Abstract
Cancer-associated stromal fibroblasts (CAFs) are the main cellular constituents of reactive stroma in primary and metastatic cancer. We analyzed phenotypical characteristics of CAFs from human colorectal liver metastases (CLMs) and their role in inflammation and cancer progression. CAFs displayed a vimentin+, α-smooth-muscle actin+, and Thy-1+ phenotype similar to resident portal-located liver fibroblasts (LFs). We demonstrated that CLMs are inflammatory sites showing stromal expression of interleukin-8 (IL-8), a chemokine related to invasion and angiogenesis. In vitro analyses revealed a striking induction of IL-8 expression in CAFs and LFs by tumor necrosis factor-α (TNF-α). The effect of TNF-α on CAFs is inhibited by the nuclear factor-κB inhibitor parthenolide. Conditioned medium of CAFs and LFs similarly stimulated the migration of DLD-1, Colo-678, HuH7 carcinoma cells, and human umbilical vein endothelial cells in vitro. Pretreatment of CAFs with TNF-α increased the chemotaxis of Colo-678 colon carcinoma cells by conditioned medium of CAFs; however, blockage of IL-8 activity showed no inhibitory effect. In conclusion, these data raise the possibility that the majority of CAFs in CLM originate from resident LFs. TNF-α-induced up-regulation of IL-8 via nuclear factor-κB in CAFs is an inflammatory pathway, potentially permissive for cancer invasion that may represent a novel therapeutic target.
Colorectal cancer is one of the most common causes of cancer death in Western countries. The outcome of the disease is determined by the occurrence of metastatic dissemination, mostly to the liver.1 Surgical resection, the only curative therapy for colorectal liver metastases (CLMs), is possible in less than 25% of the patients at time of diagnosis, and the overall prognosis of nonresected colorectal liver metastases is dismal.2 A detailed understanding of the biological processes that regulate the establishment and progression of CLMs may lead to improvements in nonsurgical antitumor therapy.
Cancer-associated stromal fibroblasts (CAFs) represent the major cellular component of the desmoplastic stroma of solid cancers and their metastases.3,4 In hepatocellular carcinoma and CLMs, most related investigations implicated activated hepatic stellate cells (HSCs) responsible for the formation of cancer stroma and fibrotic capsule because of their ability do undergo spontaneous myofibroblastic transdifferentiation in vitro.5,6,7 HSCs are located around the sinusoidal endothelial cells in the space of Disse and have commonly been regarded as the principal matrix-producing cell type of the liver involved in fibrogenesis.8,9 Recently, other cell types, such as portal fibroblasts, smooth muscle cells, and circulating mesenchymal cells, have been identified and discussed to contribute to fibrogenesis and cirrhosis formation in chronic liver disease.10,11,12,13 The fibroblastic cells present in CLMs, where there exists a large amount of stroma, have not yet been sufficiently characterized according to their phenotype and functions in comparison with resident fibroblast subpopulations.
Inflammation has increasingly been considered as a pivotal environmental factor contributing to tumor progression.14 Invading inflammatory cells and cancer cells are known to produce a variety of mediators such as tumor necrosis factor-α (TNF-α), transforming-growth factor-β1, and platelet-derived growth factor (PDGF), thereby generating a favorable microenvironment for cancer cell invasion and angiogenesis.15,16,17,18 TNF-α is a key mediator of the inflammatory response that acts through activation of nuclear factor-κB (NF-κB), which in turn modulates transcription of genes encoding cytokines, cell adhesion molecules, and anti-apoptotic proteins.19,20,21 Among these factors, the CXC chemokine interleukin-8 (IL-8) has received much interest. IL-8 is a potent chemoattractant for leukocytes in benign inflammatory conditions and wound healing, and many cell types, including fibroblasts from lung, colon, skin, or synovial tissue, elicited increased IL-8 expression after exposure to TNF-α.22,23,24,25,26,27 In malignancy, IL-8 has been shown to promote angiogenesis and tumor cell invasion.28,29 It has been observed that the amount of IL-8 in primary colorectal cancer was positively correlated to the stage and presence of liver metastases.30 Furthermore, there exist several reports showing that IL-8 increases migration of colon carcinoma cells in vitro.31,32 Whether IL-8 plays a functional role in metastasis progression, as well as its cellular source and regulating factors in CLM, has not yet been elucidated.
The aim of this study was first to investigate the phenotype of human CAFs isolated from colorectal liver metastases. We found that CAFs are phenotypically similar to a population of resident portal liver fibroblasts (LFs) distinct from HSCs. This raises the possibility that these LFs significantly contribute to the CAF population in CLM when recruited and embedded in the malignant process. Because of their close relationship to morphologically evident inflammation and IL-8 immunoreactivity in CLM, we hypothesized that CAFs play a significant role in IL-8 expression. Our results point to the existence of an inflammatory, TNF-α/NF-κB-mediated mechanism for stromal IL-8 expression that might be of potential biological significance in CLM.
Materials and Methods
Human Tissue Samples
Samples of CLM, adjacent liver tissue, and distant healthy liver tissue were obtained from 20 patients undergoing liver resection in accordance with the local ethical committee and after written informed consent. For immunohistochemistry, tissue specimens were immediately removed and embedded in Tissue-Tek (Sakura Finetek, Zoeterwoude, The Netherlands), frozen in liquid nitrogen, and stored at −20°C. For RNA isolation, small tissue pieces were stored at −80°C. For isolation and culturing of fibroblastic cells, tissue samples were kept in Medium 199 (Invitrogen, Karlsruhe, Germany). The fibroblastic cells that were generated from tumor tissue were defined as CAFs, and those that were isolated from the respective distant liver tissue were regarded as LFs.
Primary Culture of CAFs and LFs
Minced specimens of liver metastases and corresponding distant liver tissue were incubated in 1 mg/ml collagenase type IV (Sigma, Deisenhofen, Germany) in Medium 199 (Invitrogen) for 30 minutes. Isolated cells were cultured in 145-cm2 Petri dishes (Nunclon; Nunc, Roskilde, Denmark) in 30 ml of Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum (FBS; Invitrogen), 1% penicillin, 1% streptomycin, and 1% amphotericin B (Invitrogen) at 37°C in 5% CO2. For all experiments described below, cells between passages 3 and 10 were used. For sampling of conditioned medium (CM), 1 × 106 CAFs and 1 × 106 LFs were cultured in DMEM + 10% FBS for 48 hours, followed by incubation for 24 hours in DMEM + 0.5% FBS with or without TNF-α.
Cell Lines
DLD-1 and Colo-678 colon carcinoma cells (DSMZ, Braunschweig, Germany) and HuH7 hepatoma cell lines (JCRB Cell Bank, Tokyo, Japan) were grown in cell culture dishes in medium DMEM supplemented with 10% FBS and containing 1% penicillin, 1% streptomycin, and 1% amphotericin B. Human umbilical vein endothelial cells (HUVECs) were purchased from Cascade Biologics (Mansfield, UK) and grown in Medium 200 (M200; Cascade Biologics) supplemented with penicillin/streptomycin/amphotericin B and low-serum growth supplement (LSGS; Cascade Biologics).
Stimulation Experiments
CAFs (1 × 106) and LFs (1 × 106) grown for 48 hours in 145-cm2 Petri dishes were pretreated for 4 hours in DMEM containing 0.5% FBS. Then they were incubated for 24 hours in DMEM + 0.5% FBS with or without (control) human growth factors. The following human growth factors and cytokines were used: platelet-derived growth factor (PDGF-BB; Roche, Basel, Switzerland), TNF-α (Sigma), and transforming growth factor-β1 (Roche). The medium was then collected for protein analysis (enzyme-linked immunosorbent assay), and the cell layer was subjected to RNA isolation.
Inhibition of NF-κB
The herbal sesquiterpene lactone parthenolide (Calbiochem, Bad Soden, Germany), which inhibits activation of NF-κB, was dissolved in tissue culture-grade dimethyl sulfoxide and subjected in increasing concentrations to the above-described stimulation experiments in the presence or absence of TNF-α. Final dimethyl sulfoxide concentration did not exceed 0.1%, a concentration ascertained not to interfere with the experiments.
Immunocytochemistry
For phenotypical characterization of cultured CAFs and LFs, the cells were seeded at 3 × 105 cells/well onto eight-chamber slides (BD Falcon; BD Biosciences, Heidelberg, Germany) and cultured for 48 hours until subconfluent to confluent. The slides were fixed in acetone and stained with the primary antibodies listed in Table 1 (all monoclonal mouse anti-human). After blocking with biotin (DAKO, Hamburg, Germany) and horse serum, slides were incubated with the primary antibody for 60 minutes. The reactivity was detected by using the Vectastain ABC-AP Kit (Vector Laboratories, Grünberg, Germany) according to the manufacturer’s instructions. Slides were counterstained with hematoxylin. Negative controls were prepared by substituting the primary antibody with isotype-matched mouse immunoglobulins.
Table 1.
Marker Profile of CAFs, Portal LFs, perisinusoidal HSCs, and Smooth Muscle Cells (SMCs) from Vessel Walls in Human Tissue Samples and of Cultured CAFs and LFs, and Antibodies Used for Immunocytochemistry
| Human tissue
|
Cultured cells
|
Antibody (dilution; clone; provider) | |||||
|---|---|---|---|---|---|---|---|
| CAFs | LFs | HSCs | SMCs | CAFs | LFs | ||
| Vimentin | + | + | + | + | + | + | 1/50; V9; Dako, Glostrup, Denmark |
| Thy-1 | + | + | − | + | + | + | 1/25; 5E10; BD Biosciences, Bedford, MA |
| α-SMA | + | + | − | + | + | + | 1/50; 1A4; Dako |
| Desmin | − | − | − | + | − | − | 1/50; D33; Dako |
| CD45 | − | − | − | − | − | − | 1/50; T29/33; Dako |
| ICAM-1 | + | ± | ± | ± | ± | ± | 1/50; 6.5B5; Dako |
| NCAM | − | − | − | − | − | − | 1/25; T199; Dako |
| Glial fibrillary acidic protein | − | − | − | − | − | − | 1/25; 6F2; Dako |
| CK-7 | − | − | − | − | ± | ± | 1/50; OV-TL 12/30; Dako |
| CK-19 | − | − | − | − | − | − | 1/100; RCK108; Dako |
| Laminin | + | + | ± | + | + | + | 1/25; 4C7; Dako |
CK, cytokeratin; NCAM, neural cell adhesion molecule.
+, strongly positive; ±, mildly positive; −, not detected.
To characterize CAFs and LFs in situ, 5-μm thin cryosections of liver metastasis specimens were immunostained as described above with the antibodies listed in Table 1. In addition, these cryosections were stained with an antibody against IL-8 (1/50, clone B-K8; Serotec, Düsseldorf, Germany). The percentages of CD45-positive cells in the metastases, the peritumor margins, and the distant liver tissues were quantified by two independent observers by counting the number of stained and unstained cells in four different high-power magnification fields (×400).
Chemotaxis Assay
The migration of HuH7, DLD-1, Colo-678 cells, and HUVECs toward increasing amounts of concentrated CM obtained from cultures of CAFs and LFs was investigated and compared using a modified 96-well Boyden chamber assay as previously described.33 The cells (15 × 103 cells/50 μl) were seeded in the upper chambers. Furthermore, CM of CAFs that were exposed for 24 hours to TNF-α (10 ng/ml) was compared with CM of nonstimulated cells. To exclude an influence of TNF-α on the assay, the respective concentration of TNF-α was added to the CM of nonstimulated cells after the incubation period. In these experiments, the incubating medium in the upper chambers was DMEM + 0.5%. The effect of blockage of IL-8 activity was tested by preincubation of the respective CM with an inhibiting antibody (10 μg/ml; mouse monoclonal anti-human IL-8, clone 6217; R&D Systems, Minneapolis, MN). We furthermore analyzed the effect of increasing concentrations of recombinant human IL-8 (R&D Systems). The chambers were covered with an 8-μm pore size Nucleopore filter (Neuroprobe) that was coated with Vitrogen 100 (Cohesion, Palo Alto, CA). The incubation time was 5 hours. After fixing and staining, the migration was quantified by counting cell nuclei in 10 high-power fields using a ×40 objective and a calibrated ocular grid.33
Enzyme-Linked Immunosorbent Assay
Release of IL-8 by cultivated CAFs and LFs was quantified using commercially available enzyme-linked immunosorbent assays (ELISAs) according to the manufacturer’s instructions (EH2 IL-8; Pierce Endogen, Woburn, MA).
RNA Extraction and Northern Blot Analysis
Total RNA was extracted from cultivated cells or tissue samples by using the RNeasy Midi Kit (Qiagen, Hilden, Germany) according to the manufacturer’s protocols. Five micrograms of total RNA per lane was separated on a 1% denaturing agarose gel. The synthesis of digoxigenin-labeled antisense probes was performed by two subsequent PCR steps using the PCR DIG Probe Synthesis Kit (Roche) as previously described.34 The following sets of primers were used: IL-8 (GenBank accession no. NM_000584), forward-17 5′-CTTTCAGAGACAGCAGAGCAC-3′, reverse-972 5′-ACTGTGAGGTAAGATGGTGGC-3′; and glyceraldehyde-3-phosphate dehydrogenase (NM_002046.2), forward-81 5′-GAAGGTGAAGGTCGGAGTC-3′, reverse-306 5′-GAAGATGGTGATGGGATTTC-3′.
Primers were purchased from MWG-Biotech (Ebersberg, Germany). Hybridization and detection were performed as described earlier.34
Statistical Analysis
Data are presented as mean and SEM. For statistical analysis, at least four experiments using different cell cultures from different patients were performed. Differences between experimental groups were analyzed by one-way analysis of variance (analysis of variance) and Bonferroni multiple comparison tests. A P value <0.05 was considered statistically significant.
Results
CAFs are Phenotypically Similar to Resident Portal LFs
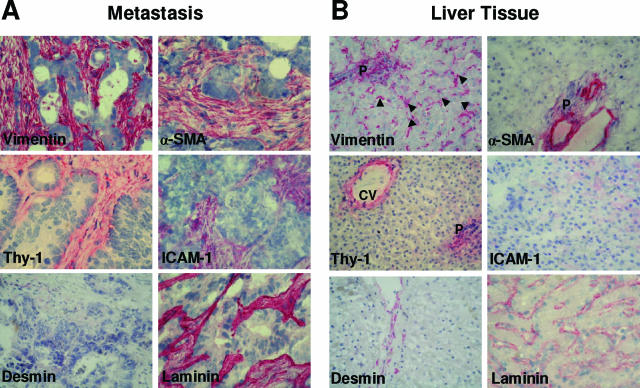
We first classified fibroblastic cell populations according to their immunostaining marker profiles on histological sections of CLM and corresponding distant liver tissues (at least 3 cm apart the metastasis; n = 20). Within the tumor stroma, the majority of cells showed a myofibroblastic shape and differentiation being positive for vimentin and α-smooth muscle actin (α-SMA), as described previously.35 In addition, these CAFs displayed immunoreactivity for Thy-1 (Figure 1A), a surface glycoprotein that may be functionally involved in adhesion, migration, and myofibroblastic differentiation.36,37 Desmin immunoreactivity was detected in the walls of larger vessels but not within the perivascular stroma. Moreover, the stroma of the metastases was positive for intercellular adhesion molecule-1 (ICAM-1) and laminin (Figure 1A and Table 1).
Figure 1.
Phenotype of CAFs and fibroblastic hepatic cell populations in situ. Immunohistochemical analyses of vimentin, α-SMA, Thy-1, ICAM-1, desmin, and laminin. Representative images of cryosections from metastatic tissue (A) and liver tissue (B) of 20 patients. Original magnification, ×400 (P, portal area; CV, central vein). The stromal compartment of the metastatic tissue displays intense immunoreactivity for vimentin, α-SMA, Thy-1, ICAM-1, and laminin. Desmin was detected in the walls of larger vessels. The arrowheads in the vimentin staining of B indicate vimentin-positive hepatic stellate cells or Kupffer cells that are located along the sinusoid linings. In portal and pericentral regions there are vimentin+, α-SMA+, and Thy-1+ cells (LFs), whereas the HSCs residing in perisinusoidal linings showed no immunoreactivity for α-SMA and Thy-1.
In distant liver tissues, we identified two cell types that exhibited immunoreactivity for vimentin, α-SMA, and Thy-1. First, there were smooth muscle cells that assemble vessel walls in the portal fields. In larger vessels, these cells moreover showed immunoreactivity for desmin. Second, there were vimentin+, α-SMA+, and Thy-1+ fibroblastic cells that are arranged as a cellular network in the portal areas and around the central veins (Figure 1B). Along the hepatic sinusoids, there were regularly distributed vimentin+ cells, most probably HSCs or Kupffer cells.10,38 These cells stained negative for Thy-1 and α-SMA (Figure 1B). ICAM-1 was only scarcely expressed along the sinusoid linings (Figure 1B). Thus, the fibroblasts present in colorectal liver metastases exhibit a myofibroblastic phenotype, which is, with respect to marker expression profile, similar to resident fibroblasts residing perivascular connective tissue of portal fields in normal liver tissue (Table 1).
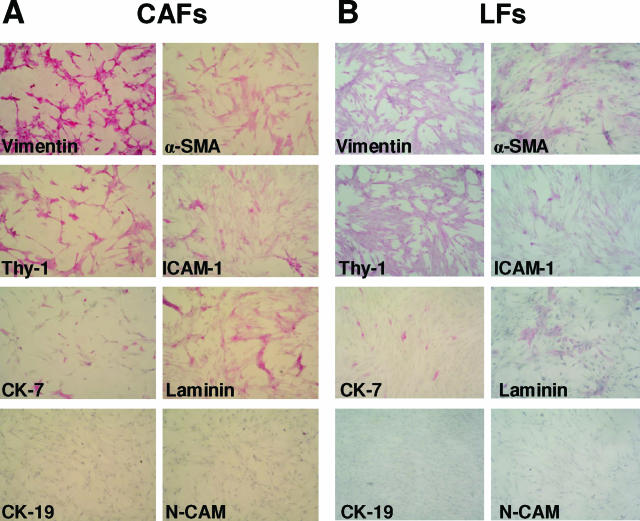
Next, we analyzed the phenotype of collagenase-isolated and subsequently cultured fibroblasts from metastatic tissue (CAFs) and compared these cells with fibroblasts generated from liver tissue (LFs) by immunohistochemistry. Both cell types stained positive for vimentin, Thy-1, α-SMA, ICAM-1, and laminin. Moreover, few cells expressed cytokeratin 7 (Figure 2, A and B). Marker proteins related to HSCs,9,10 like glial fibrillary acidic protein, desmin, or neural cell adhesion molecule, were not detected. In addition, CAFs and LFs were negative for CD45, a panleukocytic marker that is reported to be expressed by bone marrow-derived fibroblasts in experimental liver fibrosis.13 In conclusion, the phenotypical analysis of cultured CAFs and LFs suggest that these cultures are, respectively representative for the CAFs and portal liver fibroblasts described on tissue sections and that both populations of fibroblasts are identical (Table 1).
Figure 2.
Representative images of cultured CAFs (A) and LFs (B) stained for vimentin, α-SMA, Thy-1, ICAM-1, cytokeratin (CK)-7, laminin, CK-19, and neural cell adhesion molecule (NCAM), indicating that the myofibroblastic phenotype of CAFs and LFs was stable in vitro (original magnification, ×400; positive staining, red).
Liver Metastases Represent a Site of Inflammation
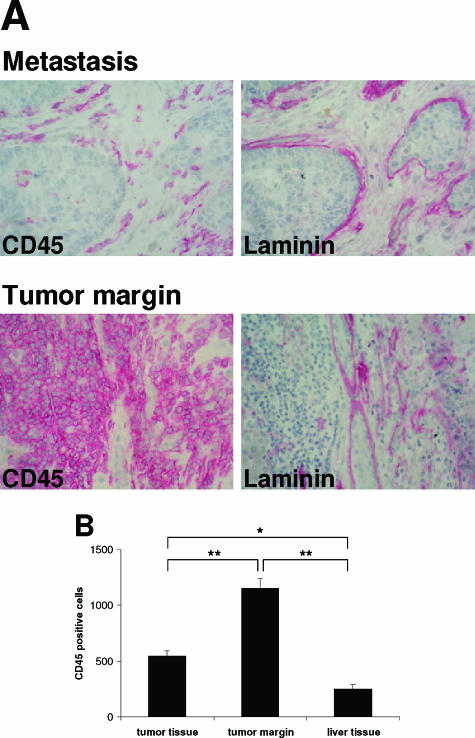
To validate inflammation in CLM, we analyzed cryosections of colorectal liver metastases and corresponding distant liver tissues for the presence of CD45-positive cells by immunohistochemistry. Staining of liver tissue for CD45 (also referred to as leukocyte common antigen) identifies Kupffer cells, which are resident macrophages, and infiltrating leukocytes.39 As shown in Figure 3A, many infiltrating CD45-positive cells were found within the stromal septa in close proximity to stromal fibroblasts. Large infiltrations of CD45-positive cells were detected at the tumor margin. Staining for laminin, a basement membrane glycoprotein, revealed that the CD45-positive cells are located outside vessel- or duct-like structures, which are surrounded by a laminin-positive layer (Figure 3A). Quantification of the number of CD45-positive cells unveiled that most leukocytes are located at the boundary region of the metastasis. In comparison with distant normal liver tissue, the number of CD45-positive cells was markedly elevated, even within the metastases (Figure 3B). The presence of inflammation was furthermore reflected by increased stromal immunoreactivity for ICAM-1 (Figure 1), a cell surface glycoprotein implicated in inflammation and cancer invasion that is regulated by TNF-α and NF-κB.40
Figure 3.
The metastatic site is associated with leukocyte infiltration. A: Representative immunohistochemical staining of serial sections from colorectal liver metastases and their margins for CD45 and laminin (original magnification, ×400). B: Mean numbers of CD45-positive cells within tumor, tumor margin, and liver tissue (n = 14; mean ± SEM; *P < 0.05, **P < 0.01).
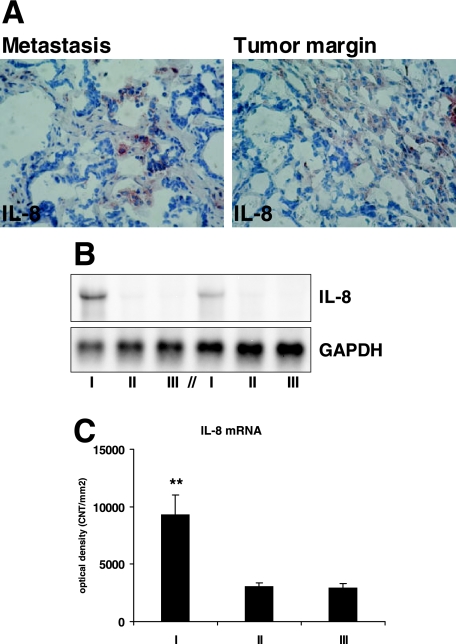
Colorectal Liver Metastases Express High Levels of IL-8
Recognized as a potent chemoattractant for leukocytes in inflammation, IL-8 has recently been shown to be implicated in tumor invasion and angiogenesis.29,30,31 We next confirmed IL-8 expression in CLM by immunohistochemistry. IL-8 was detected within the stromal septae and at the boundary region of the metastases. Most fibroblasts showed weak staining, but individual cell populations within the stroma strongly expressed IL-8 (Figure 4A). On the mRNA level, IL-8 expression was increased threefold in the metastasis tissue compared with adjacent and distant liver tissue (n = 10, P < 0.01; Figure 4, B and C).
Figure 4.
CAFs in situ stain positive for IL-8, and IL-8 mRNA is increased in metastatic tissue. A: Representative immunohistochemical analysis of IL-8 in colorectal liver metastases and the tumor margin (original magnification, ×400). B: Representative Northern blot analysis showing IL-8 mRNA expression in tumor tissue (I), adjacent, peritumor tissue (II), and distant liver tissue (III) in tissue samples from two different patients. Rehybridization for glyceraldehyde-3-phosphate dehydrogenase for normalization. In the diagram below (C), mean results of Northern analyses for IL-8 mRNA expressions in tumor tissue (I), adjacent, peritumor tissue (II), and distant liver tissue (III) are quantified (n = 10; mean ± SEM; **P < 0.01 versus peritumor tissue (II) and distant liver tissue (III)).
TNF-α Induces IL-8 Expression by CAFs and LFs in Vitro
To investigate the mRNA expression of IL-8 and the effect of various cytokines on IL-8 expression by primary CAFs and LFs, we performed nonradioactive Northern blot analyses using digoxigenin-labeled antisense DNA probes. The advantage of this technique is that it provides a reproducible quantitative expression analysis of a selected transcript from a total RNA sample without potential bias caused by prior reverse transcription and amplification. PDGF-BB (10 ng/ml) slightly induced the expression of IL-8 mRNA by CAFs and LFs, and TNF-α (50 ng/ml) markedly increased IL-8 expression (Figure 5, A and B), whereas transforming-growth factor-β1 (5 ng/ml) showed no effect. Following incubation with TNF-α, mean expression of IL-8 as measured by densitometric band analysis increased approximately 12-fold in CAFs (n = 4, P < 0.01) and 34-fold in LFs (n = 4, P < 0.01). However, this difference was not statistically significant. The inducing effect of TNF-α on IL-8 expression was confirmed at the protein level by ELISA measurements of the cell culture supernatants (Figure 5C). The constitutive IL-8 expression levels in controls (CAFs and LFs cultured in the presence of 0.5% FBS) ranged from 0 to 390 pg/ml in CAFs and from 0 to 175 pg/ml in LFs (n = 5). As shown in Figure 5C, TNF-α (50 ng/ml) up-regulated the expression of IL-8 protein in both cell types without significant difference. A slight increase on IL-8 protein expression was observed by stimulation with PDGF-BB (10 ng/ml) in both CAFs and LFs, but this effect was not statistically significant.
Figure 5.
TNF-α induces expression of IL-8 by human CAFs and LFs in vitro. A: Representative Northern blot analysis showing the effect of cytokines [transforming growth factor-β (TGF-β), 5 ng/ml; PDGF-BB, 10 ng/ml; and TNF-α, 50 ng/ml) and increased concentration of FBS (10%) on IL-8 mRNA expression by CAFs and liver fibroblasts. Controls (CON) are nonstimulated CAFs or LFs (0.5% FBS) (ST, molecular RNA weight marker). The lower bands show glyceraldehyde-3-phosphate dehydrogenase mRNA expression after rehybridization for normalization. Note that the IL-8-specific band is still abundant. B: Results of densitometric band analysis of IL-8 mRNA expression by CAFs and LFs (n = 4; mean ± SEM; ns, not significant; * and #P < 0.01 versus respective control). C: Protein expression of IL-8 by CAFs and LFs in vitro, determined by ELISA measurements (n = 5; mean ± SEM; * and #P < 0.01 versus respective control).
Parthenolide Suppresses TNF-α-Mediated IL-8 Expression by CAFs
NF-κB has been identified as the pivotal TNF-α downstream signaling component in inflammation.19,21 Once activated, NF-κB dissociates from its inhibitors and translocates to the nucleus where it leads to the activation of proinflammatory and chemotactic agents and adhesion molecules, thereby creating an inflammatory self-maintaining state. The sesquiterpene lactone parthenolide has recently been shown to inhibit the activation of NF-κB.41 To analyze whether TNF-α acts via NF-κB on CAFs, increasing concentrations of parthenolide (1, 5, and 10 μmol/L) in the absence or presence of TNF-α (10 ng/ml) have been tested. Whereas the lowest concentration of parthenolide tested in our experiments (1 μmol/L) had no effect on TNF-α-induced IL-8 expression, we found that the addition of 5 μmol/L parthenolide significantly inhibited TNF-α-mediated IL-8 mRNA expression (Figure 6, A and B). Similar results were obtained by analyzing IL-8 protein by ELISA (Figure 6C).
Figure 6.
The NF-κB inhibitor parthenolide inhibits the effect of TNF-α on IL-8 expression by CAFs. A: Representative Northern blot analysis of IL-8 mRNA expression by the CAFs in vitro under incubation with or without TNF-α in the presence or absence of increasing concentrations of parthenolide. B: Results of densitometric band analyses of IL-8 mRNA expression by CAFs that were exposed to TNF-α in either the presence or absence of increasing concentrations of parthenolide (n = 4; mean ± SEM; *P < 0.05, **P < 0.001). C: The combined effect of increasing concentrations parthenolide and TNF-α on IL-8 protein expression released by CAFs that were incubated for 24 hours was measured by ELISA and quantified for statistical analysis (n = 4; mean ± SEM; *P < 0.05, **P < 0.001).
CM from CAF and LF Cultures Similarly Promotes Tumor and Endothelial Cell Migration
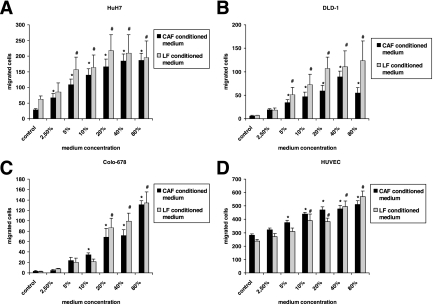
We next studied the effect of conditioned media from CAF and LF cultures on tumor and endothelial cell chemotaxis using a modified Boyden chamber assay. Conditioned media from both cultures significantly increased the number of migrating HuH-7 hepatoma, DLD-1, and Colo-678 colon carcinoma cells as well as HUVECs (Figure 7, A–D) toward CM from CAFs and LFs in a concentration-dependent manner. Unexpectedly, the response of the DLD-1 cells to conditioned media from LF cultures was stronger than that observed with conditioned media from CAF cultures. However, this difference was statistically not significant. The differential responses of HUVECs to CM from CAF and LF (Figure 7D) were also not significant. Thus, both CAF and LF secrete factors that direct migration of different tumor cells and endothelial cells in vitro.
Figure 7.
Boyden chamber analyses testing chemotaxis of HuH7 hepatoma cells (A), DLD1 colon carcinoma cells (B), Colo-678 colon carcinoma cells (C), and HUVECs (D) induced by conditioned medium from CAFs and LFs. Increasing concentrations of the conditioned media were placed in the lower chamber of a modified Boyden chamber system as described in Materials and Methods. Tumor cells (15 × 103) or HUVECs in 50-μl medium containing 2% bovine serum albumin were seeded in the upper wells. Each experimental condition was examined by quadruplicate measurements. Quantification results from five different CAF cultures and corresponding LF cultures are shown (n = 5; mean ± SEM; * and #P < 0.001 versus respective control).
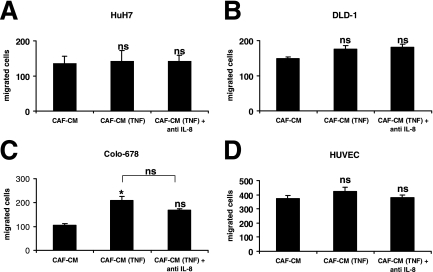
CM from CAFs Exposed to TNF-α Increase Migration of Colo-678 Cells, but Blockage of IL-8 Had No Inhibitory Effect
IL-8 has been previously described to promote the migration of colon cancer cells and endothelial cells in vitro.31,32,42 We speculated that the increased IL-8 protein levels in cell culture supernatants of CAFs exposed to 10 ng/ml TNF-α (Figure 6C) would increase the migration of these cells in comparison with CM of nonstimulated CAFs. As shown in Figure 8, Colo-678 cells showed increased migration toward CM from CAFs incubated with TNF-α in comparison with CM of CAFs that were incubated in 0.5% FBS for the same time period. Blockage of IL-8 by neutralizing antibody as described in Materials and Methods showed a mild, but not significant, inhibitory effect (Figure 8C). We followed this lack of evidence for a role of IL-8 as a chemoattractant of the tested cell lines by investigating their migration toward increasing concentrations of IL-8 in the lower chamber. Among the tested cell lines, these experiments revealed only slight increases for migratory activity in Colo-678 cells and HUVECs (data not shown). With respect to the concentration-dependent increases as shown in Figure 7, the lack of responsiveness to IL-8 in our Boyden system strongly indicates that CAFs release other as yet unidentified chemoattractants.
Figure 8.
Effect of TNF-α on chemotactic properties of CAFs. The migration of HuH7 hepatoma cells (A), DLD1 colon carcinoma cells (B), Colo-678 colon carcinoma cells (C), and HUVECs (D) toward conditioned medium of CAFs that were incubated for 24 hours in 10 ng/ml TNF-α [CAF-CM (TNF)] and toward CM of nonstimulated CAFs (CAF-CM) were compared. In the CM of nonstimulated CAFs, TNF-α was added after the incubation time to exclude that differences in migration were caused by the presence of exogenous TNF-α. The effect of IL-8 blockage was tested by preincubation with an IL-8-neutralizing antibody (10 μg/ml; R&D Systems). The experiments were repeated four times using CAF cultures from different patients (n = 4; mean ± SEM; *P < 0.05 versus CAF-CM).
Discussion
In this study, we present three novel observations with respect to CAF biology and inflammation in CLM. First, we show that the CAFs are phenotypically and functionally similar to a population of fibroblastic cells located in the portal area of normal liver tissue, raising the possibility that these resident liver fibroblasts significantly contribute to the CAF population. Second, we show that IL-8 expression is increased in CLM in comparison with surrounding liver tissue. Third, we show for the first time that CAFs are highly responsive to proinflammatory TNF-α by means of up-regulation of IL-8 through activation of NF-κB. We conclude that the proinflammatory milieu in CLM is at least in part generated by fibroblasts that originate in the liver itself.
In established CLM, the cellular origin of the CAF population is not fully defined. With respect to gene expression patterns, a recent study showed a higher homology between CAFs and liver fibroblasts in comparison with skin fibroblasts.43 It is generally believed that CAFs are generated from HSCs, which are well characterized for their ability to undergo myofibroblastic transformation in liver fibrogenesis.8,9,10 One aim of our study was to provide further insight into this issue. We have observed by immunohistochemistry on tissue sections that CAFs from CLM are phenotypically similar to liver (myo)fibroblasts residing in the portal and pericentral area (Figure 1 and Table 1), being vimentin+, α-SMA+, and Thy-1+. These findings are in agreement with our morphological in vitro analyses (Figure 2 and Table 1). In addition, both cell types release mediators that promote tumor and endothelial cell migration to a comparable dose-dependent extend (Figure 7). Recently, it has been described that blood or bone marrow-derived mesenchymal precursors contribute to the excessive population of fibroblasts in liver fibrosis,12,13 and this may potentially represent an alternative source for CAFs in solid organ malignancy. There exist several reports showing that a proportion of fibroblasts located in experimental tumors have a bone marrow origin.44,45 Direkze et al44 observed a proportion of 25% myofibroblasts derived from transplanted bone marrow in a model of murine pancreas tumor. There is also experimental data supporting the concept that the percentage of bone marrow-derived fibroblasts increases in advanced stages of cancer development.45 Therefore, it is possible that bone marrow-derived mesenchymal precursors contribute to the CAF population in established CLM.
Our results indicate that the CAFs are located in an inflammatory milieu, as evidenced by ICAM-1 immunohistochemistry (Figure 1) and the presence of CD45-positive leukocyte cluster within the tumor stroma (Figure 3). Among the various growth factors and cytokines that are expected to be released in this microenvironment, some were clearly related to specific functional roles in metastasis progression. For example, it has been shown that targeting of stromal PDGF receptors decreases growth and metastasis of orthotopic implanted colon cancer cells at the primary and the metastatic site.18 These data are compatible with our previous observation that PDGF-BB is a mitogen for cultured CAFs from CLM,35 suggesting a role in the recruitment of resident fibroblasts from liver tissue to generate the CAF population.
We hypothesized that the morphologically evident inflammation is associated with IL-8 expression, because the latter is reputed for its role as a chemoattractant for leukocytes.27 Several functional implications arise from our observation of increased IL-8 expression in CLM in comparison to surrounding liver tissue. IL-8 has been established as a proinvasive factor for malignant cells, as a proangiogenic factor, and as a chemotactic factor, that maintains the inflammatory microenvironment. In colon cancer cells, a positive correlation between their level of endogenous IL-8 expression and invasive capacity in vitro has been reported,31 and exogenous IL-8 enhanced the proliferation and adhesion to endothelial cells in cell lines with low endogenous expression of IL-8.31 In accordance with these data, Terada et al30 recently described an association between IL-8 levels and tumor size, depth of infiltration, Dukes stage, and presence of liver metastasis in primary colorectal carcinoma. Apart from experimental data on xenografts,46 a proangiogenic role of IL-8 in primary colorectal cancer or metastases is less evident based on the existing literature. Recently, Miyagawa et al47 described a significant positive correlation between macrophage density and microvessel count in 71 cases of CLM. It is interesting to speculate whether the relation between inflammation and angiogenesis is mediated by IL-8. Collectively, it seems plausible to conclude that the increased IL-8 levels in CLM contribute to a microenvironment that favors metastasis progression.
The screening for a possible role of inflammatory mediators that could regulate IL-8 expression by CAFs from CLM clearly point to TNF-α. Recently, increased TNF-α production by Kupffer cells in vivo has been shown to be an essential step during the formation of colorectal liver metastasis in mice.16 Increased TNF-α levels were moreover found around colorectal liver metastases and within mononuclear cells in the tumor periphery of intrahepatic cholangiocarcinoma.48,49 Our in vitro analyses suggest that the increased expression of IL-8 in CLM is in part due to TNF-α-mediated release by fibroblasts (Figure 5). Moreover, the finding that CAFs and LFs were similarly responsive to TNF-α raises the possibility that resident liver fibroblasts may already contribute to IL-8 production following paracrine stimulation without direct contact to tumor cells. Because IL-8 itself promotes chemotaxis of neutrophils and macrophages, important cellular sources of TNF-α,27 it is likely that the effect of TNF-α on CAFs and LFs helps to generate a self-maintaining inflammatory microenvironment.
We have shown that the extracellular signal-activated transcription factor NF-κB contributes to TNF-α-mediated induction of IL-8 in human CAFs from CLM as a downstream effector (Figure 6). Thus, NF-κB-selective inhibitors such as parthenolide may have potential clinical benefit in the context of anticancer drug development. It was already shown that NF-κB up-regulated chemokine expression in fibroblasts associated with nonmalignant inflammation as well as in cancer cells.22,50 However, a link between NF-κB and IL-8 expression has not yet been described for fibroblasts from cancerous stroma. It cannot be excluded that fibroblasts from other human tissues would behave like the tested CAFs or LFs because there exists published data that fibroblast populations from benign tissue are more or less responsive to TNF-α by means of IL-8 induction,22,23,24,25 most probably to a different extent because of their heterogeneity.26 Therefore it seems necessary to evaluate carefully the potential side effects of a NF-κB inhibition on non-cancer related inflammatory conditions, eg, wound healing, by appropriate in vivo experiments.
A potential limitation of this study is that we were not able to provide clear evidence that IL-8 acts as a chemoattractant for tumor cells and endothelial cells (Figure 8). Contrary to our results, the latter has been described by several authors in the literature.28,31,32,42 Indeed, there exist numerous possibilities to perform migration analyses in vitro, and we cannot exclude the possibility that the usage of other experimental methods would lead to different results. However, our observation of increased migration of Colo-678 cells toward CM of CAFs stimulated with TNF-α points to a potential role of other chemokines that are transcriptional regulated by NF-κB.
In summary, CAFs from human CLM are myofibroblastic cells that show clear similarities to resident portal LFs. CAFs are located in an inflammatory microenvironment and contribute significantly to IL-8 expression that is increased in CLM in comparison with surrounding liver tissue. The IL-8 expression by CAFs is highly inducible by TNF-α through activation of NF-κB. Thereby, these cells may help to form a permissive microenvironment for cancer invasion and angiogenesis.
Acknowledgments
We thank Sigrid Himpel for her excellent technical and administrative assistance and Regina Fillbrandt for her technical help with the Boyden chamber assays.
Footnotes
Address reprint requests to Lars Mueller, M.D., Department of General and Thoracic Surgery, University Hospital of Schleswig-Holstein, Campus Kiel, Arnold-Heller-Str. 7, 24105 Kiel, Germany. E-mail: lars.mueller@uksh-kiel.de.
References
- Jemal A, Tiwari RC, Murray T, Ghafoor A, Samuels A, Ward E, Feuer EJ, Thun MJ. Cancer statistics, 2004. CA Cancer J Clin. 2004;54:8–29. doi: 10.3322/canjclin.54.1.8. [DOI] [PubMed] [Google Scholar]
- Khatri VP, Petrelli NJ, Belghiti J. Extending the frontiers of surgical therapy for hepatic colorectal metastases: is there a limit? J Clin Oncol. 2005;23:8490–8499. doi: 10.1200/JCO.2004.00.6155. [DOI] [PubMed] [Google Scholar]
- Desmoulière A, Guyot C, Gabbiani G. The stroma reaction myofibroblast: a key player in the control of tumor cell behavior. Int J Dev Biol. 2004;48:509–517. doi: 10.1387/ijdb.041802ad. [DOI] [PubMed] [Google Scholar]
- Bhowmick NA, Neilson EG, Moses HL. Stromal fibroblasts in cancer initiation and progression. Nature. 2004;432:332–337. doi: 10.1038/nature03096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzocca A, Coppari R, De Franco R, Cho JY, Libermann TA, Pinzani M, Toker A. A secreted form of ADAM9 promotes carcinoma invasion through tumor-stromal interactions. Cancer Res. 2005;65:4728–4738. doi: 10.1158/0008-5472.CAN-04-4449. [DOI] [PubMed] [Google Scholar]
- Ooi LP, Crawford DH, Gotley DC, Clouston AD, Strong RW, Gobe GC, Halliday JW, Bridle KR, Ramm GA. Evidence that “myofibroblast-like” cells are the cellular source of capsular collagen in hepatocellular carcinoma. J Hepatol. 1997;26:798–807. doi: 10.1016/s0168-8278(97)80245-0. [DOI] [PubMed] [Google Scholar]
- Lunevicius R, Nakanishi H, Ito S, Kozaki K, Kato T, Tatematsu M, Yasui K. Clinicopathological significance of fibrotic capsule formation around liver metastasis from colorectal cancer. J Cancer Res Clin Oncol. 2001;127:193–199. doi: 10.1007/s004320000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gressner AM, Weiskirchen R. Modern pathogenetic concepts of liver fibrosis suggest stellate cells and TGF-β as major players and therapeutic targets. J Cell Mol Med. 2006;10:76–99. doi: 10.1111/j.1582-4934.2006.tb00292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyot C, Lepreux S, Combe C, Doudnikoff E, Bioulac-Sage P, Balabaud C, Desmouliere A. Hepatic fibrosis and cirrhosis: the (myo)fibroblastic cell subpopulations involved. Int J Biochem Cell Biol. 2006;38:135–151. doi: 10.1016/j.biocel.2005.08.021. [DOI] [PubMed] [Google Scholar]
- Cassiman D, Roskams T. Beauty is in the eye of the beholder: emerging concepts and pitfalls in hepatic stellate cell research. J Hepatol. 2002;37:527–535. doi: 10.1016/s0168-8278(02)00263-5. [DOI] [PubMed] [Google Scholar]
- Andrade ZA, Guerret S, Fernandes AL. Myofibroblasts in schistosomal portal fibrosis of man. Mem Inst Oswaldo Cruz. 1999;94:87–93. doi: 10.1590/s0074-02761999000100018. [DOI] [PubMed] [Google Scholar]
- Forbes SJ, Russo FP, Rey V, Burra P, Rugge M, Wright NA, Alison MR. A significant proportion of myofibroblasts are of bone marrow origin in human liver fibrosis. Gastroenterology. 2004;126:955–963. doi: 10.1053/j.gastro.2004.02.025. [DOI] [PubMed] [Google Scholar]
- Kisseleva T, Uchinami H, Feirt N, Quintana-Bustamante O, Segovia JC, Schwabe RF, Brenner DA. Bone marrow-derived fibrocytes participate in pathogenesis of liver fibrosis. J Hepatol. 2006;45:429–438. doi: 10.1016/j.jhep.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudmik LR, Magliocco AM. Molecular mechanisms of hepatic metastasis in colorectal cancer. J Surg Oncol. 2005;92:347–359. doi: 10.1002/jso.20393. [DOI] [PubMed] [Google Scholar]
- Khatib AM, Auguste P, Fallavollita L, Wang N, Samani A, Kontogiannea M, Meterissian S, Brodt P. Characterization of the host proinflammatory response to tumor cells during the initial stages of liver metastases. Am J Pathol. 2005;167:749–759. doi: 10.1016/S0002-9440(10)62048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsushima H, Ito N, Tamura S, Matsuda Y, Inada M, Yabuuchi I, Imai Y, Nagashima R, Misawa H, Takeda H, Matsuzawa Y, Kawata S. Circulating transforming growth factor β1 as a predictor of liver metastasis after resection in colorectal cancer. Clin Cancer Res. 2001;7:1258–1262. [PubMed] [Google Scholar]
- Kitadai Y, Sasaki T, Kuwai T, Nakamura T, Bucana CD, Fidler IJ. Targeting the expression of platelet-derived growth factor receptor by reactive stroma inhibits growth and metastasis of human colon carcinoma. Am J Pathol. 2006;169:2054–2065. doi: 10.2353/ajpath.2006.060653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karin M, Greten FR. NF-κB: linking inflammation and immunity to cancer development and progression. Nat Rev Immunol. 2005;5:749–759. doi: 10.1038/nri1703. [DOI] [PubMed] [Google Scholar]
- Hanada T, Yoshimura A. Regulation of cytokine signaling and inflammation. Cytokine Growth Factor Rev. 2002;13:413–421. doi: 10.1016/s1359-6101(02)00026-6. [DOI] [PubMed] [Google Scholar]
- Aggarwal BB. Nuclear factor-κB: the enemy within. Cancer Cell. 2004;6:203–208. doi: 10.1016/j.ccr.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Gelbmann CM, Leeb SN, Vogl D, Maendel M, Herfarth H, Scholmerich J, Falk W, Rogler G. Inducible CD40 expression mediates NFκB activation and cytokine secretion in human colonic fibroblasts. Gut. 2003;52:1448–1456. doi: 10.1136/gut.52.10.1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stebulis JA, Rossetti RG, Atez FJ, Zurier RB. Fibroblast-like synovial cells derived from synovial fluid. J Rheumatol. 2005;32:301–306. [PubMed] [Google Scholar]
- Larsen CG, Anderson AO, Oppenheim JJ, Matsushima K. Production of interleukin-8 by human dermal fibroblasts and keratinocytes in response to interleukin-1 or tumour necrosis factor. Immunology. 1989;68:31–36. [PMC free article] [PubMed] [Google Scholar]
- Monick MM, Aksamit TR, Geist LJ, Hunninghake GW. Dexamethasone inhibits IL-1 and TNF activity in human lung fibroblasts without affecting IL-1 or TNF receptors. Am J Physiol. 1994;267:L33–L38. doi: 10.1152/ajplung.1994.267.1.L33. [DOI] [PubMed] [Google Scholar]
- Parsonage G, Falciani F, Burman A, Filer A, Ross E, Bofill M, Martin S, Salmon M, Buckley CD. Global gene expression profiles in fibroblasts from synovial, skin and lymphoid tissue reveals distinct cytokine and chemokine expression patterns. Thromb Haemost. 2003;90:688–697. doi: 10.1160/TH03-04-0208. [DOI] [PubMed] [Google Scholar]
- Mukaida N, Harada A, Matsushima K. Interleukin-8 (IL-8) and monocyte chemotactic and activating factor (MCAF/MCP-1), chemokines essentially involved in inflammatory and immune reactions. Cytokine Growth Factor Rev. 1998;9:9–23. doi: 10.1016/s1359-6101(97)00022-1. [DOI] [PubMed] [Google Scholar]
- Belperio JA, Keane MP, Arenberg DA, Addison CL, Ehlert JE, Burdick MD, Strieter RM. CXC chemokines in angiogenesis. J Leukoc Biol. 2000;68:1–8. [PubMed] [Google Scholar]
- Lane BR, Liu J, Bock PJ, Schols D, Coffey MJ, Strieter RM, Polverini PJ, Markovitz DM. Interleukin-8 and growth-regulated oncogene alpha mediate angiogenesis in Kaposi’s sarcoma. J Virol. 2002;76:11570–11583. doi: 10.1128/JVI.76.22.11570-11583.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terada H, Urano T, Konno H. Association of interleukin-8 and plasminogen activator system in the progression of colorectal cancer. Eur Surg Res. 2005;37:166–172. doi: 10.1159/000085964. [DOI] [PubMed] [Google Scholar]
- Li A, Varney ML, Singh RK. Expression of interleukin 8 and its receptors in human colon carcinoma cells with different metastatic potentials. Clin Cancer Res. 2001;7:3298–3304. [PubMed] [Google Scholar]
- Itoh Y, Joh T, Tanida S, Sasaki M, Kataoka H, Itoh K, Oshima T, Ogasawara N, Togawa S, Wada T, Kubota H, Mori Y, Ohara H, Nomura T, Higashiyama S, Itoh M. IL-8 promotes cell proliferation and migration through metalloproteinase-cleavage proHB-EGF in human colon carcinoma cells. Cytokine. 2005;29:275–282. doi: 10.1016/j.cyto.2004.11.005. [DOI] [PubMed] [Google Scholar]
- Lamszus K, Schmidt NO, Jin L, Laterra J, Zagzag D, Way D, Witte M, Weinand M, Goldberg ID, Westphal M, Rosen EM. Scatter factor promotes motility of human glioma and neuromicrovascular endothelial cells. Int J Cancer. 1998;75:19–28. doi: 10.1002/(sici)1097-0215(19980105)75:1<19::aid-ijc4>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- Mueller L, Broering DC, Meyer J, Vashist Y, Goettsche J, Wilms C, Rogiers X. The induction of the immediate-early-genes Egr-1. PAI-1 and PRL-1 during liver regeneration in surgical models is related to increased portal flow. J Hepatol. 2002;37:606–612. doi: 10.1016/s0168-8278(02)00238-6. [DOI] [PubMed] [Google Scholar]
- Mueller L, Goumas FA, Himpel S, Brilloff S, Rogiers X, Broering DC. Imatinib mesylate inhibits proliferation and modulates cytokine expression of human cancer-associated stromal fibroblasts from colorectal metastases. Cancer Lett. 2007;250:329–338. doi: 10.1016/j.canlet.2006.10.024. [DOI] [PubMed] [Google Scholar]
- Rege TA, Hagood JS. Thy-1 as a regulator of cell-cell and cell-matrix interactions in axon regeneration, apoptosis, adhesion, migration, cancer, and fibrosis. FASEB J. 2006;20:1045–1054. doi: 10.1096/fj.05-5460rev. [DOI] [PubMed] [Google Scholar]
- Koumas L, Smith TJ, Feldon S, Blumberg N, Phipps RP. Thy-1 expression in human fibroblast subsets defines myofibroblastic or lipofibroblastic phenotypes. Am J Pathol. 2003;163:1291–1300. doi: 10.1016/S0002-9440(10)63488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marugg RA, Gehr P, de Leeuw M. Secondary lysosomes as an integral part of the cytoskeleton: a morphological study in rat Kupffer cells. J Struct Biol. 1990;105:146–153. doi: 10.1016/1047-8477(90)90108-o. [DOI] [PubMed] [Google Scholar]
- Solaun MS, Mendoza L, De Luca M, Gutierrez V, Lopez MP, Olaso E, Lee Sim BK, Vidal-Vanaclocha F. Endostatin inhibits murine colon carcinoma sinusoidal-type metastases by preferential targeting of hepatic sinusoidal endothelium. Hepatology. 2002;35:1104–1116. doi: 10.1053/jhep.2002.32528. [DOI] [PubMed] [Google Scholar]
- Collins T, Read MA, Neish AS, Whitley MZ, Thanos D, Maniatis T. Transcriptional regulation of endothelial cell adhesion molecules: NF-κB and cytokine-inducible enhancers. FASEB J. 1995;9:899–909. [PubMed] [Google Scholar]
- García-Piñeres AJ, Castro V, Mora G, Schmidt TJ, Strunck E, Pahl HL, Merfort I. Cysteine 38 in p65/NF-κB plays a crucial role in DNA binding inhibition by sesquiterpene lactones. J Biol Chem. 2001;276:39713–39720. doi: 10.1074/jbc.M101985200. [DOI] [PubMed] [Google Scholar]
- Li A, Varney ML, Valasek J, Godfrey M, Dave BJ, Singh RK. Autocrine role of interleukin-8 in induction of endothelial cell proliferation, survival, migration and MMP-2 production and angiogenesis. Angiogenesis. 2005;8:63–71. doi: 10.1007/s10456-005-5208-4. [DOI] [PubMed] [Google Scholar]
- Nakagawa H, Liyanarachchi S, Davuluri RV, Auer H, Martin EW, Jr, de la Chapelle A, Frankel WL. Role of cancer-associated stromal fibroblasts in metastatic colon cancer to the liver and their expression profiles. Oncogene. 2004;23:7366–7377. doi: 10.1038/sj.onc.1208013. [DOI] [PubMed] [Google Scholar]
- Direkze NC, Hodivala-Dilke K, Jeffery R, Hunt T, Poulsom R, Oukrif D, Alison MR, Wright NA. Bone marrow contribution to tumor-associated myofibroblasts and fibroblasts. Cancer Res. 2004;64:8492–8495. doi: 10.1158/0008-5472.CAN-04-1708. [DOI] [PubMed] [Google Scholar]
- Ishii G, Sangai T, Oda T, Aoyagi Y, Hasebe T, Kanomata N, Endoh Y, Okumura C, Okuhara Y, Magae J, Emura M, Ochiya T, Ochiai A. Bone-marrow-derived myofibroblasts contribute to the cancer-induced stromal reaction. Biochem Biophys Res Commun. 2003;309:232–240. doi: 10.1016/s0006-291x(03)01544-4. [DOI] [PubMed] [Google Scholar]
- Mizukami Y, Jo WS, Duerr EM, Gala M, Li J, Zhang X, Zimmer MA, Iliopoulos O, Zukerberg LR, Kohgo Y, Lynch MP, Rueda BR, Chung DC. Induction of interleukin-8 preserves the angiogenic response in HIF-1α-deficient colon cancer cells. Nat Med. 2005;11:992–997. doi: 10.1038/nm1294. [DOI] [PubMed] [Google Scholar]
- Miyagawa S, Miwa S, Soeda J, Kobayashi A, Kawasaki S. Morphometric analysis of liver macrophages in patients with colorectal liver metastasis. Clin Exp Metastasis. 2002;19:119–125. doi: 10.1023/a:1014571013978. [DOI] [PubMed] [Google Scholar]
- Gulubova MV. Expression of cell adhesion molecules, their ligands and tumour necrosis factor alpha in the liver of patients with metastatic gastrointestinal carcinomas. Histochem J. 2002;34:67–77. doi: 10.1023/a:1021304227369. [DOI] [PubMed] [Google Scholar]
- Ohira S, Sasaki M, Harada K, Sato Y, Zen Y, Isse K, Kozaka K, Ishikawa A, Oda K, Nimura Y, Nakanuma Y. Possible regulation of migration of intrahepatic cholangiocarcinoma cells by interaction of CXCR4 expressed in carcinoma cells with tumor necrosis factor-alpha and stromal-derived factor-1 released in stroma. Am J Pathol. 2006;168:1155–1168. doi: 10.2353/ajpath.2006.050204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasumoto K, Okamoto S, Mukaida N, Murakami S, Mai M, Matsushima K. Tumor necrosis factor alpha and interferon gamma synergistically induce interleukin 8 production in a human gastric cancer cell line through acting concurrently on AP-1 and NF-κB-like binding sites of the interleukin 8 gene. J Biol Chem. 1992;267:22506–22511. [PubMed] [Google Scholar]