Abstract
Objective
Compare occlusal contacts calculated from 3D virtual models created from clinical records to contacts identified clinically using shimstock and transillumination.
Methods
Upper and lower full arch alginate impressions and vinyl polysiloxane centric interocclusal records were made of 12 subjects. Stone casts made from the alginate impressions and the interocclusal records were optically scanned. Three-dimensional virtual models of the dental arches and interocclusal records were constructed using the Virtual Dental Patient Software©. Contacts calculated from the virtual interocclusal records and from the aligned upper and lower virtual arch models were compared to those identified clinically using 0.01 shimstock and transillumination of the interocclusal record. Virtual contacts and transillumination contacts were compared by anatomical region and by contacting tooth pairs to shimstock contacts. Because there is no accepted standard for identifying occlusal contacts, methods were compared in pairs with one labeled “standard” and the second labeled “test”. Accuracy was defined as the number of contacts and non-contacts of the “test” that were in agreement with the “standard” divided by the total number of contacts and non-contacts of the “standard”.
Results
Accuracy of occlusal contacts calculated from virtual interocclusal records and aligned virtual casts compared to transillumination were: 0.87±0.05 and 0.84±0.06 by region and 0.95±0.07 and 0.95±0.05 by tooth, respectively. Comparisons with shimstock were: 0.85±0.15 (Record), 0.84±0.14 (Casts), and 81 ± 17 (Transillumination).
Conclusions
The virtual record, aligned virtual arches, and transillumination methods of identifying contacts are equivalent, and show better agreement with each other than with the shimstock method.
Keywords: Occlusal Contacts, 3D scanning, Interocclusal Record, Transillumination
1. Introduction
The relationship between occlusion, mastication and dental disorders, is not well understood because of the lack of accurate, quantitative measures of occlusal parameters.1 To understand jaw function and its effects on biological tissues, dental materials, and dental reconstructions, it is imperative to know how chewing forces are distributed. The first step is quantitative identification of occlusal contacts. Thin foils or films, which are used universally in clinics for occlusal adjustment or analysis, are partially subjective measures.2 Contact information is limited to the width of the measuring media, requiring multiple jaw closures to gather contact information around the entire arch.3 Even when colored media are used to mark contacts, properties of the colorant may lead to false positive and negative markings.4-6 These factors make the foil method less than ideal for quantifying contacts in clinical studies.
Three systems provide quantitative measures of contact forces: Photoocclusion, T-Scan, and Dental Prescale System.7-11 Contact information from these systems is limited because their sensors could interfere with and alter occlusion, contacts are not directly related to occlusal anatomy, and the results are two-dimensional.12,13
Addition silicones are frequently used to record contacts because of their low viscosity, accuracy, and stability. The flow properties and uniform distribution of the materials across occlusal surfaces of teeth ensure minimal interference on closure. These properties make addition silicone an ideal material for identifying occlusal contacts; however, the problem of quantifying the information remains. One method, transillumination, converts the transparency of the record to digital data.2,14-21 Because silicones become translucent in relatively thick sections, occlusal surfaces separated by as much as 0.350 mm are considered to be in contact or “near” contact. 14, 16, 17 Transillumination is limited because the results are two-dimensional and depend on the orientation of the record to the light source.2
Another method for quantifying contacts involves digitizing the interocclusal record using a three-dimensional laser scanner while the record is seated on a mandibular cast.22 The record is removed (the cast position remains fixed) and the occlusal surface of the cast is scanned. The scans capture three-dimensional images of the maxillary and mandibular occlusal surfaces in the relationship defined by the interocclusal record. Occlusal contacts are regions of closest approach between the two virtual images. Estimated accuracy was 0.050 mm. This method provides quantitative, three-dimensional locations of occlusal contacts; however, its accuracy in reproducing clinical contacts is unknown.
One difficulty with the clinical application of the method proposed by Hayashi et al. is accurately reseating the interocclusal record on the cast. This can be avoided by either scanning both sides of the interocclusal record without reseating it on the cast, or by calculating contacts from 3D images of the casts that have been aligned to each other using the digital image of the interocclusal record.23 The purpose of this study was to determine the accuracy of these two 3D scanning methods in identifying occlusal contacts. Calculated contacts were compared to those identified clinically using shimstock and transillumination.
2. Methods and Materials
IRB approval was obtained for a cross sectional study with 12 subjects (6 Males, mean age: 41.5 yrs., range: 36-55 yrs.; 6 females, mean age: 40.2 yrs., range: 25-51 yrs.). Consent forms were signed by all participating subjects. Occlusal contacts were identified in maximum intercuspal position (MIP) using 0.01 mm shimstock (Almore International, Inc; Portland, OR). Fujirock (GC Europe, Leuven, Belgium) stone casts were made from alginate impressions of the upper and lower arches. Interocclusal records were made by expressing Exabite II NDS (GC America, Inc.) onto the occlusal surfaces of the teeth then having the subject close into the MIP. Prior to removing the MIP record, a full arch First Bite Disposable Impression Tray (Caulk/Densply International Inc; Milford, DE), which had the center gauze removed and perforations placed uniformly around the rim, was attached using additional impression material (Fig. 1A). The tray served as a support during the scanning process.
Fig. 1.
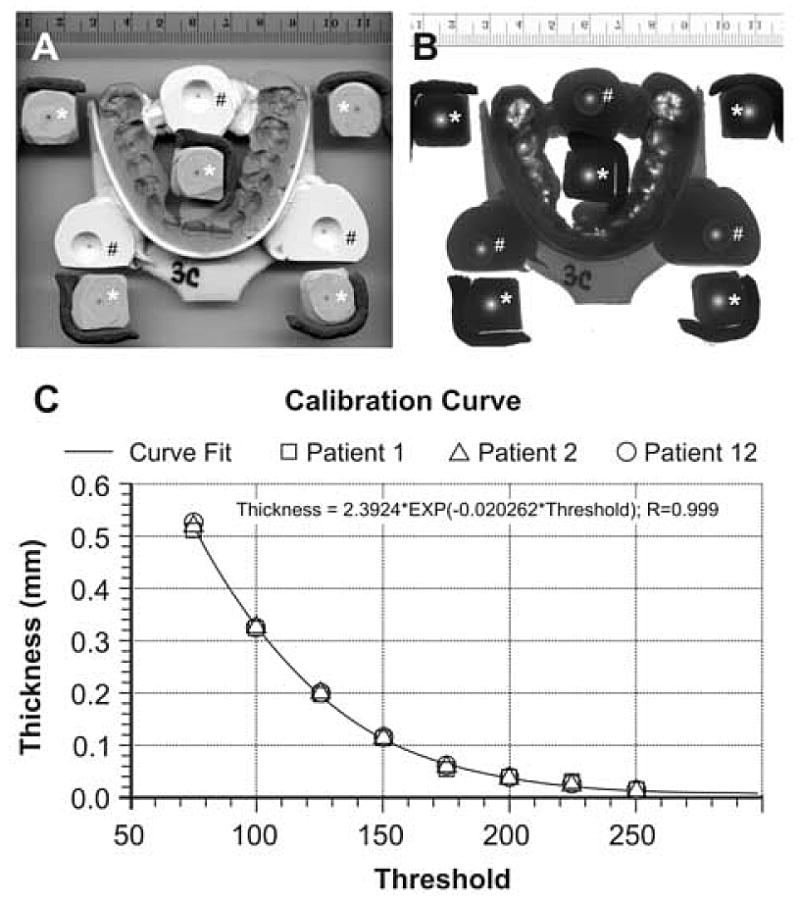
Calibration of transillumination brightness to impression material thickness. Images of a MIP record, impressions of 8 ball bearings in contact with a flat plane, and a scale scanned at 300 dpi in a Hewlett Packard ScanJet 5370C using reflective lighting (A) and the ScanJet XPA Transparency Light (B). Light regions on the transilluminated image (B) represent thin regions of the record. The five sphere-to-plane impressions with the plane side visible (*) provided calibration points for calculating record thickness. The three sphere-to-plane impressions with the sphere side visible (#) are reference points for maintaining alignment between the two sides of the record while constructing its 3D virtual image. The calibration curve for converting brightness to thickness (C) shows data for three subjects; however, all twelve were used in deriving the best fit calibration curve.
Casts and MIP records were scanned from multiple views (casts: 24 views; interocclusal records: 16 views) using a Comet 100 optical scanner (Steinbichler Optical Technologies, Germany). The Comet 100 has an XYZ measurement volume of 85 × 65 × 80 mm3, accuracy of 0.040 mm, and X, Y and Z precision of 0.130 mm, 0.130 mm, and 0.005 mm, respectively. Individual views were aligned to each other using PolyWorks (InnovMetric Software; Quebec, Canada). The aligned views were combined into a single data set representing the object (virtual model), rendered as 3D surfaces, and analyzed using the Virtual Dental Patient (VDP) software developed in the Minnesota Dental Research Center for Biomaterials and Biomechanics under NIH/NIDCR grant RO1 DE12225.
Upper and lower virtual casts were aligned in MIP using the virtual MIP record.23 Maxillary cusp indents of the virtual MIP record were aligned to the corresponding cusps of the maxillary virtual cast by minimizing distances between points representing the two virtual surfaces. After the virtual MIP record was aligned to the maxillary virtual cast, the cusps of the mandibular virtual cast were similarly aligned to their corresponding indents on the virtual record, which aligned the casts in MIP. Virtual occlusal contacts were calculated both for the articulated virtual casts (virtual cast contacts) and directly from the virtual MIP records (virtual record contacts) using the VDP software. Virtual contacts were regions on opposing virtual surfaces that were within 0.350 mm of each other. Opposing surfaces were the articulated occlusal surfaces of the upper and lower virtual casts for the virtual cast contacts and the opposite sides of the virtual MIP record for the virtual MIP record contacts.
MIP contacts were also identified by transillumination of the interocclusal record following the method proposed by Owens et al. (Fig.1).14 MIP records were scanned at 300 dpi with 8-bit grayscale in a Hewlett Packard ScanJet 5370C using the ScanJet XPA Transparency Light. Record calibration used five impressions of a ball bearing (radius: 4.761 mm) in contact with a flat plane. Calibration standards were made from the same impression material used for the MIP records. The calibration impressions and a millimeter scale were scanned with the MIP record (Fig. 1A). Scanned images were imported into Corel PhotoPaint® 10 (Corel Corporation; Ontario, Canada) and converted to black and white using the Threshold tool. Pixel values below the threshold were converted to black; the remaining pixels were converted to white. For ease of analysis, images were inverted. In this form, black regions represented contacts. A series of converted images was created for each scanned image using Threshold values from 25 to 250 in steps of 25. Converted images were imported into CorelDraw® 10 (Corel Corporation; Ontario, Canada) where a circle was drawn around, and the same size as, each of the five black regions representing the ball bearing contact with the plane. Knowing the diameter of the black region (D), the ball bearing radius (4.761 mm), and the length of the scale image, the maximum impression material thickness for the threshold value was calculated from the equation:
The equation defining the impression material thickness as a function of Threshold:
was derived by fitting the calibration data (Fig. 1C). A record thickness of 0.350 mm or less indicated a contact or “near contact”.
Occlusal contacts calculated from the virtual MIP records, the aligned upper and lower virtual casts, and transillumination were compared by anatomical region (Fig. 2) and by contacting tooth pairs to shimstock contacts. Because there is no accepted standard for identifying occlusal contacts, methods were compared in pairs with one labeled “standard” and the second labeled “test”. Accuracy was defined as the number of contacts and non-contacts of the “test” that were in agreement with the “standard” divided by the total number of contacts and non-contacts of the “standard”. For each standard, test methods' accuracies were compared using repeated measures ANOVA, with subjects as “subject”. Contacting tooth pairs and virtual contacts by anatomical regions were tested separately. If significant differences were found in the ANOVA (p < 0.05), post-hoc tests were done applying the Bonferroni correction for multiple comparisons (p < 0.05/3).
Fig. 2.
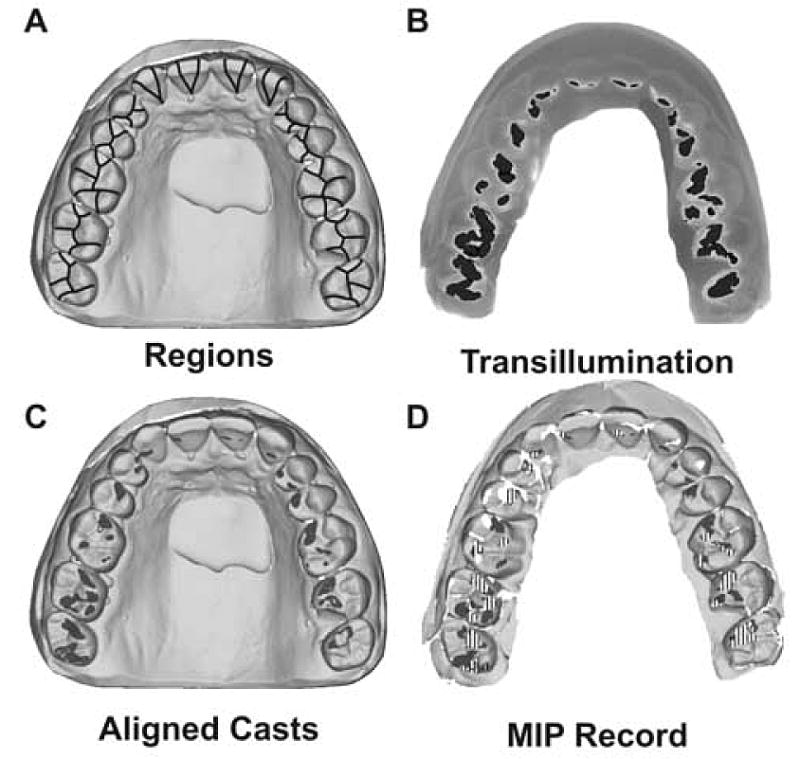
Relationship of transillumination, virtual MIP records, and aligned virtual casts' occlusal contacts to anatomically defined regions. Anatomical regions were used to qualitatively define the locations of the occlusal contacts following the method suggested by Plasmans et al. (A).24 A single contact crossing boundaries was counted in all regions in which it resided. Transillumination contacts (B), black areas, were regions where the MIP record thickness was 0.35 mm or less. Aligned virtual cast contacts (C), dark gray areas, were regions where the two virtual casts were separated by 0.35 mm or less. Virtual MIP record contacts (D), dark gray regions, were regions where the upper and lower sides of the virtual MIP record were within 0.35 mm of each other. White areas in the MIP virtual record represent portions of the record that could not be scanned. Regions where the teeth are in contact and the record was too thin to scan are indicated with vertical lines.
3. Results
Shimstock consistently identified fewer contacts than the other methods. The median contacts per subject were 11, 14, 14, and 14 for shimstock, transillumination, virtual casts, and virtual MIP records, respectively.
Using shimstock as the standard, accuracies were similar for comparisons between transillumination (p=1.0), virtual casts (p=0.61), and virtual interocclusal records (p=0.61), Table 1. When either shimstock or transillumination was the standard, the best agreement was virtual interocclusal record with aligned virtual casts. Comparisons with shimstock were not as good (p < 0.017 for all comparisons). The virtual interocclusal record had the best agreement with shimstock; while transillumination had the worst agreement.
Table 1.
Accuracy of the Four Methods for Identifying Occlusal Contacts (n = 12 subjects)
| Standard | Test* | Accuracy ± SD (%) | Standard Error (%) | Minimum (%) | Maximum (%) |
|---|---|---|---|---|---|
| Comparing tooth-to-tooth contacts | |||||
| Transillumination | Virtual Cast | 95 ± 5 | 2 | 86 | 100 |
| Virtual MIP record | 95 ± 7 | 2 | 79 | 100 | |
| Shimstock | 81 ± 17 | 5 | 50 | 100 | |
| Shimstock | Transillumination | 81 ± 17 | 5 | 50 | 100 |
| Virtual Cast | 84 ± 14 | 4 | 53 | 100 | |
| Virtual MIP record | 85 ± 15 | 4 | 47 | 100 | |
| Virtual Cast | Transillumination | 95 ± 5 | 2 | 86 | 100 |
| Virtual MIP record | 97 ± 4 | 1 | 93 | 100 | |
| Shimstock | 84 ± 14 | 4 | 53 | 100 | |
| Virtual MIP record | Transillumination | 95 ± 7 | 2 | 79 | 100 |
| Virtual Cast | 97 ± 4 | 1 | 93 | 100 | |
| Shimstock | 85 ± 15 | 4 | 47 | 100 | |
|
| |||||
| Comparing anatomical region contacts | |||||
| Transillumination | Virtual Cast | 84 ± 6 | 2 | 70 | 93 |
| Virtual MIP record | 87 ± 5 | 2 | 77 | 97 | |
| Virtual Cast | Transillumination | 84 ± 6 | 2 | 69 | 93 |
| Virtual MIP record | 90 ± 4 | 1 | 80 | 96 | |
| Virtual MIP record | Transillumination | 87 ± 6 | 2 | 77 | 97 |
| Virtual Cast | 91 ± 5 | 1 | 80 | 96 | |
Comparisons linked by vertical lines are not significantly different, p > 0.05/3
Accuracies for contacts compared by region were less than those found when comparing contacting opposing teeth, Table 1. Trends were the same as those found with the tooth-to-tooth comparisons. Again, the best agreement was the virtual interocclusal records with the aligned virtual casts; however, all three methods were similar, and were judged to be equivalent.
Agreement between shimstock and transillumination tooth-to-tooth contacts was less than expected. Therefore, comparisons were made with transillumination for threshold thicknesses of 0.050 mm and by optimizing the threshold thickness to provide the best agreement with the shimstock contacts, Table 2. Optimizing the threshold thickness provided an accuracy equivalent to those of the other methods. Average thickness for the optimized transillumination was 0.12 mm (SD: ±0.09 mm; Range: 0.017 mm – 0.349 mm). Median contacts were 12 for both 0.050 mm and optimized thicknesses. The average threshold thickness that just produced a contact was consistent for 11 of the 12 subjects (mean: 0.014 mm; SD: ± 0.002 mm; 0.097 for the 12th subject).
Table 2.
Shimstock and Transillumination Contact Comparison (n=12 subjects)
| Standard | Test | Threshold (mm) | Accuracy ± SD (%) | Standard Error (%) | Minimum (%) | Maximum (%) |
|---|---|---|---|---|---|---|
| Shimstock | Transillumination | 0.05 | 76 ± 23 | 7 | 13 | 93 |
| Transillumination | 0.35 | 81 ± 17 | 5 | 50 | 100 | |
| Transillumination | Variable | 94 ± 5 | 1 | 86 | 100 |
4. Discussion
The objective of this study was to measure the accuracy of two 3D quantitative methods for identifying occlusal contacts. Measuring accuracy requires comparing the test results to a gold standard. Unfortunately, there is no universally accepted gold standard for identifying occlusal contacts clinically. Shimstock is often accepted as the standard; however, it has severe limitations. Interocclusal records, which capture all the required contact information, are likewise limited because there is no accepted method for extracting the contacts. Therefore, both methods were used as the gold standard for clinical contacts.
The fact that shimstock and transillumination of the interocclusal record found similar contacts only 81% of the time demonstrates the gold standard problem. Transillumination consistently found more contacts. This is expected because tooth separations of up to 0.35 mm were considered to be in contact with the transillumination method; whereas, with shimstock, tooth separations were limited to 0.01 mm. Reducing the allowable tooth separation to 0.05 mm for the transillumination contacts did not improve the agreement with shimstock. Varying the allowable separation on a subject by subject basis improved the agreement between shimstock and transillumination (94%); however, contact-defining separations varied from 0.017 mm to 0.349 mm. This variation could not be explained by differences in biting forces between subjects because the minimal record thickness that just produced a contact was consistent in 11 of the 12 subjects, and was only marginally greater than the thickness of shimstock (0.014 mm vs. 0.010 mm). Therefore, the increased allowable tooth separation used to identify contacts on the MIP record does not fully explain the differences in the two methods.
These findings imply that there is a fundamental difference between measuring contacts individually with shimstock and simultaneously with the impression material. With the interocclusal record method, one is reasonably assured that all contacts were measured with the same total bite force and with the upper and lower jaws in the same occlusal relationship. The same is not true for the shimstock method, which requires multiple jaw closures to identify contacts around the arch. Therefore, the interocclusal method of identifying contacts is the preferred standard for clinical studies with outcomes dependent on occlusal contact locations.
Accuracy of the virtual interocclusal record (95%) and virtual cast (95%) methods of identifying contacting teeth was very good when transillumination was used as the standard, and was similar to, but better than, transillumination when shimstock was the standard. Comparing the more detailed regional contact information versus transillumination decreased the accuracy (Interocclusal record: 87%; Virtual cast: 84%). The fact that the agreement between the virtual MIP record and the virtual cast (91%) was better than their agreement with the transillumination contacts may be a consequence of comparing two-dimensional transillumination with three-dimensional virtual models. Contacts in the transillumination method are determined from a single direction whereas the three-dimensional models measure thickness normal to the surface.
The advantage of the two computer methods (interocclusal record and casts) for identifying contacts is that they are three-dimensional and quantitative. Once a contact is identified, the area, location, and orientation of the contact can be calculated and displayed on the three-dimensional tooth surface for evaluation. The advantage of the cast method over the interocclusal record method is that one does not have to worry about the effects of scanning holes and translucent regions in the record that occur where the teeth contact. The disadvantage of the cast method is that full arch impressions are made with the teeth out of contact. Therefore, movements caused by interactions between the teeth when they are in contact are not recorded, as they are with the interocclusal record method. This may account for differences between the contacts calculated with the MIP and cast virtual models. A possible solution is to use a dual-arch tray to capture the upper and lower occlusal anatomy and the MIP simultaneously. This will reduce the effects of holes and translucent regions and account for tooth movement. This concept is currently under investigation.
5. Conclusions
It is unrealistic to expect shimstock and transillumination to provide similar occlusal contacts because the methods are fundamentally different.
Transillumination, virtual MIP record, and virtual cast methods provide similar contact results.
The virtual interocclusal record and virtual cast methods provide accurate, quantitative measures of occlusal contacts when transillumination contacts are the gold standard.
Acknowledgments
This study was supported in part by USPHS Research Grant R01 DE-12225-05 from the National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD 20892, the Minnesota Dental Research Center for Biomaterials and Biomechanics, and 3M/ESPE.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
S. Knorr, Minnesota Dental Research Center for Biomaterials and Biomechanics, Department of Restorative Sciences, University of Minnesota School of Dentistry
G.C. Anderson, Department of Developmental and Surgical Sciences, University of Minnesota School of Dentistry
J. Hodges, Division of Biostatistics and Oral Health Clinical Research Center, Department of Oral Sciences, University of Minnesota School of Dentistry
M.R. Pintado, Minnesota Dental Research Center for Biomaterials and Biomechanics, Department of Restorative Sciences, University of Minnesota School of Dentistry nesota
References
- 1.Ogawa T, Ogimoto T, Koyano K. Validity of the examination method of occlusal contact pattern relating to mandibular position. Journal of Dentistry. 2000;28:23–9. doi: 10.1016/s0300-5712(99)00045-7. [DOI] [PubMed] [Google Scholar]
- 2.Gurdsapsri W, Ai M, Baba K, Fueki K. Influence of clenching level on intercuspal contact area in various regions of the dental arch. Journal of Oral Rehabilitation. 2000;27:239–44. doi: 10.1046/j.1365-2842.2000.00527.x. [DOI] [PubMed] [Google Scholar]
- 3.McDevitt WE, Wareth AA. Occlusal contacts in maximum intercuspation in normal dentitions. Journal of Oral Rehabilitation. 1997;24:725–34. doi: 10.1046/j.1365-2842.1997.00596.x. [DOI] [PubMed] [Google Scholar]
- 4.Halperin GC, Halperin AR, Norling BK. Thickness, strength, and plastic deformation of occlusal registration strips. Journal of Prosthetic Dentistry. 1982;48:575–8. doi: 10.1016/0022-3913(82)90367-5. [DOI] [PubMed] [Google Scholar]
- 5.Gazit E, Fitzig S, Lieberman MA. Reproducibility of occlusal marking techniques. Journal of Prosthetic Dentistry. 1986;55:505–9. doi: 10.1016/0022-3913(86)90188-5. [DOI] [PubMed] [Google Scholar]
- 6.Millstein PL, Maya A. An evaluation of occlusal contact marking indicators. Journal of American Dental Association. 2001;132:1280–6. doi: 10.14219/jada.archive.2001.0373. [DOI] [PubMed] [Google Scholar]
- 7.Dawson PE, Arcan M. Attaining harmonic occlusion through visualized strain analysis. Journal of Prosthetic Dentistry. 1981;46:615–622. doi: 10.1016/0022-3913(81)90067-6. [DOI] [PubMed] [Google Scholar]
- 8.Arcan M, Zandman F. A method for in vivo quantitative occlusal strain and stress analysis. Journal of Biomechanics. 1984;17:67–79. doi: 10.1016/0021-9290(84)90125-8. [DOI] [PubMed] [Google Scholar]
- 9.Maness WL, Benjamin M, Podoloff R, Bobbick A, Golden RF. Computerized occlusal analysis: A new technology. Quintessence International. 1987;4:287–92. [PubMed] [Google Scholar]
- 10.Matsui Y, Ohno K, Michi K, Suzuki Y, Yamagata K. A computerized method for evaluating balance of occlusal load. Journal of Oral Rehabilitation. 1996;23:530–5. doi: 10.1111/j.1365-2842.1996.tb00891.x. [DOI] [PubMed] [Google Scholar]
- 11.Suzuki T, Kumangai H, Watanabe T, Uchida T, Nagao M. Evaluation of complete denture occlusal contacts using pressure-sensitive sheets. International Journal of Prosthodontics. 1997;10:386–91. [PubMed] [Google Scholar]
- 12.Hidaka O, Iwasaki M, Saito M, Morimoto T. Influence of clenching intensity on bite force balance, occlusal contact area, and average bite pressure. Journal of Dental Research. 1999;78:1336–44. doi: 10.1177/00220345990780070801. [DOI] [PubMed] [Google Scholar]
- 13.Kumagai H, Suzuki T, Hamada T, Sondang P, Fuitani M, Nikawa H. Occlusal force distribution on the dental arch during various levels of clenching. Journal of Oral Rehabilitation. 1999;26:932–5. doi: 10.1046/j.1365-2842.1999.00473.x. [DOI] [PubMed] [Google Scholar]
- 14.Owens S, Buschang PH, Throckmorton GS, Palmer L, English J. Masticatory performance and areas of occlusal contact and near contact in subjects with normal occlusion and malocclusion. American Journal of Orthodontics and Dentofacial Orthopedics. 2002;121:602–9. doi: 10.1067/mod.2002.122829. [DOI] [PubMed] [Google Scholar]
- 15.Parker MH, Cameron SM, Hughbanks JC, Reid DE. Compariosn of occlusal contacts in maximum intercuspation for two impression techniques. Journal of Prosthetic Dentistry. 1997;78:255–9. doi: 10.1016/s0022-3913(97)70023-4. [DOI] [PubMed] [Google Scholar]
- 16.Takai A, Nakano M, Bando E, Hewlett ER. Evaluation of three occlusal examination methods used to record tooth contacts in lateral excursive movements. Journal of Prosthetic Dentistry. 1993;70:500–5. doi: 10.1016/0022-3913(93)90262-m. [DOI] [PubMed] [Google Scholar]
- 17.Wright PS. Image analysis and occlusion. Journal of Prosthetic Dentistry. 1992;68:487–91. doi: 10.1016/0022-3913(92)90416-8. [DOI] [PubMed] [Google Scholar]
- 18.Korioth TWP. Number and location of occlusal contacts in intercuspal position. Journal of Prosthetic Dentistry. 1990;64:206–10. doi: 10.1016/0022-3913(90)90180-k. [DOI] [PubMed] [Google Scholar]
- 19.Molligoda MA, Berry DC, Gooding PG. Measuring diurnal variations in occlusal contact areas. Journal of Prosthetic Dentistry. 1986;56:487–92. doi: 10.1016/0022-3913(86)90395-1. [DOI] [PubMed] [Google Scholar]
- 20.Millstein PL. A method to determine occlusal contact and noncontact areas: Preliminary report. Journal of Prosthetic Dentistry. 1984;52:106–10. doi: 10.1016/0022-3913(84)90191-4. [DOI] [PubMed] [Google Scholar]
- 21.Russell MD, Grant AA. The relationship of occlusal wear to occlusal contact area. Journal of Oral Rehabilitation. 1983;10:383–91. doi: 10.1111/j.1365-2842.1983.tb00134.x. [DOI] [PubMed] [Google Scholar]
- 22.Hayashi T, Saitoh A, Ishioka K, Miyakawa M. A computerized system for analyzing occlusal relations during mandibular movements. International Journal of Prosthodontic. 1994;7:108–114. [PubMed] [Google Scholar]
- 23.DeLong R, Ko CC, Anderson GC, Hodges JS, Douglas WH. Comparing maximum intercuspal contacts of virtual dental patients and mounted dental casts. Journal of Prosthetic Dentistry. 2002;88:622–30. doi: 10.1067/mpr.2002.129379. [DOI] [PubMed] [Google Scholar]
- 24.Plasmans PJ, van Eil FA, Vrijhoef MM, van't Hof MA. The occlusal topographic contact method for the assessment of occlusal contacts. Journal of Dentistry. 1988;16:18–21. doi: 10.1016/0300-5712(88)90098-x. [DOI] [PubMed] [Google Scholar]


