Abstract
Bevirimat (BVM; formerly known as PA-457) is a novel inhibitor of human immunodeficiency virus (HIV) maturation that is being developed for the treatment of HIV infection. The pharmacokinetics of this agent in healthy male volunteers were studied in a randomized, double-blind study in which the participants received single oral doses of placebo (n = 8) or escalating doses of BVM at 25, 50, 100, or 250 mg (n = 6 per dose); escalation was performed only after the pharmacokinetics and safety of the preceding dose had been evaluated. Plasma was collected over 480 h after dosing and urine was collected over 48 h after dosing for determination of the values of pharmacokinetic parameters. BVM was well absorbed after oral administration, with peak plasma concentrations being achieved 1 to 3 h after dosing. The half-life was 60 to 80 h. The exposure assessed by determination of the peak concentration and the area under the concentration-time curve was dose proportional. Single oral doses of BVM were well tolerated: there were no dose-limiting toxicities, and no serious adverse events were reported. These findings suggest that that BVM offers a favorable pharmacokinetic profile, with predictable pharmacokinetics following the oral administration of single doses. The long half-life of BVM may facilitate once-daily dosing.
Although the introduction of highly active antiretroviral therapy regimens has significantly improved the prognosis for people infected with human immunodeficiency virus (HIV) type 1 (HIV-1) (2, 9), the development of viral resistance presents a major clinical challenge. It is estimated that up to 78% of individuals with HIV-1 infection harbor drug-resistant strains (10) and that 5 to 10% of strains are resistant to all classes of reverse transcriptase and viral protease inhibitors (4). The growing problem of resistance necessitates the development of new agents and regimens for the control of HIV infection (1). One response to this need has been to investigate therapeutic targets other than reverse transcriptase and viral protease, which have traditionally been the targets of highly active antiretroviral therapy regimens.
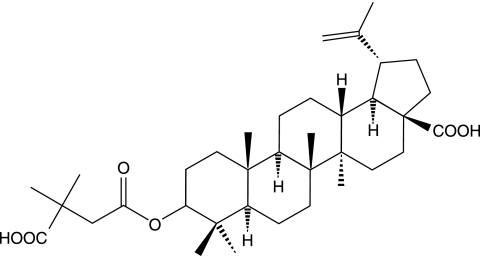
Bevirimat (BVM; formerly known as PA-457) [3-O-(3′,3′-dimethylsuccinyl)betulinic acid] (Fig. 1) is the first of a new class of antiretroviral agents that inhibit HIV-1 replication by disrupting virus maturation. BVM inhibits the final step in the Gag processing cascade, resulting in defective core condensation and the release of noninfectious virus particles from HIV-1-infected cells, thus blocking the spread of the infection to new cells (5). Due to this novel mechanism of action, BVM shows potent activity against HIV-1 strains that are resistant to all currently approved classes of antiretroviral agent (3).
FIG. 1.
Structure of BVM [3-O-(3′,3′-dimethylsuccinyl)betulinic acid].
In vitro studies have shown that BVM does not undergo oxidative metabolism in human microsomes, does not inhibit the cytochrome P450 system, and does not interact with human Pgp (6). It is a substrate for UDP-glucuronosyltransferases, and since it contains two carboxylic acid moieties and no other functional groups that are commonly conjugated with glucuronic acid, it is likely that the formation of acyl glucuronide metabolites may contribute to its elimination (13). This may result in a more favorable safety profile, with less potential for drug interactions, than those of existing antiretroviral therapies. This paper describes the first study of the safety, tolerability, and pharmacokinetics of BVM in healthy volunteers.
MATERIALS AND METHODS
The study was a double-blind, randomized, placebo-controlled, parallel-group, dose-escalation study conducted at a single center in the United States. It was conducted according to the principles of the Declaration of Helsinki and Good Clinical Practice, and the protocol was approved by the Integreview Ethical Review Board (Austin, TX).
Participants.
Male volunteers (age range, 18 to 55 years) of any race were eligible to participate in the study. Participants were required to have a body mass index (BMI) of between 18.5 and 30 kg/m2 and to be in good health, as judged by medical history, physical examination, and clinical laboratory evaluation. Participants with clinically significant medical or psychiatric conditions or abnormal laboratory test results were excluded from the study, as were those with a history of excessive alcohol consumption or drug abuse or who tested positive for hepatitis virus or HIV infection. Written informed consent was obtained from all participants prior to inclusion in the study.
Treatment.
Participants were randomized in a 2:6 ratio to receive placebo or single oral doses of BVM. BVM was given as a solution containing the di-N-methylglucamine salt in escalating doses equivalent to 25, 50, 100, and 250 mg of the free acid. The investigators were blinded to the treatment allocation (BVM or placebo) but not to the dose of BVM; doses were escalated for successive cohorts of eight participants only after the safety and pharmacokinetic data for the previous dose had been evaluated. Each dose was given, after an overnight fast of at least 8 h, as 60 ml of the oral solution, and the dosing vessel was rinsed three times with 60 ml tap water, which was consumed by the participant. A standardized meal (∼150 protein calories, ∼250 carbohydrate calories, and ∼500 to 600 fat calories) was provided 4 h after dosing. Alcohol-, caffeine-, and xanthine-containing foods or beverages were prohibited from 24 h before to 48 h after dosing. Grapefruit and grapefruit-containing juices were prohibited from 1 week before dosing until the completion of the study. The participants were asked to refrain from excessive physical exercise or contact sports during the same period. The use of any unauthorized prescription or over-the-counter medication was prohibited from 14 days prior to dosing until the completion of the study, although the participants could take acetaminophen up to 48 h before dosing. The participants were also asked to avoid the use of drugs known to inhibit or induce hepatic drug metabolism from 30 days prior to dosing. The study participants remained in the dosing unit for 48 h after dose administration and were then required to report back for blood sampling during the remainder of the study.
Pharmacokinetic analysis.
Blood samples (10 ml) were obtained via an indwelling catheter or by venipuncture prior to dosing and at 0.25, 0.5, 0.75, 1, 1.5, 2, 3, 4, 6, 8, 10, 12, 18, 24, 30, 36, 42, 48, 96, 144, 192, 240, 288, 336, 384, 432, and 480 h after dosing (or at times within 10% of those time points after 48 h). Samples were collected into heparinized tubes, and plasma was separated within 30 min of collection by centrifugation at 1,500 × g for 10 min at 4°C. Duplicate plasma samples were stored at −70°C prior to analysis.
Urine was collected over time periods of approximately 0 to 12, 12 to 24, 24 to 36, and 36 to 48 h after dosing. The urine volume and the creatinine concentration were measured, and duplicate 20-ml samples were stored at −70°C.
The concentrations of BVM in plasma and urine were measured by means of validated high-performance liquid chromatography assays with tandem mass spectrometric detection. The internal standard was 2,2-dimethylsuccinyl-4-dihydrobetulinic acid ester (DSD). The precursor/fragment ions of BVM were 583.5→455.4 m/z in heparinized plasma and acidified urine and 583.3→455.2 m/z in acidified plasma; the precursor/fragment ions of DSD were 585.3→457.3 m/z for both plasma and urine samples. The assays were validated over the range 0.02 to 60.0 μg/ml (plasma) and 100 to 40,000 ng/ml (urine). The accuracy and precision (measured as the relative standard deviation) ranged from 96.3 to 105% and 5.5 to 9.6%, respectively, in plasma and from 83.7 to 94.2% and 3.8 to 10.3%, respectively, in urine.
Since acyl glucuronides can be unstable at neutral pH (11), one plasma sample from each pair of duplicates from the participants receiving the highest dose of BVM was acidified to pH 3 to 4 by the addition of glacial acetic acid in order to stabilize any putative glucuronide conjugates of BVM. These samples were then assayed with and without enzymatic hydrolysis with β-glucuronidase for 18 h at 37°C. The concentrations of conjugated BVM were calculated as the differences in the concentrations between the hydrolyzed and the nonhydrolyzed samples. The BVM concentrations measured in acidified and hydrolyzed samples were not significantly different from those measured in acidified and nonhydrolyzed samples or nonacidified and nonhydrolyzed samples. This shows that the circulating concentrations of BVM conjugates are very low and that analysis of nonacidified, nonhydrolyzed samples accurately measures plasma BVM concentrations. Hence, all concentrations presented in this paper represent those of the free acid of BVM.
The concentrations of BVM conjugates in urine were measured as the difference between the concentrations in acidified samples with and without enzymatic hydrolysis (β-glucuronidase, 4 h at 37°C).
The values of the pharmacokinetic parameters of BVM in plasma were estimated by noncompartmental methods. Maximum concentrations in plasma (Cmaxs) and the times to the Cmaxs (Tmaxs) were derived directly from concentration-time plots. The following pharmacokinetic parameters were estimated: the area under the concentration-time curve (AUC) to the time of the last quantifiable concentration, the AUC extrapolated to infinity (AUC0-∞), the elimination rate constant (λz; determined by linear regression analysis of the terminal points of the log-linear plasma concentration-time curve), the terminal half-life [t1/2; determined as ln(2)λz]), and the apparent oral clearance (CL/F; calculated as the dose divided by AUC0-∞). The amount of BVM excreted in the urine was calculated from the urine data.
Safety analyses.
Safety was assessed by monitoring the participants for adverse events throughout the study. In addition, a physical examination was performed at the beginning of the study and at follow-up 21 days after dosing; and vital signs were measured and an electrocardiogram (ECG) and clinical laboratory testing were performed prior to dosing, at various times during the study, and at follow-up.
Statistics.
Statistical analysis was performed by using the SAS System for Windows (version 8.2; SAS Institute Inc., Cary, NC). For the pharmacokinetic analyses, plasma concentrations and pharmacokinetic parameters were summarized by dose and treatment by using descriptive statistics; missing data were omitted from these calculations. Dose proportionality was assessed by means of the following power model: log(parameter) = a + b·log(dose), where a is the intercept and b is the slope. Dose proportionality was assumed if the 95% confidence intervals for the estimate of the slope included 1.0. A two-tailed probability of 0.05 or less was regarded as statistically significant. Demographic and baseline characteristics were summarized by using descriptive statistics for continuous variables and frequency distributions for discrete variables.
Due to the variation in sampling times between 48 and 480 h (after the participants left the clinical study unit), group mean and median pharmacokinetic variables could not be calculated for discrete time points after 48 h. The pharmacokinetic parameters for individuals during the elimination phase were calculated on the basis of individual data, and summary statistics were calculated to describe the results by dose group.
All safety data were summarized by dose level. Descriptive statistics and the mean change from the baseline were determined for clinical laboratory tests, vital signs, and ECG variables.
RESULTS
A total of 32 volunteers were enrolled, all of whom completed the study. Eight participants received placebo, and 24 (six per dose level) received BVM. The demographic characteristics of the participants are summarized in Table 1.
TABLE 1.
Baseline demographic characteristics
| Treatment group (n) | Mean age ± SD (yr), range | Race (no. [%] African/Caucasian/Hispanic) | Mean ht ± SD (cm), range | Mean wt ± SD (kg), range | Mean BMI ± SD (kg/m2), range |
|---|---|---|---|---|---|
| Placebo (8) | 30.4 ± 8.9 (20-46) | 4/4/0 (50/50/0) | 181.3 ± 6.9 (170.2-193.0) | 89.3 ± 16.0 (59.1-108.6) | 27.0 ± 3.7 (19.2-30.0) |
| BVM, 25 mg (6) | 33.3 ± 11.0 (18-46) | 3/2/1 (50/33/16.7) | 176.1 ± 8.5 (165.1-188.0) | 87.0 ± 10.2 (69.1-99.5) | 28.1 ± 2.7 (24.1-30.0) |
| BVM, 50 mg (6) | 29.5 ± 14.6 (19-54) | 0/5/1 (0/83.3/16.7) | 174.8 ± 6.5 (170.2-185.4) | 84.1 ± 7.0 (78.6-95.0) | 27.6 ± 2.6 (22.9-30.2) |
| BVM, 100 mg (6) | 31.0 ± 12.9 (20-49) | 1/5/0 (16.7/83.3/0) | 177.0 ± 8.3 (162.6-185.4) | 77.7 ± 10.6 (60.9-91.4) | 24.8 ± 3.0 (21.7-28.9) |
| BVM, 250 mg (6) | 33.8 ± 9.2 (20-43) | 3/3/0 (50/50/0) | 174.8 ± 5.7 (167.6-182.9) | 77.8 ± 13.5 (64.1-96.4) | 25.3 ± 3.8 (20.3-30.5) |
| Total (32) | 31.5 ± 10.7 (18-54) | 11/19/2 (34.4/59.4/6.3) | 177.1 ± 7.2 (162.6-193.0) | 83.5 ± 12.4 (59.1-108.6) | 26.6 ± 3.3 (19.2-30.5) |
Pharmacokinetics.
There were no significant differences between the mean BVM concentrations obtained from acidified plasma samples (hydrolyzed and nonhydrolyzed) and nonacidified plasma samples. Thus, the amount of circulating BVM glucuronides was low or nonexistent, and analysis of nonacidified plasma samples was used to quantitate BVM.
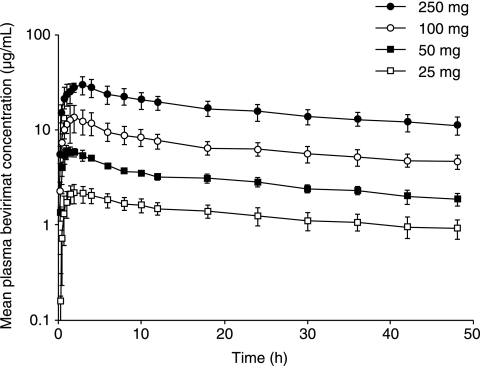
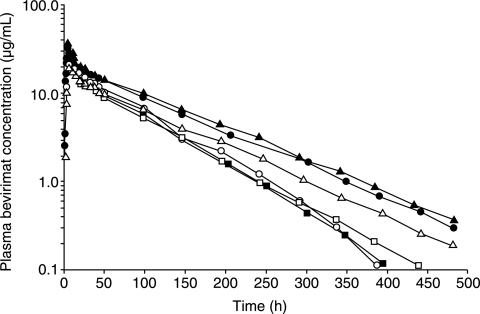
BVM was rapidly absorbed after oral administration: in all participants, detectable concentrations were present in the plasma within 15 min after administration and peak concentrations were reached within 1 to 3 h. The mean concentration-time profiles to 48 h for the four doses of BVM are shown in Fig. 2; the exact timing of collection of the samples obtained after 48 h varied between participants (but were within 10% of the specified dosing interval) and therefore are not summarized with descriptive statistics. Data for up to at least 336 h were available for 19 of 24 of the study participants, and data for the full 480-h period were available for 12 of 24 subjects. All participants had measurable concentrations of BVM in their final sample, and the observed data represented more than 97% of the AUC0-∞ values for all participants. Inspection of the individual concentration-time profiles for each participant did not reveal any secondary peaks of BVM that would be consistent with the enterohepatic circulation of glucuronide conjugates; Fig. 3 shows the concentration-time profiles for the duration of the study for participants who received the 250-mg dose as examples of the individual plots obtained.
FIG. 2.
Mean plasma concentration-time profiles (±standard deviation) to 48 h following the administration of single oral doses of BVM at 25, 50, 100, and 250 mg.
FIG. 3.
Concentration-time profiles for participants who received BVM at 250 mg.
The values of the pharmacokinetic parameters for BVM in plasma are summarized in Table 2. The median Tmax ranged from 1.0 to 2.5 h across the dose groups. The mean t1/2 ranged from 58 to 80 h, and the mean CL/F ranged from 1.55 to 2.11 ml/h/kg.
TABLE 2.
Pharmacokinetic parameters of BVM in plasmaa
| Dose | AUC0-∞ (μg·h/ml)b | AUC0-∞ (μg·h/ml) (normalized)c | Cmax (μg/ml) | Cmax (μg/ml) (normalized)c | Tmax (h) | t1/2 (h) | CL/F (ml/h/kg) |
|---|---|---|---|---|---|---|---|
| 25 | 151.2 (102.5-190.2) | 170.2 (127.0-223.8) | 2.24 (1.75-3.02) | 2.8 (2.1-3.9) | 1.75 (1.0-3.0) | 55.82 (49.74-72.27) | 173.36 (135.64-251.72) |
| 50 | 312.1 (258.6-443.4) | 362.1 (281.3-552.5) | 6.06 (5.68-7.21) | 7.3 (6.2-7.9) | 1.0 (1.0-2.0) | 56.69 (50.33-85.66) | 165.34 (116.36-199.57) |
| 100 | 982.8 (592.7-1,117.4) | 1,014.0 (682.7-1,294.0) | 13.65 (8.65-22.60) | 14.9 (10.0-19.6) | 2.0 (1.0-3.0) | 75.39 (62.72-99.52) | 105.18 (92.36-174.11) |
| 250 | 1,795.7 (1,433.9-2,793.2) | 2,221.8 (1,556.3-2,513.0) | 30.05 (25.50-38.40) | 31.1 (27.1-44.2) | 2.5 (1.0-3.0) | 69.00 (54.29-82.46) | 145.68 (93.66-182.44) |
Data are presented as median (range); n = 6 for all dosage groups.
Percentage of AUC extrapolated to infinity was <3% in all participants.
Adjusted for the target dose in a 70-kg subject.
Due to the variability in subject body weight within and across cohorts, Cmax and AUC0-∞ were normalized to a body weight of 70 kg to assess the relationship between dose and exposure (Table 2). Doubling of the dose from 25 mg to 50 mg resulted in an approximately 2.2-fold increase in the mean normalized AUC0-∞ and a 2.6-fold increase in the mean normalized Cmax, while a 4-fold increase in dose from 25 mg to 100 mg resulted in an approximately 5.5-fold increase in the mean normalized AUC0-∞ and Cmax, and a 10-fold increase in dose from 25 mg to 250 mg resulted in an approximately 12-fold increase in the mean normalized AUC0-∞ and Cmax. The linear test for dose proportionality showed that increases in the normalized Cmax (mean ± standard error slope, 1.07 ± 0.05 μg/ml; 95% confidence interval = 0.95, 1.18) and AUC0-∞ (mean ± standard error slope, 1.10 ± 0.06 μg·h/ml; 95% confidence interval = 0.98, 1.22) were dose proportional.
The measurement of unconjugated and conjugated BVM in urine samples from subjects in the highest-dose group (250 mg) accounted for approximately 0.82% of the administered dose with collections to 48 h. As a result, no formal estimation of renal clearance was done.
Safety and tolerability.
All doses of BVM were well tolerated. A total of 18 treatment-emergent adverse events were reported by seven participants receiving BVM (29.2%) and four placebo-treated participants (50%); within the BVM groups, the numbers of participants reporting treatment-emergent adverse events were one each (16.7%) with the 25- and 50-mg doses, three (50%) with the 100-mg dose, and two (33.3%) with the 250-mg dose. Headache was the most frequently reported adverse event, being reported by four participants receiving BVM and one participant receiving placebo, followed by pharyngitis in two participants receiving BVM. All adverse events were mild in severity. No serious adverse events were reported, and no participants discontinued taking the study drug due to adverse events. Six adverse events (33.3%) were considered drug related. There were sporadic elevations in clinical laboratory variables, but none of the abnormal laboratory values were considered clinically significant and none were reported to be adverse events. There were no clinically relevant changes in vital signs, ECGs, or physical examinations.
DISCUSSION
This study showed that the oral administration of BVM in humans resulted in plasma levels that increased with dose. Exposure to BVM based on Cmax and AUC was dose proportional across all doses studied. The protein binding-adjusted 90% inhibitory concentration of BVM is ∼2.3 μg/ml (7), and the Cmaxs of the two higher doses studied exceeded this value for at least 48 h following dose administration.
Compliance with complicated multidrug antiviral regimens is a major issue in the successful treatment of HIV. Effective antiviral medications that can be administered once daily should result in increased compliance, an enhanced quality of life, and improved treatment outcomes. The long t1/2 observed following oral dosing makes BVM a potential candidate for once-daily dosing. This long t1/2 suggests that accumulation in the range of three- to fivefold is likely to occur during regular dosing (7, 12) and is consistent with the extensive protein binding of BVM in plasma. Plasma protein binding is also compatible with the low levels of glucuronidation and urinary excretion of BVM observed in this study.
BVM was well tolerated by the subjects in all dose groups when it was administered as single oral doses. There were no dose-limiting toxicities, and no serious adverse events were reported. No clinically relevant findings in clinical laboratory values, vital signs, ECGs, or physical examinations were noted during the study.
The safety profile and potential for drug interactions are also important aspects of multidrug antiviral regimens. In vitro studies have shown that BVM does not undergo oxidative metabolism in human liver microsomes, does not inhibit the cytochrome P450 system, and does not interact with human Pgp (6). BVM has been shown to be glucuronidated in the rat (9), and hence, one objective of this study was to determine the concentrations of putative BVM glucuronides in human plasma and urine following oral dosing. The results showed that the levels of glucuronidated BVM in plasma are either extremely low or nonexistent in humans. A small fraction of the dose (less than 1%) was measurable in urine as putative BVM glucuronides, whereas unconjugated BVM was unmeasurable in urine; thus, renal clearance appears to be insignificant for the elimination of single doses of BVM. BVM glucuronides may be excreted in bile, but further in vivo studies are required to fully define the metabolism and excretion of BVM.
In summary, the pharmacokinetics of BVM following the oral administration of single doses are predictable in healthy volunteers, and its long t1/2 may support once-daily dosing (8). The good safety profile of BVM seen after the administration of single oral doses is also encouraging. These issues are important when drugs are selected for inclusion in multidrug antiviral regimens for the treatment of HIV infection, and these data warrant further investigation of BVM in patients with HIV infection.
Acknowledgments
Panacos Pharmaceuticals, Inc., sponsored and funded the research described in this report.
We gratefully acknowledge the contributions of Buffalo Clinical Research Center, Buffalo, NY, and Quintiles Inc., Kansas City, MO. We thank M. Shaw for his assistance in the generation of the manuscript.
Footnotes
Published ahead of print on 18 June 2007.
REFERENCES
- 1.Blaise, P., P. Clevenbergh, D. Vaira, M. Moutschen, and P. Dellamonica. 2002. HIV resistance to antiretroviral drugs: mechanisms, genotypic and phenotypic resistance testing in clinical practice. Acta Clin. Belg. 57:191-201. [DOI] [PubMed] [Google Scholar]
- 2.Hogg, R. S., K. V. Heath, B. Yip, K. J. Craib, M. V. O'Shaughnessy, M. T. Schechter, and J. S. Montaner. 1998. Improved survival among HIV-infected individuals following initiation of antiretroviral therapy. JAMA 279:450-454. [DOI] [PubMed] [Google Scholar]
- 3.Kilgore, N., M. Reddick, M. Zuiderhof, F. Li, Y. Abdul, C. Matallana, D. Zoumplis, A. Castillo, K. Salzwedel, and C. Wild. 2006. Abstr. 13th Conf. Retrovir. Opportunist. Infect., abstr. 509.
- 4.LaBonte, J., J. Lebbos, and P. Kirkpatrick. 2003. Enfuvirtide. Nat. Rev. Drug Discovery 5:345-346. [DOI] [PubMed] [Google Scholar]
- 5.Li, F., R. Goila-Gaur, K. Salzwedel, N. R. Kilgore, M. Reddick, C. Matallana, A. Castillo, D. Zoumplis, D. E. Martin, J. M. Orenstein, G. P. Allaway, E. O. Freed, and C. T. Wild. 22 October 2003, posting date. A new class of potent HIV inhibitors disrupts core condensation by targeting a late step in gag processing. Proc. Natl. Acad. Sci. USA doi: 10.1073/pnas.2234683100. [DOI] [PMC free article] [PubMed]
- 6.Martin, D. E., P. Smith, R. Goila-Gaur, K. Salzwedel, F. Li, N. Kilgore, M. Reddick, C. Matallana, A. Castillo, D. Zoumplis, G. Allaway, E. Freed, and C. Wild. 2004. Abstr. 11th Conf. Retrovir. Opportunist. Infect., abstr. 545.
- 7.Martin, D. E., C. H. Ballow, R. Blum, J. Doto, C. T. Wild, and G. P. Allaway. 2005. Abstr. 12th Conf. Retrovir. Opportunist. Infect., abstr. 551.
- 8.Molina, J. M., G. Peytavin, S. Perusat, C. Lascoux-Combes, D. Sereni, W. Rozenbaum, and G. Chene. 2004. Pharmacokinetics of emtricitabine, didanosine and efavirenz administered once-daily for the treatment of HIV-infected adults (pharmacokinetic substudy of the ANRS 091 trial). HIV Med. 5:99-104. [DOI] [PubMed] [Google Scholar]
- 9.Palella, F. J., Jr., K. M. Delaney, A. C. Moorman, M. O. Loveless, J. Fuhrer, G. A. Satten, D. J. Aschman, S. D. Holmberg, et al. 1998. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N. Engl. J. Med. 338:853-860. [DOI] [PubMed] [Google Scholar]
- 10.Richman, D., S. Morton, T. Wrin, N. Hellmann, S. Berry, F. Shapiro, and S. Bozzette. 2004. The prevalence of antiretroviral drug resistance in the United States. AIDS 18:1393-1401. [DOI] [PubMed] [Google Scholar]
- 11.Smith, P. C., J. Hasegawa, P. N. J. Langendijk, and L. Z. Benet. 1985. Stability of acyl glucuronides in biological fluids: studies with zomepirac. Drug Metab. Dispos. 13:110-112. [PubMed] [Google Scholar]
- 12.Smith, P. F., A. Ogundele, A. Forrest, and D. E. Martin. 2005. Abstr. 45th Intersci. Conf. Antimicrob. Agents Chemother., abstr. A-1149.
- 13.Wen, Z., S. T. Stern, D. E. Martin, K. H. Lee, and P. C. Smith. 2006. Structural characterization of anti-HIV drug candidate PA-457 [3-O-(3′,3′-dimethylsuccinyl)-betulinic acid] and its acyl glucuronides in rat bile and evaluation of in vitro stability in human and animal liver microsomes and plasma. Drug Metab. Dispos. 34:1436-1442. [DOI] [PubMed] [Google Scholar]