Abstract
OBJECTIVES
To measure the prevalence of fear of falling in older adults at the time of long- term care (LTC) enrollment and identify potentially treatable risk factors for low fall related self-efficacy.
DESIGN
Prospective cohort study.
SETTING
Three LTC programs in Upstate New York.
PARTICIPANTS
112 new enrollees in LTC, aged 55 or older, who passed a cognitive screen.
MEASUREMENTS
Self-reported falls, the falls efficacy scale (FES), medical conditions, the short geriatric depression scale, and physical performance measures (Berg balance scale, hip flexor, knee extensor and grip strength, gait speed and a six-minute walk).
RESULTS
Of the 54 subjects (48.2%) who reported fear of falling, 41 (75.9%) reported activity modification secondary to fear. Fearful subjects were more likely to be female (P=.003), report low back pain (P=.030) and lower extremity arthritis (P=.048). Fearful subjects were weaker at the hip (P<.001) and knee (P=.001), and had shorter six-minute walk distances. Subjects with better FES scores had better Berg scores (P<.001), had greater hip and knee strength, had faster gait speeds and walked further in six minutes (P<.001, P=.006, P=.001 and P=.001 respectively). Subjects with low FES scores and fearful subjects were more likely to have depressive symptoms (P=.003, P=.044, respectively).
CONCLUSION
Falls and fear of falling are more common in new LTC enrollees than in previously described community dwelling and SNF cohorts. Attention to associated characteristics like depression, arthritis, low back pain and lower extremity weakness may identify opportunities to reduce fear and improve patient safety during this transitional period.
Keywords: accidental falls, fear of falling, long-term care, transitions of care
INTRODUCTION
Long-term care (LTC) programs provide personal care and related health services on an extended basis to those who are unable to care for themselves. LTC programs are based in a variety of settings including the home, the community, and skilled nursing facilities. Efforts to create safe transitions are especially important for those newly enrolling in LTC programs, as this population, by virtue of its medical complexity, prevalent cognitive impairment and low health literacy, is particularly vulnerable to adverse events during transitional periods (1). Transition of older adults into LTC is common. Individuals at the age of 65 are estimated to have a 46 percent lifetime risk of being admitted to a nursing home (2). During the transition period to a new LTC facility, older adults are at increased risk of falls (3). Falls have significant morbidity and mortality for older adults.
Fear of falling is a risk factor for falls in older adults. It has widespread physical and psychological impacts. Decreases in physical activity associated with fear of falling are thought to decrease strength, physical function and socialization, and thereby further increase the risk of falling and incite a dangerous cycle of more fear and falls (4). In community dwellers, frailty, high burden of medical conditions and depression have been recognized as risk factors for fear (5–7). Studies suggest that fear of falling contributes to poor quality of life and is a risk factor for institutionalization (6, 8–11). Despite these findings, a paucity of studies address fear of falling in LTC participants.
In a study of fear of falling in established nursing home residents, 46 percent of subjects reported fear of falling when asked simply “are you afraid of falling?” Fearful subjects were more likely to have low functional status and impaired balance and gait. Over time, fear of falling was predictive of further functional declines (12). An important next step to understanding fear in LTC is exploring whether residents enter programs with high rates of fear or if fear develops after enrollment. Understanding of fear of falling at enrollment is critical because this is when many interventions to improve physical function and decrease falls are initiated. Identification of risk factors for fear could improve efforts to prevent the adverse outcomes of fear.
In community dwellers, fear of falling that leads to activity modification is associated with significant consequences including loss of strength, poor physical performance, and increased risk of falls (13). For community dwellers, risk factors for activity modification secondary to fear include physical frailty, medical co-morbidities and depressive symptoms (14). Prevalence and risk factors for activity modifying fear in new LTC enrollees have not been described.
We hypothesized that fear of falling and activity-modifying fear of falling would be common in new enrollees in LTC. We also hypothesized that identifiable, potentially treatable risk factors for low falls related self-efficacy and fear of falling exist in new LTC enrollees.
METHODS
Subject Recruitment
Data used are from the study “Function, Quality of Life and Health Care Utilization in Three LTC Models” which was supported by a grant from the National Institute on Aging and a General Clinical Research Center grant from the National Center for Research Resources, NIH. New enrollees in three LTC programs in Upstate New York were invited to participate. Programs included were: 1) a Program of All – Inclusive Care for the Elderly [PACE] 2) a long-term home health care program [LTHHC] and 3) a skilled nursing facility [SNF]. During the enrollment period (October 2002 - May 2005), 380 people enrolled in these programs. Inclusion criteria included age 55 and older, English speaking and life expectancy of at least three months. Short stay rehabilitation admissions to LTC were excluded, leaving only LTC admissions to the SNF eligible for the study. Study enrollment is shown in Figure 1. The University of Rochester Institutional Review Board approved this study.
Figure 1.
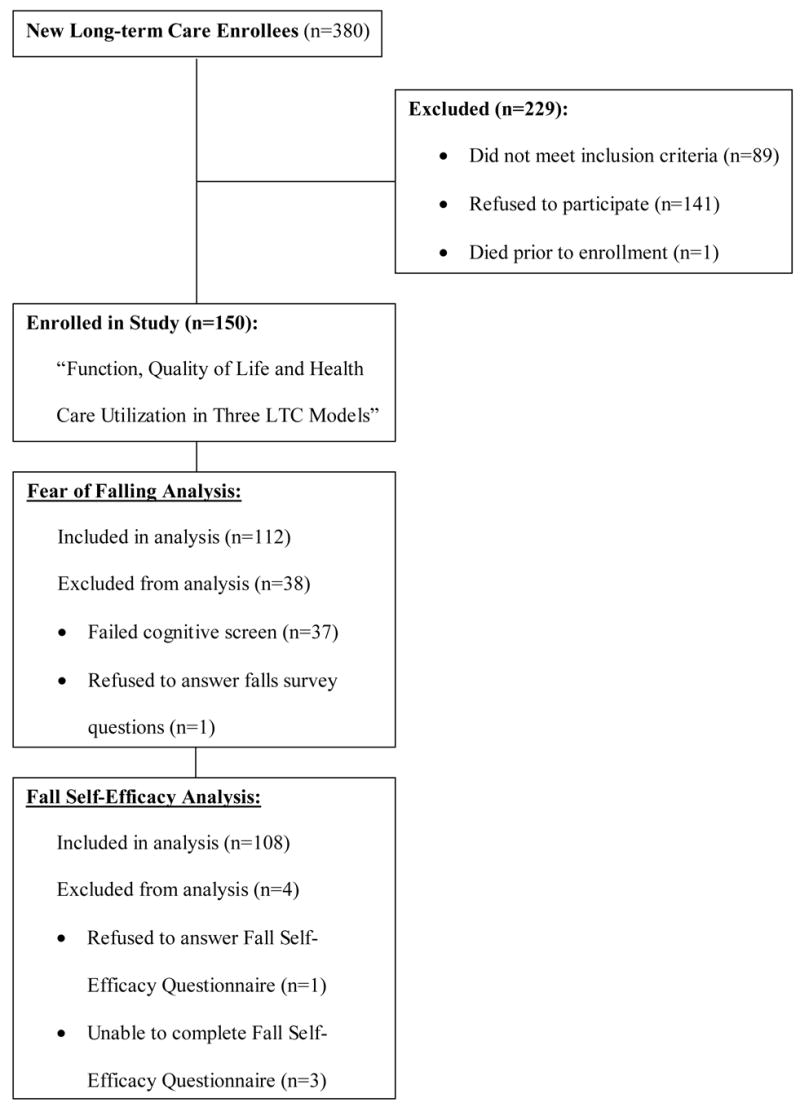
Subject Enrollment and Sampling for Fear of Falling and Fall Self- Efficacy Analyses.
Data Collection
Subjects were evaluated within three weeks of LTC program enrollment. Trained nurses collected information on demographics, medical conditions, and falls. Subjects underwent cognitive screening at enrollment. The screen included a three-item recall and three simple questions where subjects rated their health. When subjects could not recall at least one of three items after five minutes and answer all questions, they were considered cognitively impaired (15). One hundred and thirteen (75.3%) subjects passed this cognitive screen. These subjects were given subjective questionnaires, including the short geriatric depression scale (GDS) and the FES.
Falls/Fear of Falling
Subjects answered the questions, “Apart from being in a high place, in the past 12 months, have you been worried or afraid you might fall?” and “Do you ever limit your activities, for example, what you do and where you go, because you are afraid of falling?” (4).
Subjects also completed Tinetti’s Falls Efficacy Scale (FES). The FES is a 10-question scale that assesses the impact of fear of falling on confidence in performing everyday tasks. Subjects are asked questions like “How confident are you that you can get dressed and undressed without falling?” Subjects answer with a rating from zero (not confident) to 10 (very confident). Ratings are combined, giving scores from zero (low fall related self-efficacy) to 100 (high fall related self-efficacy). The internal reliability (Cronbach alpha=0.91) and test-retest consistency (r=0.71) have been described (16).
Subject Sample for Fear of Falling and Fall Self-Efficacy Analyses
Subject sampling for fear of falling and fall self-efficacy analyses is shown in Figure 1. Of the 112 subjects who passed the cognitive screen, 104 completed all 10 questions on the FES. Three subjects answered “don’t know” to the majority of FES questions and one subject refused to participate in FES questioning. Four subjects completed nine out of 10 FES questions but were unable to complete one question. Using a previously described method, these subjects were scored on the nine available items and that score was converted to a 100-point scale (11). Including these subjects’ FES scores in analysis did not significantly alter findings, and therefore results include 108 subjects.
Medical Conditions
Subjects were asked if they had: angina, hypertension, coronary heart disease, congestive heart failure, myocardial infarction, stroke, emphysema or chronic obstructive pulmonary disease, inflammatory bowel disease, arthritis of the hip or knee, arthritis of the hand or wrist, low back pain, diabetes mellitus and cancer other than skin cancers.
Physical Performance Measures
Fitness testing included measuring distance traveled during a six-minute walk. Gait speed was measured by recording the time needed to traverse four-meters at usual walking pace. Using the Lafayette Manual Muscle test system (model 01163), knee extensors and hip flexors strength were measured to the nearest 0.1 kg resistance in subjects who had not had recent knee, hip or hernia surgeries, did not have extremity contractures and who were not limited by pain. Two trials were performed on each side and the strongest trial was included in analysis. Hand held dynamometer measured grip strength on the strongest side in all pain free subjects who had not had recent hand or arm surgery or pain, arthritis or tendonitis of the wrist. Subjects could refuse to participate with any testing if they felt unsafe. The number of subjects participating in each physical performance measure is presented in Table 1.
Table 1.
Characteristics of Subjects who Passed the Cognitive Screen at Enrollment*.
| Variable | Subjects (N=112) |
|---|---|
| Age, mean (SD) | 75.6 (10.9) |
| Male, N (%) | 38 (33.9) |
| White, N (%) | 86 (76.8) |
| Completed high school, N (%) | 70 (62.5) |
| Mini Mental State Exam, mean (SD) maximum=30 points | 24.9 (3.9) |
| Long term care program type, N (%): | |
| Program of All-Inclusive Care for the Elderly | 39 (34.8) |
| Skilled nursing facility | 36 (32.1) |
| Home-care based long-term care | 37 (33.0) |
| Berg balance scale, mean (SD) maximum=56 points | 21.8 (15.9) (N=111) |
| Six-min walk (feet), mean (SD) | 146 (190) (N=95) |
| Gait speed (m/s), mean (SD) | 0.22 (0.24) (N=97) |
| Hip strength (kg), mean (SD) | 14.4 (11.3) (N=91) |
| Knee strength (kg), mean (SD) | 14.6 (10.9) (N=91) |
| Grip strength (kg), mean (SD) | 13.4 (8.2) (N=105) |
Note: Number of participating subjects (N) varies among measures secondary to subject physical limitations and refusals.
The Berg Balance Scale was performed according to published protocols (17). The scale objectively measures balance by testing ability to change and maintain positions. Subjects are asked to perform 14 activities of increasing difficulty levels due to decreasing bases of support. Points are given for ability to accomplish movements and length of time positions are held. Scores range from 0 to 56, with higher scores reflecting better balance.
Depressive Symptoms
The Geriatric Depression Scale Short Form (GDS-15) was developed as a basic screening measure for depression in older adults (18, 19). It consists of 15 yes or no items. It was completed by 111 subjects. A score of five or greater was considered suggestive of depression. The internal consistency reliability for functionally impaired subjects (Cronbach alpha=0.749) has been described. Sensitivity and specificity of the GDS-15 to discriminate between depressed and non-depressed functionally impaired individuals are 89.5% and 65.3% respectively at a cutoff of five items (20). Reliability and validity are also previously described in nursing home residents (21).
Cognitive testing
In addition to the cognitive screen, cognitive function was assessed using the Folstein Mini-Mental State Exam (22). Scores range from zero to 30, with lower scores indicating more cognitive impairment.
Statistical Methods
Baseline descriptive characteristics of study participants were summarized using mean with standard deviation for continuous variables and frequency for categorical variables. FES scores were empirically trichotomized into low (<48), moderate (48–75), and high (76–100) scores by tertiles. Statistical significance of associations between the outcomes of FES category or fear of falling and their predictors was assessed using unpaired t-tests (continuous variables) and Pearson chi squared analysis (categorical variables). Associations were evaluated based on previous literature in other populations that showed these characteristics, or similar characteristics, to be predictors of fear of falling (4–7, 12–14, 28, 30). Statistical significance was set at P<.05. Analysis was performed with SPSS for Windows statistical software (version 14.0).
RESULTS
Baseline demographics and mean performance measures are detailed in Table 1. One hundred and eleven (98.2%) subjects reported chronic medical conditions, with 71 (62.8%) subjects reporting 4 or more conditions.
Prevalence of falls, fear and FES scores are shown in Table 2. There was no significant difference in prevalence of fear of falling between those who had fallen (36/70, 51.5%) and those who had not fallen (18/42, 42.9%; P=.374).
Table 2.
Prevalence of Falls, Fear of Falling and Fall Self-Efficacy Overall and by Program Type in New Long-Term Care Enrollees.
| Variable | All Subjects | PACE Program | Skilled Nursing Facility | Long-Term Home Health Care |
|---|---|---|---|---|
| N=112 | N=39 | N=36 | N=37 | |
| Fell in last year, N (%) | 70 (62.5) | 21 (53.8) | 23 (63.9) | 26 (70.3) |
| Falls in last year, median (range) | 1 (0–99) | 1 (0–12) | 1 (0–25) | 1 (0–99) |
| Falls in last year, mean (SD) | 2.8 (9.7) | 1.7 (2.8) | 2.4 (4.3) | 4.5 (16.1) |
| Subjects afraid of falling, N (%)* | 54 (48.2) | 12 (30.8) | 18 (50.0) | 24 (64.9) |
| Fearful with activity modification, | 41 (75.9) | 8 (66.7) | 12 (66.7) | 21 (87.5) |
| N (% of fearful subjects) | ||||
| FES, mean (SD) | 59.7 (26.7) N=108 | 68.1 (22.9) N=38 | 63.0 (30.4) N=34 | 47.6 (22.7)† N=36 |
Notes: There is a significant difference in the prevalence of fear of falling between the three programs (P=.007). The difference between the PACE and long-term home health care programs is significant (P=.003).
Mean FES score of long-term home health care subjects is significantly lower than PACE (P<.001) and skilled nursing facility subjects scores (P=.019). Differences between programs for other measures did not reach statistical significance.
FES=Falls Efficacy Scale; PACE=Program of All–Inclusive Care for the Elderly.
The prevalence of subjects falling in the prior year did not differ between LTC programs (P=.328). Prevalence of fear of falling and activity modifying fear of falling are shown in Figure 2. Prevalence of fear was significantly lower in PACE participants than in LTHHC participants (P=.003) and there was a trend towards less fear in the PACE program than in the SNF (P=.089). Activity modification by fearful subjects was comparable in all programs (P=.205).
Figure 2.
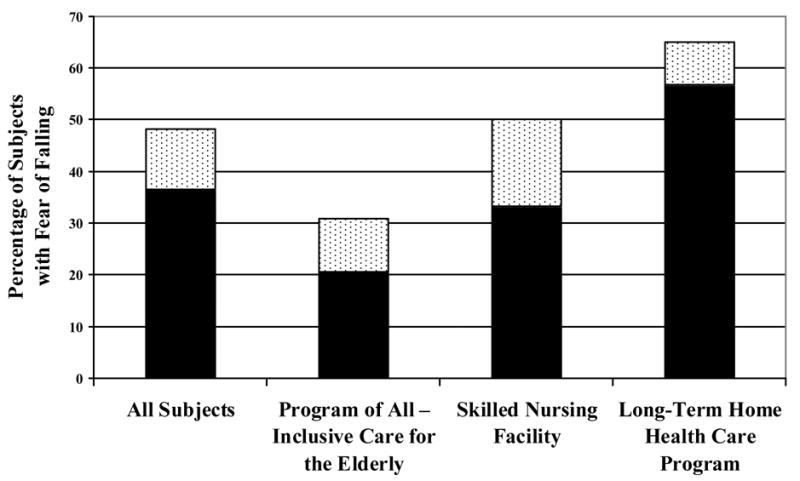
Prevalence of Fear of Falling and Activity Modification Overall and by Program Type in New Long-Term Care Enrollees, (▮ Fearful with activity modification,
 Fearful without activity modification).
Fearful without activity modification).
Associations between subject characteristics, FES scores and fear of falling are displayed in Table 3.
Table 3.
Associations between Subject Characteristics, Fall Self-Efficacy and Fear of Falling in New Long-Term Care Enrollees.
| Variable | FES Score | Fear of Falling | |||||
|---|---|---|---|---|---|---|---|
| Low (0–47) | Moderate (48–75) | High (76–100) | High vs. Low | Yes | No | ||
| N=36 | N=36 | N=36 | P value | N=54 | N=58 | P value | |
| Female, N (%) | 27 (75.0) | 22 (61.1) | 23 (63.9) | .306 | 43 (79.6) | 31 (53.4) | .003 |
| Age, mean (SD) | 74.8 (11.2) | 75.9 (10.5) | 75.6 (10.8) | .752 | 76.5 (11.7) | 74.7 (10.1) | .385 |
| MMSE, mean (SD) | 25.3 (3.9) | 24.7 (4.2) | 24.6 (3.9) | .453 | 24.4 (4.1) | 25.3 (3.8) | .221 |
| Fell in last year, N (%) | 22 (61.1) | 27 (75.0) | 18 (50.0) | .343 | 36 (56.7) | 34 (58.6) | .379 |
| Falls in last year, mean (SD) | 4.1 (16.4) | 2.3 (2.7) | 2.3 (4.7) | .520 | 4.2 (13.7) | 1.6 (2.2) | .175 |
| Fear of falling, N (%) | 26 (72.2) | 17 (47.2) | 10 (27.8) | <.001 | -- | -- | -- |
| FES, mean (SD) | 29.5 (13.5) | 59.4 (7.8) | 90.1 (6.8) | <.001 | 48.9 (26.1) N=53 | 69.9 (23.1) N=55 | <.001 |
| Positive GDS, N (%)* | 19 (52.8) N=36 | 10 (27.8) N=35 | 7 (19.4) N=36 | .003 | 23 (42.6) N=54 | 14 (24.6) N=57 | .044 |
Notes: GDS score of five or greater was considered positive.
MMSE=Mini-Mental State Exam; FES=Falls Efficacy Scale; GDS=Geriatric Depression Scale.
Subjects who reported fear of falling were more likely to report low back pain (37/54, 68.5% vs. 17/54, 17.5%; P=.030) and lower extremity arthritis (40/54, 74.1% vs. 14/54, 25.9%; P=.037). Subjects with high FES scores were least likely to report angina (2/36), as compared with those with moderate (9/36, P=.022) or low (13/36, P=.001) FES scores. No other significant relationships between fall-related self-efficacy and medical conditions were identified.
Associations between physical performance measures, FES scores and fear of falling are displayed in Table 4. Greater hip strength was measured in those with high and moderate FES scores than those with low FES scores (P<.001, P=.002, respectively). Subjects with low FES also had significantly weaker knee extension than subjects with moderate or high FES scores (P=.018, P=.006, respectively).
Table 4.
Associations between Performance Measures, Fall Self-Efficacy and Fear of Falling in New Long-Term Care Enrollees.
| Variable mean (SD) | FES Score | Fear of Falling | |||||
|---|---|---|---|---|---|---|---|
| Low (0–47) | Moderate (48–75) | High (76–100) | High vs. Low | Yes | No | ||
| N=36 | N=36 | N=36 | P value | N=54 | N=58 | P value | |
| Berg Balance Scale | 14.5 (11.7) N=36 | 19.2 (14.2) N=36 | 32.0 (16.2) N=36 | <.001 | 18.8 (13.4) N=54 | 24.7 (17.6) N=57 | .052 |
| Six-minute walk, feet | 88 (128) N=32 | 117 (191) N=32 | 244 (213) N=30 | .001 | 106 (141) N=45 | 182 (220) N=50 | .045 |
| Gait speed, m/s | 0.16 (0.23) N=32 | 0.16 (0.18) N=33 | 0.36 (0.26) N=30 | .001 | 0.19 (0.23) N=47 | 0.25 (0.25) N=50 | .235 |
| Hip strength, kg | 8.5 (9.2) N=31 | 17.1 (11.6) N=28 | 18.4 (10.6) N=31 | <.001 | 9.8 (9.2) N=42 | 18.4 (11.6) N=49 | <.001 |
| Knee strength, kg | 9.9 (9.8) N=29 | 16.7 (11.2) N=29 | 17.4 (10.3) N=32 | .006 | 10.6 (8.6) N=40 | 17.8 (11.6) N=51 | .001 |
| Grip strength, kg | 11.7 (7.3) N=33 | 13.9 (7.8) N=34 | 14.3 (9.4) N=36 | .207 | 11.9 (7.1) N=49 | 14.8 (8.9) N=56 | .077 |
Notes: FES=Falls Efficacy Scale.
DISCUSSION
This article provides information about falls and fear of falling in new enrollees in LTC that has not previously been described in the literature. The new enrollees in our study reported an annual fall rate of more than 60 percent, surpassing the 30 to 40 percent generally quoted for community dwelling older adults (6, 23–25) and the 40 percent rate cited in SNF residents (26–27). Overall, the high fall rate of our cohort likely reflects the frailty of individuals at the time of LTC enrollment and a group whose health status is in transition. It also underscores the importance of efforts to optimize safety with respect to falls during this time.
Fear of falling was also common with nearly 50 percent of new enrollees reporting fear of falling. Importantly, subjects were not simply afraid of falling. Fear influenced more than three quarters of subjects to modify their activities. A similar rate of activity restriction secondary to fear of falling has been reported in community-based seniors using home care services (28). Activity modification may lead to poor functional trajectories in these populations. Fall related self-efficacy was low compared to previously measured community groups, further demonstrating the severity of fear in new LTC enrollees (11, 29). The low FES scores of this study reflect the severity of fear in LTC enrollees during everyday tasks and this group’s high risk for associated functional declines and falls.
Our study suggests that modifiable risk factors for fear of falling and low fall related self-efficacy exist in new LTC enrollees. Hip and knee strength were associated with both low fall related self-efficacy and fear of falling. Similar findings have been reported in community dwelling older adults (13). As suggested in other populations, fall reduction interventions targeting lower extremity strength may be important in new LTC enrollees (30–32). Poor balance was associated with worse falls efficacy. Programs that improve balance, like Tai Chi, have been shown to reduce fear of falling in other populations and may be helpful to new LTC enrollees (32–35). Associations between these measures and fear of falling highlight important opportunities for rehabilitative therapy in new LTC enrollees. Similarly, associations of depression, low back pain and lower extremity arthritis with fear may inform interventions to reduce fear and falling in LTC enrollees.
Significant differences in report of fear of falling were seen in the two community based LTC programs studied, PACE and LTHHC. Nearly two-thirds of the LTHHC subjects were afraid of falling, while less than one-third of PACE subjects reported this fear. New PACE enrollees were less likely to have fallen in the preceding year and to report fear of falling and had the highest FES scores. These differences may be particularly relevant as community based falls have been identified as a strong predictor of SNF admission and presumably enrollees in community-based LTC programs would prefer to avoid institutionalization in a SNF (29, 36). The role of fear and self-efficacy in election of one LTC program rather than another may be important to understanding falls and function in LTC. The PACE program, which requires travel to a day health center on a regular basis, may be more acceptable to a patient population with less fear of falling than the LTHHC program, in which care is provided predominantly in the home.
CONCLUSION
In summary, new enrollees in LTC have high rates of fear of falling and activity modification secondary to fear. The transition into LTC represents a window of opportunity for the multidisciplinary team to intervene upon falls and fear of falling and improve safety. Modifiable risk factors like depressive symptoms, lower extremity weakness, poor balance and low back pain should be targeted by care-planning interventions.
Acknowledgments
This work was supported in part by a General Clinical Research Center (GCRC) grant, 5 M01 RR-00044 from the National Center for Research Resources, NIH. Dr. Friedman received support for this study from a K23 grant, #5K23AG19545, from the National Institute on Aging.
Footnotes
CONFLICTS OF INTEREST:
None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Committee on Redesigning Health Insurance Performance Measures, Payment, and Performance Improvement Programs. Performance measurement: Accelerating improvement. Washington, D.C: Institute of Medicine of the National Academy of Sciences; 2006. [Google Scholar]
- 2.Spillman BC, Lubitz J. New estimates of lifetime nursing home use: Have patterns of use changed? Med Care. 2002;40:965–75. doi: 10.1097/00005650-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Friedman SM, Williamson JD, Lee BH, et al. Increased fall rates in nursing home residents after relocation to a new facility. J Am Geriatr Soc. 1995;43:1237. doi: 10.1111/j.1532-5415.1995.tb07399.x. [DOI] [PubMed] [Google Scholar]
- 4.Friedman SM, Munoz B, West SK, et al. Falls and fear of falling: Which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50:1329–35. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 5.Kressig RW, Wolf SL, Sattin RW, et al. Associations of demographic, functional, and behavioral characteristics with activity-related fear of falling among older adults transitioning to frailty. J Am Geriatr Soc. 2001;49:1456–62. doi: 10.1046/j.1532-5415.2001.4911237.x. [DOI] [PubMed] [Google Scholar]
- 6.Arfken CL, Lach HW, Birge SJ, et al. The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Public Health. 1994;84:565–70. doi: 10.2105/ajph.84.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gagnon NF, Alastair JN, Devins G, et al. Affective correlates of fear of falling in elderly persons. Am J Geriatr Psychiatry. 2005;13:7–14. doi: 10.1176/appi.ajgp.13.1.7. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki MO, Yamada N, Kanamori K, et al. The relationship between fear of falling, activities of daily living and quality of life among elderly individuals. Nurs Health Sci. 2002;4:155–161. doi: 10.1046/j.1442-2018.2002.00123.x. [DOI] [PubMed] [Google Scholar]
- 9.Parry SW, Steen N, Galloway SR, et al. Falls and confidence related quality of life outcome measures in an older British cohort. Postgrad Med. 2001;77:103–8. doi: 10.1136/pmj.77.904.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lachman ME, Howland J, Tennstedt S, et al. Fear of falling and activity restriction: The survey of activities and fear of falling in the elderly (SAFE) J Gerontol B Psychol Sci Soc Sci. 1998;53:P43–50. doi: 10.1093/geronb/53b.1.p43. [DOI] [PubMed] [Google Scholar]
- 11.Cumming RG, Salkeld G, Thomas M, et al. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol A Biol Sci Med Sci. 2000;55:M299–305. doi: 10.1093/gerona/55.5.m299. [DOI] [PubMed] [Google Scholar]
- 12.Franzoni S, Rozzini R, Boffelli S, et al. Fear of falling in nursing home patients. Gerontology. 1994;40:38–44. doi: 10.1159/000213573. [DOI] [PubMed] [Google Scholar]
- 13.Delbaere K, Crombez G, Vanderstraeten G, et al. Fear-related avoidance of activities, falls and physical frailty. A prospective community-based cohort study. Age Ageing. 2004;33:368–73. doi: 10.1093/ageing/afh106. [DOI] [PubMed] [Google Scholar]
- 14.Murphy SL, Williams CS, Gill TM. Characteristics associated with fear of falling and activity restriction in community-living older persons. J Am Geriatr Soc. 2002;50:516–20. doi: 10.1046/j.1532-5415.2002.50119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eggert GM, Wamsley BR. Submitted to the Centers for Medicare and Medicaid Services. East Rochester, NY: Monroe County Long Term Care Program, Inc; December 31, 2002. A randomized controlled trial of primary and consumer-directed care for people with chronic illnesses: Final program report. Parkersburg, WV: Center for Aging and Healthcare in West Virginia, Inc. [Google Scholar]
- 16.Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45:P239–43. doi: 10.1093/geronj/45.6.p239. [DOI] [PubMed] [Google Scholar]
- 17.Berg K, Wood-Dauphinee S, Williams JI, et al. Measuring balance in the elderly: Preliminary development of an instrument. Physiother Can. 1989;41(6):304. [Google Scholar]
- 18.Sheikh JI, Yesavage JA. Geriatric depression scale (GDS): Recent evidence and development of a shorter version. In: Brink TL, editor. Clinical Gerontology: A Guide to Assessment and Intervention. New York: The Haworth Press; 1986. pp. 165–73. [Google Scholar]
- 19.Sheikh JI, Yesavage JA, Brooks JO, et al. Proposed factor structure of the geriatric depression scale. Int Psychogeriatr. 1991;3:23–8. doi: 10.1017/s1041610291000480. [DOI] [PubMed] [Google Scholar]
- 20.Freidman B, Heisel MJ, Delaven RL. Psychometric properties of the 15-item Geriatric Depression Scale in a functionally impaired, cognitively intact, community-dwelling elderly primary care patients. J Am Geriatr Soc. 2005;53:1570–76. doi: 10.1111/j.1532-5415.2005.53461.x. [DOI] [PubMed] [Google Scholar]
- 21.Koehler M, Rabinowicz T, Hirdes J, et al. Measuring depression in nursing-home residents with the MDS and GDS: An observational psychometric study. BMC Geriatric. 2005;5:1. doi: 10.1186/1471-2318-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 24.Walker JE, Howland J. Falls and fear of falling among elderly persons living in the community: Occupational therapy interventions. Am J Occup Ther. 1991;45:119–22. doi: 10.5014/ajot.45.2.119. [DOI] [PubMed] [Google Scholar]
- 25.Howland J, Peterson EW, Levin WC, et al. Fear of falling among the community-dwelling elderly. J Aging Health. 1993;5:229–43. doi: 10.1177/089826439300500205. [DOI] [PubMed] [Google Scholar]
- 26.Aronow WS, Ahn C. Association of postprandial hypotension with incidence of falls, syncope, coronary events, stroke, and total mortality at 29-month follow-up in 499 older nursing home residents. J Am Geriatr Soc. 1997;45:1051–3. doi: 10.1111/j.1532-5415.1997.tb05965.x. [DOI] [PubMed] [Google Scholar]
- 27.Nygaard HA. Falls and psychotropic drug consumption in long-term care residents: Is there an obvious association? Gerontology. 1998;44:46–50. doi: 10.1159/000021982. [DOI] [PubMed] [Google Scholar]
- 28.Fletcher PC, Hirdes JP. Restriction in activity associated with fear of falling among community-based seniors using home care services. Age Ageing. 2004;33:273–9. doi: 10.1093/ageing/afh077. [DOI] [PubMed] [Google Scholar]
- 29.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279–84. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 30.Brouwer B, Musselman K, Culham E. Physical function and health status among seniors with and without a fear of falling. Gerontology. 2004;50:135–41. doi: 10.1159/000076771. [DOI] [PubMed] [Google Scholar]
- 31.Moreland JD, Richardson JA, Goldsmith CH, et al. Muscle weakness and falls in older adults: A systematic review and meta-analysis. J Am Geriatr Soc. 2004;52:1121–9. doi: 10.1111/j.1532-5415.2004.52310.x. [DOI] [PubMed] [Google Scholar]
- 32.Schoenfelder DP, Rubenstein LM. An exercise program to improve fall-related outcomes in elderly nursing home residents. Appl Nurs Res. 2004;17:21–31. doi: 10.1016/j.apnr.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 33.Li F, Harmer P, Fisher KJ, et al. Tai chi and fall reductions in older adults: A randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60:187–94. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- 34.Wolf SL, Barnhart HX, Kutner NG, et al. Reducing frailty and falls in older persons: An investigation of tai chi and computerized balance training. J Am Geriatr Soc. 1996;44:489–97. doi: 10.1111/j.1532-5415.1996.tb01432.x. [DOI] [PubMed] [Google Scholar]
- 35.Sattin RW, Easley KA, Wolf SL, et al. Reduction in fear of falling through intense tai chi exercise training in older, transitionally frail adults. J Am Geriatr Soc. 2005;53:1168–78. doi: 10.1111/j.1532-5415.2005.53375.x. [DOI] [PubMed] [Google Scholar]
- 36.Donald IP, Bulpitt CJ. The prognosis of falls in elderly people living at home. Age Ageing. 1999;28:121–5. doi: 10.1093/ageing/28.2.121. [DOI] [PubMed] [Google Scholar]


