Abstract
Focal nodular hyperplasia (FNH) is a benign condition of the liver that is often discovered incidentally on radiological investigation. FNH has no malignant potential, is rarely symptomatic and surgical intervention is almost never required. However, eight patients with a diagnosis of FNH associated with upper abdominal pain or rapid growth were referred for surgery. All patients had been extensively investigated for other causes of pain and had been observed for between 1 and 7 years prior to surgical referral. The FNH lesions were between 1 cm and 8 cm in diameter. One FNH lesion 7.5 cm in diameter lay in segment VII/VIII and was related to the right and middle hepatic veins. All patients were resected with immediate and lasting control of their symptoms. Based on this experience FNH should be managed in a manner similar to haemangiomas with most lesions being safe to observe. However, it should be recognized that symptomatic FNH does occur, as well as FNH behaving in an unusual fashion such as rapid growth. Both of these findings are indications for resection.
Introduction
Focal nodular hyperplasia (FNH) lesions are benign liver lesions characterized by the presence of a vascular red-brown or tan mass with nodules of benign hepatic parenchyma laced with fibrous septa that may extend out from a broad central stellate scar 1,2. FNH is more common in premenopausal women, although up to 10% may occur in males 3,4. The lesions are often detected incidentally during imaging for non-specific symptoms of the abdomen and, once the diagnosis has been established, active treatment is almost never required 1. We present a small series of eight patients with proven FNH who were referred for surgery for relief of symptoms or because of rapid growth. Hepatic resection was undertaken in all patients with excellent outcome.
Methods
A prospective computerized database of patients managed by the Upper Gastrointestinal/Hepatobiliary Unit at Auckland Hospital was established in the year 2000 for the purposes of audit after consultation with the Northern Regional Ethics Committee in Auckland, New Zealand. Demographic, clinical, pathological, management and follow-up data are recorded pro-spectively on all patients managed by the unit. Retrospective review of the database identified eight patients with a proven diagnosis of FNH of the liver who had undergone resection of the lesion for relief of symptoms or documented rapid increase in size. All patients were then followed up prospectively to assess the effectiveness of resection for control of symptoms.
Results
Demographics
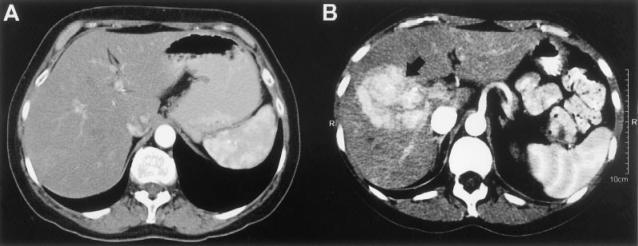
All patients with FNH were Caucasian females with a median age of 37 years (range 16–52 years). The presenting symptom in seven of them was abdominal pain present for a median of 2 years (range 1–7 years). Apart from patient no. 8 the pain was uniformly described as a constant dull ache in the right upper quadrant without exacerbating or relieving factors (Table I). Patient no. 8 experienced pain only on running or jogging, with pain increasing in severity with the duration of exercise. Patient no. 4 was referred because of a rapidly enlarging lesion noted incidentally on ultrasound carried out to investigate mildly abnormal liver function tests. Subsequently a contrast-enhanced CT scan was obtained (Figure 1). This patient was also taking immunosuppressive therapy following a successful kidney/pancreas transplant for diabetes mellitus. None of the patients had symptoms of jaundice or hepatic failure. Of the eight patients, patient no. 2 was taking a combined oral contraceptive and patient no. 6 was taking hormone replacement therapy for menopause-related symptoms (Table I).
Table I. Demographic details of eight patients with FNH.
| Patient no. | Age (years) | Sex | Symptoms | Duration (years) | Hormone therapy |
|---|---|---|---|---|---|
| 1 | 45 | F | RUQ pain | 1 | Nil |
| 2 | 23 | F | RUQ pain | 1 | Oral |
| contraceptive | |||||
| 3 | 38 | F | RUQ pain | 3 | Nil |
| 4 | 36 | F | Incidental, | — | Nil |
| ∣ size | |||||
| 5 | 27 | F | RUQ pain | 7 | Nil |
| 6 | 52 | F | RUQ and | 2 | Hormone |
| flank pain | replacement | ||||
| therapy | |||||
| 7 | 43 | F | RUQ pain | 1.5 | Nil |
| 8 | 16 | F | RUQ pain | 4 | Nil |
RUQ, right upper quadrant.
Figure 1. .
(A) Arterial phase CT scan from patient no. 4 following kidney/pancreas transplant showing no abnormality. (B) Arterial phase CT scan from patient no. 4 taken 18 months after scan A demonstrating a hypervascular mass (arrow) in the right lobe of the liver.
Investigations
All patients were initially investigated with ultrasound as part of the work-up for upper abdominal pain. Subsequently all patients were investigated with CT scan of the liver and three patients also were examined by MRI (Table II). In all cases the ultrasound, CT and MRI appearances of the lesions showed hypervascular soft tissue masses consistent with a diagnosis of FNH. However patient no. 4 did not have an obvious central scar and, because of the rapid growth and aggressive appearance of this lesion, biopsy was undertaken. This demonstrated only blood and a definitive diagnosis of FNH was not established preoperatively in this patient. In addition to investigations specific for the liver lesions, all patients had undergone a variety of tests to exclude other causes of right upper quadrant pain (most commonly gastroduodenoscopy, colonoscopy and biliary HIDA scan).
Table II. Details of investigations in eight patients with FNH.
| Patient no. | US scan | CT scan | MRI | Biopsy | Size of FNH (cm) | Segment |
|---|---|---|---|---|---|---|
| 1 | N | Y | N | N | 7×6 | II/III |
| 2 | Y | Y | Y | Y | 5.5×4×5 | V |
| 3 | Y | Y | N | N | 1.4×0.5×1 | IV/V |
| 4 | Y | Y | Y | Y | 6×6 | VII/VII |
| 5 | Y | Y | N | N | 8×8 | II/III |
| 6 | N | Y | Y | Y | 4×4 | VII |
| 7 | Y | Y | N | N | 1×2 | IVB/VIII |
| 8 | N | Y | N | N | 7.5×6.5×5.5 | VIII |
US, ultrasound; CT, computed tomography; MRI, magnetic resnance imaging.
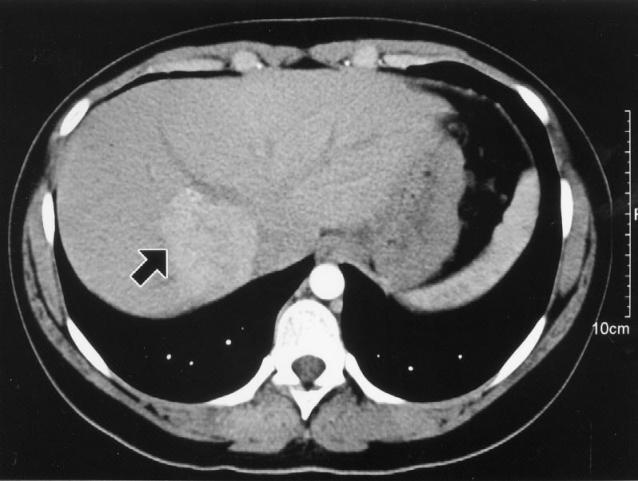
The size of the lesions varied between 1 cm in diameter (patient no. 7) and nearly 8 cm in diameter (patient no. 5). Most lesions were situated peripherally in the liver, although patient no. 8 had a large FNH lesion that lay in an intrahepatic position related to the right and middle hepatic veins (Figure 2).
Figure 2. .
Contrast-enhanced CT scan from patient no. 8 demonstrating a biopsy-proven FNH lesion (arrow) closely related to the origins of the right and middle hepatic veins. This patient complained of pain beginning shortly after exercising.
Treatment
All patients were referred for hepatic resection following extended periods of observation. The duration of observation ranged from 1 to 7 years. None of the patients experienced any relief of symptoms or shrinkage of the lesions on surveillance scans during observation. All patients were taking regular oral medications for pain (including opiates) preoperatively.
After preoperative review surgical resection was undertaken in all cases (Table III). Following resection patient nos 1, 3 and 5–8 who had presented with a long history of pain had relief of their symptoms. These patients were followed up at 6 weeks, 3 months and 6 months after resection with no recurrence of their presenting symptoms and without the need to recommence regular analgesia (median follow-up 2.0 years, range 1–4 years). Postoperative histology showed FNH of the traditional type containing abnormal nodular architecture, abnormal vessels and cholangiolar proliferation in all cases. All resected FNH also contained a typical central scar histologically.
Table III. Details of treatment in eight patients with FNH.
| Patient number | Procedure | Blood loss (ml) | Complication | Hospital stay (days) | Symptom relief |
|---|---|---|---|---|---|
| 1 | Segment 2/3 resection | 200 | Nil | 7 | Yes |
| 2 | Segment 5 resection | 200 | Wound sinus | 7 | Yes |
| 3 | Segment 5/6 resection | 300 | Mild pancreatitis | 7 | Yes |
| 4 | Right lobectomy | 400 | Wound collection | 6 | Yes |
| 5 | Segment 2/3 resection | 300 | Nil | 5 | Yes |
| 6 | Segment 4 resection | 400 | Nil | 9 | Yes |
| 7 | Segment 4 resection | 50 | Nil | 4 | Yes |
| 8 | Right lobectomy | 800 | Pneumonia | 10 | Yes |
Discussion
Focal nodular hyperplasia comprises benign tumour-like lesions that are the result of a hyperplastic rather than a neoplastic process. They are classically described as containing thickened plates of hepatic parenchyma surrounding a central fibrous scar containing malformed vascular structures with radiating fibrous septa 2. The pathogenesis of FNH is unclear; however, Wanless et al.5 have suggested that FNH develops as hyperplastic nodules caused by blood flow in an anomalous hepatic artery branch. Kondo 6 has also proposed that FNH lesions are a result of regional abnormalities in either portal or hepatic arterial blood flow. Certainly FNH lesions are characterized macroscopically by the presence of abnormal, dilated capsular blood vessels 2, they are known to occur simultaneously with other vascular hepatic lesions such as haemangiomas and adenomas 7, and their incidence may be increased following blunt abdominal trauma 8 and chemotherapy 9, both of which are associated with intrahepatic vascular damage. In addition, an Italian case control study found that cigarette smoking was an indicator of elevated risk of FNH 10.
The mechanisms by which FNH lesions may cause pain are unclear. Malignant change has never been reported in FNH 2, although FNH may occur in association with hepatocellular carcinoma 11 and other tumours 9. However, there are well documented cases of intra-lesional haemorrhage 2 and rupture 12. As the lesions are intensely vascular and all of the FNH lesions in this series were related to the liver capsule it is possible that variations in blood flow caused pain because of capsular distension. In addition, patient no. 8 had an FNH lesion that was closely related to the right and middle hepatic veins and may have caused pain by restricting hepatic venous outflow, particularly during exercise. Other investigators have also noted this phenomenon 13. Interestingly, in a large study of over 300 FNH cases, Nguyen et al.2 found that traditional FNH lesions (i.e. those containing abnormal nodular architecture, malformed appearing vessels and cholangiolar proliferation) were most likely to be associated with symptoms. Other histological types such as telangiectatic, mixed and atypical forms were less likely to be associated with symptoms.
Painful, symptomatic FNH lesions or FNH behaving in an unusual manner are rare. The eight cases reported in this small series represent a very small fraction of the total numbers of FNH seen by our unit and constitute only a very small percentage of the total numbers of FNH present in the community, although the exact denominator is unknown. We currently only record data on patients who undergo resections in our unit. However, many more patients are seen and assessed with asymptomatic FNH and discharged from follow-up. The discovery of an FNH is almost always an incidental finding. However, the purpose of presenting these eight patients is to draw attention to the fact that, while most FNH lesions do not require intervention, a small minority are associated with disabling symptoms or abnormal behaviour and should be considered for surgical resection. In most of our cases the diagnosis of FNH was not in doubt and only in patient no. 4 was resection undertaken to differentiate between FNH and other nodular hepatic lesions such as adenoma or fibrolamellar carcinoma. Currently, investigations such as triple-phase CT scan, magnetic resonance scanning and careful use of ultrasound-guided core biopsy permit most patients with FNH to be accurately diagnosed 3,14.
The use of biopsy in the diagnosis of hypervascular hepatic lesions is controversial. We believe that the role of biopsy is to confirm benign pathology in patients with radiologically benign appearing lesions 15,16. In the current series biopsy was utilized to confirm the presence of FNH and to exclude the presence of a fibrolamellar carcinoma. For the majority of patients with FNA a benign biopsy result meant that they could be reassured regarding the absence of cancer, and safely observed.
Based on our experience FNH should be managed in a manner similar to hepatic haemangiomas. Once diagnosed, most lesions do not require treatment or even regular follow-up. However, lesions should be resected if they are clearly symptomatic, are behaving in an abnormal fashion by increasing in size or if radiological investigations show signs of intra-lesional haemorrhage.
References
- 1.Foster JH, Berman MM. Foster JH, Berman MM. WB Saunders; Philadelphia: 1977. The benign lesions: adenoma and focal nodular hyperplasia, Solid liver tumors; pp. 138–78. [Google Scholar]
- 2.Nguyen B, Flejou J-F, Terris B, Belghiti J, Degott C. Focal nodular hyperplasia of the liver: a comprehensive pathologic study of 305 lesions and recognition of new histological forms. Am J Surg Pathol. 1999;23:1441–58. doi: 10.1097/00000478-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Herman P, Pugliese V, Machado M, Montagnini AL, Salem MZ, Bacchella T, et al. Hepatic adenoma and focal nodular hyperplasia: differential diagnosis and treatment. World J Surg. 2000;24:373–6. doi: 10.1007/s002689910059. [DOI] [PubMed] [Google Scholar]
- 4.Cherqui D, Rahmouni A, Charlotte F, Boulahdour H, Metreau J-M, Meignan M, et al. Management of focal nodular hyperplasia and hepatocellular adenoma in young women: a series of 41 patients with clinical, radiological, and pathological correlations. Hepatology. 1995;22:1674–81. [PubMed] [Google Scholar]
- 5.Wanless IR, Maudsley C, Adams R. On the pathogenesis of focal nodular hyperplasia of the liver. Hepatology. 1985;6:1194–200. doi: 10.1002/hep.1840050622. [DOI] [PubMed] [Google Scholar]
- 6.Kondo F. Benign nodular hepatocellular lesions caused by abnormal hepatic circulation: etiological analysis and introduction of a new concept. J Gastroenterol Hepatol. 2001;16:1319–28. doi: 10.1046/j.1440-1746.2001.02576.x. [DOI] [PubMed] [Google Scholar]
- 7.Di Carlo I, Urrico GS, Ursino V, Russello D, Puleo S, Latteri F. Simultaneous occurrence of adenoma, focal nodular hyperplasia and hemangioma of the liver: are they derived from a common origin. J Gastroenterol Hepatol. 2003;18:227–30. doi: 10.1046/j.1440-1746.2003.02840.x. [DOI] [PubMed] [Google Scholar]
- 8.Savoye-Collet C, Herve S, Koning E, Scotte M, Dacher JN. Focal nodular hyperplasia occurring after blunt abdominal trauma. Eur J Gastroenterol Hepatol. 2002;14:329–30. doi: 10.1097/00042737-200203000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Bouyn CI, Leclere J, Raimondo G, Le Pointe HD, Couanet D, Valteau-Couanet D, et al. Hepatic focal nodular hyperplasia in children previously treated for a solid tumor. Incidence, risk factors and outcome. Cancer. 2003;97:3107–13. doi: 10.1002/cncr.11452. [DOI] [PubMed] [Google Scholar]
- 10.Scalori A, Tavani A, Gallus S, La Vecchia C, Colombo M. Risk factors for focal nodular hyperplasia of the liver: an Italian case-control study. Am J Gastroenterol. 2002;97:2371. doi: 10.1111/j.1572-0241.2002.05796.x. [DOI] [PubMed] [Google Scholar]
- 11.Chen TC, Chou TB, Ng KF, Hsieh LL, Chou YH. Hepatocellular carcinoma, associated with focal nodular hyperplasia. Report of a case with clonal analysis. Virchows Archiv. 2001;438:408–11. doi: 10.1007/s004280000348. [DOI] [PubMed] [Google Scholar]
- 12.Behrend M, Flemming P, Halbfass HJ. Spontaneous bleeding of focal nodular hyperplasia as a rare cause of acute abdomen. Chirurg. 2001;72:1201–4. doi: 10.1007/s001040170061. [DOI] [PubMed] [Google Scholar]
- 13.Rangheard AS, Vilgrain V, Audet P, O'Toole D, Vullierme MP, Valla D, et al. Focal nodular hyperplasia inducing hepatic vein obstruction. Am J Roentgenol. 2002;179:759–62. doi: 10.2214/ajr.179.3.1790759. [DOI] [PubMed] [Google Scholar]
- 14.Nagorney DM. Benign hepatic tumors: focal nodular hyperplasia and hepatocellular adenoma. World J Surg. 1995;19:13–18. doi: 10.1007/BF00316973. [DOI] [PubMed] [Google Scholar]
- 15.Shawcross DL, Naoumov N, Pachiadakis I, Mamais C, Williams R, Jalan R, et al. Should a biopsy precede liver resection or transplantation for presumed hepatocellular carcinoma when the alfa fetoprotein is normal. Transplantation. 2004;77:637–8. doi: 10.1097/01.tp.0000109783.98513.e3. [DOI] [PubMed] [Google Scholar]
- 16.Durand F, Regimbeau JM, Belghiti J, Sauvanet A, Vilgrain V, Terris B, et al. Assessment of the benefits and risks of percutaneous biopsy before surgical resection of hepatocellular carcinoma. J Hepatol. 2001;35:254. doi: 10.1016/s0168-8278(01)00108-8. [DOI] [PubMed] [Google Scholar]