Abstract
The efficacy of β-lactams is thought to be dependent on the time that the unbound concentrations exceed the MIC (fT>MIC). However, the pharmacokinetic/pharmacodynamic index (PDI) that correlates best to the selection of resistance is not yet clear. The selection of ceftizoxime (CZX)-resistant Enterobacter cloacae mutant strains during the development of murine mixed-infection abscesses was studied to determine the PDI that is important for the emergence of resistance and the PDI value needed for the prevention of resistance. Studies were carried out 24 h after inoculation with Bacteroides fragilis ATCC 23745 and E. cloacae 22491. Six to 1,536 mg of CZX/kg of body weight/day given every 2 h (q2h), q4h, q6h, or q8h was started 30 min before inoculation and continued for 24 h. Resistant mutants were isolated to determine mutant frequencies (MF). The fT>MIC varied from 9 to 98% for E. cloacae, the peak concentration (unbound fraction) was 0.6 to 578 mg/liter, and the area under the concentration-time curve (unbound fraction) (fAUC) was 1.9 to 553 mg·h/liter. The fAUC-to-MIC ratio best explained the in vivo efficacy. CZX-resistant B. fragilis and E. cloacae mutants were isolated from untreated controls at an MF of 10−5 to 10−7. The MF of resistant B. fragilis did not increase during therapy. The selection of resistant E. cloacae strains at an MF of 10−1 to 10−2 was related to the fT>MIC and the ratio of fAUC to MIC following an inverse U shape. However, the ratio of fAUC to MIC was the stronger driver of resistance. The highest MFs were 0.7 to 0.9 at an fAUC-to-MIC ratio of approximately 250. We conclude that the ratio of fAUC to MIC is the PDI that correlated best to the in vivo efficacy of CZX and probably also to the emergence of resistant E. cloacae mutants. An fAUC-to-MIC ratio of 1,000 was needed to prevent the emergence of this resistance.
The emergence of resistant bacterial strains during β-lactam therapy is associated with the intensity of β-lactam use (12, 20, 32) and with prolonged antibiotic exposure (14). Until now, antibiotic dosing regimens used to treat infections have been based primarily on the pharmacokinetic/pharmacodynamic index (PDI) (18) that describes the optimal efficacy and/or prevention of toxicity. However, the increasing problem of emergence of resistance under the influence of antibiotic selection necessitates the need to determine the PDI that correlates best to the development of this resistance.
To date, there have been very few studies that have investigated the PDI that is important for the emergence of β-lactam resistance. While the ratio of the area under the concentration-time curve (AUC) at 24 h to MIC of ≥100 (10, 33, 36) or a peak-to-MIC ratio of 8 to 10 (3, 8) may significantly reduce the emergence of resistant subpopulations during treatment with fluoroquinolones and aminoglycosides, it has been reported that these indices do not appear to play an important role in the suppression of resistance during β-lactam therapy (33). However, recent findings have indicated the importance of a high-dose, short-elimination half-life regimen to minimize the emergence of cephalosporin-resistant Escherichia coli strains (25).
In a recent study, we found that the preferential selection of β-lactam-resistant mutants during the treatment of mixed-infection abscesses was dependent not only on the type of β-lactam used for therapy but also on the antibiotic doses employed. Ceftizoxime (CZX) (Cefizox)-resistant mutants of Enterobacter cloacae were selected within 24 h of treatment with lower doses of this cephalosporin but were not found with higher doses of the antibiotic. Since a single dosing frequency (every 2 h [q2h]) was used for these studies, it was not possible to distinguish between the time that the unbound concentrations exceed the MIC (fT>MIC) and other PDIs describing efficacy and emergence of resistance (30). In the present investigation, we have extended our previous study to include different dosing regimens to determine the PDI important for the emergence of resistant mutants and to establish the PDI value needed for the prevention of this type of resistance.
(This work was presented in part at the 43rd Annual Interscience Conference on Antimicrobial Agents and Chemotherapy, Chicago, IL, 2003.)
MATERIALS AND METHODS
Antibiotics and media.
CZX was supplied by Fujisawa Holland B.V. (Houten, The Netherlands). Wilkens Chalgren (WC) broth, WC agar, eosin methylene blue (EM) agar, brain heart infusion broth, and DST agar were all supplied by Unipath Ltd. (Haarlem, The Netherlands).
Bacterial strains.
Bacteroides fragilis ATCC 23745 and a clinical isolate, Enterobacter cloacae 22491, were used. The MICs of CZX for these strains were 1 and 0.25 μg/ml, respectively (30). Cultures grown overnight were obtained by inoculating 30-ml volumes of WC broth with 0.1 ml of standardized frozen bacterial suspensions (28) and incubating them aerobically (E. cloacae) or anaerobically (B. fragilis) at 37°C for 18 h.
Determination of MPC.
The mutant prevention concentration (MPC) of E. cloacae 22491 was determined by use of a method described previously by Lu et al. (16). A culture of E. cloacae 22491 grown overnight was concentrated to 1010 CFU/ml by centrifugation during 10 min at 3,000 × g. Subsequently, 1 ml of this suspension was applied to five plates (200 μl per plate) containing various concentrations of CZX. Preliminary determinations using twofold dilutions of drug provided an approximate value of the MPC. This was followed by a second, more precise determination of the MPC by using plates containing linear drug concentration increments. Agar plates were incubated for 18 h at 37°C. The MPC was defined as the lowest drug concentration that prevented bacterial colony formation from a culture containing 1010 bacteria. Colonies growing at the highest antibiotic concentration were subcultured on antibiotic-free agar plates to test the stability of the mutants.
Animals.
Female specific-pathogen-free BALB/c mice (IFFA Credo, l'Arbresle, France) that were 12 to 18 weeks of age and weighing 20 to 25 g were used throughout the study. The cecal contents of male specific-pathogen-free Swiss mice (Broekman Institute B.V., The Netherlands) were used for the production of autoclaved cecal contents (ACC) (29). All animals received water and food ad libitum. The study was approved by the Institutional Animal Care and Use Committee of Erasmus University, Rotterdam, The Netherlands.
Mouse model.
A subcutaneous abscess model described previously (28) was employed. Briefly, inocula were prepared by diluting cultures of B. fragilis and E. cloacae 22491 grown overnight in WC broth, which were then mixed together with ACC in a volume ratio of 1:1:2. Final inocula contained 107 CFU B. fragilis cells, 107 CFU E. cloacae cells, and 4 mg (dry weight) ACC in a total volume of 0.25 ml. Mice were injected subcutaneously on both flanks. Abscesses were allowed to develop for 24 h. Mice were then killed by CO2 asphyxiation, and the abscesses were dissected, weighed, and homogenized in 1 ml phosphate-buffered saline for 10 s (Pro 200; B.V. Centraal Magazijn, Abcoude, The Netherlands). Total bacterial counts were determined on the resulting suspensions by making duplicate serial 10-fold dilutions in phosphate-buffered saline and plating 20 μl of each dilution onto EM agar (E. cloacae) or WC agar containing 100 mg/liter gentamicin (B. fragilis). Plates were incubated at 37°C aerobically for 24 h (EM agar) or anaerobically for 48 h (WC agar). Bacterial counts were expressed as the mean log10 CFU/abscess of four abscesses per treatment group ± standard error of the mean. The lower threshold limit was 1.7 log10 CFU/abscess.
Pharmacokinetic studies.
Single-dose pharmacokinetic studies with 100 mg of CZX/kg of body weight were performed on groups of three mice 4 days after inoculation. Blood was removed by orbital puncture at 10, 20, 30, 45, 60, 120, 240, and 360 min after drug administration, and serum samples were stored at −80°C until they were assayed. Multiple-dose studies were carried out on mice treated with 36 doses of 100 mg/kg CZX q2h. Antibiotic concentrations were determined in duplicate by an agar diffusion bioassay outlined previously (28) using E. coli strain 62 as the test strain. Pharmacokinetic parameters were determined using the MW/Pharm computer program package (Mediware, Groningen, The Netherlands) with a one-compartment open model. The obtained parameters were used to simulate various dosing regimens and determine pharmacokinetic properties of each regimen, such as fT>MIC, fCmax, and fAUC, allowing for a protein binding of 13% of the antibiotic in mouse serum (21). As each dosing regimen in the mouse model was started 30 min before inoculation (see below), the exposure time of the bacteria to the antibiotic was 23.5 h. Therefore, to accurately determine the pharmacokinetic properties of each regimen in this model, the fT>MIC and fAUC values for all dosing regimens for the first 30 min were calculated separately and subsequently subtracted from the 24-h values. The fCmax value was not corrected, assuming only differences in absolute values, but not in values relative to each other, of the various dosing regimens.
Antibiotic treatment and emergence of resistance in early abscess development.
Groups of two mice were treated with subcutaneous daily doses of 6 to 1,536 mg/kg/day CZX. Twofold-increasing doses were given q2h, and fourfold increasing doses were given q4h and q6h. Daily doses of 384 and 1,536 mg/kg/day were given q8h. Treatment was started 30 min before inoculation with B. fragilis or E. cloacae and continued for 24 h. Resistant E. cloacae mutants were isolated from treated and untreated abscesses on WC agar plates containing 16× the MIC of CZX that had been incubated aerobically for 48 h at 37°C. To isolate B. fragilis mutants, the WC agar plates, in addition to the CZX concentration mentioned above, also contained 100 mg/liter gentamicin, which inhibited the growth of the E. cloacae mutants. These plates were incubated anaerobically at 37°C for 72 h. (Control experiments showed that gentamicin had no synergistic or antagonistic effect on the number of CZX-resistant B. fragilis mutants isolated on plates containing 16× the MIC of CZX). The mutant frequency (MF) was expressed as the ratio of the number of resistant colonies isolated per total bacterial counts found on antibiotic-free agar.
Pharmacodynamic analysis.
The PDIs that correlated best to efficacy and emergence of resistance were determined by visual inspection and nonlinear regression using GraphPad Prism version 3.0 for Windows (GraphPad Software, San Diego, CA). The Emax model with variable slope was used to fit to the fT>MIC, the ratio of fAUC to MIC, the ratio of fCmax to MIC, and the total bacterial counts, while a Gaussian-type function was used to fit to resistance data.
RESULTS
Pharmacokinetics.
After single and multiple doses of 100 mg/kg, the half-lives of CZX were 0.23 h and 0.22 h, respectively, indicating that there was no change in the pharmacokinetics of this cephalosporin during therapy. The pharmacokinetic data for CZX described previously by Murakawa et al. (21) (20 mg/kg) are similar to our findings (100 mg/kg); the half-life was 0.26 h. The model parameters used to calculate pharmacokinetic and pharmacodynamic parameters for each dosing regimen resulted in fAUC from 0.5 to 24 h of 1.9 to 553 mg·h/liter and peak concentrations (fCmax) of 0.6 to 578 mg/liter. The fT>MICs ranged from 9 to 98% of the dosing interval for E. cloacae.
Effect of CZX dosing regimens on the total bacterial populations of abscesses.
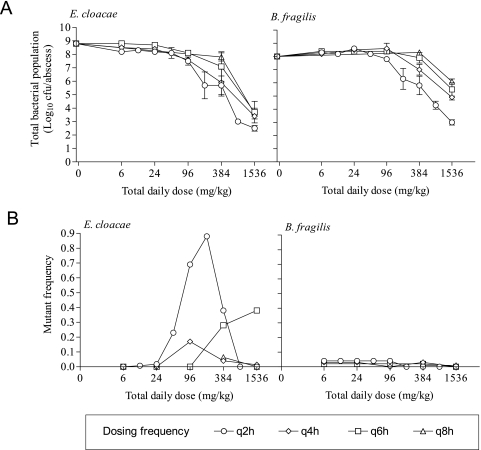
The total bacterial counts of B. fragilis and E. cloacae in untreated abscesses 23.5 h after inoculation were 8.0 ± 0.1 and 8.8 ± 0.1 log10 CFU/abscess, respectively. When treated with CZX during the development of these abscesses, there was no bacterial killing with all dosing regimens of <96 mg/kg/day (Fig. 1A). With dosing regimens of ≥96 mg/kg/day, the killings of both strains were very similar, reaching a maximum log reduction of ≥5 log10 CFU/abscess compared to untreated abscesses. The efficacy of CZX against the E. cloacae and B. fragilis strains was reduced as the frequency of the dosing regimens decreased (Fig. 1A).
FIG. 1.
In vivo effect of increasing dosings of CZX on the total bacterial counts of B. fragilis ATCC 23745 and E. cloacae 22491 isolated from mixed-infection abscesses on antibiotic-free medium (A) and on the frequency of CZX-resistant B. fragilis ATCC 23745 and E. cloacae 22491 cells isolated from mixed-infection abscesses on medium containing 16× the MIC of CZX (B). The MF is expressed as the ratio of the number of resistant colonies isolated to total bacterial numbers isolated on antibiotic-free agar as a function of total daily doses. Dosing regimens of 6 to 1,536 mg/kg/day were started 30 min before inoculation and continued for 24 h. Daily doses were divided into different dosing regimens given q2h, q4h, q6h, or q8h.
Effect of CZX dosing regimens on mutant frequency.
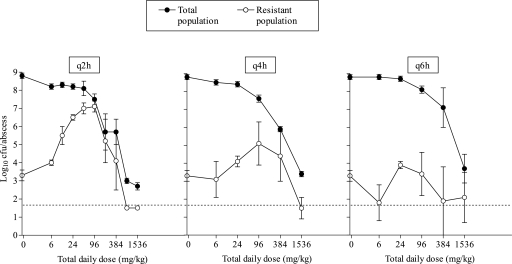
Figure 2 shows the effect of increasing daily doses on both the total population and the resistant (MIC > 16 μg/ml) population of E. cloacae for various dosing intervals. With all regimens up to 96 mg/kg/day, the numbers of resistant E. cloacae mutants increased. The most striking effect was observed for the q2h regimens, where a maximum increase of 3.8 log10 CFU/abscess was reached when the total population comprised almost exclusively resistant cells. If the same daily doses were given less frequently, i.e., q4h, significantly fewer mutant strains were selected (maximum increase of 2 log10CFU/abscess), and higher CZX doses were required before this selection occurred. The q6h dosing regimen did not preferentially select CZX-resistant E. cloacae mutants. Emergence of resistant B. fragilis strains was not observed. Figure 1B shows the mutant frequency with respect to total daily dose. In the absence of ceftizoxime, CZX-resistant mutants of B. fragilis and E. cloacae were isolated from the total bacterial population at respective frequencies of 0 to 10−7 and 10−5 to 10−7. CZX treatment had no effect on the frequency with which CZX-resistant mutants of B. fragilis were isolated from the abscesses. However, with all dosing regimens of >24 mg/kg/day, the average mutant frequency of CZX-resistant E. cloacae strains increased during therapy to between 0.01 and 0.9. At the highest total daily doses, the mutant frequencies decreased for the q2h and the q4h regimens.
FIG. 2.
Effect of CZX dosing frequency on the total and CZX-resistant populations of E. cloacae 22491 isolated from mixed-infection abscesses. Dosing regimens of 6 to 1,536 mg/kg/day were started 30 min before inoculation and continued for 24 h. Daily doses were divided into different dosing regimens given q2h, q4h, or q6h. The total bacterial population was isolated on antibiotic-free medium, and the resistant population was isolated on medium containing 16× the MIC of CZX.
Pharmacodynamic analysis.
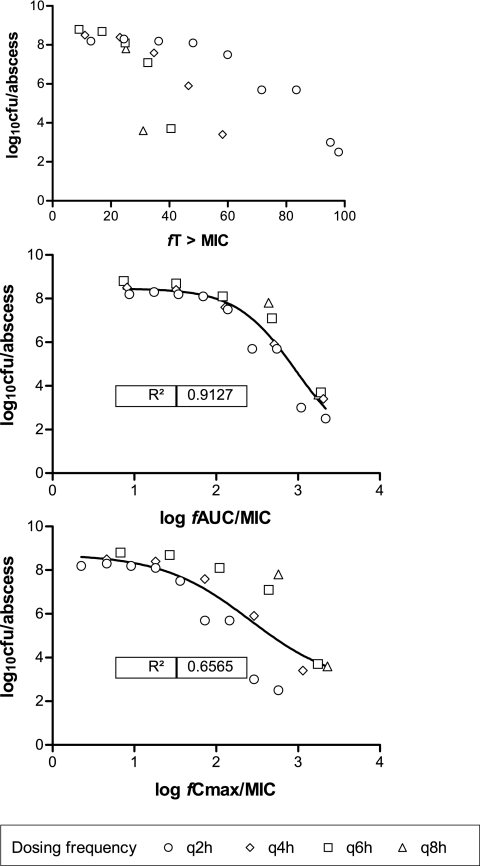
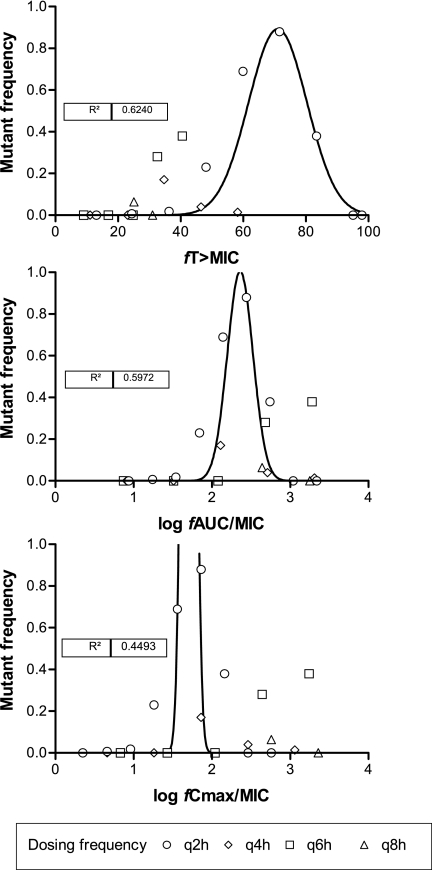
The regression analyses of the PDIs, fT>MIC, fAUC-to-MIC ratio, and fCmax-to-MIC ratio in relation to CZX efficacy and emergence of resistance of E. cloacae are presented in Fig. 3 and 4, respectively. The ratio of fAUC to MIC was the PDI that correlated best to the in vivo efficacy of CZX against the total bacterial populations of the abscesses (Fig. 3). Surprisingly, the relationship between fT>MIC and in vivo efficacy was not as good as that for the ratio of fAUC to MIC; indeed, no fit could be obtained. In contrast, the frequency that CZX-resistant E. cloacae mutants were isolated from the abscesses was related to both the fT>MIC and fAUC-to-MIC ratio. (It should be noted that because the values of the first 30 min were taken out of the calculations, the peak concentration in the graph of the ratio of fCmax to MIC corresponds to a first compartment model at time zero, that is, after the first dose and before inoculation; therefore, the fCmax-to-MIC peak extends beyond the graph [Fig. 4].) Bell-shaped curves fitted the relationship between the MF and the fT>MIC and the fAUC-to-MIC ratio, with similar R2 values of 0.624 and 0.597, respectively. However, the points that result in the fit with the fT>MIC curve are almost completely driven by one (q2h) dosing regimen, with no clear relationship of the points from the other dosing regimens, while the points that result in the fit of the fAUC-to-MIC ratio curve are derived from all regimens, with only one outlier from the highest dosing of 1,536 mg/kg. This indicates that the ratio of fAUC to MIC is probably the PDI that drives the selection of resistant E. cloacae strains in this model and that a ratio of fAUC to MIC of more than approximately 1,000 would be required to prevent the emergence of this resistance.
FIG. 3.
Relationship between the fT>MIC, fAUC-to-MIC ratio, and fCmax-to-MIC ratio of CZX and the total bacterial counts of E. cloacae 22491 isolated from mixed-infection abscesses 24 h after treatment. Lines indicate the best model fit for the Emax model.
FIG. 4.
Relationship between the fT>MIC, fAUC-to-MIC ratio, and fCmax-to-MIC ratio of CZX and the mutant frequency of CZX-resistant E. cloacae 22491 cells isolated from mixed-infection abscesses 24 h after treatment.
Relation of MPC to the number of ceftizoxime-resistant E. cloacae strains.
E. cloacae 22491 had an MPC of 384 μg/ml and an MIC99 of 0.125 μg/ml. Thus, the MPC was relatively high. Because of this, the time within the mutant selection window (MSW) (tMSW) was more or less equal to the T>MIC, and no distinction could be made between the effects of tMSW and T>MIC. The conclusions with respect to the fT>MIC therefore also apply to tMSW.
DISCUSSION
It is reported that the fT>MIC is the most important PDI to explain the efficacy of β-lactam antibiotics against Enterobacteriaceae, and for maximum efficacy, cephalosporin serum concentrations should be above the MIC for 60% to 70% of the dosing interval (4). However, the present study has demonstrated that in this mixed-infection abscess model, the fAUC-to-MIC ratio was the PDI that correlated best to the in vivo efficacy of CZX and probably also to the emergence of resistant E. cloacae mutants. Presumably, this was due to the high antibiotic concentrations required to kill the large numbers of resistant mutants present in the abscesses and also the reason efficacy was not related to fT>MIC.
In our abscess model, the selective pressure of CZX was correlated to both the fAUC-to-MIC ratio and fT>MIC, although the fAUC-to-MIC ratio seems to explain the emergence of resistance better over all dosing regimens. The Gaussian distribution was used to fit the MF data. This function was chosen because the MIC distributions are log-normally distributed (15, 34). Thus, if the probability of emergence of resistance is to be related to the MIC, and independent of the MIC, it follows that the distribution of the MF is distributed in a similar fashion. An fAUC-to-MIC ratio of approximately 1,000 would be required to suppress the selection of CZX-resistant E. cloacae mutants. This value is much higher than the value that is needed for optimal efficacy. If fT>MIC is also regarded as a predictor, the data suggest that values of nearly 100% are required to prevent the emergence of resistance, and this value is also relatively high (4). In a study looking at the exposure required to prevent resistance to ceftriaxone in Enterobacter in the neutropenic thigh model, Berkhout et al. previously found that T>32 times the MIC was important for efficacy, probably because that prevented the emergence of the resistant clone (2). Thus, the pharmacokinetic-pharmacodynamic relationship found here indicates that higher values of the pharmacokinetic-pharmacodynamic index are needed for the prevention of emergence of resistance compared to those needed for efficacy in this experimental setting.
In previous studies, an MSW, when the risk of mutant selection is greatest, was defined by some authors as the drug concentration range that extends from the MIC to the MPC. In those investigations, the preferential selection of antimicrobial resistance was prevented when drug concentrations fell outside this MSW, and it is postulated that a window of opportunity is created in which antibiotic levels are sufficient to kill the susceptible population yet allow the increase of the resistant population. This MSW hypothesis has been used to explain the results of several in vitro studies using an expanded-spectrum cephalosporin (22) and quinolones (7, 10, 35) against both gram-positive and gram-negative bacterial strains. For quinolones, this was achieved with dosing regimens producing ratios of the AUC at 24 h to MIC of >100 (10, 33, 36). In the present study, no distinction could be made between the effects of fT>MIC and tMSW because of the relative high MPC values of the E. cloacae strain. The relationships between these two PDIs and the MF are therefore similar, and the conclusions with respect to the fT>MIC also apply to the tMSW; that is, a reasonable correlation is found with the MF using a Gaussian distribution but with the same limitations in the interpretation.
Previous studies using in vitro models investigated the importance of dosing regimens (22), T>MIC (23), and fAUC (24) to the selection of β-lactam-resistant mutants. The results of our study concur with those reported previously for other in vivo models (1, 27). Bakker-Woudenberg et al. (1) previously demonstrated that the PDI that correlated best to the therapeutic effect of ceftazidime in an immunocompetent rat model of Klebsiella pneumoniae lung infection was dependent on the duration of treatment and/or the parameter of outcome. Concomitantly, the reduction of susceptible gut commensal E. cloacae isolates during this treatment was significantly correlated to the fAUC-to-MIC ratio (11a). Importantly, this abscess model as well as the rat model described immunocompetent animals, and this may be part of the explanation of why the effect is better correlated to AUC than to T>MIC.
The elucidation of the relationship between PDIs and the emergence of resistance during therapy facilitates the design of more effective dosing regimens. The results presented here could be relevant to the clinical situation in which an expanded-spectrum cephalosporin would be used to treat an infection resulting from complications following abdominal surgery, such as leakage of an intestinal suture (5, 6). In this case, antibiotic treatment has to be started prior to reoperation. Enterobacter strains can be involved in such infections (9, 31). We acknowledge that the PDI values reported here were obtained from experiments using a single E. cloacae-cephalosporin combination and that this preferential selection may not be common to all Enterobacter/Enterobacteriaceae strains (25, 30). Indeed, none of the dosing regimens increased the frequency with which CZX-resistant strains of B. fragilis were isolated from the abscesses (30). Nevertheless, expanded-spectrum cephalosporins are still widely used for empirical treatment (5) and surgical prophylaxis (11), and they are more likely to select resistant strains of Enterobacteriaceae than any other β-lactam (26, 30).
The findings of this study also challenge the practice of administering β-lactams in small frequent doses or by continuous infusion (19) as an appropriate procedure for treatment with certain cephalosporins. In our quest to find dosing regimens that will prevent the emergence of resistance, perhaps higher doses given less frequently may be more beneficial (11a, 24). Alternatively, the use of antibiotics with enhanced activity against resistant mutants, for example, cefepime (17, 25, 30), may be more advantageous in the treatment of infections involving “high-risk” strains.
Although not an objective of this investigation, the duration of therapy may also be a factor contributing to the emergence of antimicrobial resistance. Indeed, this appears to be an important aspect in the selection of quinolone resistance (10) and in the pharyngeal colonization of β-lactam-resistant strains (13). However, at infection sites where bacterial numbers are high, the selection of resistance may occur more readily. We found that CZX-resistant E. cloacae strains could be selected within 24 h of treatment. In previous studies involving in vitro kinetic models, the preferential selection of β-lactam-resistant strains occurred within 6 h (22) and 14 h (24) of antibiotic exposure, while prolonged exposure increased the risk of selecting mutants with an additional mutation (22).
In conclusion, this is a useful animal model to investigate PDIs that are important for the emergence of antimicrobial resistance during therapy. The fAUC-to-MIC ratio is probably the best PDI that explains the emergence of CZX-resistant E. cloacae strains during the early development of mixed-infection abscesses.
Acknowledgments
This study was financially supported by an unrestricted grant of Wyeth Lederle, Hoofddorp, The Netherlands.
Footnotes
Published ahead of print on 23 July 2007.
REFERENCES
- 1.Bakker-Woudenberg, I. A., M. T. ten Kate, W. H. Goessens, and J. W. Mouton. 2006. Effect of treatment duration on pharmacokinetic/pharmacodynamic indices correlating with therapeutic efficacy of ceftazidime in experimental Klebsiella pneumoniae lung infection. Antimicrob. Agents Chemother. 50:2919-2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berkhout, J., M. L. Van Ogtrop, P. J. van den Broek, J. A. M. van de Klundert, H. Mattie, L. G. Visser, and W. A. Craig. 1999. Pharmacodynamics of ceftriaxone against cephalosporin-sensitive and -resistant Enterobacter cloacae in vivo, abstr. 2036. Abstr. 39th Intersci. Conf. Antimicrob. Agents Chemother. American Society for Microbiology, Washington, DC.
- 3.Blaser, J., B. B. Stone, M. C. Groner, and S. H. Zinner. 1987. Comparative study with enoxacin and netilmicin in a pharmacodynamic model to determine importance of ratio of antibiotic peak concentration to MIC for bactericidal activity and emergence of resistance. Antimicrob. Agents Chemother. 31:1054-1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Craig, W. A. 1998. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin. Infect. Dis. 26:1-10; quiz, 11-12. [DOI] [PubMed] [Google Scholar]
- 5.Cunha, B. A., and J. H. Rex. 2003. Empiric therapy based on clinical syndrome, p. 18-134. In B. A. Cunha (ed.), Antibiotic essentials, 2nd ed. Physician's Press, Royal Oak, MI.
- 6.Cunha, B. A., P. E. Schoch, and J. H. Rex. 2003. Initial therapy of isolates pending susceptibility testing, p. 143-185. In B. A. Cunha (ed.), Antibiotic essentials, 2nd ed. Physician's Press, Royal Oak, MI.
- 7.Drlica, K. 2003. The mutant selection window and antimicrobial resistance. J. Antimicrob. Chemother. 52:11-17. [DOI] [PubMed] [Google Scholar]
- 8.Drusano, G. L., D. E. Johnson, M. Rosen, and H. C. Standiford. 1993. Pharmacodynamics of a fluoroquinolone antimicrobial agent in a neutropenic rat model of Pseudomonas sepsis. Antimicrob. Agents Chemother. 37:483-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunn, D. L., and R. L. Simmons. 1984. The role of anaerobic bacteria in intraabdominal infections. Rev. Infect. Dis. 6:S139-S146. [DOI] [PubMed] [Google Scholar]
- 10.Firsov, A. A., S. N. Vostrov, I. Y. Lubenko, K. Drlica, Y. A. Portnoy, and S. H. Zinner. 2003. In vitro pharmacodynamic evaluation of the mutant selection window hypothesis using four fluoroquinolones against Staphylococcus aureus. Antimicrob. Agents Chemother. 47:1604-1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Geroulanos, S., K. Marathias, J. Kriaras, and B. Kadas. 2001. Cephalosporins in surgical prophylaxis. J. Chemother. 13:23-26. [DOI] [PubMed] [Google Scholar]
- 11a.Goessens, W. H. F., J. W. Mouton, M. ten Kate, A. Ott, and I. A. J. M. Bakker-Woudenberg. 2007. Role of ceftazidime dose regimen on the selection of resistant Enterobacter cloacae in the intestinal flora of rats treated for experimental pulmonary infection. J. Antimicrob. Chemother. 59:507-516. [DOI] [PubMed] [Google Scholar]
- 12.Goossens, H., M. Ferech, R. Van der Stichele, M. Elseviers, and the ESAC Project Group. 2005. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 365:579-587. [DOI] [PubMed] [Google Scholar]
- 13.Guillemot, D., C. Carbon, B. Balkau, P. Geslin, H. Lecoeur, F. Vauzelle-Kervroedan, G. Bouvenot, and E. Eschwège. 1998. Low dosage and long treatment duration of beta-lactam. Risk factors for carriage of penicillin-resistant Streptococcus pneumoniae. JAMA 279:365-370. [DOI] [PubMed] [Google Scholar]
- 14.Harbarth, S., M. H. Samore, D. Lichtenberg, and Y. Carmeli. 2000. Prolonged antibiotic prophylaxis after cardiovascular surgery and its effect on surgical site infections and antimicrobial resistance. Circulation 101:2916-2921. [DOI] [PubMed] [Google Scholar]
- 15.Kronvall, G., G. Kahlmeter, E. Myhre, and M. F. Galas. 2003. A new method for normalized interpretation of antimicrobial resistance from disc test results for comparative purposes. Clin. Microbiol. Infect. 9:120-132. [DOI] [PubMed] [Google Scholar]
- 16.Lu, T., X. Zhao, X. Li, G. Hansen, J. Blondeau, and K. Drlica. 2003. Effect of chloramphenicol, erythromycin, moxifloxacin, penicillin and tetracycline concentration on the recovery of resistant mutants of Mycobacterium smegmatis and Staphylococcus aureus. J. Antimicrob. Chemother. 52:61-64. [DOI] [PubMed] [Google Scholar]
- 17.Mimoz, O., S. Leotard, A. Jacolot, C. Padoin, K. Louchahl, O. Petitjean, and P. Nordman. 2000. Efficacies of imipenem, meropenem, cefepime, and ceftazidime in rats with experimental pneumonia due to a carbapenem-hydrolyzing β-lactamase-producing strain of Enterobacter cloacae. Antimicrob. Agents Chemother. 44:885-890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mouton, J. W., M. N. Dudley, O. Cars, H. Derendorf, and G. L. Drusano. 2002. Standardization of pharmacokinetic/pharmacodynamic (PK/PD) terminology for anti-infective drugs. Int. J. Antimicrob. Agents 19:355-358. [DOI] [PubMed] [Google Scholar]
- 19.Mouton, J. W., and A. A. Vinks. 1996. Is continuous infusion of beta-lactam antibiotics worthwhile? Efficacy and pharmacokinetic considerations. J. Antimicrob. Chemother. 38:5-15. [DOI] [PubMed] [Google Scholar]
- 20.Mouton, R. P., J. H. Glerum, and A. C. Van Loenen. 1976. Relationship between antibiotic consumption and frequence of antibiotic resistance of four pathogens—a seven year study. J. Antimicrob. Chemother. 2:9-19. [DOI] [PubMed] [Google Scholar]
- 21.Murakawa, T., H. Sakamoto, S. Fukada, S. Nakamoto, T. Hirose, N. Itoh, and N. Nishida. 1980. Pharmacokinetics in animals after parenteral dosing. Antimicrob. Agents Chemother. 17:157-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Negri, M. C., M. Lipstich, J. Blazquez, B. R. Levin, and F. Baquero. 2000. Concentration-dependent selection of small phenotypic differences in TEM β-lactamase-mediated antibiotic resistance. Antimicrob. Agents Chemother. 44:2485-2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Odenholt, I., I. Gustafsson, and E. Lowdin. 2003. Postantibiotic and sub-MIC effects of benzylpenicillin against Streptococcus pneumoniae with different susceptibilities for penicillin. Chemotherapy 49:287-293. [DOI] [PubMed] [Google Scholar]
- 24.Olofsson, S. K., P. Geli, D. I. Andersson, and O. Cars. 2005. Pharmacodynamic model to describe the concentration-dependent selection of cefotaxime-resistant Escherichia coli. Antimicrob. Agents Chemother. 49:5081-5091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pechere, J. C., and I. R. Vladoianu. 1992. Development of resistance during ceftazidime and cefepime therapy in a murine peritonitis model. J. Antimicrob. Chemother. 29:563-573. [DOI] [PubMed] [Google Scholar]
- 26.Sanders, W. E., and C. C. Sanders. 1997. Enterobacter spp.: pathogens poised to flourish at the turn of the century. Clin. Microbiol. Rev. 10:220-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Soriano, F., P. Garcia-Corbeira, C. Ponte, R. Fernandez-Roblas, and I. Gadea. 1996. Correlation of pharmacodynamic parameters of five β-lactam antibiotics with therapeutic efficacies in an animal model. Antimicrob. Agents Chemother. 40:2686-2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stearne, L. E. T., I. C. Gyssens, W. H. Goessens, J. W. Mouton, W. J. Oyen, J. W. van der Meer, and H. A. Verbrugh. 2001. In vivo efficacy of trovafloxacin against Bacteroides fragilis in mixed infections with either Escherichia coli or a vancomycin-resistant strain of Enterococcus faecium in an established-abscess murine model. Antimicrob. Agents Chemother. 45:1394-1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stearne, L. E. T., C. Kooi, W. H. Goessens, I. A. J. M. Bakker-Woudenberg, and I. C. Gyssens. 2001. In vitro activity of trovafloxacin against Bacteroides fragilis in mixed culture with either Escherichia coli or a vancomycin resistant strain of Enterococcus faecium using an anaerobic time kill technique. Antimicrob. Agents Chemother. 45:243-251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stearne, L. E. T., D. van Boxtel, N. Lemmens, W. Goessens, J. W. Mouton, and I. C. Gyssens. 2004. Comparative study of the effects of ceftizoxime, piperacillin, and piperacillin-tazobactam concentrations on antibacterial activity and selection of antibiotic-resistant mutants of Enterobacter cloacae and Bacillus fragilis in vitro and in vivo in mixed-infection abscesses. Antimicrob. Agents Chemother. 48:1688-1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tally, F. P. 1988. Factors affecting the choice of antibiotics in mixed infections. J. Antimicrob. Chemother. 22:87-100. [DOI] [PubMed] [Google Scholar]
- 32.Tenover, F. C. 2001. Development and spread of bacterial resistance to antimicrobial agents: an overview. Clin. Infect. Dis. 33(Suppl 3):S108-S115. [DOI] [PubMed] [Google Scholar]
- 33.Thomas, J. K., A. Forrest, S. M. Bhavnani, J. M. Hyatt, A. Cheng, C. H. Ballow, and J. J. Schentag. 1998. Pharmacodynamic evaluation of factors associated with the development of bacterial resistance in acutely ill patients during therapy. Antimicrob. Agents Chemother. 42:521-527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Turnidge, J., G. Kahlmeter, and G. Kronvall. 2006. Statistical characterisation of bacterial wild-type MIC value distributions and the determination of epidemiological cutoff values. Clin. Microbiol. Infect. 12:418-425. [DOI] [PubMed] [Google Scholar]
- 35.Zhao, X., and K. Drlica. 2002. Restricting the selection of antibiotic-resistant mutant bacteria: measurement and potential use of the mutant selection window. J. Infect. Dis. 185:561-565. [DOI] [PubMed] [Google Scholar]
- 36.Zinner, S. H., I. Y. Lubenko, D. Gilbert, K. Simmons, X. Zhao, K. Drlica, and A. A. Firsov. 2003. Emergence of resistant Streptococcus pneumoniae in an in vitro dynamic model that simulates moxifloxacin concentrations inside and outside the mutant selection window: related changes in susceptibility, resistance frequency and bacterial killing. J. Antimicrob. Chemother. 52:616-622. [DOI] [PubMed] [Google Scholar]