Abstract
Azoles are extensively applied in agriculture and medicine, and a relationship between the development of azole resistance in agriculture and the development of azole resistance in clinical practice may exist. The maize pathogen Colletotrichum graminicola, causing cutaneous mycosis and keratitis, has been used to investigate the acquisition of resistance to an agricultural azole and the resulting cross-resistance to various medical antifungal agents. Azole-adapted strains were less sensitive to all azoles tested but showed increased sensitivity to caspofungin, amphotericin B, and nystatin. Viability staining and infection assays with excised human skin confirmed these data.
Five plant-pathogenic Colletotrichum species, including Colletotrichum graminicola, have been reported to cause cutaneous phaeohyphomycosis and keratitis in humans and are of clinical relevance (2, 8, 9). Most Colletotrichum crassipes, C. gloeosporioides, C. coccodes, and C. dematium strains isolated from infected tissue displayed a major degree of resistance to all azoles tested (3).
In modern agriculture, Colletotrichum species have been implicated in anthracnose plant diseases worldwide, with substantial economical losses (7). Among other antifungal agents, azoles have been used extensively to control Colletotrichum species (12). Azoles differing in structure but exhibiting the same mode of action are used to treat both fungal diseases of plants and medical mycoses. As keratitis caused by Colletotrichum infection occurs primarily after injury by plant material (8, 9, 19), it is tempting to speculate that azole-resistant strains isolated from human tissues may have developed in fungicide-treated fields (see the report on azole resistance published by the scientific steering committee of the European Commission [http://ec.europa.eu/food/fs/sc/ssc/out278_en.pdf]). As Colletotrichum species are exposed to azoles in agricultural environments and are of clinical relevance, these pathogens are well suited to investigate the acquisition of resistance to agricultural azoles and the resulting cross-resistance to antifungal agents of various different chemical classes and modes of action used in medicine.
MATERIALS AND METHODS
Cultivation of C. graminicola and adaptation to tebuconazole.
Wild-type C. graminicola isolate CgM2 was cultivated as described previously (24).
To adapt C. graminicola to tebuconazole, 1 × 106 conidia were inoculated into 50 ml complete medium (CM) (15) and incubated in darkness at 23°C for 7 days. Cultures were then transferred into fresh liquid CM with increasing tebuconazole concentrations (1 μg ml−1 for 24 h, 5 μg ml−1 for 96 h, and 20 μg ml−1 for 1 h). The mycelium was blended (Ultra Turrax; IKA Labortechnik, Staufen, Germany) at level 5 for 30 s, further cultivated on solidified CM containing 5 μg tebuconazole ml−1 and 8 μg tebuconazole ml−1 for 4 weeks each, and maintained on CM plates containing 30 μg tebuconazole ml−1.
Quantitative determination of drug sensitivity.
Radial growth rates of nonadapted and matched, adapted isolates were determined in the presence of different agricultural and medical antifungal agents, i.e., the azoles tebuconazole (Bayer Cropscience GmbH, Langenfeld, Germany), bifonazole (Bayer Vital GmbH, Leverkusen, Germany), clotrimazole and miconazole (Fagron GmbH & Co. KG, Barsbüttel, Germany), itraconazole (Janssen-Cilag, Neuss, Germany), voriconazole (Pfizer Pharma GmbH, Karlsruhe, Germany), prochloraz (BASF AG, Ludwigshafen, Germany), ketoconazole (PKH Halle GmbH, Halle, Saale, Germany), the strobilurin picoxystrobin (Syngenta Agro GmbH, Maintal, Germany), the polyenes amphotericin B (Sigma-Aldrich-Fluka, Taufkirchen, Germany) and nystatin (PKH Halle GmbH, Halle [Saale], Germany), the thiocarbamate tolnaftat (Riemser Arzneimittel AG, Greifswald, Germany), the pyridone cyclopiroxolamine (PKH Halle GmbH, Germany), the morpholine amorolfine (Galderma Laboratorium GmbH, Düsseldorf, Germany), the benzofurane griseofulvin (PKH Halle GmbH, Halle [Saale], Germany), and the echinocandin caspofungin (Cancidas; MSD Sharp & Dome, Haar, Germany). With the exception of the echinocandin and polyenes, drugs were dissolved in 12% (wt/vol) Cremophor EL (Sigma-Aldrich-Fluka, Taufkirchen, Germany) and added to CM at different concentrations (0, 0.005, 0.01, 0.025, 0.05, 0.1, 0.25, 0.5, 1, and 2.5 μg ml−1); caspofungin, amphotericin B, and nystatin and were dissolved in distilled water and added to CM plates at 0.00025 and 0.0005 μg ml−1 and the concentrations given above. In plates containing caspofungin, glucose was replaced by sucrose (10 mg ml−1). Control plates contained all ingredients except the antifungal agent to be tested. Plates were incubated at 23°C in darkness, and colony diameters were measured 3 and 6 days postinoculation.
Analyses of confidence intervals (α = 0.05), logit transformation, and linear regression were done as described previously (21).
Microscopy and viability assays.
Light microscopy was performed with a Nikon Eclipse 600 epifluorescence microscope (Nikon GmbH, Düsseldorf, Germany) as described previously (21). The fluorescence dye FUN-1 (Invitrogen GmbH, Karlsruhe, Germany) was used for viability assays (14). Briefly, mycelia grown in liquid CM containing 0, 0.0025, 0.025, 0.25, 2.5, 3.5, and 5 μg tebuconazole, bifonazole, or caspofungin ml−1 for 3 days were incubated in a solution containing 50 μM FUN-1, 2% (wt/vol) glucose, and 10 mM HEPES (pH 7.2) at 27°C for 1 h. Fluorescence microscopy was done with a GFP-LP filter (EX 460 to 500, DM 505, and BA 510). For negative controls, hyphae were incubated with ethanol (70% [vol/vol] for 30 min) prior to staining with FUN-1.
Pathogenesis of tebuconazole-adapted and nonadapted C. graminicola isolates on excised skin and efficacies of antifungal agents.
To investigate fungicide efficacies, infection assays were performed with tebuconazole-adapted and nonadapted isolates of C. graminicola on excised human skin, in agreement with the local ethics committee. Tissue sections came from reduction mammoplasty. Circular pieces of skin (diameter, 20 mm) were randomly punctured with prick needles (Allergopharma KG, Reinbek, Germany) (15 to 20 wounds per piece) and inoculated with 100 μl of a suspension containing 106 conidia ml−1. The skin specimens were placed onto filter gauze and incubated in a glass Franz diffusion cell (see Fig. S1 in the supplemental material) at 32°C, with the lower side of the skin on the filter gauze directly contacting isotonic NaCl solution. To assess drug efficacies, skin specimens from one donor were used, with three pieces of skin for controls without fungicide and for each fungicide concentration (50% effective dose [ED50], ED90, and 2× ED90). Inoculated skin was incubated for 4 days maximally. For histological analyses, three biopsies (diameter, 6 mm) were taken from the center of the infected skin, frozen at −70°C, and dissected vertically in a refrigeration microtome (Frigomobil; Jung-Leica, Bensheim, Germany).
Fungal chitin was stained by incubating microtome sections with the fluorescent brightener Uvitex 2B (6). Fluorescence or bright-field microscopy was done with a Nikon (Düsseldorf, Germany) Eclipse 600 epifluorescence microscope. For epifluorescence microscopy, a UV2A filter block (EX 330 to 380, DM 400, and BA 420; Nikon, Düsseldorf, Germany) was used. The area covered by fluorescing fungal hyphae was measured using the program Lucia 4.61 (Nikon GmbH, Düsseldorf, Germany).
Uvitex 2B-stained sections were fixed in 10% (vol/vol) formalin for 24 h, subjected to periodic acid-Schiff staining, and embedded in paraffin. Micrographs of Uvitex 2B- and periodic acid-Schiff-stained sections were merged by using the program Adobe Photoshop (Adobe Systems GmbH, Munich, Germany).
RESULTS
In order to test whether or not C. graminicola can adapt to an azole routinely used in agriculture, wild-type strain CgM2 was cultivated with stepwise increasing tebuconazole concentrations. Successful adaptation was reflected by increased rates of radial growth of adapted strains in the presence of increasing tebuconazole concentrations (see Fig. S2A in the supplemental material). Tebuconazole adaptation resulted in a 7-fold-increased ED50 and 27-fold-increased ED90 for this fungicide (Table 1; see Fig. S2A, inset, in the supplemental material). Even at 30 ppm tebuconazole, adapted strains, but not the nonadapted strains, were able to grow (see Fig. S2B in the supplemental material). Prochloraz, another agricultural C14-demethylation inhibitor tested, showed a higher efficacy than tebuconazole, but tebuconazole adaptation resulted in a 2.75-fold-increased ED50 and an 8-fold-increased ED90 for prochloraz (Table 1). Tebuconazole-adapted strains also showed cross-resistance to all medical azoles tested. Comparison of ED50 and ED90 values showed that (with the exception of clotrimazole sensitivity at the ED50 level) sensitivities to itraconazole, voriconazole, bifonazole, clotrimazole, miconazole, and ketoconazole were significantly (α = 0.05) reduced in tebuconazole-adapted strains (Table 1).
TABLE 1.
Fungicide efficacies for tebuconazole-adapted and nonadapted control strains of C. graminicolaa
| Class | Compound | Nonadapted
|
Adapted
|
||
|---|---|---|---|---|---|
| ED50 | ED90 | ED50 | ED90 | ||
| Azoles (triazoles) | Tebuconazole | 0.059 ± 0.004 | 0.504 ± 0.101 | 0.423 ± 0.056* | 13.534 ± 2.854* |
| Itraconazole | 0.007 ± 0.001 | 1.351 ± 0.041 | 0.014 ± 0.002* | 8.848 ± 1.183* | |
| Voriconazole | 0.018 ± 0.001 | 0.228 ± 0.018 | 0.045 ± 0.002* | 1.328 ± 0.175* | |
| Azoles (imidazoles) | Prochloraz | 0.004 ± 0.001 | 0.087 ± 0.023 | 0.011 ± 0.004* | 0.720 ± 0.129* |
| Bifonazole | 0.148 ± 0.018 | 1.958 ± 0.662 | 0.330 ± 0.058* | 4.892 ± 1.484* | |
| Clotrimazole | 0.128 ± 0.072 | 2.440 ± 0.584 | 0.145 ± 0.035 | 6.485 ± 2.690* | |
| Miconazole | 0.028 ± 0.002 | 1.327 ± 0.338 | 0.048 ± 0.003* | 4.386 ± 1.705* | |
| Ketoconazole | 0.115 ± 0.032 | 1.492 ± 0.344 | 0.552 ± 0.037* | 12.419 ± 1.306* | |
| Morpholine | Amorolfine | 0.030 ± 0.001* | 0.347 ± 0.033 | 0.023 ± 0.001 | 0.360 ± 0.024 |
| Strobilurin | Picoxystrobin | 0.006 ± 0.003 | 0.148 ± 0.040 | 0.026 ± 0.003 | 1.041 ± 0.435* |
| Thiocarbamate | Tolnaftate | 0.582 ± 0.098 | 104.107 ± 27.67 | 0.537 ± 0.0169 | 98.710 ± 31.089 |
| Pyridone | Cyclopiroxolamine | 9.829 ± 0.593* | 64.842 ± 13.209 | 3.671 ± 0.177 | 54.616 ± 4.127 |
| Benzofurane | Griseofulvin | 0.607 ± 0.400 | 5.503 ± 0.902 | 0.051 ± 0.012 | 5.839 ± 0.523 |
| Polyenes | Amphotericin B | 0.030 ± 0.002* | 2.147 ± 0.250* | 0.007 ± 0.001 | 0.873 ± 0.185 |
| Nystatin | 0.030 ± 0.001* | 2.412 ± 0.135* | 0.023 ± 0.001 | 0.896 ± 0.272 | |
| Echinocandin | Caspofungin | 0.032 ± 0.002* | 1.281 ± 0.104* | 0.006 ± 0.001 | 0.770 ± 0.178 |
Asterisks indicate significantly (α = 0.05) increased ED50 or ED90 values.
Furthermore, we tested for cross-resistance of tebuconazole-adapted strains to drugs showing modes of action differing from that of azoles. Tebuconazole-adapted strains tolerated higher concentrations of the agricultural antifungal agent picoxystrobin than the nonadapted control, as reflected by a fourfold-increased ED50 and a sevenfold increase in the ED90 (Table 1). Interestingly, the tebuconazole-adapted strains showed increased sensitivity to the chelator cyclopiroxolamine at low (ED50) but not at elevated (ED90) drug concentrations.
The expression of efflux transporter genes has been shown to contribute to resistance against antifungal agents in several plant pathogens and in fungi infecting humans (5). Using drugs that are active on targets in the plasma membrane that are accessible directly from the periplasm,we expected to find no statistically relevant differences between the sensitivity levels of tebuconazole-adapted strains and those of nonadapted strains of C. graminicola. Surprisingly, the tebuconazole-adapted strains showed a significantly increased sensitivity to the β-1,3-glucan synthase inhibitor caspofungin and to both polyenes tested (α = 0.05) (Table 1).
As radial growth assays do not allow discrimination between hyphal death and inactivity, fluorescence microscopy with the viability dye FUN-1 was performed (14), and Nomarski microscopy was used to evaluate cell wall rigidity after the application of different caspofungin concentrations (see Fig. S3 in supplemental material). In summary, these studies showed that tebuconazole-adapted strains were less sensitive to the medical azole bifonazole than the nonadapted strain, as cell death occurred at higher drug concentrations (not shown). In contrast, hyphae of tebuconazole-adapted strains were more sensitive to the β-1,3-glucan synthase inhibitor than those of the nonadapted control strain. Both cell death and cell wall weakening, i.e., severe swellings, occurred at lower drug concentrations in adapted strains than in the nonadapted strain (see Fig. S3 in the supplemental material). Drug sensitivity data obtained by viability staining clearly supported those obtained by radial growth assays (Table 1; see Fig. S2 and S3 in the supplemental material).
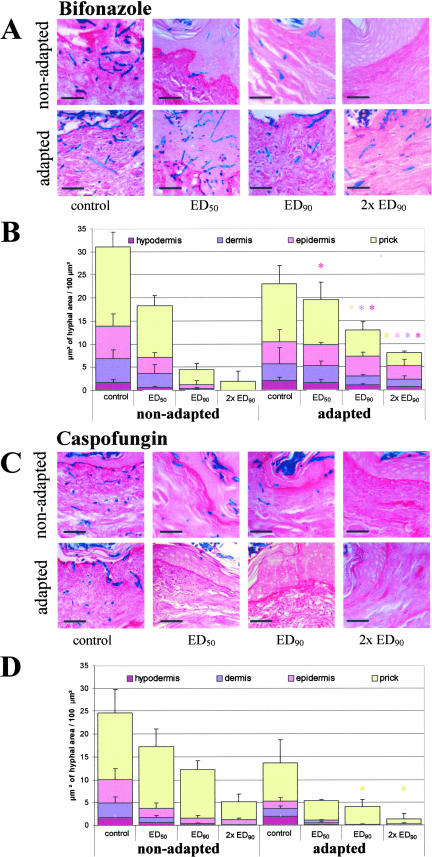
Compared with drug sensitivity quantification by growth assays, sensitivity to an antifungal agent and fitness of a pathogen may be modified under conditions of pathogenesis, as infection hyphae (16) rather than vegetative hyphae are evaluated. Therefore, we performed infection assays on excised human skin in the presence of different concentrations of bifonazole and caspofungin (Fig. 1). While infection of unwounded skin was never observed, invasive growth was initiated immediately after wounding (not shown). In the absence of drugs, extensive hyphal growth was found in the epidermis, dermis, and hypodermis (controls) (Fig. 1A and C) within the time frame of the experiment, i.e., 4 days. Nonadapted strains appeared to colonize the epidermis and dermis slightly more efficiently than the azole-adapted strain (Fig. 1A and C, compare control of nonadapted and adapted strains). Quantitative data, however, showed that the differences between the strains were not significant, and a fitness penalty could therefore not be found in infection assays. Also, in radial growth assays, only a minor fitness penalty of tebuconazole-adapted strains was observed (77.1% ± 14.0% of the nonadapted control). Bifonazole application affected invasive growth of the nonadapted strain more drastically than the tebuconazole-adapted strain (Fig. 1A), which colonized the epidermis, dermis, and hypodermis more efficiently at all drug concentrations tested (Fig. 1B). At the twofold ED90, some hyphae of the nonadapted strain grew in the wound inflicted, but invasive growth in the tissue was not observed (Fig. 1A and B). In contrast, at that concentration, tebuconazole-adapted strains showed significant hyphal growth even in the hypodermis. In the presence of caspofungin, the nonadapted strain colonized the skin at drug concentrations corresponding to the ED50, and some hyphae were found in the epidermis and dermis at the ED90 (Fig. 1C and D). Even at the twofold ED90, some growth was observed in the epidermis. Interestingly, the azole-adapted strains were clearly more affected by the β-1,3-glucan synthase inhibitor than the nonadapted control strain. At the ED90, no hyphae of the azole-adapted strains were found in the epidermis and other dermal layers (Fig. 1C and D). The fungicide sensitivity data obtained from skin infection assays clearly support those obtained from radial growth assays and viability staining.
FIG. 1.
Fungicide efficacy in skin infection assays. Wounded skin was inoculated with conidia of C. graminicola, and infections were monitored in the absence (control) or presence of different drug concentrations (ED50, ED90, or twofold ED90). Fungicides tested were bifonazole (A and B) and caspofungin (C and D). In micrographs (A and C), hyphae appear blue due to Uvitex-2B staining. Quantitative data (B and D) represent the portion of hyphal area over the skin section. Asterisks indicate statistically significant differences (α = 0.05). Bars represent 20 μm.
DISCUSSION
Fungal infections of humans have become more prevalent during the past two decades because therapeutic advances have allowed the survival of an increasing number of immunocompromised patients. Concomitantly, resistance to antifungal drugs has become a serious clinical problem. As azoles are used abundantly in agriculture, a direct relationship with developments of azole resistance in clinical environments has been proposed in scientific and political discussions (11) (http://ec.europa.eu/food/fs/sc/ssc/out278_en.pdf).
Ideally, this relationship can be studied best by using a pathogenic fungus capable of infecting both plants and humans (17). Although Colletotrichum infections in humans are rare, a growing body of literature shows that Colletotrichum species, formerly known exclusively as plant pathogens, have gained attention as causal agents of human mycoses (2, 3, 8, 9, 19, 22). Case reports indicated that several isolates of these pathogens exhibit resistance to single or multiple drugs (see, e.g., references 9 and 19), and it is tempting to speculate that drug resistance had been acquired in agricultural environments.
The maize anthracnose fungus C. graminicola represents an excellent model system to study the acquisition of azole resistance and to investigate whether isolates that are resistant to an agricultural azole show cross-resistance to azoles and antifungal agents of other chemical classes used in medicine. In agreement with reports on the development of fungicide resistance (4), our in vitro studies have shown that C. graminicola is able to efficiently adapt to azoles, and strains adapted to tebuconazole were less sensitive to all agricultural and medical azoles tested than the nonadapted control strain. Likewise, azole cross-resistance was observed between yeast isolates from the oropharynx of human immunodeficiency virus-infected patients and from environmental strains against medical and agricultural azole drugs (18).
As hyphae from fungal infections clearly differ from vegetative hyphae (16), we assessed drug efficacies in an experimental infection system with excised human skin. Radial growth assays showed that the ED90 of tebuconazole-adapted strains of C. graminicola is well above serum concentrations reported for some azoles (23, 25). In agreement with data from radial growth assays, extensive skin colonization by the azole-adapted strains was observed at the ED90 and twofold ED90 of bifonazole. These data are also in agreement with data from viability staining of azole-adapted hyphae (not shown). Also, the serum concentrations reported for amphotericin B (1) were clearly below the ED90 value measured for tebuconazole-adapted C. graminicola strains.
Interestingly, tebuconazole-adapted strains were more sensitive to caspofungin than the nonadapted control strain. The serum concentration of this drug determined in mice (10) exceeded the ED90 value of nonadapted (less sensitive) C. graminicola strains by more than twofold and that of the azole-adapted strain by fourfold. As demonstrated by infection data on excised human skin (this study), these concentrations should be fully sufficient to prevent hyphal growth in the tissue. In accordance with our studies, the staggered administration of an azole and caspofungin has been reported to increase drug efficacy (13, 20).
Although studies presented here and those of others (see, e.g., reference 4) indicate that the treatment of pathogenic fungi with sublethal azole concentrations may lead to the development of resistance to these drugs, no evidence for a direct relationship between the development of drug resistance in agricultural practice and the development of drug resistance in clinical practice has yet been presented. A strong argument against such a relationship is provided by comparing fungicide application rates in agricultural practice in the European Union and those in the United States. Almost half of the acreage of the total European Union under cereals and grapevine is treated with azoles annually, compared to less than 5% of the total crop area treated with these fungicides in the United States. Strikingly, in spite of this difference, there is no difference in the prevalence of resistance to medical treatment (http://ec.europa.eu/food/fs/sc/ssc/out278_en.pdf).
Supplementary Material
Acknowledgments
H.B.D. gratefully acknowledges financial support of this project (DE 403-11) by the Deutsche Forschungsgemeinschaft.
We further thank Ursula Schramm, Department of Dermatology and Venereology, MLU Halle (Saale), Germany, for excellent technical assistance. We thank Kerstin Neumann, Department of Otorhinolaryngology, Head and Neck Surgery, MLU Halle (Saale), Germany, and Sabine Köthke, Biocenter, MLU Halle (Saale), Germany, for help with initial experiments with caspofungin and Jorrit-Jan Krijger, Institute of Agricultural and Nutritional Sciences, MLU Halle (Saale), Germany, for critically reading the manuscript. The donation of tebuconazole (Bayer Cropscience GmbH, Langenfeld, Germany) and picoxystrobine (Syngenta Agro GmbH, Maintal, Germany), prochloraz (BASF AG, Ludwigshafen, Germany), amorolfin (Galderma Laboratorium GmbH, Düsseldorf, Germany), tolnaftate (Riemser Arzneimittel AG, Leipzig, Germany), itraconazole (Janssen-Cilag GmbH, Neuss, Germany), and voriconazole (Pfizer Pharma GmbH, Karlsruhe, Germany) is also acknowledged.
Footnotes
Published ahead of print on 9 July 2007.
Supplemental material for this article may be found at http://aac.asm.org/.
REFERENCES
- 1.Bekersky, I., R. M. Fielding, D. E. Dressler, J. W. Lee, D. N. Buell, and T. J. Walsh. 2002. Plasma protein binding of amphotericin B and pharmacokinetics of bound versus unbound amphotericin B after administration of intravenous liposomal amphotericin B (AmBisome) and amphotericin B deoxycholate. Antimicrob. Agents Chemother. 46:834-840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cano, J., J. Guarro, and J. Gené. 2004. Molecular and morphological identification of Colletotrichum species of clinical interest. J. Clin. Microbiol. 42:2450-2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castro, L. G., C. da Silva Lacaz, J. Guarro, J. Gene, E. M. Heins-Vaccari, R. S. de Freitas Leite, G. L. Arriagada, M. M. Reguera, E. M. Ito, N. Y. Valente, and R. Nunes. 2001. Phaeohyphomycotic cyst caused by Colletotrichum crassipes. J. Clin. Microbiol. 39:2321-2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cowen, L. E., D. Sanglard, D. Calabrese, C. Sirjusingh, J. B. Anderson, and L. M. Kohn. 2000. Evolution of drug resistance in experimental populations of Candida albicans. J. Bacteriol. 182:1515-1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deising, H. B., S. Reimann, A. Peil, and W. E. Weber. 2002. Disease management of rusts and powdery mildews, p. 243-269. In F. Kempken (ed.), The mycota XI. Application in agriculture. Springer, Berlin, Germany.
- 6.de Neergaard, E. (ed.). 1997. Methods in botanical histopathology. Kandrups Bogtrykkeri, Copenhagen, Denmark.
- 7.Dodd, J. C., A. Estrada, and M. J. Jeger. 1992. Epidemiology of Colletotrichum gloeosporioides in the tropics, p. 308-325. In J. A. Bailey and M. J. Jeger (ed.), Colletotrichum: biology, pathology and control. CAB International, Wallingford, United Kingdom.
- 8.Fernandez, V., D. Dursun, D. Miller, and E. C. Alfonso. 2002. Colletotrichum keratitis. Am. J. Ophthalmol. 134:435-438. [DOI] [PubMed] [Google Scholar]
- 9.Guarro, J., T. E. Svidzinski, L. Zaror, M. H. Forjaz, J. Gene, and O. Fischman. 1998. Subcutaneous hyalohyphomycosis caused by Colletotrichum gloeosporioides. J. Clin. Microbiol. 36:3060-3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hajdu, R., R. Thompson, J. G. Sundelof, B. A. Pelak, F. A. Bouffard, J. F. Dropinski, and H. Kropp. 1997. Preliminary animal pharmacokinetics of the parenteral antifungal agent MK-0991 (L-743,872). Antimicrob. Agents Chemother. 41:2339-2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hof, H. 2001. Critical annotations to the use of azole antifungals for plant protection. Antimicrob. Agents Chemother. 45:2987-2990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeffries, P., J. C. Dodd, M. J. Jeger, and R. A. Plumbley. 1990. The biology and control of Colletotrichum species on tropical fruit crops. Plant Pathol. 39:343-366. [Google Scholar]
- 13.Kontoyiannis, D. P., R. E. Lewis, M. S. Lionakis, N. D. Albert, G. S. May, and I. I. Raad. 2003. Sequential exposure of Aspergillus fumigatus to itraconazole and caspofungin: evidence of enhanced in vitro activity. Diagn. Microbiol. Infect. Dis. 47:415-419. [DOI] [PubMed] [Google Scholar]
- 14.Lass-Flörl, C., M. Nagl, C. Speth, H. Ulmer, M. P. Dierich, and R. Würzner. 2001. Studies of in vitro activities of voriconazole and itraconazole against Aspergillus hyphae using viability staining. Antimicrob. Agents Chemother. 45:124-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leach, J., B. R. Lang, and O. C. Yoder. 1982. Methods for selection of mutants and in vitro culture of Cochliobolus heterostrophus. J. Gen. Microbiol. 128:1719-1729. [Google Scholar]
- 16.Mendgen, K., and H. Deising. 1993. Infection structures of fungal plant pathogens—a cytological and physiological evaluation. New Phytol. 124:193-213. [DOI] [PubMed] [Google Scholar]
- 17.Midha, N. K., Y. Mirzanejad, and M. Soni. 1996. Colletotrichum spp: plant or human pathogen? Antimicrob. Infect. Dis. Newsl. 15:26-27. [Google Scholar]
- 18.Müller, F.-M. C., A. Staudigel, S. Salvenmoser, A. Tredup, R. Miltenberger, and J. V. Herrmann. 2007. Cross-resistance to medical and agricultural azole drugs in yeasts from the oropharynx of human immunodeficiency virus patients and from environmental Bavarian vine grapes. Antimicrob. Agents Chemother. 51:3014-3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O'Quinn, R. P., J. L. Hoffmann, and A. S. Boyd. 2001. Colletotrichum species as emerging opportunistic fungal pathogens: a report of 3 cases of phaeohyphomycosis and review. J. Am. Acad. Dermatol. 45:56-61. [DOI] [PubMed] [Google Scholar]
- 20.Perea, S., G. Gonzalez, A. W. Fothergill, W. R. Kirkpatrick, M. G. Rinaldi, and T. F. Patterson. 2002. In vitro interaction of caspofungin acetate with voriconazole against clinical isolates of Aspergillus spp. Antimicrob. Agents Chemother. 46:3039-3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reimann, S., and H. B. Deising. 2005. Inhibition of efflux transporter-mediated fungicide resistance in Pyrenophora tritici-repentis by a derivative of natural 4′-hydroxyflavone and enhancement of fungicide activity. Appl. Environ. Microbiol. 71:3269-3275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ritterband, D. C., M. Shah, and J. A. Seedor. 1997. Colletotrichum graminicola: a new corneal pathogen. Cornea 16:362-364. [PubMed] [Google Scholar]
- 23.Rump, A. F., K. Guttler, D. P. König, N. Yucel, M. Korenkov, and J. M. Schierholz. 2003. Pharmacokinetics of the antimicrobial agents rifampicin and miconazole released from a loaded central venous catheter. J. Hosp. Infect. 53:129-135. [DOI] [PubMed] [Google Scholar]
- 24.Sugui, J. A., and H. B. Deising. 2002. Isolation of infection-specific sequence tags expressed during early stages of maize anthracnose disease development. Mol. Plant Pathol. 3:197-203. [DOI] [PubMed] [Google Scholar]
- 25.Taguchi, H., M. Miyaji, and T. Yoshida. 2000. Evaluation of miconazole activity contained in human serum to hypha of Aspergillus fumigatus. Jpn. J. Med. Mycol. 41:41-44. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.