over placebo with respect to change in CD-RISC2 score from baseline to final visit.
4. DISCUSSION
Resilience has become an increasingly important concept to measure, as increased resilience may be related to neuropsychiatric disease prevention after exposure to environmental stressors. Resilience may be an important outcome measure in pharmacological trials of neuropsychiatric agents. We have shown previously with the development of the Connor-Davidson Resilience Scale (CD-RISC) that resilience is a quantifiable concept. Here, we have introduced the CD-RISC2, a 2-item version of the longer CD-RISC. Like its longer originator, the 2-item scale shows good test-retest reliability, convergent validity, and divergent validity. Further, the CD-RISC2 shows significant correlation with the overall CD-RISC score as well as with each item of the CD-RISC, suggesting that the 2 items of the CD-RISC2 are good representatives of the overall scale and the CD-RISC2 can be used in lieu of the CD-RISC.
PTSD patients had significantly lower baseline scores on the CD-RISC2 compared to the general population, family medicine clinic patients, and psychiatric outpatients. Relative to PTSD, the CD-RISC2 may have predictive utility as a screen for PTSD and is sensitive to response to PTSD treatment. Finally, resilience in PTSD (as measured by the CD-RISC2) seems to be differentially modulated by different pharmacological agents.
There are several possible applications of the CD-RISC2. It may useful either as a quick screen, or as a brief measure of resilience or progress after treatment. For research, the scale could be used as an outcome measure in treatment settings to measure effectiveness of contemporary resilience interventions, such as impacting cognitive schemas, home environment, parenting practices, and community resources (Mandleco and Peery, 2000). As discussed previously, resilience has become increasingly important to measure. For example, resilience may be related to sympathetic-parasympathetic balance (Bracha, 2004; Davidson et al., 2005). The scale could also be used in studies of the biology of resilience.
There are several limitations to this report. First, the CD-RISC2 items were chosen out of the full CD-RISC based on what items were thought to capture the essence of resilience, a subjective approach, rather than based on empirical criteria. Second, the CD-RISC2 assesses the characteristics of resilience, but does not assess the resiliency process or provide information about theories of resilience. Third, the scale has not been validated against an objective measure such as response to neuropeptide Y to extreme stress (Morgan et al., 2000), although the full scale has been shown to correspond to increased norepinephrine transporter inhibition associated with venlafaxine XR in a study of heart rate variability in depression (Davidson et al., 2005). Fourth, the study cannot allow making any firm conclusions regarding the effectiveness of various psychopharmacological agents in increasing resilience. Such conclusions must await the conduction of prospective trials with adequate power. Finally, the CD-RISC2 may be measuring a trait or it may be a proxy measure for symptom status. Because convergent validity analyses were done on symptomatic patients, it is possible that correlations between the CD-RISC2 and other measures were at least partly due to anxiety or depressive symptoms. Of note, however, there is data to support the notion that resilience can be affected by treatment (Davidson et al., 2006); in a randomized, double-blind, placebo-controlled study of venlafaxine XR in PTSD, PTSD symptoms improved first and it was not until much later that drug effects on resilience emerged, suggesting that resilience measures like the CD-RISC (which was used in the latter study) or the CD-RISC2 do not merely reflect symptom improvement.
In summary, the CD-RISC2 is a brief, self-rated measure of resilience with sound psychometric properties. This shortened scale may find greater applicability and usage in clinical settings, something which may become increasingly important in order to identify patients who may be vulnerable to development of neuropsychiatric disease.
Acknowledgments
We thank Rita Davison and Nabila Danish for help with data collection. We also thank Erik Churchill for help with statistical analysis.
Acknowledgement is made to the following organizations, who supported studies from which these data were obtained: National Institutes of Mental Heatlh, Organon, Pure World, Glaxo SmithKline and Pfizer.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andrews W, Parker G, Barrett E. The SSRI antidepressants: Exploring their “other” possible properties. Journal of Affective Disorders. 1988;49:141–144. doi: 10.1016/s0165-0327(97)00203-6. [DOI] [PubMed] [Google Scholar]
- Bracha HS. Can premorbid episodes of diminished vagal tone be detected via histological markers in patients with PTSD? International Journal of Psychophysiology. 2004;51:127–133. doi: 10.1016/j.ijpsycho.2003.08.003. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington HL, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Charney DS. Psychobiological mechanisms of resilience and vulnerability: Implications for successful adaptation to extreme stress. American Journal of Psychiatry. 2004;161:195–216. doi: 10.1176/appi.ajp.161.2.195. [DOI] [PubMed] [Google Scholar]
- Connor KM, Sutherland SM, Tupler LA, Churchill LE, Malik ML, Davidson JRT. Fluoxetine in posttraumatic stress disorder: A randomized, placebo-controlled Trial. British Journal of Psychiatry. 1999;175:17–22. doi: 10.1192/bjp.175.1.17. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JRT. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depression and Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Davidson JRT, Watkins L, Owens M, Krulewicz S, Connor K, Carpenter D, Krishnan R, Nemeroff C. Effects of paroxetine and venlafaxine XR on heart rate variability in depression. Journal of Clinical Psychopharmacology. 2005;25:480–484. doi: 10.1097/01.jcp.0000177547.28961.03. [DOI] [PubMed] [Google Scholar]
- Davidson JRT, Baldwin DS, Stein DJ, Kuper E, Benattia I, Ahmed S, Musgnung J. Treatment of posttraumatic stress disorder with venlafaxine extended release: a 6-month randomized controlled trial. Archives of General Psychiatry. 63(10):1158–1165. doi: 10.1001/archpsyc.63.10.1158. [DOI] [PubMed] [Google Scholar]
- Gervai J, Nemoda Z, Lakatos K, Ronai Z, Toth I, Ney K, Sasvari-Szekely M. Transmission disequilibrium tests confirm the link between DRD4 gene polymorphism and infant attachment. American Journal of Medical Genetics Part B (Neuropsychiatric Genetics) 2005;132B:126–130. doi: 10.1002/ajmg.b.30102. [DOI] [PubMed] [Google Scholar]
- Healey D, Healey H. The clinical pharmacologic profile of reboxetine: Does it involve the putative neurobiological substrates of wellbeing? Journal of Affective Disorders. 1996;51:313–322. doi: 10.1016/s0165-0327(98)00227-4. [DOI] [PubMed] [Google Scholar]
- Heim C, Nemeroff CB. Neurobiology of early life stress: Clinical studies. Seminars in Clinical Neuropsychiatry. 2002;7:147–159. doi: 10.1053/scnp.2002.33127. [DOI] [PubMed] [Google Scholar]
- King LA, King DW, Fairbank JA, Keane TM, Adams GA. Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: Hardiness, postwar social support, and additional stressful life events. Journal of Personality and Social Psychology. 1998;74:420–434. doi: 10.1037//0022-3514.74.2.420. [DOI] [PubMed] [Google Scholar]
- Maddi SR, Khoshaba DM. Hardiness and mental health. Journal of Personality Assessment. 1994;53:265–274. doi: 10.1207/s15327752jpa6302_6. [DOI] [PubMed] [Google Scholar]
- Mandleco BL, Peery JC. An organizational framework for conceptualizing resilience in children. Journal of Child and Adolescent Psychiatric Nursing. 2000;13:99–111. doi: 10.1111/j.1744-6171.2000.tb00086.x. [DOI] [PubMed] [Google Scholar]
- Morgan CA, Wang S, Southwick SM, Rasmusson A, Hazlett G, Hauger RL, Charney DS. Plasma neuropeptide-Y concentrations in humans exposed to military survival training. Biological Psychiatry. 2000;47:902–909. doi: 10.1016/s0006-3223(99)00239-5. [DOI] [PubMed] [Google Scholar]
- Ramaniah NV, Sharpe JP, Byravan A. Hardiness and major personality factors. Psychological Reports. 1999;84:497–500. doi: 10.2466/pr0.1999.84.2.497. [DOI] [PubMed] [Google Scholar]
- Siegel S, Castellan NJ. Nonparametric Statistics for the Behavioral Sciences. McGraw-Hill; New York: 1988. pp. 213–214. [Google Scholar]
- Waysman M, Schwarzwald J, Solomon Z. Hardiness: An examination of its relationship with positive and negative long-term changes following trauma. Journal of Traumatic Stress. 2001;14:531–548. doi: 10.1023/A:1011112723704. [DOI] [PubMed] [Google Scholar]


