Abstract
Remodeling of the dermal extracellular matrix occurs during photoaging. Here, the effect of repetitive UVB irradiation on dermal hyaluronic acid (HA) was examined. C57/BL6 mice were chronically (182 days) irradiated with UVB, and consecutive skin biopsies were collected during the irradiation period and afterward (300 and 400 days of age). UVB caused marked loss of HA from the papillary dermis and down-regulation of HA synthase 1 (HAS1), HAS2, and HAS3 mRNA expression. In contrast, hyaluronidases (HYAL) 1, HYAL2, and HA receptor CD44 were unchanged. Furthermore, transforming growth factor β-1 (TGF-β1) and TGF-β1-receptor II expression were decreased in UVB-irradiated biopsies, and TGF-β1 strongly induced HAS1 and HAS2 expression in cultured dermal fibroblasts. Therefore, TGF-β1 might be one factor involved in UVB-induced down-regulation of HAS enzymes. In addition, total cell number and the percentage of proliferating fibroblasts in the papillary dermis of UVB-irradiated mice were decreased. Down-regulation of HAS2 by lentiviral overexpression of short hairpin RNA in vitro caused inhibition of HA synthesis, DNA synthesis, and migration of dermal fibroblasts. In conclusion, chronic UVB irradiation induces loss of HA from the dermis, thereby contributing to the quiescent phenotype of dermal fibroblasts.
Solar UV irradiation of the skin causes sunburn, transient inflammation, cancer, and premature skin aging.1 Photoaging is the most common form of skin damage caused by chronic, repetitive sun exposure.2 The long-term exposure to solar UV irradiation induces damage to the dermal connective tissue and the extracellular matrix (ECM), which in turn leads to the aged appearance of photodamaged skin. Hallmark of this UV-induced ECM remodeling is the degradation of collagen and elastin through the UVB-induced activation of matrix metalloproteinases and decreased de novo synthesis of collagen. The mechanisms of UVB-induced matrix metalloproteinase activation3 and inhibition of collagen synthesis have been studied in detail.2 In contrast the effect of UVB on hyaluronic acid (HA), another key component of the dermal ECM, is much less understood, and the underlying mechanisms are primarily unknown. HA is a linear polymer composed of repeating disaccharides (d-glucuronic acid-β-1,3-N-acetylglucosamine-β-1,4-) and assembled from the respective activated nucleotide sugars (UDP-glucuronic acid, UDP-N-acetylglucosamine) at the inner plasma membrane by HA synthases (HAS). Three different HAS isoforms are known that reside in the plasma membrane and extrude the growing HA polymer into the extracellular space.4 HAS1 and HAS2 produce high molecular mass HA (2 to 4 × 106 Da), whereas HAS3 synthesizes smaller HA (0.4 to 2.5 × 105 Da).5 The variation of the MW is the only modification of HA because O- or N-sulfations do not occur. HA is an agonist of CD44 and RHAMM (receptor of HA-mediated motility), which enables HA to initiate specific signaling events.6 This receptor signaling and the formation of pericellular HA coats supports proliferation and migration of a variety of cell types including skin fibroblasts.7 In addition, antiapoptotic effects of HA have been demonstrated. After fragmentation of HA through limited cleavage by hyaluronidase-1 (HYAL-1) and HYAL-2, low and intermediate MW HA are generated.8 HA fragments in turn activate Toll-like receptors 2 and 4 and thereby modulate inflammatory responses.9,10 In skin, HA also has important structural functions that are related to the unique molecular features of HA. The high polymer length and polyanionic charge enable HA to bind water, which in turn supports volume expansion and turgidity of skin, the diffusion of metabolites and nutrients and the elasticity of the skin.11 Taken together, HA confers functions through the initiation of receptor signaling but also creates an extracellular microenvironment that supports the typical physicochemical and mechanical properties of the skin. Notably, the regulation and function of HAS isoforms have not been determined during skin aging in vivo or in dermal fibroblasts in vitro.
In the epidermis, HA was shown to be induced during wound healing and regeneration.12 In contrast, in the dermis the regulatory pathways of HA are much less understood. Interestingly, several conditions that accelerate skin aging such as estrogen deficiency13,14 are associated with loss of HA from the dermis, and treatments that counteract actinic skin aging such as retinoic acid increase dermal HA.15,16 These results strongly suggest that dermal HA plays an important role during photoaging.
In vivo ∼5% of UVB irradiation is thought to reach the upper dermis.17 Therefore both direct effects of UVB on fibroblasts in the papillary dermis and indirect effects through UVB-mediated responses in epidermal keratinocytes such as changes in gene expression, growth factor, and cytokine release must be considered.18 In addition, acute and chronic consequences of UVB irradiation must be distinguished. Acutely, UVB causes sunburn and transient inflammatory reactions.19 In the long term, UVB irradiation causes remodeling of the skin, ultimately leading to the symptoms of photoaging such as wrinkling, decreased turgidity and elasticity, pigmentation, and neovessel formation.
The aim of the present study was to elucidate further the effects of UVB on dermal HA, the underlying mechanisms, and the function of HA in dermal fibroblasts. In particular, the effect of chronic repetitive UVB irradiation on dermal HA was analyzed. For this purpose adult C57/BL6 mice were irradiated with UVB throughout a period of 182 days and the subsequent changes in HA content, HAS isoenzyme expression, and HYAL expression were determined. The function of HAS2 in dermal fibroblasts in vitro was analyzed by lentiviral expression of shRNA targeting HAS2. The present data show that chronic UVB induces a progressive loss of HA from the upper dermis because of transcriptional down-regulation of all three HAS isoforms. In addition, loss of HA and HAS2 are associated with a quiescent phenotype of dermal fibroblasts.
Materials and Methods
UV Irradiation of Mice
CL57/BL6 mice were housed according to standard procedures. Beginning at the age of 42 days, the backs of all mice were shaved once a week. The animals were divided into a control group that was shaved but not irradiated. The second group was irradiated with UVB light three times per week at a dose of 210 mJ/cm2 [∼three times minimal erythema dose (MED)] throughout a period of 182 days.20 The age of the mice at the end of the irradiation protocol was 224 days (32 weeks). The experimental design is illustrated in Figure 1A. The UVB radiation was provided by UV lamps with fluorescent bulbs (280 to 320 nm with a peak at 313 nm TL 20W/12; Philips, Eindhoven, The Netherlands). The light intensity was determined by means of a UV meter (Waldmann, Villingen-Schwennigen, Germany). All animal experiments have been approved by the local ethical committee for animal experiments.
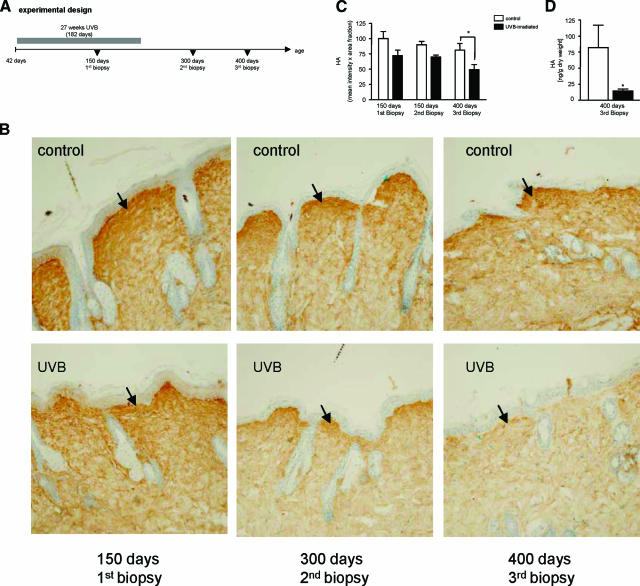
Figure 1.
Progressive loss of HA from the dermis of chronically UVB-irradiated mice. Shaved C57/BL6 mice were either sham-irradiated or UVB-irradiated (three times per week, 3 MED ∼210 mJ/cm2), and consecutive skin biopsies were collected (see Materials and Methods). HA was detected by affinity histochemistry using biotinylated HAbP. A: Experimental design. B: HA staining. Top: Intrinsic aging; sham-irradiated controls at 150, 300, and 400 days. Bottom: Extrinsic aging; UVB-irradiated C57/BL6 mice at 150, 300, and 400 days. Arrows indicate the HA-rich zone in the papillary dermis where loss of HA is strongest. C: Densitometric quantification of HA staining, controls, n = 7, and UVB, n = 8; *P < 0.05 intrinsic aging versus UVB at 400 days (two-way analysis of variance). D: Biochemical quantification of HA in the dermis of controls versus UVB-irradiated skin at 400 days; mean ± SEM, controls, n = 4, and UVB, n = 5; *P < 0.05 (t-test). Original magnifications, ×100.
Murine Skin Biopsies
Skin biopsies were obtained from control and UVB-irradiated animals during the UVB irradiation protocol at 150 days and after the UVB irradiation at 300 and 400 days of age. Mice were anesthetized with an intraperitoneal injection of Ketanest/Rompun, (Pfizer Pharma Gmblt, Karlsrüe, Germany, and Bayer, Leuerküsen, Germany, respectively) and biopsies from the dorsal skin of 1 to 2 cm2 in size were taken. Half of the tissue was subsequently snap frozen in liquid nitrogen for preparation of total RNA and extraction of HA. The other half was immersed in formalin and embedded in paraffin according to standard procedures. Sections of 3 μm in thickness were subsequently cut and deparaffinized by standard methods.
Histochemistry and Immunohistochemistry
HA staining was performed as described previously.21 In brief, deparaffinized sections were blocked with 10% fetal calf serum and 1% bovine serum albumin for 1 hour at room temperature. The slides were subsequently incubated with biotinylated HAbP (2 μg/ml; Seikagaku, Tokyo, Japan) at 4°C overnight. After three washes with phosphate-buffered saline (PBS), the sections were incubated with avidin-biotin peroxidase (Sigma, St. Louis, MO), and the color was developed with 3,3′-diaminobenzidine (DAB; Sigma) containing 0.03% H2O2. Nuclei were stained with hemalaun solution (Merck, Darmstadt, Germany). As a negative control, sections were incubated with Streptomyces hyaluronidase (ICN, Costa Mesa, CA) at a concentration of 2 U/ml (1 hour, 37°C) before HA staining.
Proliferating cell nuclear antigen (PCNA) was stained as a marker for proliferation after antigen retrieval (25 minutes, 10 mmol/L citric acid, pH 6.0, and 0.05% Tween 20). The monoclonal anti-mouse antibody against PCNA (1:1600; Biozol, Eching, Germany) was detected by sheep anti-mouse Cy3-conjugate (1:100, Sigma). In addition, the proliferation marker Ki67 was analyzed using rabbit anti-mouse antibody (1:25; Novus Biologicals, Littleton, CO) and sheep anti-rabbit IgG (Cy3-conjugate, 1:50; Sigma-Aldrich, Steinheim, Germany). For determination of the proliferative index, nuclear staining (blue, Hoechst 33324) was turned into green by analySIS software (Soft Imaging System, Münster, Germany). Total cell counts and PCNA-positive cells were subsequently counted in the same area of the papillary dermis that was also used for quantitation of HA (see below). This area of interest was marked using the ROI brush tool of the Freeware Image J (National Institutes of Health, Bethesda, MD). The number of Hoechst 33324-stained nuclei was set as total cell number. Only those cells that showed a clear overlay (yellow) of the proliferation marker PCNA or Ki-67 stained in red and the nuclei shown in green (originally blue) were assumed to represent proliferating cells. The proliferative index was expressed by the percentage of PCNA-positive or Ki67-positive nuclei. Fibroblasts were detected by the use of polyclonal rabbit anti-vimentin antibody (1:100; Novus Biologicals) and goat anti-rabbit IgG fluorescein isothiocyanate (1:200; Santa Cruz Biotechnology, Santa Cruz, CA).
Image Analysis
Brightfield images were captured of HA affinity histochemistry using a BX-50 microscope (Olympus, Hamburg, Germany) at ×100 magnification and a ColorView II camera (Soft Imaging System). AnalySIS 3.2 software (Soft Imaging System) allowed computer control of image acquisition. For quantification of HA affinity histochemistry, ImageJ 1.37v software (National Institutes of Health) was used to convert bright-field (24-bit) images of DAB stainings to 8-bit images and for all further image processing. DAB-positive and -negative images were used to determine the threshold. Threshold values were chosen that maximize selection of the DAB-positive tissue while minimizing background interference. The resulting threshold values were held constant in the analysis of all images. To quantify the HA content in the DAB-stained sections, the staining parameters percent area and mean intensity were multiplied and normalized. Percent area is defined as the area of the image classified as DAB-stained, divided by the total image area. The mean intensity corresponds to the mean gray scale intensity. The measurements were performed within the first 35 μm below the epidermis, which contains the highest amount of HA. Per skin section the quantification of three randomly selected areas (×100 magnification) were averaged. This analysis was performed two times per biopsy using independently stained sections, and the average of the two sections was used for further calculations. In Figure 1, the HA content is expressed as percentage of nonirradiated control biopsies at 150 days.
Quantitation of HA
Dermal HA was extracted from biopsies after modification of published procedures.22,23 In brief, skin biopsies were lyophilized and dry weight was determined. Subsequently, samples were digested by pronase (protease from Streptomyces griseus, 6 mg/ml in 100 mmol/L Tris-HCl, pH 8, 1 mmol/L CaCl2, and 1500 U/ml heparin, 60°C, 24 hours; Sigma-Aldrich). After ethanol precipitation (12 hours, −20°C) HA was recovered by centrifugation (10,000 × g at 4°C, 15 minutes), washed, lyophilized, and dissolved in distilled water. Samples were then diluted 1:10,000 and HA concentration determined by HA enzyme-linked immunosorbent assay (Corgenix, Peterborough, UK) and normalized to dry weight. In the supernatants of cultured human skin fibroblasts, HA concentration was determined by the HA enzyme-linked immunosorbent assay (Corgenix) 5 days after lentiviral infection and was calculated as ratio of HA and total cellular protein.
RNA Isolation and Quantification of Gene Expression
Total RNA was isolated using RNeasy total RNA kits (Qiagen, Hilden, Germany). The RNA concentration was determined via photometric measurement at 260/280. Aliquots of total RNA (100 ng) were applied for cDNA synthesis using SuperscriptIII first-strand synthesis system for reverse transcriptase-polymerase chain reaction (RT-PCR) (Invitrogen, Karlsruhe, Germany). For analysis of mouse HAS1 to HAS3, transforming growth factor (TGF)-β1, Tβ1R-II, HYAL1, HYAL2, CD44, biglycan (BGN), and GAPDH, the primer sequences are given in Table 1. For analysis of mRNA expression in human fibroblasts, a specific primer pair was designed by Primer Express 2.0 software (Applied Biosystems, Darmstadt, Germany) based on the cDNA sequence published as indicated. The following primer pairs were used: 18SrRNA: sequence of McCallum and Maden24; HAS-1 primer: sequence of Shyjan and colleagues25; HAS-2 primer: sequence of Watanabe and Yamaguchi26; HAS-3 primer: sequence of Liu and colleagues27; matrix metalloproteinase-1 primer: sequence of Whitham and colleagues.28 Five independent experiments were performed with three determinations each, and the mean value of these was calculated. The PCR reactions were performed on an Opticon 1 (MJ Research, Waltham, MA) using SYBR Green PCR Master Mix (Applied Biosystems). For comparison of relative expression in real-time PCR control cells and treated cells, the 2[−ΔΔC(T)] method was used.
Table 1.
Primer Sequences Used for Quantification of Gene Expression
| Gene | Primer sequence |
|---|---|
| Mouse HAS1 | 5′-CTATGCTACCAAGTATACCTCG-3′ |
| 5′-TCTCGGAAGTAAGATTTGGAC-3′ | |
| Mouse HAS2 | 5′-CGGTCGTCTCAAATTCATCTG-3′ |
| 5′-ACAATGCATCTTGTTCAGCTC-3′ | |
| Mouse HAS3 | 5′-GATGTCCAAATCCTCAACAAG-3′ |
| 5′-CCCACTAATACATTGCACAC-3′ | |
| Mouse biglycan | 5′-CTGAGGGAACTTCACTTGGA-3′ |
| 5′-CAGATAGACAACCTGGAGGAG-3′ | |
| Mouse TGFB1 | 5′-CCGCAACAACGCCATCTATG-3′ |
| 5′-CTCTGCACGGGACAGCAAT-3′ | |
| Mouse TGFBR2 | 5′-CAAGTCGGATGTGGAAATGG-3′ |
| 5′-AAATGTTTCAGTGGATGGATGG-3′ | |
| Mouse Hyal1 | 5′-AAGTACCAAGGAATCATGCC-3′ |
| 5′-CTCAGGATAACTTGGATGGC-3′ | |
| Mouse Hyal2 | 5′-GGTGGACCTTATCTCTACCAT-3′ |
| 5′-TATTGGCAGGTCTCCATACTT-3′ | |
| Mouse CD44 | 5′-GACCGGTTACCATAACTATTGTC-3′ |
| 5′-CATCGATGTCTTCTTGGTGTG-3′ | |
| Mouse GAPDH | 5′-TGGCAAAGTGGAGATTGTTGCC-3′ |
| 5′-AAGATGGTGATGGGCTTCCCG-3′ |
Cell Culture
Primary human dermal fibroblasts from different donors were cultured in Earle’s minimum essential medium without glutamine (PAA Laboratories GmbH, Cölbe, Germany), supplemented with antibiotics/antimycotics, 2 mmol/L l-glutamine, and 10% fetal calf serum (Invitrogen) in a CO2 incubator (5% CO2) at 37°C. Up to five different cell lines from different donors were used between passages 5 and 10 for the described experiments. For the irradiation experiments, the cells were seeded into six-well plates and grown to 100% confluency.
Lentiviral shRNA Expression
To knock-down HAS2 in skin fibroblasts, short hairpin RNA (shRNA) sequence29 targeting HAS2 was cloned into the PacI-ClaI site of the pCL1-THPC-vector (forward: 5′-GCGATTATCACTGGATTCTTTCAAGAGAAGAATCC- AGTGATAATCGCTTTTTGGAAA T-3′, reverse: 5′-GCTA- AAGGTTTTTCGCTAATAGTGACCTAAGAAGAGAACTTT- CTTAGGTCACTATTAGCGTA-3′). In this lentiviral vector, the human H1 promoter drives the expression of shRNA, whereas the expression of EGFP, which works as a positive marker for infection, is driven by the SFFV U3 region.30 The vector, harvest of recombinant lentiviral particles, and infection of skin fibroblasts were performed as previously described.30 HA concentration in the supernatant of human skin fibroblasts was determined by using HA enzyme-linked immunosorbent assay (Corgenix) 5 days after infection and was calculated as ratio of HA and total cellular protein.
DNA Synthesis and Migration
DNA synthesis and migration were determined in the presence of FCS because pericellular HA coat formation requires inter-α-inhibitor from serum.31 Five days after lentiviral infection and before the functional assays, the knockdown of HAS2 mRNA expression was verified by real-time RT-PCR. Subsequently, at day 6 after lentiviral infection, shHAS2- and pCL1-infected human skin fibroblasts were compared with respect to proliferation and migration. DNA synthesis was determined in response to 10% serum in serum-starved (24 hours) cells by measurement of [3H]thymidine incorporation as described before.32
Modified Boyden chamber microchemotaxis assays were used to assess migration of shHAS2-transfected cells. Polycarbonate filters (pore size, 10 μmol/L; Neuroprobe, Cabin John, MD) were coated with monomeric type-I collagen (Nutacon BV, Leimuiden, The Netherlands) according to the manufacturer’s instructions. Fibroblasts were trypsinized and seeded at 15,000 cells per well (250,000/cm2) into the upper wells and allowed to migrate toward 10% FCS for 6 hours at 37°C and 5% CO2. Migrated cells were fixed in methanol for 5 minutes and then stained with 5 μg/ml propidium iodide in PBS and analyzed by PhosphorImager scanning as described earlier.33 Each experiment represents the average of at least six microchemotaxis chamber wells.
UV Irradiation of Fibroblasts
For irradiation, the cell culture media were replaced by PBS. Cells were irradiated with 100 J/m2 UVB from FS20 sunlamps (Westinghouse Electric, Pittsburgh, PA). The UVB output was monitored by means of an IL1700 research radiometer and SEE240 UVB photodetector (International Light, Newburyport, MA) and was ∼2.4 W/m2 at a tube to target distance of 22 cm. Immediately after UVB exposure, PBS was replaced by fresh medium, and cells were further incubated until harvest.
Results
UVB Reduces Dermal HA
Staining with HAbP as a specific probe to detect HA revealed that the strongest staining of HA was found in papillary dermis (Figure 1B, arrows). The epidermis of adult mice showed weak HA staining as described earlier.12 As a specific negative control for the HA staining, hyaluronidase digestion was performed (not shown).
To analyze the HA content of the dermal ECM during intrinsic aging, three consecutive skin biopsies from dorsal skin were collected from shaved C57/BL6 mice at the age of 150, 300, and 400 days. HA staining revealed that during intrinsic aging HA levels showed only a slight decline up to 400 days of age (Figure 1B). This was confirmed by densitometric quantification of the HA staining (Figure 1C). Next, dermal HA staining was investigated in age-matched UVB-irradiated mice. Irradiation [three times per week, threefold MED (210 mJ/cm2)] was initiated at the age of 42 days and continued for 182 days. From these mice three consecutive skin biopsies were collected at the same age as described above for the control mice. A pronounced loss of HA especially from the HA-rich papillary dermis (arrows) was observed beginning at 300 days after initiation of UVB irradiation and continued to progress in the 400-day samples (Figure 1B, bottom). Quantitative image analysis of HA affinity histochemistry in the papillary dermis supported this impression. At 400 days (third biopsy), the HA content of the papillary dermis was significantly decreased compared with nonirradiated controls (Figure 1C). Furthermore, the amount of total dermal HA per mg dry weight was significantly reduced (Figure 1D). These results suggest that chronic repetitive UVB irradiation throughout 182 days causes pronounced loss of HA from the upper dermis and that the loss of HA progresses even after cessation of the UVB irradiation.
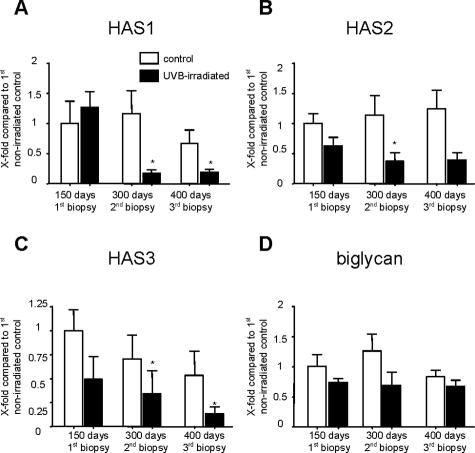
UVB Induces Down-Regulation of HAS Enzymes
To investigate whether the loss of HA from the dermis is because of decreased synthesis, the expression levels of HAS isoenzymes HAS1, HAS2, and HAS3 were determined in the dorsal skin of nonirradiated controls and UVB-irradiated mice. Real-time PCR analysis of HAS1, HAS2, and HAS3 revealed that HAS1 is expressed at the lowest level (∼30 times less than HAS2 and HAS3) and that HAS2 and HAS3 show approximately the same expression (data not shown). The expression level of HAS isoforms in adult nonirradiated control mice at the age of 150 days was set as reference (100%) for subsequent comparisons. In control mice, the expression of HAS1 was not altered up to 400 days of age. In contrast in UVB-irradiated skin, down-regulation of HAS1 occurred at 300 and 400 days compared with nonirradiated controls at 150 days (Figure 2A). HAS2 mRNA expression did not change during intrinsic aging but showed a progressive, time-dependent down-regulation after UVB irradiation (Figure 2B). HAS3 mRNA expression followed a nonsignificant trend toward decreased expression during intrinsic aging but was also significantly and time dependently down-regulated by UVB irradiation at 300 and 400 days (Figure 2C). Taken together, these results indicate that HAS isoform expression was not altered during intrinsic aging up to 400 days. However, in response to chronic UVB irradiation, a progressive down-regulation of all three HAS isoforms occurs.
Figure 2.
mRNA levels of HAS isoenzymes and BGN during intrinsic and UVB-induced aging. Shaved C57/BL6 mice were either sham-irradiated (control) or UVB-irradiated (three times per week, 3 MED ∼210 mJ/cm2), and consecutive skin biopsies were collected (see Materials and Methods). mRNA levels were estimated by real-time PCR and normalized to the expression in nonirradiated control mice at 150 days. HAS1 (A), HAS2 (B), HAS3 (C), and BGN (D) mRNA expression in nonirradiated and UVB-irradiated animals at the indicated times. Open bars represent nonirradiated controls, and black bars represent UVB-irradiated mice. Data are means ± SEM; controls, n = 8; UVB first biopsy, n = 8; UVB second biopsy, n = 7; UVB third biopsy, n = 6. P values were obtained by analysis of variance and Bonferroni’s post test to compare selected pairs; mean ± SEM; *P values <0.05.
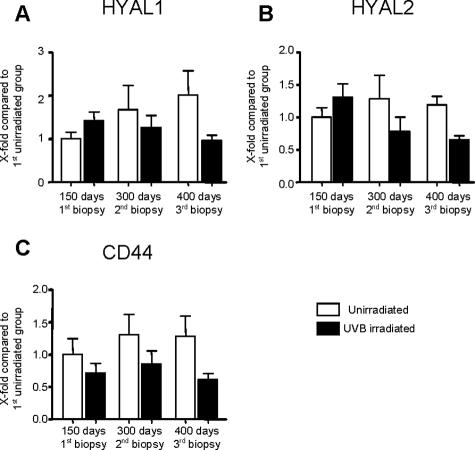
For comparison with other ECM components of the dermal matrix, the expression of BGN was analyzed in the same samples as described above. BGN, a dermatan sulfate proteoglycan, was not affected during aging and UVB irradiation up to 400 days (Figure 2D). In addition, immunohistochemistry of BGN confirmed the presence of BGN but revealed no changes under the present experimental conditions (data not shown). These results suggest that the prominent loss of HA is a specific response and does not represent a general loss of proteoglycan/HA-rich ECM. Because HA is rapidly turned over, UVB-induced degradation of HA by HYALs would also result in loss of HA from the dermis. However the mRNA expression of HYAL1 and HYAL2 were not affected by UVB irradiation (Figure 3, A and B) and neither was the expression of the HA receptor CD44 (Figure 3C). Therefore transcriptional down-regulation of HAS isoenzymes is likely to be responsible for the reduced HA content in the dermis after UVB irradiation.
Figure 3.
mRNA levels of HYAL-1, HYAL-2, and CD44 during intrinsic and UVB-induced aging. Shaved C57/BL6 mice were either sham-irradiated (control) or UVB-irradiated (three times per week, 3 MED ∼210 mJ/cm2), and consecutive skin biopsies were collected (see Materials and Methods). mRNA levels were estimated by real-time PCR and normalized to the expression of nonirradiated control mice at 150 days. Hyal1 (A), Hyal-2 (B), and CD44 (C) mRNA expression in nonirradiated and UVB-irradiated animals at the indicated times. Open bars represent nonirradiated controls, and black bars represent UVB-irradiated mice. Data are means ± SEM, controls, n = 5, and UVB, n = 6. P values were obtained by analysis of variance and Bonferroni’s post test to compare selected pairs; mean ± SEM; P values >0.05.
Regulation of HAS Expression in Skin Fibroblasts in Vitro
Because the mRNA of the skin biopsies was isolated from skin homogenates, it can be assumed that skin fibroblasts are the predominant source of mRNA and also of HA in the dermal connective tissue. Therefore, cultured human skin fibroblasts were used to study the underlying mechanisms of HAS mRNA expression. To investigate whether UVB causes down-regulation of HAS isoenzymes directly, skin fibroblasts were subjected to a single irradiation with UVB (100 J/m2), and mRNA expression was analyzed by real-time RT-PCR up to 72 hours after irradiation. HAS1 and HAS3 are transiently induced by acute UVB irradiation (not shown), which suggests that in vivo the down-regulation of these enzymes is not a direct UVB effect. HAS2 mRNA was significantly reduced 72 hours after UVB (not shown), which opens up the possibility that a direct down-regulation of HAS2 by UVB is involved in the in vivo response.
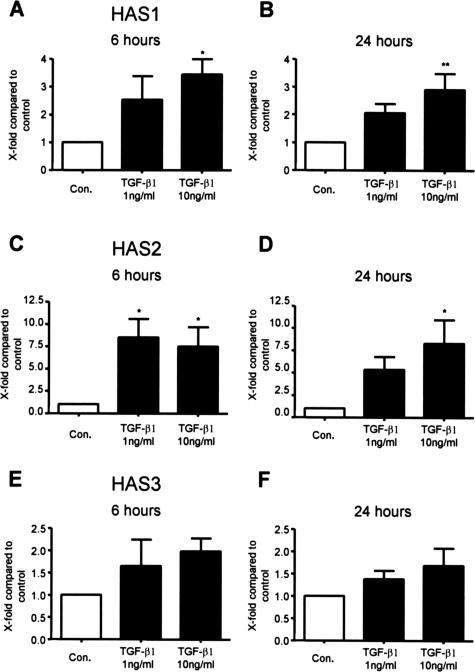
An alternative mechanism to explain loss of HA and down-regulation of HAS isoenzymes after UVB irradiation is inhibition of stimulatory mechanisms that support high expression levels of HAS1, -2, and -3 in the nonirradiated skin. HAS isoenzymes are regulated differentially and many factors have been described to induce expression of HAS isoforms in fibroblasts. Of particular interest is TGF-β1 because TGF-β1 and TGF-β1 receptor/Smad signaling have been suggested to be sensitive to UVB irradiation.34 Therefore, the effect of TGF-β1 on HAS isoenzyme expression was determined. The experiments were performed in serum-starved (24 hours) human skin fibroblasts in the presence or absence of either 1 or 10 ng/ml TGF-β1. mRNA was subsequently isolated at 3 and 24 hours, and mRNA expression of HAS isoforms was determined. Stimulation of human skin fibroblasts with TGF-β1 for 6 and 24 hours significantly induced HAS1 and HAS2 mRNA expression whereas HAS3 showed only a trend toward induction (Figure 4).
Figure 4.
mRNA levels of HAS isoenzymes in response to TGF-β1 in skin fibroblasts in vitro. Human skin fibroblasts were serum-starved for 24 hours and stimulated with either 1 or 10 ng/ml TGF-β1. mRNA levels of HAS isoforms were determined by real-time PCR at 6 and 24 hours. The data are normalized to the expression levels of serum-starved control fibroblasts. HAS1 (A and B), HAS2 (C and D), and HAS3 (E and F) mRNA at the indicated times after stimulation. Data are means ± SEM of n = 4 independent experiments in skin fibroblasts derived from two different donors. P values were calculated by analysis of variance and Bonferroni’s post test to compare selected pairs; mean ± SEM; *P values <0.05; **P values <0.01.
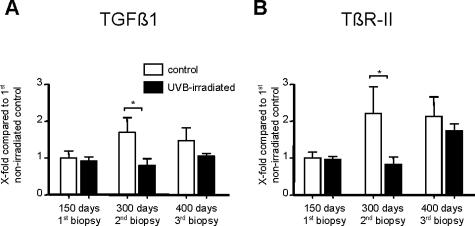
TGF-β1 and TGF-β1 Receptor II (TβR-II) in UVB-Irradiated Mouse Skin
Next, we investigated whether TGF-β1 and TβR-II are UVB sensitive in the present in vivo model of photoaging. For this purpose the mRNA expressions of TGF-β1 and TβR-II were determined using total RNA of the same skin biopsy samples that were analyzed for HA and HAS isoform expression. TGF-β1 was significantly down-regulated in 300-day-old UVB-irradiated mice (Figure 5A). In addition, at 400 days a trend toward reduced TGF-β1 mRNA levels was observed. TβR-II mRNA expression was significantly reduced in UVB-irradiated skin biopsies as well (Figure 5B). Therefore, at the same time when suppression of HAS isoenzyme mRNA first becomes significant (Figure 2), TGF-β1- and TβR-II expression are suppressed by UVB irradiation.
Figure 5.
mRNA levels of TGF-β1 and TβR-II during intrinsic and UVB-induced aging. Shaved C57/BL6 mice were either sham-irradiated or UVB-irradiated (three times per week, 3 MED ∼210 mJ/cm2) and consecutive skin biopsies were collected (see Materials and Methods). mRNA levels were estimated by real-time PCR and normalized to the expression in nonirradiated control mice at 150 days. TGF-β1 (A) and TβR-II (B) mRNA expression in nonirradiated and UVB-irradiated animals at the indicated times. Open bars represent nonirradiated controls, and black bars represent UVB-irradiated mice. Data are means ± SEM; controls, n = 5, and UVB, n = 6. P values were obtained by two-way analysis of variance and Bonferroni’s post test; mean ± SEM; *P values <0.05.
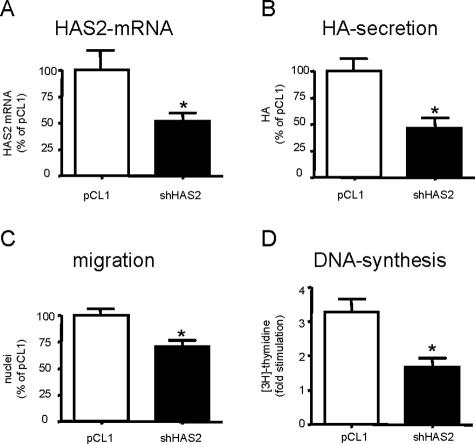
Down-Regulation of HAS2 Inhibits Dermal Fibroblasts
To investigate the functional significance of reduced HAS2 expression for the phenotype of dermal fibroblasts experimental down-regulation of HAS2 by shRNA was used. For this purpose, lentiviral overexpression of shRNA targeting HAS2 was established in human dermal fibroblasts. shHAS2 caused 60% reduction of HAS2 mRNA and ∼70% reduction of HA secretion into the cell culture medium (Figure 6, A and B). The ability of infected fibroblasts to migrate was subsequently analyzed in a modified Boyden-chamber assay on collagen-coated polycarbonate membranes (Figure 6C). shHAS2 caused ∼40% reduction of migration toward FCS. Furthermore, strong reduction of proliferation, as determined by DNA synthesis, was observed in shHAS2-infected cells compared with controls (Figure 6D). Both migration and DNA synthesis were determined in response to serum because serum contains an inter-α-inhibitor that is involved in pericellular HA coat formation.
Figure 6.
Down-regulation of HAS2 by shRNA. Lentiviral transfection with shRNA targeting HAS2 (shHAS2) and empty control vector (pCL1) was performed in human skin fibroblasts. A: Five days after infection, analysis of HAS2 mRNA expression was performed using real-time RT-PCR. B: In parallel, HA secretion was determined by enzyme-linked immunosorbent assay, normalized to total protein and expressed as percentage of pCL1-transfected cells. C: Subsequently, on day 6 after infection, the migration toward 10% FCS was determined using a modified Boyden-chamber microchemotaxis assay on collagen type-1-coated membranes. D: [3H]Thymidine incorporation was determined on day 6 after transfection using 10% FCS as mitogenic stimulus. The data were normalized to total protein and represent the fold increase over starved controls. Data are means ± SEM of n = 4 independent experiments each performed in triplicates. P values were calculated by t-test; *P values <0.05.
Decreased Fibroblast Proliferation in UVB-Irradiated Skin
To examine whether loss of HA also affects the proliferative capacity of skin fibroblasts in vivo, the sections of third biopsy derived from control and UVB-irradiated mice were stained for the proliferation markers PCNA (Figure 7) and Ki67 (not shown). Vimentin/PCNA double immunohistochemistry confirmed that the proliferating cells in the papillary dermis were mainly fibroblasts (Figure 7, A and B). The proliferation index was determined by counting PCNA-positive nuclei in the papillary dermis (Figure 7, C and D). Proliferating epithelial cells and cells associated with hair follicles were excluded. This analysis revealed that in UVB-irradiated third biopsies, the proliferation index as determined by nuclear PCNA staining was reduced to 45 ± 18% of nonirradiated controls (Figure 7E). The same result was achieved with Ki67 (not shown). Furthermore, in the third biopsy of UVB-irradiated mice, total cell number in the papillary dermis was significantly reduced (Figure 7F). Taken together these data support the conclusion that UVB-mediated loss of HA from the papillary dermis is accompanied by reduction of fibroblast proliferation in murine skin.
Figure 7.
Decreased proliferation of dermal skin fibroblasts after UVB irradiation. A and B: Double immunostaining of PCNA (red) and vimentin (green) of third biopsy samples; control (A) and UVB irradiation (B); arrowheads mark proliferating fibroblasts in A. Nuclei are stained by Hoechst 33324 in blue. C and D: Immunostaining of PCNA (red) and nuclear staining with Hoechst 33324 of third biopsy samples. To facilitate determination of the proliferative index, blue nuclear staining was turned into green to indicate PCNA-positive nuclei in the overlay in yellow; control (C) and UVB-irradiated (D); arrowheads mark proliferating cells. E: Proliferative index expressed as percent PCNA-positive nuclei. F: Total cell number in the papillary dermis determined as nuclei per μm2. Data are means ± SEM; control, n = 9, UVB, n = 10. P values were calculated by t-test; *P value <0.05. Original magnifications: ×400 (A and B); ×200 (C and D).
Discussion
HA is thought to play important functional roles in healthy skin by controlling the phenotype of epithelial cells. In addition, the HA content governs general functions of the skin such as water content, turgidity, elasticity, and diffusion of nutrients. Detailed information is available on the regulatory pathways of epidermal HA synthesis,15,35 the function of epidermal HA,36,37 and the expression of epidermal HA synthases and HA receptors.12,35 In addition, it has been shown recently that UVA and UVB irradiation decrease epidermal HA and CD44 in mice.38 In contrast only a few biochemical and histological studies addressed the effect of UV irradiation on HA content of murine and human dermis. Some studies reported increased HA content in UV-irradiated skin of mice,39,40 whereas others reported reduced HA content.16,41 The contradictory results of these studies might be attributable to the fact that different irradiation protocols were used that varied in dose and duration of the UV exposure and the time of analysis. It is likely that the acute effect of UV irradiation on dermal HA is different from the long-term effects of chronic UV irradiation. This view was recently supported by a study that specifically addressed the effects of acute UVB irradiation on HA synthesis and metabolism in keratinocytes, in human fibroblasts and in human skin.42 These studies demonstrated that keratinocytes and fibroblasts show a differential regulation of HAS isoform expression, hyaluronidase expression, and HA synthesis with respect to cell type and time after UVB irradiation (3 versus 24 hours). At 24 hours, this complex regulation resulted in increased HA content in the epidermis and decreased HA content in the dermis. The authors suggested that the observed regulations of HA metabolism are involved in the acute inflammatory response to UVB irradiation.
In contrast to the study by Averbeck and colleagues,42 the present experiments addressed specifically the long-term response of murine skin to chronic repetitive irradiation. We purposely used a model of severe UVB irradiation20 because as mentioned above uncertainty about the effects of UVB on dermal HA still exist. The present model uses UVB doses that induce skin aging and in 25% of animals squamous cell carcinoma,20 an issue that has not been addressed in this study. This model seems relevant because the simultaneous occurrence of both severe skin aging and carcinogenesis in response to UV irradiation are common in patients. We show that HA is lost from the dermis of UVB-irradiated mice at the age of 300 and 400 days. This decrease in dermal HA correlated with the down-regulation of all HAS isoforms at 300 and 400 days. Because the turnover of dermal HA is thought to be fast,43,44 decreased synthesis because of transcriptional down-regulation of HAS isoforms is sufficient to explain the long-term loss of HA in response to UVB in the present study. This conclusion is supported by the finding that HYAL1 and HYAL2 are not significantly changed by UVB.
In addition to HA and HAS isoforms, we investigated the content of the dermatan sulfate proteoglycan BGN, which belongs to the family of small leucine-rich proteoglycans. By immunohistochemistry and real-time RT-PCR, BGN was detected in mouse dermis as has been shown before.45 However, the expression of BGN was affected neither during intrinsic aging nor by UVB. These data suggest that UVB-induced loss of HA and down-regulation of HAS are specific responses and not part of a general down-regulation of polysaccharides and proteoglycans.
It should be emphasized that down-regulation of HAS isoenzymes was a slow response that already started during the irradiation protocol and progressed after the end of the UVB irradiation. This is in line with another study in mice showing progressive loss of HA even after cessation of UVB irradiation.16 The progressive long-term down-regulation of all HAS isoenzymes after the end of the UVB irradiation protocol suggests that UVB does not inhibit HAS expression directly. This conclusion was supported by the present in vitro result that acute UVB irradiation induces rather than inhibits HAS1 and HAS3 expression. Only HAS2 was down-regulated by UVB in vitro. Therefore, we hypothesize that the observed down-regulation of all three HAS isoforms is mainly because of indirect UVB-mediated effects such as altered growth factor and cytokine expression, release, or signaling.
UVB irradiation of skin leads to inhibition of collagen synthesis and increased collagen fragmentation in the dermis. TGF-β1 through the TβR-II is an important stimulator of dermal type I procollagen expression and accumulation.46,47,48 In irradiated fibroblasts and biopsies of sun-exposed skin, TGF-β1/Smad signaling and TβR-II expression are inhibited34,49; which subsequently causes decreased collagen expression and loss of collagen from irradiated skin. In addition, TGF-β1 is also a strong inducer of HA synthesis in human fibroblasts.50 However, the precise effect on HAS isoforms has not yet been determined in human dermal fibroblasts. The present results revealed that TGF-β1 induces expression of HAS1, HAS2, and to a lesser extent HAS3. In vivo, we detected down-regulation of both TGF-β1 and TβR-II mRNA in UVB-irradiated mice at the age of 300 days. Therefore, we hypothesize that UVB-induced loss of TGF-β1 signaling and TβR-II expression is involved in the initial phase of UVB-induced decrease of HAS isoform expression in murine skin.
It has been shown before that HA is involved in proliferation of skin fibroblasts.7 However, nothing is known about the role of HAS isoform-specific HA synthesis during aging and in phenotypic control of skin fibroblasts. The present study provides the first direct evidence, by using the shRNA methodology, that endogenous HA synthesized in physiological concentrations by HAS2 is indeed required for migration and proliferation of skin fibroblasts. This might be of in vivo relevance because the loss of HA in photoaged mouse skin was associated with reduced cell number and proliferative activity. In addition analysis of skin biopsies from chronically sun-exposed versus sun-protected areas of human skin revealed loss of HA as well.51,52,53
In summary, the current data demonstrate that chronic, repetitive UVB irradiation induces loss of HA from murine dermis because of transcriptional down-regulation of HAS1, HAS2, and HAS3. The underlying mechanism might involve decreased transcriptional activation of HAS expression through TGF-β1-dependent pathways. Furthermore, decreased expression of HAS2 is inhibitory for fibroblast migration and proliferation, which might partially explain the thinning and reduced regenerative capacity of photoaged skin.
Footnotes
Address reprint requests to Jens W. Fischer, Molecular Pharmacology, Institut für Pharmakologie and Klinische Pharmakologie, Heinrich-Heine-Universität Düsseldorf, Moorenstrasse 5, D-40225 Düsseldorf. E-mail: jens.fischer@uni-duesseldorf.de.
Supported by Deutsche Forschungsgemeinschaft, SFB 728, TP C6, C1.
References
- Cooper KD, Oberhelman L, Hamilton TA, Baadsgaard O, Terhune M, LeVee G, Anderson T, Koren H. UV exposure reduces immunization rates and promotes tolerance to epicutaneous antigens in humans: relationship to dose, CD1a−DR+ epidermal macrophage induction, and Langerhans cell depletion. Proc Natl Acad Sci USA. 1992;89:8497–8501. doi: 10.1073/pnas.89.18.8497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher GJ, Wang ZQ, Datta SC, Varani J, Kang S, Voorhees JJ. Pathophysiology of premature skin aging induced by ultraviolet light. N Engl J Med. 1997;337:1419–1428. doi: 10.1056/NEJM199711133372003. [DOI] [PubMed] [Google Scholar]
- Fisher GJ, Datta SC, Talwar HS, Wang ZQ, Varani J, Kang S, Voorhees JJ. Molecular basis of sun-induced premature skin ageing and retinoid antagonism. Nature. 1996;379:335–339. doi: 10.1038/379335a0. [DOI] [PubMed] [Google Scholar]
- Itano N, Kimata K. Molecular cloning of human hyaluronan synthase. Biochem Biophys Res Commun. 1996;222:816–820. doi: 10.1006/bbrc.1996.0827. [DOI] [PubMed] [Google Scholar]
- Itano N, Sawai T, Yoshida M, Lenas P, Yamada Y, Imagawa M, Shinomura T, Hamaguchi M, Yoshida Y, Ohnuki Y, Miyauchi S, Spicer AP, McDonald JA, Kimata K. Three isoforms of mammalian hyaluronan synthases have distinct enzymatic properties. J Biol Chem. 1999;274:25085–25092. doi: 10.1074/jbc.274.35.25085. [DOI] [PubMed] [Google Scholar]
- Toole BP, Wight TN, Tammi MI. Hyaluronan-cell interactions in cancer and vascular disease. J Biol Chem. 2002;277:4593–4596. doi: 10.1074/jbc.R100039200. [DOI] [PubMed] [Google Scholar]
- Yoneda M, Yamagata M, Suzuki S, Kimata K. Hyaluronic acid modulates proliferation of mouse dermal fibroblasts in culture. J Cell Sci. 1988;90:265–273. doi: 10.1242/jcs.90.2.265. [DOI] [PubMed] [Google Scholar]
- Stern R. Hyaluronan catabolism: a new metabolic pathway. Eur J Cell Biol. 2004;83:317–325. doi: 10.1078/0171-9335-00392. [DOI] [PubMed] [Google Scholar]
- Termeer C, Benedix F, Sleeman J, Fieber C, Voith U, Ahrens T, Miyake K, Freudenberg M, Galanos C, Simon JC. Oligosaccharides of hyaluronan activate dendritic cells via toll-like receptor 4. J Exp Med. 2002;195:99–111. doi: 10.1084/jem.20001858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang D, Liang J, Fan J, Yu S, Chen S, Luo Y, Prestwich GD, Mascarenhas MM, Garg HG, Quinn DA, Homer RJ, Goldstein DR, Bucala R, Lee PJ, Medzhitov R, Noble PW. Regulation of lung injury and repair by Toll-like receptors and hyaluronan. Nat Med. 2005;11:1173–1179. doi: 10.1038/nm1315. [DOI] [PubMed] [Google Scholar]
- Manuskiatti W, Maibach HI. Hyaluronic acid and skin: wound healing and aging. Int J Dermatol. 1996;35:539–544. doi: 10.1111/j.1365-4362.1996.tb03650.x. [DOI] [PubMed] [Google Scholar]
- Tammi R, Pasonen-Seppanen S, Kolehmainen E, Tammi M. Hyaluronan synthase induction and hyaluronan accumulation in mouse epidermis following skin injury. J Invest Dermatol. 2005;124:898–905. doi: 10.1111/j.0022-202X.2005.23697.x. [DOI] [PubMed] [Google Scholar]
- Kanda N, Watanabe S. Regulatory roles of sex hormones in cutaneous biology and immunology. J Dermatol Sci. 2005;38:1–7. doi: 10.1016/j.jdermsci.2004.10.011. [DOI] [PubMed] [Google Scholar]
- Sator PG, Schmidt JB, Rabe T, Zouboulis CC. Skin aging and sex hormones in women—clinical perspectives for intervention by hormone replacement therapy. Exp Dermatol. 2004;13(Suppl 4):36–40. doi: 10.1111/j.1600-0625.2004.00259.x. [DOI] [PubMed] [Google Scholar]
- Saavalainen K, Pasonen-Seppanen S, Dunlop TW, Tammi R, Tammi MI, Carlberg C. The human hyaluronan synthase 2 gene is a primary retinoic acid and epidermal growth factor responding gene. J Biol Chem. 2005;280:14636–14644. doi: 10.1074/jbc.M500206200. [DOI] [PubMed] [Google Scholar]
- Margelin D, Medaisko C, Lombard D, Picard J, Fourtanier A. Hyaluronic acid and dermatan sulfate are selectively stimulated by retinoic acid in irradiated and nonirradiated hairless mouse skin. J Invest Dermatol. 1996;106:505–509. doi: 10.1111/1523-1747.ep12343819. [DOI] [PubMed] [Google Scholar]
- Bruls WA, van Weelden H, van der Leun JC. Transmission of UV-radiation through human epidermal layers as a factor influencing the minimal erythema dose. Photochem Photobiol. 1984;39:63–67. doi: 10.1111/j.1751-1097.1984.tb03405.x. [DOI] [PubMed] [Google Scholar]
- Averbeck M, Beilharz S, Bauer M, Gebhardt C, Hartmann A, Hochleitner K, Kauer F, Voith U, Simon JC, Termeer C. In situ profiling and quantification of cytokines released during ultraviolet B-induced inflammation by combining dermal microdialysis and protein microarrays. Exp Dermatol. 2006;15:447–454. doi: 10.1111/j.0906-6705.2006.00429.x. [DOI] [PubMed] [Google Scholar]
- Matsumura Y, Ananthaswamy HN. Short-term and long-term cellular and molecular events following UV irradiation of skin: implications for molecular medicine. Expert Rev Mol Med. 2002;2002:1–22. doi: 10.1017/S146239940200532X. [DOI] [PubMed] [Google Scholar]
- Aszterbaum M, Epstein J, Oro A, Douglas V, LeBoit PE, Scott MP, Epstein EH., Jr Ultraviolet and ionizing radiation enhance the growth of BCCs and trichoblastomas in patched heterozygous knockout mice. Nat Med. 1999;5:1285–1291. doi: 10.1038/15242. [DOI] [PubMed] [Google Scholar]
- Ripellino JA, Klinger MM, Margolis RU, Margolis RK. The hyaluronic acid binding region as a specific probe for the localization of hyaluronic acid in tissue sections. J Histochem Cytochem. 1985;33:1060–1066. doi: 10.1177/33.10.4045184. [DOI] [PubMed] [Google Scholar]
- Calabro A, Hascall VC, Midura RJ. Adaptation of FACE methodology for microanalysis of total hyaluronan and chondroitin sulfate composition from cartilage. Glycobiology. 2000;10:283–293. doi: 10.1093/glycob/10.3.283. [DOI] [PubMed] [Google Scholar]
- Papakonstantinou E, Roth M, Block LH, Mirtsou-Fidani V, Argiriadis P, Karakiulakis G. The differential distribution of hyaluronic acid in the layers of human atheromatic aortas is associated with vascular smooth muscle cell proliferation and migration. Atherosclerosis. 1998;138:79–89. doi: 10.1016/s0021-9150(98)00006-9. [DOI] [PubMed] [Google Scholar]
- McCallum FS, Maden BE. Human 18 S ribosomal RNA sequence inferred from DNA sequence. Variations in 18 S sequences and secondary modification patterns between vertebrates. Biochem J. 1985;232:725–733. doi: 10.1042/bj2320725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shyjan AM, Heldin P, Butcher EC, Yoshino T, Briskin MJ. Functional cloning of the cDNA for a human hyaluronan synthase. J Biol Chem. 1996;271:23395–23399. doi: 10.1074/jbc.271.38.23395. [DOI] [PubMed] [Google Scholar]
- Watanabe K, Yamaguchi Y. Molecular identification of a putative human hyaluronan synthase. J Biol Chem. 1996;271:22945–22948. doi: 10.1074/jbc.271.38.22945. [DOI] [PubMed] [Google Scholar]
- Liu N, Gao F, Han Z, Xu X, Underhill CB, Zhang L. Hyaluronan synthase 3 overexpression promotes the growth of TSU prostate cancer cells. Cancer Res. 2001;61:5207–5214. [PubMed] [Google Scholar]
- Whitham SE, Murphy G, Angel P, Rahmsdorf HJ, Smith BJ, Lyons A, Harris TJ, Reynolds JJ, Herrlich P, Docherty AJ. Comparison of human stromelysin and collagenase by cloning and sequence analysis. Biochem J. 1986;240:913–916. doi: 10.1042/bj2400913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiznerowicz M, Trono D. Conditional suppression of cellular genes: lentivirus vector-mediated drug-inducible RNA interference. J Virol. 2003;77:8957–8961. doi: 10.1128/JVI.77.16.8957-8961.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmes M, Neumeyer A, Rio P, Hanenberg H, Fritsche E, Blomeke B. Impact of the arylhydrocarbon receptor on eugenol- and isoeugenol-induced cell cycle arrest in human immortalized keratinocytes (HaCaT). Biol Chem. 2006;387:1201–1207. doi: 10.1515/BC.2006.148. [DOI] [PubMed] [Google Scholar]
- Carrette O, Nemade RV, Day AJ, Brickner A, Larsen WJ. TSG-6 is concentrated in the extracellular matrix of mouse cumulus oocyte complexes through hyaluronan and inter-alpha-inhibitor binding. Biol Reprod. 2001;65:301–308. doi: 10.1095/biolreprod65.1.301. [DOI] [PubMed] [Google Scholar]
- van den Boom M, Sarbia M, von Wnuck Lipinski K, Mann P, Meyer-Kirchrath J, Rauch BH, Grabitz K, Levkau B, Schror K, Fischer JW. Differential regulation of hyaluronic acid synthase isoforms in human saphenous vein smooth muscle cells: possible implications for vein graft stenosis. Circ Res. 2006;98:36–44. doi: 10.1161/01.RES.0000199263.67107.c0. [DOI] [PubMed] [Google Scholar]
- Conley BA, Koleva R, Smith JD, Kacer D, Zhang D, Bernabeu C, Vary CP. Endoglin controls cell migration and composition of focal adhesions: function of the cytosolic domain. J Biol Chem. 2004;279:27440–27449. doi: 10.1074/jbc.M312561200. [DOI] [PubMed] [Google Scholar]
- Quan T, He T, Kang S, Voorhees JJ, Fisher GJ. Solar ultraviolet irradiation reduces collagen in photoaged human skin by blocking transforming growth factor-β type II receptor/Smad signaling. Am J Pathol. 2004;165:741–751. doi: 10.1016/s0002-9440(10)63337-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pienimaki JP, Rilla K, Fulop C, Sironen RK, Karvinen S, Pasonen S, Lammi MJ, Tammi R, Hascall VC, Tammi MI. Epidermal growth factor activates hyaluronan synthase 2 in epidermal keratinocytes and increases pericellular and intracellular hyaluronan. J Biol Chem. 2001;276:20428–20435. doi: 10.1074/jbc.M007601200. [DOI] [PubMed] [Google Scholar]
- Rilla K, Lammi MJ, Sironen R, Torronen K, Luukkonen M, Hascall VC, Midura RJ, Hyttinen M, Pelkonen J, Tammi M, Tammi R. Changed lamellipodial extension, adhesion plaques and migration in epidermal keratinocytes containing constitutively expressed sense and antisense hyaluronan synthase 2 (Has2) genes. J Cell Sci. 2002;115:3633–3643. doi: 10.1242/jcs.00042. [DOI] [PubMed] [Google Scholar]
- Tammi R, Tammi M. Correlations between hyaluronan and epidermal proliferation as studied by [3H]glucosamine and [3H]thymidine incorporations and staining of hyaluronan on mitotic keratinocytes. Exp Cell Res. 1991;195:524–527. doi: 10.1016/0014-4827(91)90405-j. [DOI] [PubMed] [Google Scholar]
- Calikoglu E, Sorg O, Tran C, Grand D, Carraux P, Saurat JH, Kaya G. UVA and UVB decrease the expression of CD44 and hyaluronate in mouse epidermis which is counteracted by topical retinoids. Photochem Photobiol. 2006;82:1342–1347. doi: 10.1562/2006-02-10-RA-801. [DOI] [PubMed] [Google Scholar]
- Koshiishi I, Horikoshi E, Mitani H, Imanari T. Quantitative alterations of hyaluronan and dermatan sulfate in the hairless mouse dorsal skin exposed to chronic UV irradiation. Biochim Biophys Acta. 1999;1428:327–333. doi: 10.1016/s0304-4165(99)00081-1. [DOI] [PubMed] [Google Scholar]
- Schwartz E. Connective tissue alterations in the skin of ultraviolet irradiated hairless mice. J Invest Dermatol. 1988;91:158–161. doi: 10.1111/1523-1747.ep12464405. [DOI] [PubMed] [Google Scholar]
- Takahashi Y, Ishikawa O, Okada K, Ohnishi K, Miyachi Y. Disaccharide analysis of the skin glycosaminoglycans in chronically ultraviolet light-irradiated hairless mice. J Dermatol Sci. 1995;10:139–144. doi: 10.1016/0923-1811(95)00396-a. [DOI] [PubMed] [Google Scholar]
- Averbeck M, Gebhardt CA, Voigt S, Beilharz S, Anderegg U, Termeer CC, Sleeman JP, Simon JC. Differential regulation of hyaluronan metabolism in the epidermal and dermal compartments of human skin by UVB irradiation. J Invest Dermatol. 2007;127:687–697. doi: 10.1038/sj.jid.5700614. [DOI] [PubMed] [Google Scholar]
- Tammi R, Agren UM, Tuhkanen AL, Tammi M. Hyaluronan metabolism in skin. Prog Histochem Cytochem. 1994;29:1–81. doi: 10.1016/s0079-6336(11)80023-9. [DOI] [PubMed] [Google Scholar]
- Stern R. Devising a pathway for hyaluronan catabolism: are we there yet? Glycobiology. 2003;13:105R–115R. doi: 10.1093/glycob/cwg112. [DOI] [PubMed] [Google Scholar]
- Wegrowski Y, Pillarisetti J, Danielson KG, Suzuki S, Iozzo RV. The murine biglycan: complete cDNA cloning, genomic organization, promoter function, and expression. Genomics. 1995;30:8–17. doi: 10.1006/geno.1995.0002. [DOI] [PubMed] [Google Scholar]
- Ghosh AK, Yuan W, Mori Y, Varga J. Smad-dependent stimulation of type I collagen gene expression in human skin fibroblasts by TGF-β involves functional cooperation with p300/CBP transcriptional coactivators. Oncogene. 2000;19:3546–3555. doi: 10.1038/sj.onc.1203693. [DOI] [PubMed] [Google Scholar]
- Chen SJ, Yuan W, Mori Y, Levenson A, Trojanowska M, Varga J. Stimulation of type I collagen transcription in human skin fibroblasts by TGF-β: involvement of Smad 3. J Invest Dermatol. 1999;112:49–57. doi: 10.1046/j.1523-1747.1999.00477.x. [DOI] [PubMed] [Google Scholar]
- Chen SJ, Yuan W, Lo S, Trojanowska M, Varga J. Interaction of smad3 with a proximal smad-binding element of the human α2(I) procollagen gene promoter required for transcriptional activation by TGF-β. J Cell Physiol. 2000;183:381–392. doi: 10.1002/(SICI)1097-4652(200006)183:3<381::AID-JCP11>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Han KH, Choi HR, Won CH, Chung JH, Cho KH, Eun HC, Kim KH. Alteration of the TGF-β/SMAD pathway in intrinsically and UV-induced skin aging. Mech Ageing Dev. 2005;126:560–567. doi: 10.1016/j.mad.2004.11.006. [DOI] [PubMed] [Google Scholar]
- Heldin P, Laurent TC, Heldin CH. Effect of growth factors on hyaluronan synthesis in cultured human fibroblasts. Biochem J. 1989;258:919–922. doi: 10.1042/bj2580919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghersetich I, Lotti T, Campanile G, Grappone C, Dini G. Hyaluronic acid in cutaneous intrinsic aging. Int J Dermatol. 1994;33:119–122. doi: 10.1111/j.1365-4362.1994.tb01540.x. [DOI] [PubMed] [Google Scholar]
- Takahashi Y, Ishikawa O, Okada K, Kojima Y, Igarashi Y, Miyachi Y. Disaccharide analysis of human skin glycosaminoglycans in sun-exposed and sun-protected skin of aged people. J Dermatol Sci. 1996;11:129–133. doi: 10.1016/0923-1811(95)00430-0. [DOI] [PubMed] [Google Scholar]
- Südel KM, Venzke K, Mielke H, Breitenbach U, Mundt C, Jaspers S, Koop U, Sauermann K, Knussman-Hartig E, Moll I, Gercken G, Young AR, Stab F, Wenck H, Gallinat S. Novel aspects of intrinsic and extrinsic aging of human skin: beneficial effects of soy extract. Photochem Photobiol. 2005;81:581–587. doi: 10.1562/2004-06-16-RA-202. [DOI] [PubMed] [Google Scholar]