Abstract
Tuberculosis (TB) is the most important zoonotic bacterial disease in nonhuman primates (NHP). The current diagnostic method, the intradermal palpebral tuberculin test, has serious shortcomings. We characterized antibody responses in NHP against Mycobacterium tuberculosis to identify immunodominant antigens and develop a rapid serodiagnostic test for TB. A total of 422 NHP were evaluated, including 243 rhesus (Macaca mulatta), 46 cynomolgus (Macaca fascicularis), and 133 African green (Cercopithecus aethiops sabaeus) monkeys at five collaborative centers. Of those, 50 monkeys of the three species were experimentally inoculated with M. tuberculosis. Antibody responses were monitored every 2 to 4 weeks for up to 8 months postinfection by MultiAntigen Print ImmunoAssay with a panel of 12 recombinant antigens. All of the infected monkeys produced antibodies at various levels and with different antigen recognition patterns. ESAT-6 and MPB83 were the most frequently recognized proteins during infection. A combination of selected antigens which detected antibodies in all of the infected monkeys was designed to develop the PrimaTB STAT-PAK assay by lateral-flow technology. Serological evaluation demonstrated high diagnostic sensitivity (90%) and specificity (99%). The highest rate of TB detection was achieved when the skin test was combined with the PrimaTB STAT-PAK kit. This novel immunoassay provides a simple, rapid, and accurate test for TB in NHP.
Tuberculosis (TB) remains one of the most important bacterial diseases of nonhuman primates (NHP) because of its frequency of occurrence, ability to spread rapidly, high mortality rates, and zoonotic potential (14, 26, 32). The disease in NHP is caused by the same organisms that are responsible for TB in humans (Mycobacterium tuberculosis) and cattle (Mycobacterium bovis) (4, 11, 33, 35). Infection can be readily transmitted from one monkey to another or from monkeys to humans and vice versa (26, 31).
To control the spread of this devastating illness, captive NHP are screened for TB regularly. The USDA-approved method tests for delayed hypersensitivity in response to an intradermal injection of mammalian old tuberculin (MOT) into the skin of the eyelid (intrapalpebral tuberculin test) (8). MOT is composed of poorly defined mycobacterial antigens that are known to be highly cross-reactive (12, 25). The visual scoring of the test is largely subjective, often allowing confusion between negative and positive results (6, 15). In spite of rigorous testing and import quarantine measures, outbreaks of TB in NHP continue to occur in research laboratories, resulting in the destruction of numerous valuable animals in the United States and elsewhere (14, 32). Many healthy primates are also euthanized unnecessarily because of false-positive skin test reactions that might be due to a nonspecific inflammatory response to MOT or because of sensitization with cross-reactive nonpathogenic species of environmental mycobacteria (10, 15, 17, 19). Thus, alternative diagnostic approaches for antemortem TB testing of NHP are urgently needed.
We have recently developed two membrane-based antibody detection methods, MultiAntigen Print ImmunoAssay (MAPIA) and a lateral-flow test, and demonstrated the potential for rapid TB serodiagnosis in various host species (16, 23, 34). In the present study, we characterized the antibody responses in NHP experimentally infected with M. tuberculosis and developed the PrimaTB STAT-PAK assay, a novel lateral-flow test for antibody detection in TB. This test was evaluated in comparison with the intradermal palpebral tuberculin test and other laboratory diagnostic methods over the course of experimental infection.
MATERIALS AND METHODS
Animals and infection.
A total of 422 NHP were used, including 243 rhesus (Macaca mulatta), 46 cynomolgus (Macaca fascicularis), and 133 African green (Cercopithecus aethiops sabaeus) monkeys from five collaborative centers (Table 1). At four research sites, experimental infection with M. tuberculosis was performed on 50 animals, including 29 rhesus, 16 cynomolgus, and 5 African green monkeys. Animal infection experiments were performed in biosafety level 3 facilities according to the study protocols approved by the Institutional Animal Care and Use Committees. After prestudy quarantine and extensive evaluation for TB, monkeys were inoculated intratracheally with various doses and strains of M. tuberculosis (or M. avium or M. kansasii at the Tulane National Research Primate Center [TNPRC]) as indicated in Table 1. Every 2 to 4 weeks after inoculation, the intrapalpebral MOT test was performed and at certain sites, tracheal wash specimens were collected for culture and PCR-based testing (Amplified MTD; Gen-Probe, Inc., San Diego, CA). Serum samples were collected at the same time for antibody detection methods. Durations of the experiments at different sites varied from 7 weeks to 8 months, depending on the study design and/or survival rates of infected monkeys. TB was confirmed by careful postmortem examination including histopathology and acid-fast bacillus detection, as well as culture and PCR probes. The control group combined 214 rhesus, 30 cynomolgus, and 128 African green monkeys. This group included six rhesus macaques experimentally inoculated with two species of non-TB mycobacteria (three with M. avium and three with M. kansasii), and the rest were uninoculated monkeys.
TABLE 1.
Study population
| Research site and monkey species | Infection (no. of CFU) | No. of monkeys |
|---|---|---|
| TNPRC | ||
| Rhesus | M. tuberculosis Erdman (30) | 5 |
| Rhesus | M. tuberculosis H37Rv (210) | 4 |
| Rhesus | M. kansasii ATCC 12478 (260) | 3 |
| Rhesus | M. avium ATCC 15769 (100) | 3 |
| Rhesus | None | 160 |
| Cynomolgus | M. tuberculosis Erdman (1,000) | 7 |
| Cynomolgus | None | 24 |
| African green | None | 33 |
| USAb | ||
| Rhesus | M. tuberculosis Erdman (100) | 5 |
| Rhesus | Nonea | 5 |
| MRL | ||
| Rhesus | M. tuberculosis Erdman (100) | 6 |
| Cynomolgus | M. tuberculosis Erdman (100) | 6 |
| African green | M. tuberculosis Erdman (100) | 5 |
| BPRCc | ||
| Rhesus | M. tuberculosis Erdman (1,000) | 6 |
| Rhesus | M. tuberculosis Beijing (1,000) | 3 |
| Rhesus | None | 48 |
| Cynomolgus | M. tuberculosis Erdman (1,000) | 3 |
| Cynomolgus | None | 6 |
| BSFLd | ||
| African green | None | 95 |
Preinoculation serum samples were used as a negative control group.
USA, University of South Alabama.
BPRC, Biomedical Primate Research Centre.
BSFL, Behavioral Sciences Foundation Laboratories.
Antigens.
A panel of 12 defined proteins of M. tuberculosis (8 single recombinant proteins and 4 polyprotein fusions) was used in the MAPIA described below. The following antigens were purified to near homogeneity as polyhistidine-tagged proteins: ESAT-6 and CFP-10, produced at the Statens Serum Institut (Copenhagen, Denmark); Mtb8 and Mtb48, kindly supplied by Raymond Houghton of Corixa Corp. (Seattle, WA); MPB70 and MPB83, produced at the Veterinary Sciences Division (Stormont, United Kingdom); and α-crystallin (Acr1) and the 38-kDa protein, purchased from Standard Diagnostics (Seoul, South Korea). Hybrids CFP10/ESAT-6 and Acr1/MPB83 were constructed at the Statens Serum Institut (Copenhagen, Denmark) by overlapping PCR with gene-specific oligonucleotides to amplify the genes from M. tuberculosis H37Rv chromosomal DNA. The fused polygene PCR products were cloned into the pMCT6 Escherichia coli expression vector with the SmaI/BamHI restriction enzymes. Polyprotein fusions TBF10 and TBF6 were developed by Corixa Corp. and purified as described earlier (18). Both constructs included Mtb8, CFP10, and the 38-kDa protein; TBF6, additionally, had Mtb48 sequence. The M. bovis culture filtrate used in the MAPIA was obtained from a field strain of M. bovis (T/91/1378; Veterinary Sciences Division, Belfast, United Kingdom) cultured in synthetic Sauton's medium for 21 days.
MAPIA.
The MAPIA immunoassay was performed as previously described (21). Briefly, purified antigens were immobilized on nitrocellulose membrane (Schleicher & Schuell, Keene, NH) at a protein concentration of 0.05 mg/ml with a semiautomatic microaerosolization device (Linomat IV; Camag Scientific Inc., Wilmington, DE) to generate invisible parallel bands. After antigen printing, the membrane was cut into strips 3.5 mm wide, perpendicular to the antigen bands, so that each strip carried all of the antigens. Next, the strips were blocked for 1 h with 1% nonfat skim milk in phosphate-buffered saline containing 0.05% Tween 20 and then incubated with individual serum samples diluted 1:50 in blocking solution for 1 h at room temperature. After washing, the strips were incubated for 1 h with peroxidase-conjugated protein G (Sigma) diluted 1:1,000 (Kirkegaard & Perry Laboratories), followed by another washing step. Immunoglobulin G (IgG) antibodies bound to immobilized antigens were visualized with 3,3′,5,5′-tetramethylbenzidine (Kirkegaard & Perry Laboratories). MAPIA results were scored by two independent operators, with a band of any intensity being read as a positive reaction.
PrimaTB STAT-PAK assay.
The lateral-flow kit for rapid detection of antibodies against M. tuberculosis and M bovis in NHP (Chembio Diagnostic Systems, Inc., Medford, NY) uses a cocktail of recombinant antigens including ESAT-6, CFP10, MPB83, and TBF10, as well as a blue latex bead-based signal detection system. The ready-to-use disposable device consists of a plastic cassette containing a strip of nitrocellulose membrane impregnated with test antigen and laminated with several pads made of glass fiber and cellulose. The test requires a 30-μl serum sample (plasma or whole blood) and 3 drops of sample diluent buffer (included in the kit) that are added sequentially to the sample pad. As the diluted sample migrates to the conjugate pad, the latex particles conjugated to the antigen bind the antibody, if present, thus creating a colored immune complex. Driven by capillary forces, the complex flows laterally across the nitrocellulose membrane and binds to the immobilized antigen, thus producing a visible blue band in the test area of the device. In the absence of a specific antibody, no band develops in the test window. The liquid continues to migrate along the membrane, producing a similar blue band in the control area of the device, irrespective of the presence of a specific antibody in the test sample, demonstrating that the test reagents are functioning properly. Results are read visually 20 min after diluent addition. Any visible band in the test area, in addition to the control line, is considered an antibody-positive result. The absence of a band in the test area is considered an antibody-negative result. Figure 1 shows examples of PrimaTB STAT-PAK assay results obtained with antibody-positive and -negative samples.
FIG. 1.
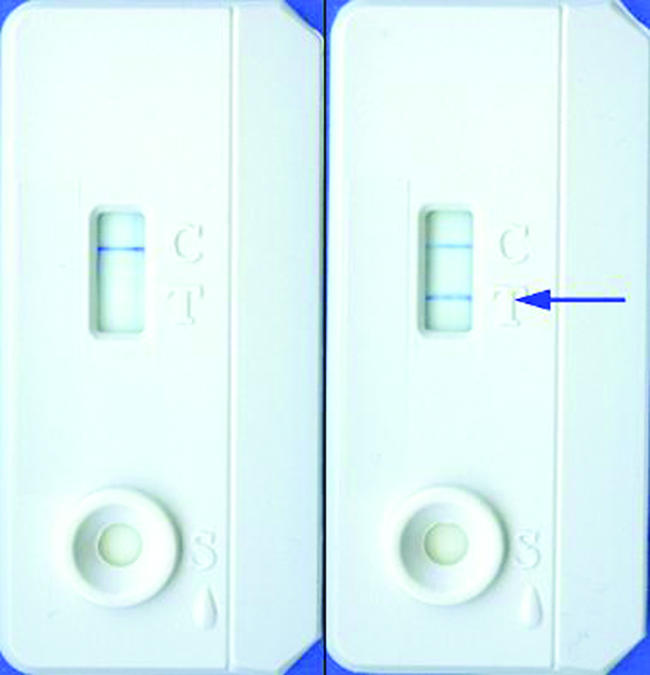
The PrimaTB STAT-PAK assay, a rapid lateral-flow test for TB antibody detection in NHP. Shown are a negative result (on the left) and a positive result (on the right); in the test window, the upper line present in both devices is a control band; the lower line shown with an arrow is the test band indicating a positive result.
RESULTS
Antibody responses and antigen recognition.
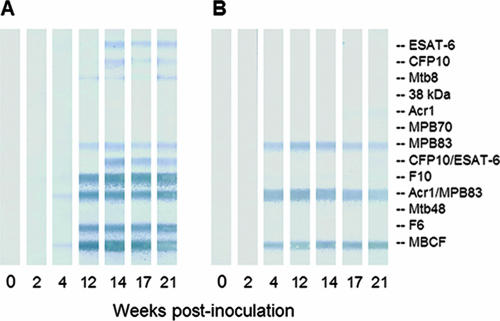
The humoral immune response during experimental TB was characterized in 14 rhesus monkeys infected with M. tuberculosis at the TNPRC and the University of South Alabama. To identify immunodominant antigens, MAPIA was performed with serum samples sequentially collected at different time points during infection. Examples of MAPIA strips obtained with serial specimens collected from two of the infected monkeys representing different antigen reactivity patterns are shown in Fig. 2. The overall results of the antigen recognition study are summarized in Table 2.
FIG. 2.
Serum IgG antibody responses in rhesus macaques experimentally infected with M. tuberculosis. MAPIA was performed as described in Materials and Methods. Panels: A, monkey no. 304; B, monkey no. 595. Each panel of strips shows results obtained with a set of serum samples serially collected over time from an experimentally infected monkey. Each strip represents one serum sample collected at the time point indicated. Bands on MAPIA strips show the presence of antibodies to antigens printed onto the membrane (listed on the right).
TABLE 2.
Antigen recognition by serum antibodies in 14 rhesus macaques infected with M. tuberculosis at the TNPRC and the University of South Alabama
| Antigen | No. (%) of antibody reactors |
|---|---|
| Single proteins | |
| ESAT-6 | 10 (71) |
| MPB83 | 10 (71) |
| CFP10 | 7 (50) |
| Acr1 | 6 (43) |
| MPB70 | 5 (36) |
| Mtb8 | 2 (14) |
| 38 kDa | 1 (7) |
| Mtb48 | 0 (0) |
| Polyprotein fusions | |
| CFP10/ESAT-6 | 11 (79) |
| Acr1/MPB83 | 12 (86) |
| TBF10 | 9 (64) |
| TBF6 | 9 (64) |
The infected animals started producing antibodies at various time points postinoculation. Specific IgG responses could be detected as early as 4 weeks after a challenge with M. tuberculosis. The postinfection serum samples from different monkeys showed various recognition patterns reacting with one or more antigens in the MAPIA (Fig. 2). Seven of eight single recombinant proteins and all four polyprotein fusions were reactive with samples from at least one monkey. None of the antigens was positive with preinfection serum samples. The most frequently recognized proteins were ESAT-6 and MPB83, followed by CFP10, Acr1, MPB70, Mtb8, and the 38-kDa protein of M. tuberculosis (Table 2). The polyproteins had particularly strong reactivity with serum samples that recognized single antigens which were part of the respective fusions (Fig. 2).
Analysis of ESAT-6 and MPB83 seroreactivities.
Antibody responses against the two most dominant antigens were further characterized (Table 3). We tested serial serum samples from infected monkeys by MAPIA in three independent experiments (two at the TNPRC and one at the University of South Alabama) to compare antigen recognition patterns, the magnitudes of the antibody responses, and the times from inoculation of M. tuberculosis to onset of seroconversion found with these antigens because detection of earlier and stronger antibody responses may provide a more robust TB test. We found that in each experiment the infected monkeys produced a spectrum of antibody responses of various magnitudes and antigen recognition profiles. There appeared to be no difference between the animal groups infected with different doses (30, 100, or 210 CFU) or strains of M. tuberculosis (Erdman or H37Rv). Interestingly, while the total numbers of antibody reactors to ESAT-6 and MPB83 were identical (10/14), the proportions of earlier antibody responders to each of the antigens were significantly different (seven for MPB83 versus three for ESAT-6 and three for both antigens simultaneously). One animal (no. 653) recognized neither of the two antigens but had antibody against CFP10.
TABLE 3.
Animal-to-animal variation of antibody recognition of the two immunodominant antigens during experimental TB in rhesus macaques evaluated at the TNPRC and the University of South Alabama
| M. tuberculosis strain (dose [CFU]) and animal identification no. | Antibody responsea
|
|
|---|---|---|
| ESAT-6 | MPB83 | |
| Erdman (30) | ||
| 209 | ++ | − |
| 283 | ++ | + |
| 304 | + | + |
| 653 | − | − |
| 814 | + | ++ |
| Erdman (100) | ||
| 847 | + | + |
| 855 | + | + |
| 861 | − | + |
| 867 | + | − |
| 056 | − | + |
| H37Rv (210) | ||
| 590 | + | − |
| 595 | − | +++ |
| 727 | + | + |
| 729 | +++ | +++ |
The results for antigens eliciting the earliest antibody in each infected animal are in bold. The magnitude of the antibody response was visually scored for each antigen as very strong (+++), strong (++), weak (+), or nonreactive (−).
Although each of the two immunodominant proteins, ESAT-6 and MPB83, was reactive in 71% of the infected monkeys, a combination of the two antigens in the MAPIA detected 93% (13/14) of this group. By week 12 postinoculation, antibody against at least one recombinant antigen in the panel was present in 100% of the infected monkeys, thus suggesting that a multiantigen cocktail would provide optimal serodiagnostic sensitivity.
Development and evaluation of the PrimaTB STAT-PAK assay.
On the basis of the antigen screening results, we selected ESAT-6, CFP10, MPB83, and TBF10 for inclusion in the antigen cocktail to develop a lateral-flow test. These antigens, when combined, were sufficient to cover animal-to-animal variation in antibody reactivity patterns. The ESAT-6 and CFP10 proteins were incorporated as a CFP10/ESAT-6 hybrid molecule which displayed superior antigen reactivity over the single proteins (an example is shown in Fig. 2A). Several key lateral-flow assay conditions (antigen coating concentration, membrane type, sample diluent composition, and conjugate type) were optimized to provide the best discrimination between TB and control serum samples.
The PrimaTB STAT-PAK assay developed was then evaluated with serum samples from the experimentally infected rhesus macaques used for the MAPIA-based antigen screening work, as well as with additional specimens derived from other experimental infection studies performed with rhesus, cynomolgus, and African green monkeys. Extended control groups of the same species were also included.
We found that the serological performance of the PrimaTB STAT-PAK assay was in agreement with the MAPIA data obtained with the same set of serum samples. The rapid test was able to detect serum antibody in all three host species starting at 4 to 8 weeks postinfection with relatively high diagnostic accuracy. The overall sensitivity of the PrimaTB STAT-PAK assay in this evaluation was 90.0%, and the specificity was 98.9% (Table 4). On the basis of these results, the positive predictive value was 91.8% and the negative predictive value was 98.7%. When the specificity of the PrimaTB STAT-PAK assay was challenged in one of the TNPRC experiments with rhesus macaques inoculated twice with M. avium or M. kansasii, no serological cross-reactivity was found in the six monkeys used in the study.
TABLE 4.
Diagnostic performance of the PrimaTB STAT-PAK assay evaluated at the five research sites
| Monkey species | % Sensitivity (no. positive/total) | % Specificity (no. positive/total) |
|---|---|---|
| Rhesus | 89.7 (26/29) | 98.6 (216/219) |
| Cynomolgus | 93.8 (15/16) | 100.0 (30/30) |
| African green | 80.0 (4/5) | 99.2 (127/128) |
| All | 90.0 (45/50) | 98.9 (373/377) |
How the PrimaTB STAT-PAK assay compares with other antemortem tests.
The intrapalpebral tuberculin test was repeatedly performed during experimental TB in two of the studies reported here, one at the University of South Alabama with five rhesus macaques and the other at Merck Research Laboratories (MRL) with 17 NHP including groups of rhesus, cynomolgus, and African green monkeys. The antibody responses could therefore be compared with the skin test results obtained with these animals at the same time points during infection.
In the University of South Alabama study, positive skin test results were documented at week 6 in two of five infected monkeys and at week 8 in one of five infected monkeys; none was reactive at week 4 or between weeks 8 and 14 (end of study). The PrimaTB STAT-PAK assay started showing positive results by weeks 6 and 8 of infection (one of five and two of five, respectively), followed by consistent antibody detection in four of five infected monkeys in the following 6 weeks.
In the MRL experiment, the PrimaTB STAT-PAK assay was compared with the intrapalpebral tuberculin test, bacterial culture, and PCR-based probes with tracheal wash samples over the course of infection (Table 5). We found that while the skin test was most sensitive (88%) at 4 weeks postinoculation, its diagnostic value declined drastically in the following 4 to 8 weeks and no MOT reactors were detected after 2 months postinoculation until the end of the experiment (up to 8 months). In contrast, the PrimaTB STAT-PAK assay turned increasingly positive between weeks 4 and 8 postinoculation, consistently detecting 100% of the infected monkeys thereafter. Tracheal wash culture and PCR testing showed variable performance with intermittent positive and negative results obtained with the same animals. If the skin test and the PrimaTB STAT-PAK assay are combined, such a testing algorithm holds promise to be the most sensitive diagnostic approach for the early and reliable detection of TB in NHP (Table 5).
TABLE 5.
Numbers of positive results obtained by different methods over the course of experimental infection with M. tuberculosis in NHP performed at MRL
| Method | No. positive/total (%) at postinoculation wk:
|
||||||
|---|---|---|---|---|---|---|---|
| 0 | 4 | 8 | 12 | 16 | 20 | 24 | |
| Skin testa | 0/17 (0) | 15/17 (88) | 7/17 (41) | 0/6 (0) | 0/6 (0) | 0/6 (0) | 0/6 (0) |
| PrimaTB STAT-PAK | 0/17 (0) | 3/17 (18) | 10/15 (67) | 11/11 (100) | 10/10 (100) | 10/10 (100) | 8/8 (100) |
| Tracheal wash culture | 0/17 (0) | 7/17 (41) | 8/17 (47) | 9/12 (75) | 5/7 (71) | 6/10 (60) | 5/8 (63) |
| Tracheal wash PCR | 0/17 (0) | 4/17 (24) | 5/17 (29) | 2/12 (17) | 1/9 (11) | 5/10 (50) | 4/8 (50) |
| Skin test + PrimaTB STAT-PAK | 0/17 (0) | 16/17 (94) | 14/17 (82) | 11/11 (100) | 10/10 (100) | 10/10 (100) | 8/8 (100) |
Starting at 12 weeks postinoculation, the skin test was performed only on the group of six infected cynomolgus monkeys.
DISCUSSION
TB control programs in NHP research colonies require urgent improvements of testing methods. The only USDA-approved technology, the intradermal palpebral tuberculin test, has serious limitations. Both false-negative and false-positive reactions are common, often resulting in spread of infection and devastating TB outbreaks or leading to unjustified euthanasia of valuable noninfected animals (15, 32). To further complicate early diagnosis, symptoms suggestive of TB in NHP are not always obvious to help recognize disease. In a recent TB outbreak due to M. bovis in a conditioned colony, clinical signs were observed in 5 of 8 infected rhesus macaques and only 1 of 19 infected cynomolgus macaques (14). In the latter group, the intrapalpebral MOT test failed to identify three infected monkeys, suggesting that additional diagnostic methods must be implemented to improve TB screening programs.
Blood-based immunoassays constitute a promising alternative for TB detection (1, 23). Tuberculin-induced lymphocyte transformation methods showed promise in early studies (2, 5, 27), but this approach has never resulted in the development of a diagnostic test. Recent studies evaluated the whole-blood in vitro gamma interferon assay (Primagam; Prionics, Schlieren-Zurich, Switzerland) in experimental and natural infections (13, 32). Although encouraging results were presented in comparison with the tuberculin skin test, the authors revealed interspecies differences and recommended a certain optimization of the Primagam interpretation cutoff values, particularly for cynomolgus macaques (13). This laboratory immunoassay requires dedicated equipment and technical expertise.
Antibody detection methods are simple, rapid, accurate, and relatively inexpensive. Attempts have been made to develop a serodiagnostic TB test for NHP by using various antigens and techniques (3, 7, 9, 20, 24). Lateral-flow technology offers important features that make it a most attractive and user-friendly immunoassay format, especially for animal-side applications. Although numerous attempts to develop a rapid serodiagnostic test for human TB have been disappointing (28, 29, 30), the potential of this approach for TB detection in animals has been recently demonstrated (16, 23). In the present report, we describe the development and evaluation of the PrimaTB STAT-PAK assay, a novel, rapid lateral-flow device for the detection of antibodies to M. tuberculosis in NHP. The test uses a unique cocktail of selected M. tuberculosis recombinant antigens. The PrimaTB STAT-PAK assay is an easy-to-perform all-inclusive disposable kit which can use serum, plasma, or fresh whole-blood samples to provide yes-or-no results within 15 to 20 min. The test is stable at room temperature for up to 12 months, and it does not require refrigeration for storage, electricity, equipment, laboratory setting, or skilled personnel. In addition to the visual reading option, an optical reader can be used (23), if desired, for printable numerical readouts, as well as data documentation and storage. This novel immunodiagnostic method is an improvement over the current tuberculin test in that it can produce almost instant results instead of the currently required 72 h of repeated observations.
To develop the PrimaTB STAT-PAK assay, we first characterized the antibody responses of rhesus macaques with experimental TB. The primary goal was to identify the seroreactive antigens by MAPIA with serum samples serially collected from monkeys inoculated with M. tuberculosis. The present study has confirmed that ESAT-6 is among the most prominent proteins of M. tuberculosis recognized by antibodies during TB in NHP (3). We have also found that the CFP10/ESAT-6 hybrid used in the membrane-based immunoassays is a more sensitive reagent for the detection of anti-ESAT-6 antibody than the single ESAT-6 protein. Further, we identified another prominent B-cell antigen, MPB83, which showed a rate of seroreactivity (71%) equal to that of ESAT-6 but stronger recognition at earlier stages of infection. These two proteins were combined with CFP10 and TBF10 for the development of the PrimaTB STAT-PAK assay. Importantly, the selected antigens are known to be specific for the M. tuberculosis complex, thus providing the necessary basis for a highly accurate TB serodiagnostic test (1).
Evaluation of the PrimaTB STAT-PAK assay with well-characterized serum samples from 50 infected and 377 control NHP including rhesus, cynomolgus, and African green monkeys showed that the test could detect serum antibody in all three species. The PrimaTB STAT-PAK assay demonstrated high positive and negative predictive values, correctly identifying 90% of the animals in the infected group and 99% of the animals in the control group. Importantly, the test did not have any cross-reactivity with serum samples from monkeys inoculated with M. avium or M. kansasii, the species known to be involved in non-TB mycobacterioses in NHP that can produce false-positive tuberculin skin test reactions (15, 17, 19).
The MRL study revealed noticeable differences among the three NHP species in susceptibility to experimental TB and the clinical course of the disease. African green monkeys were exquisitely sensitive to M. tuberculosis inoculation, with all five animals in the group euthanized within 2 months of infection because of persistent clinical signs such as coughing, anorexia, and/or weight loss. They displayed intermittent-to-chronic coughing from about 4 weeks postinoculation until termination. Rhesus monkeys had a variable course of disease, with four animals euthanized between 2 and 6 months postinfection and two animals euthanized at 7.5 months (study termination). They all coughed from 1 to 5 months postinoculation. Cynomolgus monkeys displayed a more chronic infection, with two animals euthanized at 5.5 and 7 months, respectively, and the other four at study termination. In this group, three of the six cynomolgus monkeys coughed between 3 and 6 months postinoculation. On necropsy, all of the animals had gross evidence of TB and M. tuberculosis was isolated via culture and PCR assay of various tissues. Pathology was generally related to the length of time the disease progressed, with all of the animals displaying various degrees of severity of generalized disseminated TB. Acute, multifocal necrosis was seen in tissues from the vervets, granulomas with multinucleate giant cells were present in rhesus monkey tissues, and caseous granulomas with mature fibrous connective tissue capsules were apparent in the cynomolgus monkeys. Importantly, the PrimaTB STAT-PAK assay could detect specific antibody in all of the infected monkeys, irrespective of the host species, the clinical course of the disease, the extent of pathology, and the results of other diagnostic tests.
One common limitation of the serodiagnostic methods compared to the cell-mediated immune response assays, such as the intradermal test or Primagam, is that antibody responses in TB typically develop at later stages of infection (1, 22). In this study, we have demonstrated, however, that certain antigens, such as MPB83, can elicit antibodies much earlier than others and that the PrimaTB STAT-PAK assay can detect infected monkeys as early as week 4 of infection. Furthermore, the diagnostic window may be reduced by the use of more than one assay. Since the PrimaTB STAT-PAK assay could detect antibody in the infected monkeys with advanced disease which became consistently negative by the tuberculin skin test (anergic), we suggest that a combined application of the two tests will likely provide the best testing algorithm for earlier and more reliable detection of TB in NHP. Our recent observations in several TB outbreaks where the PrimaTB STAT-PAK assay was compared with the tuberculin test and Primagam support this view (K. P. Lyashchenko, unpublished data).
The present report does not address two important questions, i.e., (i) whether the experimental infection models used for test development and evaluation adequately reflect naturally occurring disease and (ii) whether the PrimaTB STAT-PAK assay can detect TB caused by M. bovis. Preliminary evidence suggests that the PrimaTB STAT-PAK assay can work equally well in natural infections with M. tuberculosis and M. bovis (Lyashchenko et al., unpublished). Additional work is in progress to extend this application to other primate species. Also, the NHP models of latent TB and active disease (11) may offer a useful approach for the further characterization of serological responses in human patients and the development of more accurate TB assays where certain immunological aspects cannot be addressed otherwise.
In summary, the present report described the antibody responses against multiple recombinant proteins of M. tuberculosis over the course of experimental infection in rhesus monkeys. We identified and characterized previously unknown immunodominant antigens and potent fusion polyproteins. A unique cocktail of selected TB-specific antigens was incorporated in the optimized lateral-flow format to develop the PrimaTB STAT-PAK assay. Serologic evaluation of this novel diagnostic tool used alone or in conjunction with the intradermal tuberculin test demonstrated the potential for improved sensitivity of TB screening programs in NHP research colonies.
Acknowledgments
We are grateful to Serge Lyashchenko and Alex Lyashchenko for excellent technical assistance. Certain recombinant antigens used in the MAPIA were kindly supplied by Raymond Houghton.
This project was supported by SBIR grant RR019845 from the NIH.
The content of this report is solely our responsibility and does not necessarily represent the official views of the NIH.
Footnotes
Published ahead of print on 25 July 2007.
REFERENCES
- 1.Andersen, P., M. E. Munk, J. M. Pollock, and T. M. Doherty. 2000. Specific immune-based diagnosis of tuberculosis. Lancet 3561099-1104. [DOI] [PubMed] [Google Scholar]
- 2.Baram, P., L. Soltysik, and W. Condoulis. 1971. The in vitro assay of tuberculin hypersensitivity in Macaca mulatta sensitized with Bacille Calmette Guerin cell wall vaccine and/or infected with virulent Mycobacterium tuberculosis. Lab. Anim. Sci. 21727-733. [PubMed] [Google Scholar]
- 3.Brusasca, P. N., R. L. Peters, S. L. Motzel, H. J. Klein, and M. L. Gennaro. 2003. Antigen recognition by serum antibodies in non-human primates experimentally infected with Mycobacterium tuberculosis. Comp. Med. 53165-172. [PubMed] [Google Scholar]
- 4.Capuano, S. V., III, D. A. Croix, S. Pawar, A. Zinovik, A. Myers, P. L. Lin, S. Bissel, C. Fuhrman, E. Klein, and J. L. Flynn. 2003. Experimental Mycobacterium tuberculosis infection of cynomolgus macaques closely resembles the various manifestations of human M. tuberculosis infection. Infect. Immun. 715831-5844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaparas, S. D., R. C. Good, and B. W. Janicki. 1975. Tuberculin-induced lymphocyte transformation and skin reactivity in monkeys vaccinated or not vaccinated with Bacille Calmette-Guérin, then challenged with virulent Mycobacterium tuberculosis. Am. Rev. Respir. Dis. 11243-47. [DOI] [PubMed] [Google Scholar]
- 6.Corcoran, K. D., and G. P. Jaax. 1991. An attempt to predict anergy in tuberculosis suspect cynomolgus monkeys. Lab. Anim. Sci. 4157-62. [PubMed] [Google Scholar]
- 7.Corcoran, K. D., and C. O. Thoen. 1991. Application of an enzyme immunoassay for detecting antibodies in sera of Macaca fascicularis naturally exposed to Mycobacterium tuberculosis. J. Med. Primatol. 20404-408. [PubMed] [Google Scholar]
- 8.DeMarcus, T. A., M. A. Tipple, and S. R. Ostrowski. 1999. US policy for disease control among imported nonhuman primates. J. Infect. Dis. 179(Suppl. 1)S281-S282. [DOI] [PubMed] [Google Scholar]
- 9.Fife, E. H., Jr., R. H. Kruse, A. J. Toussaint, and E. V. Staab. 1970. Serodiagnosis of simian tuberculosis by soluble antigen fluorescent antibody (SAFA) tests. Lab. Anim. Care 20969-978. [PubMed] [Google Scholar]
- 10.Fleischman, R. W., G. C. Du Moulin, H. J. Esber, V. Ilievski, and A. E. Bogden. 1982. Nontuberculous mycobacterial infection attributable to Mycobacterium intracellulare serotype 10 in two rhesus monkeys. J. Am. Vet. Med. Assoc. 1811358-1362. [PubMed] [Google Scholar]
- 11.Flynn, J. L., S. V. Capuano, D. Croix, S. Pawar, A. Myers, A. Zinovik, and E. Klein. 2003. Non-human primates: a model for tuberculosis research. Tuberculosis 83116-118. [DOI] [PubMed] [Google Scholar]
- 12.Fox, J. G., S. M. Niemi, and J. C. Murphy. 1982. A comparison of two tuberculins in nonsensitized macaques. J. Med. Primatol. 11380-388. [PubMed] [Google Scholar]
- 13.Garcia, M. A., J. Yee, D. M. Bouley, R. Moorhead, and N. W. Lerche. 2004. Diagnosis of tuberculosis in macaques, using whole-blood in vitro interferon-gamma (Primagam) testing. Comp. Med. 5486-92. [PubMed] [Google Scholar]
- 14.Garcia, M. A., D. M. Bouley, M. J. Larson, B. Lifland, R. Moorhead, M. D. Simkins, D. C. Borie, R. Tolwani, and G. Otto. 2004. Outbreak of Mycobacterium bovis in a conditioned colony of rhesus (Macaca mulatta) and cynomolgus (Macaca fascicularis) macaques. Comp. Med. 54578-584. [PubMed] [Google Scholar]
- 15.Goodwin, B. T., C. P. Jerome, and B. C. Bullock. 1988. Unusual lesion morphology and skin test reaction for Mycobacterium avium complex in macaques. Lab. Anim. Sci. 3820-24. [PubMed] [Google Scholar]
- 16.Greenwald, R., J. Esfandiari, S. Lesellier, R. Houghton, J. Pollock, C. Aagaard, P. Andersen, R. G. Hewinson, M. Chambers, and K. Lyashchenko. 2003. Improved serodetection of Mycobacterium bovis infection in badgers (Meles meles) using multiantigen test formats. Diagn. Microbiol. Infect. Dis. 46197-203. [DOI] [PubMed] [Google Scholar]
- 17.Holmberg, C. A., R. V. Henrickson, C. Malaga, R. Schneider, and D. Gribble. 1982. Nontuberculous mycobacterial disease in rhesus monkeys. Vet. Pathol. Suppl. 79-16. [PubMed] [Google Scholar]
- 18.Houghton, R. L., M. J. Lodes, D. C. Dillon, L. D. Reynolds, C. H. Day, P. D. McNeill, R. C. Hendrickson, Y. A. W. Skeiky, D. P. Sampaio, R. Badaro, K. P. Lyashchenko, and S. G. Reed. 2002. Use of multiepitope polyproteins in serodiagnosis of active tuberculosis. Clin. Diagn. Lab. Immunol. 9883-891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jackson, R. K., R. A. Juras, S. M. Stiefel, and J. E. Hall. 1989. Mycobacterium kansasii in a rhesus monkey. Lab. Anim. Sci. 39425-428. [PubMed] [Google Scholar]
- 20.Kanaujia, G. V., M. A. Garcia, D. M. Bouley, R. Peters, and M. L. Gennaro. 2003. Detection of early secretory antigenic target-6 antibody for diagnosis of tuberculosis in non-human primates. Comp. Med. 53602-606. [PubMed] [Google Scholar]
- 21.Lyashchenko, K. P., M. Singh, R. Colangeli, and M. L. Gennaro. 2000. A multi-antigen print immunoassay for the serological diagnosis of infectious diseases. J. Immunol. Methods 24291-100. [DOI] [PubMed] [Google Scholar]
- 22.Lyashchenko, K., A. O. Whelan, R. Greenwald, J. M. Pollock, P. Andersen, R. G. Hewinson, and H. M. Vordermeier. 2004. Association of tuberculin-boosted antibody responses with pathology and cell-mediated immunity in cattle vaccinated with Mycobacterium bovis BCG and infected with M. bovis. Infect. Immun. 722462-2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyashchenko, K. P., R. Greenwald, J. Esfandiari, J. H. Olsen, R. Ball, G. Dumonceaux, F. Dunker, C. Buckley, M. Richard, S. Murray, J. B. Payeur, P. Andersen, J. M. Pollock, S. Mikota, M. Miller, D. Sofranko, and W. R. Waters. 2006. Tuberculosis in elephants: antibody responses to defined antigens of Mycobacterium tuberculosis, potential for early diagnosis, and monitoring of treatment. Clin. Vaccine Immunol. 13722-732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mahfouz, O., C. Mahfouz, E. O. Fraser, and A. B. MacDonald. 1980. An immunofluorescence test for detection of antibodies to Mycobacterium tuberculosis. Tubercle 611-9. [DOI] [PubMed] [Google Scholar]
- 25.McLaughlin, R. M., J. R. Thoenig, and G. E. Marrs. 1976. A comparison of several intradermal tuberculins in Macaca mulatta during an epizootic of tuberculosis. Lab. Anim. Sci. 2644-50. [PubMed] [Google Scholar]
- 26.Michel, A. L., and H. F. Huchzermeyer. 1998. The zoonotic importance of Mycobacterium tuberculosis: transmission from human to monkey. J. S. Afr. Vet. Assoc. 6964-65. [DOI] [PubMed] [Google Scholar]
- 27.Muscoplat, C. C., C. O. Thoen, R. M. McLaughlin, J. R. Thoenig, A. W. Chen, and D. W. Johnson. 1975. Comparison of lymphocyte stimulation and tuberculin skin reactivity in Mycobacterium bovis-infected Macaca mulatta. Am. J. Vet. Res. 36699-701. [PubMed] [Google Scholar]
- 28.Okuda, Y., R. Maekura, A. Hirotani, S. Kitada, K. Yoshimura, T. Niraga, Y. Yamamoto, M. Itou, T. Ogura, and T. Ogihara. 2004. Rapid serodiagnosis of active pulmonary Mycobacterium tuberculosis by analysis of results from multiple antigen-specific tests. J. Clin. Microbiol. 421136-1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perkins, M. D., M. B. Conde, M. Martins, and A. L. Kritski. 2003. Serologic diagnosis of tuberculosis using a simple commercial multiantigen assay. Chest 123107-112. [DOI] [PubMed] [Google Scholar]
- 30.Steingart, K. R., M. Henry, S. Laal, P. C. Hopewell, A. Ramsay, D. Menzies, J. Cunningham, K. Weldingh, and M. Pai. 2007. Commercial serological antibody detection tests for the diagnosis of pulmonary tuberculosis. PLoS Med. 4e202 [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tauraso, N. M. 1973. Review of recent epizootics in nonhuman primate colonies and their relation to man. Lab. Anim. Sci. 23201-210. [PubMed] [Google Scholar]
- 32.Vervenne, R. A., S. L. Jones, D. van Soolingen, T. van der Laan, P. Andersen, P. J. Heidt, A. W. Thomas, and J. A. Langermans. 2004. TB diagnosis in non-human primates: comparison of two interferon-gamma assays and the skin test for identification of Mycobacterium tuberculosis infection. Vet. Immunol. Immunopathol. 10061-71. [DOI] [PubMed] [Google Scholar]
- 33.Walsh, G. P., E. V. Tan, E. C. dela Cruz, R. M. Abalos, L. G. Villahermosa, L. J. Young, R. V. Cellona, J. B. Nazareno, and M. A. Horwitz. 1996. The Philippine cynomolgus monkey (Macaca fascicularis) provides a new nonhuman primate model of tuberculosis that resembles human disease. Nat. Med. 2430-436. [DOI] [PubMed] [Google Scholar]
- 34.Waters, W. R., M. V. Palmer, J. P. Bannantine, D. L. Whipple, R. Greenwald, J. Esfandiari, P. Andersen, J. McNair, J. M. Pollock, and K. P. Lyashchenko. 2004. Antigen recognition by serum antibodies in white tailed-deer (Odocoileus virginianus) experimentally infected with Mycobacterium bovis. Clin. Diagn. Lab. Immunol. 11849-855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zumpe, D., M. S. Silberman, and R. P. Michael. 1980. Unusual outbreak of tuberculosis due to Mycobacterium bovis in a closed colony of rhesus monkeys (Macaca mulatta). Lab. Anim. Sci. 30237-240. [PubMed] [Google Scholar]