Abstract
Background
Type 2 diabetes is becoming more prevalent and its successful management relies on patients' self-care behaviours. Measures focusing on patients' perceptions can be effective behavioural interventions.
Aim
To gain insight into the perceptions of patients with diabetes, especially ideas of the illness course and perceived severity, and their impacts on self-care behaviour.
Design of study
Qualitative approach with in-depth patient interviews (n = 22) and seven focus groups (n = 53).
Setting
A rural town in Taiwan.
Method
The interview protocol was mainly derived from Kleinman's explanatory model. Purposive sampling strategies of maximum variation were used. The transcript of the interviews was analysed with editing and immersion/crystallisation styles.
Results
Diabetes is regarded as an incurable, inevitably deteriorating disorder of sugar metabolism with many chronic complications. Patients thought that renal injury, followed by blindness, leg amputation, and poor peripheral circulation, were the most frequent complications. They also assessed their perceived severity of the disease at specific points in time through different indicators in their daily lives, such as sugar level, presence of complications, and medications used. Patients felt that these aspects progressed concurrently and that the illness course followed a unidimensional process. The ever-increasing doses of medication was considered by these patients to be a side-effect of the drugs taken.
Conclusion
Physicians should clarify with their patients that the risks of uraemia, blindness, and leg amputation are less prevalent than expected and that patients should pay more attention to cardiovascular complications. Certain oral hypoglycaemic agents may not cause a vicious cycle of ever-increasing doses of medication and the drugs that need to be taken should not be seen as indicators of severity but, rather, measures taken to prevent the diabetes becoming severe in the future.
Keywords: cognition, illness course, patient non-adherence, qualitative research, severity of illness, type 2 diabetes
INTRODUCTION
Type 2 diabetes and its complications are becoming more prevalent around the world.1 Several clinical trials have demonstrated the benefits of aggressive treatments2,3 that rely heavily on self-management.4 The development of more effective behavioural strategies to promote adherence is needed to achieve maximum benefit to the patient.
To better understand patients' self-care behaviours many researchers have examined cognitive factors, such as patients' perceptions of their diseases;5,6 these factors can be changed to enable more effective behavioural interventions.6 Among different models proposed, Kleinman's explanatory model with five components (aetiology, time and mode of onset of symptoms, pathophysiology, course of sickness, and treatment),7 is well known for being culture sensitive and context rich.8,9
Leventhal et al, proposed a similar construct ‘illness representation’, which also has five attributes (identity, timeline, causal, controllability, and consequences), in their self-regulatory model and provided another useful framework.10 One of the unique contributions of this model is the attribute of ‘identity’. As some patients with early diabetes have no symptoms, the attribute of identity — indicating that the disease can be identified by the placed-on label, concrete signs, or symptoms11 — can portray the illness more adequately than the second component of the explanatory model, namely ‘time and mode of onset of symptoms’. These personal models were integrated dynamically with the contextual environment, addressing the changing nature of laymen's beliefs about illness.9,11
Illness course is the time-extended and richly informative component of the explanatory model and self-regulatory model. Many researchers regard it as an important theme from the patients' viewpoint.12 The construct of perceived severity, which is part of illness course in the explanatory model, was first proposed in the health belief model.5 It has been argued that it has a positive relationship with self-care behaviour in patients with diabetes.13–15 This and other severity-related notions15,16 focus on the disease as a whole, explaining the patients' perception of how serious it is.
This article presents the results of a qualitative study with in-depth interviews and focus groups of Chinese patients with type 2 diabetes. With the exception of the analysis of patients' ideas relating to treatment strategies, which have been reported elsewhere,17 the presentations given here focus on participants' perceptions of diabetes per se, including identity and illness course. An alternative meaning of ‘perceived severity’ is also proposed as an estimate of a patient's health status at a specific point in time. Finally, patients' notions found in this study that are incompatible with current biomedical knowledge as sources of non-adherence are highlighted and explanations and clarifications that need to be given during medical encounters are suggested.
METHOD
This study was performed in a rural town in central Taiwan. This town, with a population of around 70 000, has several economic activities, including agriculture, fishing, and light industry. People in this town, typical of those in Taiwan, were immigrants or offspring of immigrants who had come from mainland China either decades or hundreds of years ago. Traditional Chinese medicine (TCM) is still popular and supported by government policy as it is reimbursed by national health insurance. With comprehensive healthcare services supported by national health insurance (implemented in 1995), most Taiwanese, with £4–8 co-payment, can see their doctors without making an appointment in advance. There is little difference between the quality of healthcare services in rural and urban areas.
How this fits in
Patients' ideas of illness course and perceived severity of the disease as a whole were assumed to be associated with their adherent behaviours. In this article, an alternative meaning of perceived severity as an estimate of somebody's health status at a specific point in time, which has a different impact on patients' adherent behaviours, is proposed. Patients generally see different indicators of perceived severity in daily life progressing in a concurrent pattern, so they regard the clinical and underlying pathophysiological courses of diabetes as unidimensional processes. Some misconceptions that may result in patients' non-adherent behaviour need to be clarified: patients should pay more attention to cardiovascular, rather then renal, complications; certain oral hypoglycaemic agents may not cause a vicious cycle of ever-increasing medication doses; and the necessary medications should not be seen as indicators of severity but measures to prevent future complications.
A purposive sampling strategy of maximum variation18 was adopted to enrol patients with different demographic backgrounds and to avoid omitting some important layman perspectives. With the help of public health nurses, 22 in-depth interviews and seven focus groups (53 participants) were conducted. All the interviewees and focus group members came from the community case-management programme and had had type 2 diabetes for more than 1 year (Table 1). Recruitment continued until no new themes emerged from the interviews in concurrent data analysis.
Table 1.
Participants' sociodemographic characteristics and health status (n = 53).
| Characteristic | In-depth interviewees | Focus group participants |
|---|---|---|
| Sex | ||
| Male | 12 | 19 |
| Female | 10 | 34 |
| Mean age in years (range) | 60.2 (44–80) | 56.9 (41–78) |
| Mean number of years with diabetes (range) | 8.3 (2–25) | 9.3 (1–25) |
| Status of diabetes (HbA1c level [%]) | ||
| <7 | 9 | 17 |
| 7–9 | 4 | 12 |
| >9 | 2 | 6 |
| Unknown | 7 | 18 |
| Comorbidity | ||
| Hypertension | 9 | 29 |
| Proliferative diabetic retinopathy and background diabetic retinopathy | 2+1 | 5+3 |
| Smoking | 3 | 7 |
| Cardiovascular disorder | 3 | 8 |
| Family history of diabetes mellitus | 9 | 25 |
All the interviews were conducted in community health stations (in-depth interviews from May to October 2002; focus groups from March to June 2004). They were done with predetermined protocols modified from the explanatory7 and self-regulatory models,10 and addressed patients' emotional and cognitive perspectives. Given the fact that some patients had a low level of education, oral consent, witnessed by the first author, was obtained from each patient after explaining the aims and methods of this study and promising confidentiality.
After transcribing the audiotaped dialogues verbatim (in Chinese), the data were analysed using strategies of editing and immersion/crystallisation styles.19 All authors read the transcripts, met for lengthy discussions to reach a consensus on emerging themes, and edited reports. The quotations listed below were translated into English by the first author and corrected by an English teacher, familiar with the Chinese language in Taiwan.
RESULTS
Identity of diabetes and the main features of its illness course
Generally speaking, diabetes was regarded as a ‘disorder of sugar metabolism’, which manifested itself frequently with sugar-related symptoms and was caused by inherited genes and the over-consumption of sugary foods.
Participants further identified several main features of the course of the illness. They believed their illness to be incurable and their current treatment was for sugar control only:
‘Diabetes cannot be cured, I know that clearly. The drugs are only for control; you just have to take them …’ (Male, 80 years old)
Participants also expected and worried about future chronic complications. Renal problems were the complication most often mentioned (11 out of 22 in-depth interviewees) and were regarded by some as a side-effect of hypoglycaemic agents:
‘I'm afraid of xi-shen [dialysis, or literally ‘wash-kidney’ in Chinese], like my mum, her kidney was becoming worse continuously; it's a matter of time …’(Female, 44 years old)
‘…not all diabetic patients get niao-du zheng [uraemia, urine-toxic disorder in Chinese], do they? I think that some diabetics have to get dialysis, some don't. I worry about this. I hear that dialysis is horrible …’ (Female, 49 years old)
‘… it seems that having diabetes for a while will hurt the kidneys … I told the doctor not to give me medicine that would hurt my kidneys … I've heard people say that drugs for sugar and for lowering blood pressure will hurt the kidneys more than other drugs …’ (Female, 67 years old)
Blindness, leg amputation, and poor peripheral circulation were also complications that were frequently mentioned:
‘I think that the worse situation is not being able to see. It's okay to lose one's hearing but not being able to see is the most painful thing …’ (Female, 58 years old)
‘… there are canes or wheelchairs if you can't move your hands or legs, but what would you do if you cannot see. I really worry more about this …’ (Female, 49 years old)
‘Diabetes will only get worse and worse. As you get older, you suffer more. Like my mum — her feet are so sore that she can't walk. The blood doesn't flow to her feet …’ (Female, 49 years old)
Furthermore, they thought that their illness was ‘dreary’ and ‘tortuous’, and would become increasingly severe as time went by:
‘Diabetes has a lot of complications … that's what's bad about diabetes … it's a slow and tortuous process since the complications will appear one by one. Poor eyesight, blood vessels, everything goes bad, not being able to walk and to sit … losing the strength in your legs … it's a long process before you die …’ (Female, 54 years old)
‘If you get diabetes, it'll get long and slow and at the end you will need wash-kidney [dialysis]. Every diabetic needs it in the long run; it's their fate …’ (Female, 44 years old)
Contrary to scientific medical knowledge, stroke and coronary heart diseases were not seen as major long-term complications. Some even regarded strokes as unrelated disorders:
‘My father passed away…he was a diabetic, but he didn't die of diabetes; it was … a kind of stroke …’ (Female, 67 years old)
Perceived severity and its assessment
The concept of perceived severity, as an estimate of health status at a specific point in time, did exist in patients' minds. They indicated, in their daily conversations, the perceived severity of their own or other people's illnesses. Some of them gauged it through their sugar level or complications that caused disabilities:
‘My diabetes is OK, not like some others with sugar levels reaching several hundred …’ (Female, 67 years old)
‘One of my neighbours is more serious. He had two toes cut. It won't get better … How serious? He is already blind in one eye. They call it retinal detachment …’ (Male, 72 years old)
However, some other patients judged how severe their illness was by the medications they were using. They thought that the larger the dose, the more severe their illness:
‘My sugar level is not too bad. Not like my sister; she takes three or four pills every day, two at each meal, three times a day; that's serious …’ (Female, 52 years old)
‘I have an aunt who is 78 years old. Her diabetes is very serious … needs shots [insulin]. It's very serious …’ (Male, 65 years old)
The use of insulin injections, as an indicator of very severe illness, was closely linked to death:
‘If you need an insulin shot, it means the diabetes is more serious … it's more difficult to treat … there's not much time left …’ (Male, 61 years old)
‘If you have to get a shot, you have to get a shot. What can you do? It's that serious … nothing to hesitate about … got to be brave to face the facts. When you reach the end of your life, that's OK … I told [my children] just leave me alone, I will handle it myself. I don't want to lie on a hospital bed. I may hang myself or jump off a building to kill myself …’ (Male, 72 years old)
An ever-increasing dose was recognised by some as an indicator of disease progression. They suspected that it was a side-effect of the drugs taken and created a vicious cycle of drug taking, so they hesitated to increase the dose if they did not see an absolute need for it:
‘I feel that you shouldn't increase your dosage unless you absolutely have to, because the more you add, the more you need later …’ (Female, 53 years old)
Interviewer: ‘… would you worry about taking too much [sic] drugs?
Patient: ‘I think that the more medicine I have taken, the more amount of medicine I have to take every day. So I want to take less [drugs] … to keep my sugar level up to 300 …’ (Male, 52 years old)
Unidimensionality and its impact on health behaviours
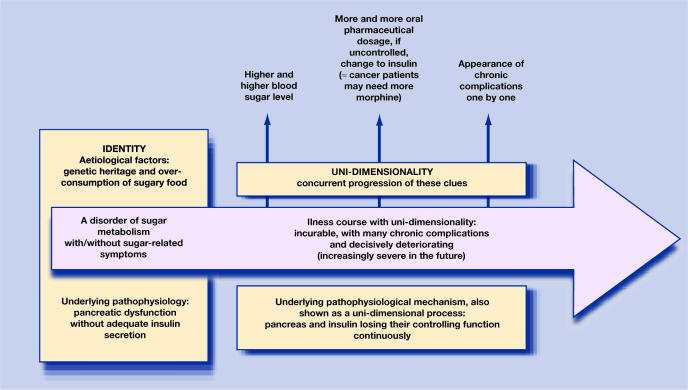
Generally speaking, patients thought of diabetes as incurable and inevitability deteriorating. At the same time, they assessed its perceived severity through different indicators in their daily lives, such as sugar level, dosage of medications, and complications (Figure 1). As most patients were unclear about the complex interplay of different indicators, they regarded them as progressing in a concurrent pattern in their illness courses:
‘If my [sugar level] is raised to more than 300 … [then I need] medication three times every day, before and after each meal … that is about it … it's so bad that [my sugar level] cannot go down, and I'm about to get a stroke … [patients with diabetes have] a higher probability of getting strokes … Diabetes often induces high blood pressure and uncontrolled blood pressure will induce a stroke …’ (Male, 62 years old)
Figure 1.
Three indicators of perceived severity.
Many, therefore, wrongly assumed that the illness progressed in a step-by-step, unidimensional manner:
‘I'm afraid that at the end, just like my cousin says, take drugs, get insulin shots, then washkidney [dialysis], then at last say goodbye [die], step-by-step like that …’ (Female, 44 years old)
The unidimensionality was also reflected in the pathophysiological story that patients told:
‘If you take more and more medication, then it means that your metabolic function in your pancreas is getting worse. If you need insulin shots, that means your pancreas fails totally, cannot work properly … that's the end. Just like cancer … at the end stage, you need morphine. You start with 1cc then two, three … at last, your heart cannot tolerate it and that's it. This is just like when we feel thirsty and need a cup of water to quench it. Now we need two cups, that's being “very” thirsty, that's “serious”.’ (Male, 62 years old)
This unidimensionality was the reason why some patients intentionally refused to adhere to pharmaceutical prescriptions. When asked about opinions regarding insulin shots, one participant responded:
‘I'm thinking, “is it really that serious?”.‘ (Female, 45 years old)
Another participant, based on her assessment of perceived severity, insisted on refraining from increasing her dosage of hypoglycaemic agents:
‘I thought that my pancreas was only a little abnormal. My sugar level is not very high. The doctor told me to take one pill but I insist on taking only half. Since I was first diagnosed, I've always taken only half a pill. It's just for controlling it and preventing it from getting higher …’ (Female, 53 years old)
DISCUSSION
Summary of main findings
The findings of this study demonstrated that the explanatory model and illness representation are useful frameworks in describing the layman's perspective. The extensive content of perceptions of illness course is at the heart of these personal models.
In general, diabetes was identified by these patients as a disorder of sugar metabolism. They generally considered it to be incurable, to have many chronic complications, and expected their condition to deteriorate. They thought that renal problems, followed by blindness, leg amputation, and poor peripheral circulation, were the most frequent complications.
The construct of perceived severity, which means the evaluation of a patient's health status at a specific point in time, was developed in their minds and assessed through different indicators in daily lives including sugar level, disabling complications, and the dose of medications taken. Some participants believed that an ever-increasing dose was not only an indicator of disease progression, but also resulted in a vicious cycle of drug taking that would become addictive.
As most participants didn't realise the complex interplay of these indicators, which were regarded as progressing in a concurrent pattern, they considered their illness as progressing unidimensionally and that the perceived severity could be measured on a unidimensional scale.
Strengths and limitations of the study
This research inherits common strengths of qualitative research, such as emic perspectives, with richly contextual discourse of patients with diabetes. The adoption of the purposive sampling strategy of maximum variation18 and the inclusion of data from in-depth interviews and focus groups further strengthen and justify these conclusions.
This research still suffers some limitations, however. As the analysis was restricted on cross-sectional narrations and without longitudinal or observational data, some patients' memory bias or subjective prejudice would not have been illuminated. In addition, because all participants who had had diabetes for more than a year came from the case-management programme of public health nurses, the perspectives of patients with a new diagnosis, those who may be naïve in terms of education, and those refusing health care were not included in the results.
Comparison with existing literature
The fact that the participants overstated the importance of renal disease may reflect the education they had received and their experience of having diabetes as well as the high incidence rate of diabetic nephropathy in Taiwan.20 This notion may also be accentuated by the metaphor of the kidney in Chinese culture. The kidney is seen as containing the inherited ‘vital essence’ and sperm. A kidney injury is, therefore, viewed quite seriously because of the tightly semantic network between lumbago, kidney deficiency (shen xu), and loss of vital essence, which leads to a shortened lifespan.21 Some of our participants did, however, suggest that renal injury was caused by hypoglycaemic agents.
The ambivalent attitudes towards medication may be universal and span different cultures,22,23 but these attitudes differed in their content and buffering measures. People from traditional Chinese cultural arenas focused on nephrotoxicity and took to sweating and passing urine to eliminate toxins;17,24 those from South Asian cultural areas used traditional foodstuffs to fortify properties and balance out the side-effects of their oral hypoglycaemic agents.23
Another negative perception of medications held by the participants was their concern about the addictive side-effects of drugs. Similar concern regarding psychotropic or antihypertensive medicines was found by many different studies in New Zealand, Germany, and the UK,25 so this notion — which has come about since the introduction of chemical-based Western medicine — may be universal rather than culturally specific.
After reviewing and synthesising many qualitative studies, Pound et al,25 argued that as taking medicine was equated with having an illness, non-acceptance of patients' identity impeded them from taking medicines. They also indicated the tendency to downplay the severity of disease. The current study demonstrated that doses of medications used were also regarded by our patients as something of a bad omen with regards to disease progression. In comparison with current medical recommendations of earlier use of combined oral hypoglycaemic agents and/or insulin injections to prevent future complications, doses of medication should not be regarded as indicators of disease severity.26 This confused idea and non-acceptance of the perceived severity interfered with patients receiving necessary treatment.
Implications for future research and clinical practice
Most of the participants' notions of the course of diabetes and its perceived severity are compatible with orthodox medical knowledge.27 However, the three incompatible notions significantly influencing patients' self-care behaviours that were found in this study should be clarified in medical encounters.
Most participants were concerned about renal failure followed by blindness, leg amputation, and poor peripheral circulation. Some of them thought that uraemia caused by drugs was their ‘decisive life destiny’. Many patients did not pay attention to, and even neglected to, take note of cardiovascular complications. These notions, similar to the findings of a UK qualitative study,27 may promote unnecessary worries and result in patients disregarding necessary beneficial treatments. According to orthodox medical knowledge, cardiovascular complications are the major cause of death in this population.28 Uraemia, blindness, and leg amputations are less prevalent than expected;29 their risk can be reduced substantially by strictly controlling blood pressure and sugar levels.2,3,28
As diabetes was regarded as an inevitably deteriorating condition and pharmaceutical doses (or the use of insulin) were seen as indicators in assessing severity, ever-increasing doses were not only seen as an indicator of disease progression, but also suspected to be a vicious cycle related to the side-effects of the drugs. This idea is similar to the notion of addiction, which has been cited as laymen's negative views regarding medication, and one of the key reasons for intentional non-adherence. 22 Recent clinical trials have demonstrated that some hypoglycaemic agents can delay the onset of type 2 diabetes in populations considered to be at high risk,30,31 partially refuting this addictive hypothesis held by these patients. This argument, if confirmed by further biomedical investigations, should be widely disseminated to dispel the fear of drug addiction.
The last incompatible notion reported here regards unidimensional illness course. As some patients regarded different indicators of severity as concurrent progression, indicating the underlying pathophysiological course of pancreatic dysfunction, they wrongly assumed that their illness progressed in a unidimensional course and, as such, perceived severity to be on a unidimensional scale. In current orthodox medicine, more aggressive approaches with earlier commencement of oral combination therapy and/or insulin should be considered to achieve tighter glycaemic control, thereby reducing future risks of complications.26 Necessary doses of hypoglycaemic agents should not be seen as indicators for severity, therefore, but as measures to prevent illness progression and future problems.
Based these findings, it is suggested that some notions of the illness course that may be negatively associated with self-care behaviours should be clarified in medical encounters:
The risks of uraemia, blindness, and leg amputation are less prevalent than cardiovascular diseases and can be reduced by strict controlled management. Patients should put this worry aside and pay more attention to cardiovascular complications.
There is no evidence of the existence of addictive side effects in terms of hypoglycaemic drug taking and patients should be made aware of this when an in increase in dose is suggested.
It is the presence of complications, not medication dose, that indicates illness severity. Necessary doses of hypoglycaemic agents should not be seen as indicators of severity but, rather, as measures to prevent the progression of the disease and it becoming severe in the future.
Acknowledgments
We are indebted to the public nurses for their help and the participants with diabetes for giving us their own perspectives of living with it. This research is a part of the first author's PhD dissertation. We thank the members of the PhD dissertation advisory committee for their helpful comments in the design and implementation of the study.
Funding body
Taichung Veterans' General Hospital Research Programme (915702A)
Ethics committee
The Ethics Committee of College of Public Health, National Taiwan University.
Competing interests
The authors have stated that there are none
REFERENCES
- 1.World Health Organisation. Global burden of diabetes. http://www.who.int/inf-pr-1998/en/pr98-63.html(accessed 28 Feb 2007)
- 2.Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J med. 2003;348(5):383–393. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 3.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 4.Glasgow RE, Fisher EB, Anderson BJ, et al. Behavioral science in diabetes. contributions and opportunities. Diabetes Care. 1999;22(5):832–843. doi: 10.2337/diacare.22.5.832. [DOI] [PubMed] [Google Scholar]
- 5.Sheeran P, Abraham C. The health belief model. In: Conner M, Norman P, editors. Predicting health behaviour: research and practice with social cognition models. Buckingham: Open University Press; 1996. pp. 23–61. [Google Scholar]
- 6.Conner M, Norman P. The role of social cognition in health behaviours. In: Conner M, Norman P, editors. Predicting health behaviour: research and practice with social cognition models. Buckingham: Open University Press; 1996. pp. 1–22. [Google Scholar]
- 7.Kleinman A. Patients and healers in the context of culture. Berkeley: University of California Press; 1980. [Google Scholar]
- 8.McElroy A, Jezewski MA. Cultural variation in the experience of health and illness. In: Albrecht GL, Fitzpatrick R, Scrimshaw SC, editors. The handbook of social studies in health and medicine. London: Sage; 2000. pp. 191–209. [Google Scholar]
- 9.Good BJ. Medicine, rationality, and experience: an anthropological perspective. Cambridge: Cambridge University Press; 1994. [Google Scholar]
- 10.Leventhal H, Benyamini Y, Brownlee S, et al. Illness representations: theoretical foundations. In: Petrie KJ, Weinman JA, editors. Perceptions of health and illness. Singapore: Harwood Academic Publishers; 1997. pp. 19–45. [Google Scholar]
- 11.Scharloo M, Kaptein A. Measurement of illness perceptions in patients with chronic somatic illness: a review. In: Petrie KJ, Weinman JA, editors. Perceptions of health and illness. Singapore: Harwood Academic Publishers; 1997. pp. 103–154. [Google Scholar]
- 12.Hornsten A, Sandstrom H, Lundman B. Personal understandings of illness among people with type 2 diabetes. J Adv Nurs. 2004;47(2):174–182. doi: 10.1111/j.1365-2648.2004.03076.x. [DOI] [PubMed] [Google Scholar]
- 13.Daniel M, Messer LC. Perceptions of disease severity and barriers to self-care predict glycaemic control in Aboriginal persons with type 2 diabetes mellitus. Chronic Dis Can. 2002;23(4):130–138. [PubMed] [Google Scholar]
- 14.Dietrich UC. Factors influencing the attitudes held by women with type II diabetes: a qualitative study. Patient Educ Couns. 1996;29:13–23. doi: 10.1016/0738-3991(96)00930-5. [DOI] [PubMed] [Google Scholar]
- 15.Hampson SE. Illness representations and the self-management of diabetes. In: Petrie KJ, Weinman JA, editors. Perceptions of health and illness. Singapore: Harwood Academic Publishers; 1997. pp. 323–347. [Google Scholar]
- 16.Murphy E, Kinmonth AL. No symptoms, no problem? Patients' understandings of non-insulin dependent diabetes. Fam Pract. 1995;12(2):184–192. doi: 10.1093/fampra/12.2.184. [DOI] [PubMed] [Google Scholar]
- 17.Lai WA, Lew-Ting CY, Chie WC. How diabetic patients think about and manage their illness in Taiwan. Diabet Med. 2005;22(3):286–292. doi: 10.1111/j.1464-5491.2004.01406.x. [DOI] [PubMed] [Google Scholar]
- 18.Kuzel AJ. Sampling in qualitative inquiry. In: Crabtree BF, Miller WL, editors. Doing qualitative research. California: Sage Publications; 1992. pp. 31–44. [Google Scholar]
- 19.Miller WL, Crabtree BF. Primary care research: a multimethod typology and qualitative road map. In: Silverman D, editor. Doing qualitative research. California: Sage Publications; 1992. pp. 3–30. [Google Scholar]
- 20.Ritz E, Tarng DC. Renal disease in type 2 diabetes. Nephrol Dial Transplant. 2001;16(Suppl 5):11–18. doi: 10.1093/ndt/16.suppl_5.11. [DOI] [PubMed] [Google Scholar]
- 21.Ots T. The angry liver, the anxious heart and the melancholy spleen. The phenomenology of perceptions in Chinese culture. Cult Med Psychiatry. 1990;14(1):21–58. doi: 10.1007/BF00046703. [DOI] [PubMed] [Google Scholar]
- 22.Horne R. Representations of medication and treatment: advances in theory and measurement. In: Petrie KJ, Weinman JA, editors. Perceptions of health and illness. Singapore: Harwood Academic Publishers; 1997. pp. 155–188. [Google Scholar]
- 23.Lawton J, Ahmad N, Hallowell N, et al. Perceptions and experiences of taking oral hypoglycaemic agents among people of Pakistani and Indian origin: qualitative study. BMJ. 2005;330:1247. doi: 10.1136/bmj.38460.642789.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mull DS, Nguyen N, Mull JD. Vietnamese diabetic patients and their physicians: what ethnography can teach us. Western J Med. 2001;175:307–311. doi: 10.1136/ewjm.175.5.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pound P, Britten N, Morgan M, et al. Resisting medicines: a synthesis of qualitative studies of medicine taking. Soc SciMed. 2005;61(1):133–155. doi: 10.1016/j.socscimed.2004.11.063. [DOI] [PubMed] [Google Scholar]
- 26.Chan JL, Abrahamson MJ. Pharmacological management of type 2 diabetes mellitus: rationale for rational use of insulin. Mayo Clin Proc. 2003;78(4):459–467. doi: 10.4065/78.4.459. [DOI] [PubMed] [Google Scholar]
- 27.Stewart J, Brown K, Kendrick D, Dyas J. Understanding of blood pressure by people with type 2 diabetes: a primary care focus group study. Br J Gen Pract. 2005;55:298–304. [PMC free article] [PubMed] [Google Scholar]
- 28.American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2005;28:S4–36. [PubMed] [Google Scholar]
- 29.American Diabetes Association. Nephropathy in diabetes. Diabetes Care. 2004;27:S79–83. doi: 10.2337/diacare.27.2007.s79. [DOI] [PubMed] [Google Scholar]
- 30.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl JMed. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chiasson JL, Josse RG, Gomis R, et al. Acarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trial. Lancet. 2002;359:2072–2077. doi: 10.1016/S0140-6736(02)08905-5. [DOI] [PubMed] [Google Scholar]