Abstract
This article reviews the preoperative evaluation and operative considerations in patients with hilar cholangiocarcinoma. The preoperative evaluation is based on the imaging evaluation of the longitudinal and radial extent of the tumour along and around the hepatic duct confluence. The use of portal vein embolization to increase the safety of extended hepatectomy and the extent of surgical resection (caudate lobe and portal vein) are discussed within the context of recently published series.
Keywords: Hilar, cholangiocarcinoma, surgery, resection
Introduction
Of the estimated 6950 cases of extrahepatic biliary tract cancer that occur each year in the United States, approximately one-half are proximal bile duct adeno-carcinoma (hilar cholangiocarcinoma—CCA) 1,2. These tumours develop in a confined space between the portal vein, hepatic artery, liver and pancreas and present unique pathological and anatomical features 2. Left untreated, patients rarely survive more than 6 months and resection remains the only hope for long-term survival.
The purposes of surgical resection are twofold—to relieve the biliary obstruction caused by the tumour and to provide hope of cure for some patients. Although resection generally affords the patient the best chance for survival, only a small subset of patients with hilar CCA are candidates for surgical resection. In addition, resection of hilar CCA is often associated with significant morbidity and therefore proper patient selection is paramount. For those patients deemed unresectable, palliative options may be entertained.
In spite of recent advances in the evaluation and treatment of hilar CCA, several controversies remain. These include the role of preoperative portal vein embolization (PVE), the type and extent of resection, resection of the caudate lobe or portal vein and the value of lymphadenectomy. These topics will be the subject of this review.
Criteria of unresectability
The ultimate goal of surgical resection is to achieve negative margins, i.e. R0 resection. In contrast to most gastrointestinal cancers, in which clear margins are common, resection for hilar CCA only allows for limited surgical clearance margins 3. This may explain why even curative resections are associated with high local recurrence rates 4. These limitations and the associated perioperative risks emphasize the need for detailed preoperative evaluation.
In general, criteria of unresectability include 2: (1) bilateral intrahepatic bile duct spread to secondary or segmental biliary radicals; (2) involvement of the main trunk of the portal vein (except in unusual circumstances); (3) bilobar involvement of hepatic arterial and/or portal venous branches; (4) a combination of unilateral hepatic arterial involvement with cholangiographic evidence of extensive contralateral duct spread.
Classification of hilar cholangiocarcinoma/extent of resection
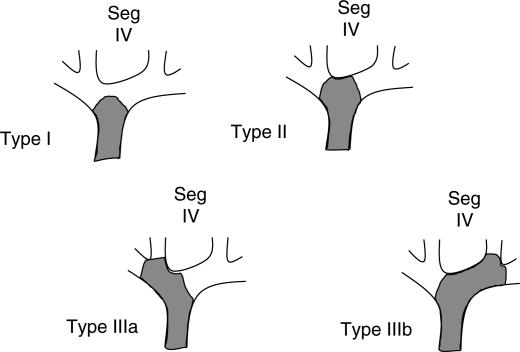
In order to determine resectability the preoperative evaluation should provide information regarding: (1) ductal involvement and (2) the radial extent of the tumour (involvement of the vasculature and the extent of hypertrophy/atrophy). Typically, this is achieved by: (1) direct cholangiography (percutaneous or endoscopic retrograde) or magnetic resonance cholangiography and (2) multiphasic intravenous contrast-enhanced helical computed tomography (CT) with thin cuts in an oblique coronal plane. This CT is also used to obtain a three-dimensional volumetric reconstruction of the future liver remnant to determine the need for portal vein embolization. In most resectable cases, the resection strategy will depend on the longitudinal tumour extent as defined based on the cholangiographic classification of Bismuth and Corlette 5 (Figure 1).
Figure 1. .
Bismuth–Corlette classification of potentially resectable (excludes type IV) hilar cholangiocarcinoma.
Local or hilar resections of the extrahepatic biliary tract represent the least extensive resection and in our opinion should only be performed—if at all—in mid bile duct CCA. Although no prospective randomized trials comparing common bile duct versus combined hepatic and common bile duct resection for hilar CCA have been done, several retrospective studies have indicated improved negative margin rates and increased overall survival with combined resections, despite higher overall morbidity and mortality 6,7,8,9,10,11,12. Recent studies have also shown that the complication rates with major hepatic resections have declined 7,9,11,13. The extent of resection and the survival data from series of patients who underwent resection of proximal CCA are presented in Table I9,11,14,15,16,17.
Table I. Results for resection of hilar cholangiocarcinoma.
| Reference | Patients resected (n) | Hepatic resection (%) | Curative (R0) resection (%) | Operative mortality (%) | 5-year survival after R0 resection (%) |
|---|---|---|---|---|---|
| Launois et al. 1999 14 | 40 | 62 | 80 | 12 | – |
| Kosuge et al. 1999 9 | 65 | 88 | 52 | 9 | 52 |
| Miyazaki et al. 1999 11 | 93 | 86 | 70 | 10 | 38 |
| Neuhaus et al. 1999 15 | 95 | 84 | 46 | 6 | 37 |
| Nimura et al. 2000 16 | 142 | 90 | 76 | – | – |
| Jarnagin et al. 2001 17 | 80 | 78 | 78 | 10 | 30 |
Ductal anatomy
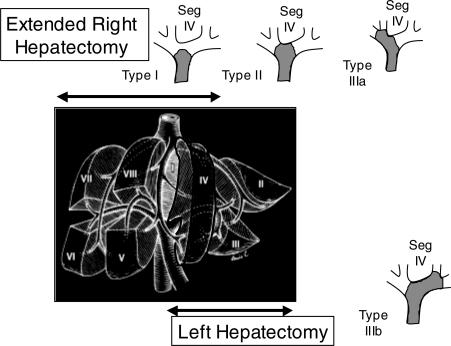
A thorough knowledge of hepatic ductal anatomy and its variants is essential in the planning of surgical resection. The right hepatic duct is inconstant and short (<1 cm). In contrast, the left hepatic duct is present in 97% of patients and is longer (1–5 cm) 15,18,19. In order to achieve negative margins for type I, II and IIIa tumours, therefore, we recommend an extended right hepatectomy with resection of segment IV (Figure 2). The relatively long and extra-hepatic course of the left hepatic duct can thus be utilized for reconstruction while optimizing surgical clearance margins. In contrast, for type IIIb hilar tumours, we recommend a left or extended left hepatectomy with resection of segment IV (Figure 2).
Figure 2. .
Extent of hepatic resection for types I-IIIb hilar cholangiocarcinoma.
Caudate lobe resection
Removal of the caudate lobe during hepatic resection for CCA, although somewhat controversial, has also gained acceptance. Proponents argue that improved margins can be achieved with minimal additional morbidity, while others suggest that removal should be performed in selected cases. Although specific studies comparing routine and selective caudate resection have not been performed, several studies have reported caudate lobe involvement in a high percentage of resected specimens, and the caudate lobe is the most frequent site of hepatic recurrence 12,20,21.
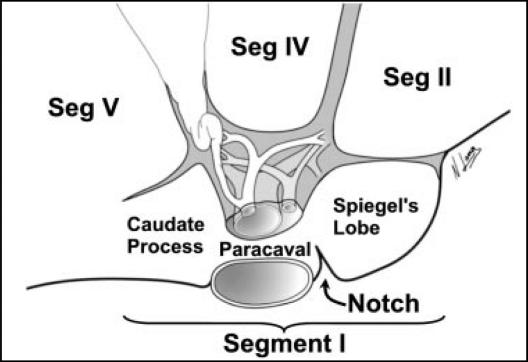
Removal of the caudate lobe requires a thorough understanding of its anatomy and relationship to the hepatic vasculature and ductal system. The caudate lobe (segment I) is divided into three subsegments (Figure 3). To the right of the inferior vena cava (IVC) and portal structures lies the caudate process while to the left of these structures and frequently visible beneath the lesser omentum lies Spiegel's lobe or the papillary process of the caudate lobe. The paracaval portion of the caudate lobe lies between these two and drapes the IVC 22.
Figure 3. .
Anatomy of the caudate lobe (segment I). Reproduced with permission from: Abdalla EK, Vauthey JN, Couinaud C. The caudate lobe of the liver: implications of embryology and anatomy for surgery. Surg Oncol Clin North Am. 2002;11(4):835–48.
We recommend that resection of the caudate process and paracaval caudate lobe be performed in all hepatic resections for hilar CCA since these lie in close proximity to the hepatic duct confluence. In performing a left hepatectomy for Bismuth–Corlette type IIIb tumours, Spiegel's lobe (papillary process) should also be removed. Whether or not Spiegel's lobe (papillary process) needs to be removed routinely or on the basis of tumour extent in type I-IIIa hilar CCA will need to be determined by further studies.
Portal vein resection
Portal vein resection and reconstruction has been traditionally performed only if gross invasion was noted at the time of hepatic resection or in select cases with invasion detected on preoperative imaging 12,23. More recently, portal vein resection has been proposed as part of a "no-touch" technique in resection of hilar CCA. In this study, portal vein resection was utilized in both right and left hepatectomies and histologically confirmed tumour infiltration was detected in 22% of specimens (50% in left-sided resections). Although portal vein resection was associated with improved survival, this was only evident when initial 60-day deaths were excluded. Overall 60-day mortality after resection was 17%, however, as compared with 5% for patients without portal vein resection 15. Considering this high complication rate and the lack of portal vein infiltration in the majority of specimens, routine resection of the portal vein cannot be recommended without additional evidence.
Preoperative portal vein embolization
A concern regarding major liver resection for hilar CCA is the potential for postoperative hepatic insufficiency reported in up to 32% of patients after combined resections 24. Although survival after >80% hepatic resection is possible in adults, extensive resections are associated with an increased risk of complications and postoperative hepatic dysfunction 25,26. An innovative strategy to increase the volume and function of the future remnant liver is the use of preoperative portal vein embolization (PVE) 27. With this procedure portal flow and the hepatrophic factors (interleukin-6, insulin, glucagon) are redistributed, resulting in ipsilateral apoptosis and contralateral regeneration.
Several studies have reported that preoperative PVE is safe and results in atrophy of the embolized lobe and hypertrophy of the remnant liver 28,29,30,31. Although preoperative PVE has not been compared to resection alone in a prospective randomized trial, there are significant data that support the safety and efficacy of this technique 23,32,33,34. For hilar CCA, therefore, if extensive hepatic resection is required, preoperative PVE should be strongly considered in patients with an anticipated future liver remnant volume of ≤20% of the total estimated liver volume 34,35.
Lymph node metastasis
Nodal status, including regional and para-aortic nodes, has been shown to be an important predictor of survival after resection for hilar CCA 9,36,37. Some authors have reported a benefit of lymphadenectomy with hepatic resection for CCA, although routine regional and para-aortic lymphatic resection have been performed in 3–53%, making comparisons difficult 9,11,12,15,36. A recent study from Japan reported on 110 patients with 2652 resected lymph nodes, with 14% containing metastatic disease 38. Although lymph node resection was reported as safe, that study and several others have shown that only 1–5% of patients with positive lymph nodes, particularly when outside the regional area, will survive 5 years 9,11,15,36,37,38,39. These data suggest that lymph node dissection may add valuable staging and prognostic information, but that the impact on overall survival is minimal. In light of this, routine lymphadenectomy beyond the hepatoduodenal ligament cannot be recommended.
References
- 1.Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, et al. Cancer statistics, 2004. CA Cancer J Clin. 2004;54:8–29. doi: 10.3322/canjclin.54.1.8. [DOI] [PubMed] [Google Scholar]
- 2.Vauthey JN, Blumgart LH. Recent advances in the management of cholangiocarcinomas. Semin Liver Dis. 1994;14:109–14. doi: 10.1055/s-2007-1007302. [DOI] [PubMed] [Google Scholar]
- 3.Nagorney DM, Donohue JH, Farnell MB, Schleck CD, Ilstrup DM. Outcomes after curative resections of cholangiocarcinoma. Arch Surg 1993;128:871–7; discussion 877–9. [DOI] [PubMed] [Google Scholar]
- 4.Macdonald OK, Crane CH. Palliative and postoperative radiotherapy in biliary tract cancer. Surg Oncol Clin North Am. 2002;11:941–54. doi: 10.1016/s1055-3207(02)00038-8. [DOI] [PubMed] [Google Scholar]
- 5.Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet. 1975;140:170–8. [PubMed] [Google Scholar]
- 6.Bismuth H, Nakache R, Diamond T. Management strategies in resection for hilar cholangiocarcinoma. Ann Surg. 1992;215:31–8. doi: 10.1097/00000658-199201000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burke EC, Jarnagin WR, Hochwald SN, Pisters PW, Fong Y, Blumgart LH. Hilar cholangiocarcinoma: patterns of spread, the importance of hepatic resection for curative operation, and a presurgical clinical staging system. Ann Surg. 1998;228:385–94. doi: 10.1097/00000658-199809000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cameron JL, Pitt HA, Zinner MJ, Kaufman SL, Coleman J. Management of proximal cholangiocarcinomas by surgical resection and radiotherapy. Am J Surg 1990;159:91–7; discussion 97–8. [DOI] [PubMed] [Google Scholar]
- 9.Kosuge T, Yamamoto J, Shimada K, Yamasaki S, Makuuchi M, et al. Improved surgical results for hilar cholangiocarcinoma with procedures including major hepatic resection. Ann Surg. 1999;230:663–71. doi: 10.1097/00000658-199911000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee SG, Lee YJ, Park KM, Hwang S, Min PC. One hundred and eleven liver resections for hilar bile duct cancer. J Hepatobiliary Pancreat Surg. 2000;7:135–41. doi: 10.1007/s005340050167. [DOI] [PubMed] [Google Scholar]
- 11.Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Okaya T, et al. Parenchyma-preserving hepatectomy in the surgical treatment of hilar cholangiocarcinoma. J Am Coll Surg. 1999;189:575–83. doi: 10.1016/s1072-7515(99)00219-7. [DOI] [PubMed] [Google Scholar]
- 12.Nimura Y, Hayakawa N, Kamiya J, Kondo S, Shionoya S. Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg 1990;14:535–43; discussion 544. [DOI] [PubMed] [Google Scholar]
- 13.Neuhaus P, Jonas S. Surgery for hilar cholangiocarcinoma – the German experience. J Hepatobiliary Pancreat Surg. 2000;7:142–7. doi: 10.1007/s005340050168. [DOI] [PubMed] [Google Scholar]
- 14.Launois B, Terblanche J, Lakehal M, Catheline JM, Bardaxoglou E, Landen S, et al. Proximal bile duct cancer: high resectability rate and 5-year survival. Ann Surg. 1999;230:266–75. doi: 10.1097/00000658-199908000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg 1999;230:808–18; discussion 819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nimura Y, Kamiya J, Kondo S, Nagino M, Uesaka K, Oda K, et al. Aggressive preoperative management and extended surgery for hilar cholangiocarcinoma: Nagoya experience. J Hepatobiliary Pancreat Surg. 2000;7:155–62. doi: 10.1007/s005340050170. [DOI] [PubMed] [Google Scholar]
- 17.Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BSJ, et al. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 2001;234:507–17; discussion 517–1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bismuth H. Surgical anatomy and anatomical surgery of the liver. World J Surg. 1982;6:3–9. doi: 10.1007/BF01656368. [DOI] [PubMed] [Google Scholar]
- 19.Couinaud C. Le foie. Etudes anatomiques et churgicales. InParis, 1957. pp.469–79. [Google Scholar]
- 20.Mizumoto R, Kawarada Y, Suzuki H. Surgical treatment of hilar carcinoma of the bile duct. Surg Gynecol Obstet. 1986;162:153–8. [PubMed] [Google Scholar]
- 21.Baer HU, Stain SC, Dennison AR, Eggers B, Blumgart LH. Improvements in survival by aggressive resections of hilar cholangiocarcinoma. Ann Surg. 1993;217:20–7. doi: 10.1097/00000658-199301000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abdalla EK, Vauthey JN, Couinaud C. The caudate lobe of the liver: implications of embryology and anatomy for surgery. Surg Oncol Clin North Am. 2002;11:835–48. doi: 10.1016/s1055-3207(02)00035-2. [DOI] [PubMed] [Google Scholar]
- 23.Ebata T, Nagino M, Kamiya J, Uesaka K, Nagasaka T, Nimura Y. Hepatectomy with portal vein resection for hilar cholangiocarcinoma: audit of 52 consecutive cases. Ann Surg. 2003;238:720–7. doi: 10.1097/01.sla.0000094437.68038.a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nagino M, Ando M, Kamiya J, Uesaka K, Sano T, Nimura Y. Liver regeneration after major hepatectomy for biliary cancer. Br J Surg. 2001;88:1084–91. doi: 10.1046/j.0007-1323.2001.01832.x. [DOI] [PubMed] [Google Scholar]
- 25.Abdalla EK, Hicks ME, Vauthey JN. Portal vein embolization: rationale, technique and future prospects. Br J Surg. 2001;88:165–75. doi: 10.1046/j.1365-2168.2001.01658.x. [DOI] [PubMed] [Google Scholar]
- 26.Shoup M, Gonen M, D'Angelica M, Jarnagin WR, DeMatteo RP, Schwartz LH, et al. Volumetric analysis predicts hepatic dysfunction in patients undergoing major liver resection. J Gastrointest Surg. 2003;7:325–30. doi: 10.1016/s1091-255x(02)00370-0. [DOI] [PubMed] [Google Scholar]
- 27.Vauthey JN, Chaoui A, Do KA, Bilimoria MM, Fenstermacher MJ, Charnsangavej C, et al. Standardized measurement of the future liver remnant prior to extended liver resection: methodology and clinical associations. Surgery. 2000;127:512–19. doi: 10.1067/msy.2000.105294. [DOI] [PubMed] [Google Scholar]
- 28.Nagino M, Kamiya J, Kanai M, Uesaka K, Sano T, Yamamoto H, et al. Right trisegment portal vein embolization for biliary tract carcinoma: technique and clinical utility. Surgery. 2000;127:155–60. doi: 10.1067/msy.2000.101273. [DOI] [PubMed] [Google Scholar]
- 29.Nagino M, Nimura Y, Kamiya J, Kondo S, Uesaka K, Kin Y, et al. Right or left trisegment portal vein embolization before hepatic trisegmentectomy for hilar bile duct carcinoma. Surgery. 1995;117:677–81. doi: 10.1016/s0039-6060(95)80012-3. [DOI] [PubMed] [Google Scholar]
- 30.Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunven P, et al. Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery. 1990;107:521–7. [PubMed] [Google Scholar]
- 31.Imamura H, Shimada R, Kubota M, Matsuyama Y, Nakayama A, Miyagawa S, et al. Preoperative portal vein embolization: an audit of 84 patients. Hepatology. 1999;29:1099–105. doi: 10.1002/hep.510290415. [DOI] [PubMed] [Google Scholar]
- 32.Abdalla EK, Barnett CC, Doherty D, Curley SA, Vauthey JN. Extended hepatectomy in patients with hepatobiliary malignancies with and without preoperative portal vein embolization. Arch Surg 2002;137:675–80; discussion 680–1. [DOI] [PubMed] [Google Scholar]
- 33.Madoff DC, Hicks ME, Abdalla EK, Morris JS, Vauthey JN. Portal vein embolization with polyvinyl alcohol particles and coils in preparation for major liver resection for hepatobiliary malignancy: safety and effectiveness – study in 26 patients. Radiology. 2003;227:251–60. doi: 10.1148/radiol.2271012010. [DOI] [PubMed] [Google Scholar]
- 34.Vauthey JN, Pawlik TM, Abdalla EK, Arens JF, Nemr RA, Wei SH, et al. Is extended hepatectomy for hepatobiliary malignancy justified? Ann Surg. 2004;239:722–32. doi: 10.1097/01.sla.0000124385.83887.d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abdalla EK, Denys A, Chevalier P, Nemr RA, Vauthey JN. Total and segmental liver volume variations: implications for liver surgery. Surgery. 2004;135:404–10. doi: 10.1016/j.surg.2003.08.024. [DOI] [PubMed] [Google Scholar]
- 36.Todoroki T. Chemotherapy for bile duct carcinoma in the light of adjuvant chemotherapy to surgery. Hepatogastroenterology. 2000;47:644–9. [PubMed] [Google Scholar]
- 37.Klempnauer J, Ridder GJ, von Wasielewski R, Werner M, Weimann A, Pichlmayr R. Resectional surgery of hilar cholangiocarcinoma: a multivariate analysis of prognostic factors. J Clin Oncol. 1997;15:947–54. doi: 10.1200/JCO.1997.15.3.947. [DOI] [PubMed] [Google Scholar]
- 38.Kitagawa Y, Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, et al. Lymph node metastasis from hilar cholangiocarcinoma: audit of 110 patients who underwent regional and paraaortic node dissection. Ann Surg. 2001;233:385–92. doi: 10.1097/00000658-200103000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ogura Y, Mizumoto R, Tabata M, Matsuda S, Kusuda T. Surgical treatment of carcinoma of the hepatic duct confluence: analysis of 55 resected carcinomas. World J Surg 1993;17:85–92; discussion 92–3. [DOI] [PubMed] [Google Scholar]