Abstract
In a multi-health center study, a new rapid optical immunoassay (OIA) for the detection of Shiga toxin types 1 and 2, the BioStar OIA SHIGATOX kit (Inverness Medical Professional Diagnostics, Inc.), was used to prospectively screen 742 fresh fecal samples for Shiga toxins in parallel with the Premier enterohemorrhagic Escherichia coli (EHEC) kit (Meridian BioScience, Inc.) with and without enrichment of the specimens by incubation in MacConkey broth. Additionally, 85 previously tested frozen fecal samples were assessed as described above. All positive immunoassay results were confirmed by the Vero cell cytotoxicity assay. A further modification of the screening procedure was evaluated on 470 of the prospectively screened specimens. Swabs of growth from conventionally plated stool culture media were subjected to the OIA SHIGATOX, and results were compared with those obtained with the Premier EHEC kit following broth enrichment. Overall, the OIA SHIGATOX kit was significantly more sensitive than the Premier EHEC kit on fresh direct stool specimens (sensitivities, 96.8% and 83.9%, respectively; P < 0.05). The two assays performed equally well with each other on frozen and broth-enriched samples. The colony sweep method used in conjunction with the OIA kit was somewhat more effective at detection of Shiga toxins from growth on agar than the overnight broth enrichment procedure used with the Premier EHEC assay (sensitivities, 100% and 92%, respectively; P < 0.09). Overall, the OIA SHIGATOX kit provided rapid, easy-to-interpret results and was highly effective at detection of Shiga toxin-producing E. coli in fecal samples and overnight cultures.
Since the emergence of Shiga toxin (Stx)-producing Escherichia coli (STEC) serotype O157:H7 as an agent of hemorrhagic colitis and the hemolytic-uremic syndrome (HUS) in 1982, hundreds of outbreaks of disease associated with enterohemorrhagic E. coli (EHEC) have been reported in the United States (12), including a large multistate outbreak associated with bagged spinach last year (3). The serotype (O157) and the characteristic phenotype of these strains to generally not ferment sorbitol have aided their recognition in the microbiology laboratory (6). However, numerous other serotypes of STEC have also been documented to cause a spectrum of diseases, ranging from mild diarrhea to HUS, that present sporadically or in outbreak situations (8). In 1999 the CDC estimated from clinical and laboratory data that 110,000 cases of STEC infection occur annually in the United States, with 73,000 cases attributable to E. coli O157:H7 and the remaining one-third (37,000 cases) attributed to non-O157 serotypes (10). Unfortunately, culture strategies that are used only for patients with bloody diarrhea, methods based strictly on screens for non-sorbitol fermenters or serotype O157, and the limited use of techniques for the detection of Shiga type toxins fail to capture the true incidence of non-O157 STEC or the extent of STEC infections in general. In some settings where methods for the detection of Stx(s) have been used, the incidence of non-O157 strains appears to be greater than that estimated earlier, accounting for 46 to >50% of STEC isolates (1, 4). Since non-O157 STEC strains became reportable pathogens in 2000, the U.S. CDC recommends that laboratories routinely screen stool cultures for STEC and utilize methods for Stx detection such as immunoassay or PCR (2, 16). If Stx detection is to be practical and widely implemented, the method must be rapid, sensitive when used directly on clinical specimens, and conducive to timely application without the need for batch testing. The BioStar SHIGATOX test is a 15-min, self-contained assay for Stx types 1 and 2 (Stx1 and Stx2) (without differentiation of types) that uses the optical immunoassay (OIA) format for toxin detection. In the OIA method in general, slight changes in the optical thickness caused by antigen-antibody interactions on the surface of a silicon wafer alter light reflection, a phenomenon that is visually perceived as a color change. For the SHIGATOX test, the optical surface is coated with heterologous anti-Stx antibodies that capture Stx1 and/or Stx2 if it is present in a test sample. The subsequent addition of secondary anti-Stx1 and -2 antibodies increases the thickness of the assay surface, and light reflection is altered to the extent that the surface then appears purple rather than gold.
In a prospective study conducted from July 2005 to September 2006 at three clinical laboratories in the eastern (Inova Fairfax Hospital, Falls Church, VA), southern (Children's Healthcare of Atlanta, Atlanta, GA), and western (Primary Children's Medical Center and University of Utah Hospital, Salt Lake City) regions of the United States, the OIA SHIGATOX method was compared to the established Premier EHEC enzyme-linked immunoassay (EIA) for the detection of STEC (9). We report the findings of that investigation here and conclude that the SHIGATOX OIA toxin detection method is a more sensitive, faster, and easier method for the detection of Stx's directly from stool and after culture enrichment than the Premier EIA method.
MATERIALS AND METHODS
Sample collection.
Seven hundred forty-two fresh liquid or semisolid fecal samples (without transport media) that were submitted to the participating laboratories for culture of enteric pathogens were sequentially enrolled in the phase I prospective study. Samples from patients over the age of 5 months were included without limitation by sex or by inpatient or outpatient status, provided there was an adequate amount of sample for culture, the Premier EHEC assay, the SHIGATOX assay, and the cytotoxicity assay (at least 15 ml for liquid stools or a walnut-sized mass for semisolid stools). One sample per patient per 24-h period was allowed. The date and time of stool collection and the date of enrollment in the study were recorded. Each sample was assigned the next sequential study identification number, and patient confidentiality was maintained during all subsequent steps of the studies. Samples were either tested as received on the day shift or refrigerated for no more than 36 h prior to processing. Two 1-ml aliquots were collected and frozen for future testing (Vero cytotoxicity assay).
Culture methods.
Stool samples were plated and streaked for isolation on xylose lysine decarboxylase (XLD) and/or sorbitol MacConkey (SMAC) agar, and MacConkey broth was inoculated. Agar plates were examined after overnight incubation at 37°C, and non-sorbitol-fermenting colonies were verified to be E. coli by biochemical testing performed with the Vitek-2 system (BioMérieux, Inc., Durham, NC). The O157 serotype was determined by latex agglutination. MacConkey broth cultures were incubated for 18 to 24 h at 35°C and assayed for toxin (see below). Additionally, 85 previously tested fecal samples (contributed by Choong Park and Judy Daly from frozen [−70°C] sample libraries) were cultured as described above and screened for Stx's.
Culture sweep method.
At one center, Inova Fairfax Hospital (IFH), an additional 470 fresh stool specimens were prospectively screened for STEC by an alternate method (phase II). In that procedure, four to six sweeps of surface growth from SMAC agar plates that had been incubated overnight were collected on a rayon swab. The swabs were then screened by the OIA SHIGATOX method according to the manufacturer's directions for direct stool samples. For 200 of the colony sweep cultures, growth was also taken from XLD agar plates for comparison of Stx detection with XLD versus SMAC agar. In addition, 24 frozen stool specimens, previously identified as STEC culture positive, were thawed and cultured on SMAC agar and in MacConkey broth. The results obtained by the OIA detection method were compared to those obtained from overnight MacConkey broth cultures tested by the Premier EHEC EIA method.
Cross-reactivity studies.
A selection of organisms commonly isolated from feces, taken from a library of frozen clinical isolates previously identified mostly with the Vitek-2 gram-negative system, was tested by the OIA with the colony sweep method (described above) after growth on blood agar plates to assess the potential for cross-reactivity. These organisms included Acinetobacter, Aeromonas, Campylobacter jejuni, Candida, Citrobacter, Enterococcus, Stx-negative Escherichia coli, Enterobacter, Klebsiella, Morganella, Providencia, Proteus, Pseudomonas, Salmonella, Shigella, Serratia, Staphylococcus, Vibrio parahaemolyticus, Vibrio vulnificus, and Yersinia enterocolitica isolates.
Stx detection.
Fresh or frozen and thawed fecal samples were screened directly by OIA or EIA according to the manufacturer's kit instructions (SHIGATOX or Premier EHEC, respectively). Participating technologists received on-site training in interpretation of the OIA by an Inverness Medical representative (Fig. 1). An enrichment step in which fecal samples were incubated overnight in MacConkey agar was also done. Although not recommended by either kit manufacturer, a “blind” sweep of culture growth was also tested for toxin detection as previously described (15). Direct fecal samples or enrichment broth culture samples that were positive by either toxin assay or by SMAC agar screening were frozen and shipped with dry ice to the Uniformed Services University of the Health Sciences for testing in a blinded fashion by the Vero cell cytotoxicity assay as described by Gentry and Dalrymple (7). Samples were scored positive by the cytotoxicity assay if either the enrichment broth or the direct specimen yielded ≥500 50% cytotoxic doses per ml of sample on Vero cells. Sensitivity was calculated as the number of true positives divided by the sum of true positives plus false negatives and expressed as a percentage. Specificity was determined as the number of true negatives divided by the sum of false positives and true negatives and expressed as a percentage. The statistical significance of differences in sensitivity and specificity values between the two assay methods was determined by chi-square analysis.
FIG. 1.
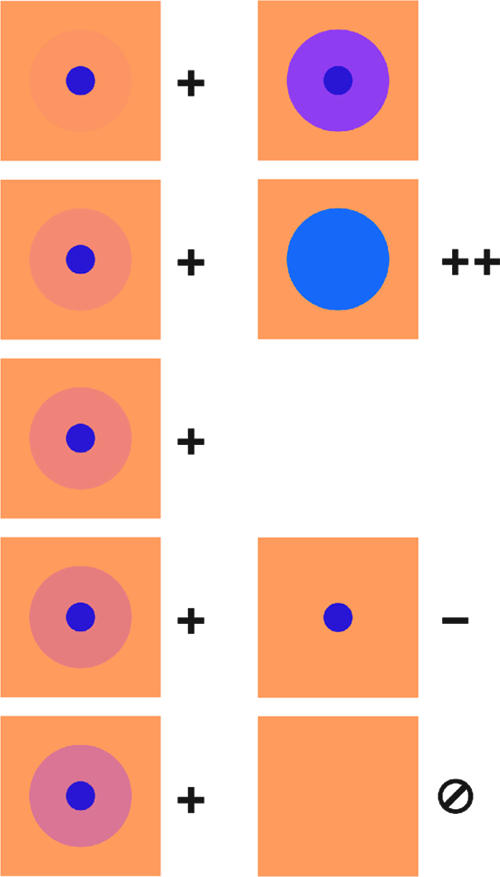
Graphic representation of the OIA SHIGATOX test interpretation, courtesy of Inverness Medical Professional Diagnostics. The optical chip surface appears gold, and any change in refraction that yields a blue to purple color change is scored as positive. Symbols: +, positive;, negative, weak positive; ‡, strong positive, as shown in both panels at upper right.
RESULTS
Phase I studies.
In the prospective screening of fecal samples (Table 1), the OIA Stx detection kit was more sensitive than the Premier EHEC kit (sensitivities, 96.8% and 83.9%, respectively [P < 0.05]), with no statistical difference in specificity. Four false-positive results were obtained by the OIA method on fecal samples that were noted to have a very mucoid consistency. We considered that the presence of mucus in such specimens may alter the refractivity of the OIA reaction surface. Although we did not modify the study protocol to retest these samples, we speculate that the presence of mucus may warrant more-stringent washing of the OIA kit detection surface or dilution of the stool sample (see below) to avoid false positives.
TABLE 1.
Detection of Shiga toxins in fresh stool specimens and corresponding broth enrichment cultures by prospective screening with the BioStar OIA SHIGATOX and Premier EHEC kitsa
| Test | No. of results
|
Sensitivity (%) | Specificity (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| True positive | True negative | False positive | False negative | |||||||||
| Direct stool | ||||||||||||
| OIA | 30 | 707 | 4 | 1 | 96.8b | 99.4 | ||||||
| EIA | 26 | 710 | 1 | 5 | 83.9b | 99.8 | ||||||
| Broth enrichment | ||||||||||||
| OIA | 31 | 711 | 0 | 0 | 100 | 100 | ||||||
| EIA | 30 | 711 | 0 | 1 | 96.8 | 100 | ||||||
A total of 742 specimens were tested. Positive reactions were confirmed by a Vero cytotoxicity assay.
Significantly different from the result by the other method (P < 0.05).
As anticipated, enrichment of stool samples by broth culture improved the detection of Stx(s) by both methods (sensitivities, 100% for the OIA and 96.8% for the EIA [not significantly different]). Broth enrichment also corresponded to a reduction in the number of false-positive OIA results from those obtained for direct samples, an observation that may be the result of dilution in broth of the mucus in the sample.
Technologists at two of the clinical sites also retrospectively tested 85 frozen archived fecal specimens that had previously been screened for Stx(s) by EIA. Thawed samples were tested directly and cultured in enrichment broth (Table 2); however, 11 previously frozen samples failed to grow in enrichment broth. The sensitivities and specificities of the two methods correlated well when tested on the thawed samples, and no false positives were encountered by either method (100% specificity for both methods). The sensitivities of both assays on frozen samples were somewhat lower than those observed with fresh samples. We considered that the Shiga toxins may have deteriorated somewhat after freezing and thawing. Thus, a reduction in toxin concentration may have occurred and resulted in false negatives by both the EIA and OIA direct methods compared to the extremely sensitive Vero cytotoxicity assay for Shiga toxins. Freezing and thawing might also have adversely affected bacterial viability and contributed to reduced sensitivity of toxin detection in enrichment broth cultures from frozen specimens, a hypothesis supported by the failure of some samples previously reported to contain STEC to grow in enrichment cultures.
TABLE 2.
Detection of Shiga toxins in frozen stool specimens tested directly after thawing and following broth enrichment with the BioStar OIA SHIGATOX and Premier EHEC kitsa
| Test | No. of results
|
Sensitivity (%) | Specificity (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| True positive | True negative | False positive | False negative | |||||||||
| Direct stool | ||||||||||||
| OIA | 46 | 33 | 0 | 6 | 88.5 | 100 | ||||||
| EIA | 44 | 33 | 0 | 8 | 84.6 | 100 | ||||||
| Broth enrichmentb | ||||||||||||
| OIA | 44 | 24 | 0 | 6 | 88.0 | 100 | ||||||
| EIA | 43 | 24 | 0 | 7 | 86.0 | 100 | ||||||
A total of 85 samples were tested. Positive results were confirmed by the Vero cytotoxicity assay.
Eleven previously frozen samples failed to grow when subcultured in MacConkey broth for enrichment.
Phase II study.
In one case study, swabs of fecal flora grown overnight on solid agar were reported to provide an alternative method to overnight broth enrichment and detection of STECs when used with an investigational immunochromatographic handheld Stx detection kit similar in design to the OIA kit (15). Here we sought to evaluate this colony sweep method in conjunction with the rapid OIA kit. As a standard we chose to use the well-accepted method of overnight broth enrichment assayed with the Premier EHEC kit (shown in this report to provide comparable sensitivity to the OIA method following broth enrichment). OIA results on swabs from conventionally plated fresh or frozen fecal samples were compared with EIA results on the same specimens following growth for enrichment in MacConkey broth (Table 3). As before, we noticed a slight drop in the sensitivity of the EIA after sample freezing with the broth enrichment method; however, the sensitivity and specificity of the colony sweep OIA were both 100% compared to conventional culture and/or direct fecal screening by EIA. Growth derived from XLD agar or SMAC agar gave equivalent results, while none of the colony sweeps from pure cultures of non-Shiga-toxigenic organisms reacted in the OIA. Together these findings suggest that screening of growth from routinely plated fecal cultures may serve as a reliable backup STEC screening method.
TABLE 3.
Detection of Shiga toxins by OIA following agar enrichment (colony sweep) and by EIA following broth enrichmenta
| Test | No. of results
|
Sensitivity (%) | Specificity (%) | |||
|---|---|---|---|---|---|---|
| True positive | True negative | False positive | False negative | |||
| OIA colony sweep | 42 | 452 | 0 | 0 | 100* | 100 |
| EIA broth enrichment | 39 | 452 | 0 | 3 | 92.9* | 100 |
Phase II study. A total of 494 samples were tested, including 470 fresh samples tested prospectively and 24 frozen samples previously identified as STEC positive by culture. True and false reactions were determined by comparison with culture results for recovery of STEC from stool. *, P < 0.09.
In Table 4, some characteristics of the 27 STEC-positive individuals identified in the prospective patient screening at IFH are summarized. The symptom of blood in the stool was observed with similar frequencies in O157 and non-O157 STEC infections (73.7% and 75%, respectively), and approximately 25% of the STEC-infected patients did not exhibit this symptom. No cases of HUS occurred among this population, and fewer than half of these patients were under the age of 18 years.
TABLE 4.
Selected characteristics of the STEC-positive patients who were identified during phases I and II of the prospective Shiga toxin screening at IFH
| Parameter | Value for the following group of confirmed STEC-positive patients:
|
||
|---|---|---|---|
| All | Confirmed O157:H7 | Confirmed non-O157:H7 | |
| No. of patients | 27 | 19 | 8 |
| % of all positive patients | 100 | 70 | 30 |
| Blood in stool sample (% [no./total]) | 74.1 (20/27) | 73.7 (14/19) | 75 (6/8) |
| Age, <18 yr (% [no./total]) | 44.4 (12/27) | 47.4 (9/19) | 37.5 (3/8) |
| No. with HUS | 0 | 0 | 0 |
DISCUSSION
Our evaluation of the OIA SHIGATOX detection method showed very good correlation with the results obtained by the well-accepted Premier EHEC method. In addition, we observed that the OIA method was more sensitive than the EIA method, with the added advantage of requiring less than 20 min to perform compared to the 2.5 h required to complete the EIA procedure. The OIA method was easy to use and interpret, and as a self-contained handheld device, the SHIGATOX method is suitable for point-of-care testing. The use of such rapid Stx detection strategies for the identification of Stx-producing organisms in patients with diarrhea is an extremely valuable tool to alert the physician to avoid antibiotics, antimotility agents, narcotics, and nonsteroidal anti-inflammatory drugs, which can increase the risk of HUS (14). In addition, therapies such as humanized monoclonal antibodies that can be passively administered to protect against Shiga toxins are in development (5, 13). Once these therapies are available, at-risk patients who have been identified by rapid toxin detection methods can be treated promptly, since the efficacy of such interventions is likely to be proportional to the speed with which therapy is administered.
Another important observation from these studies is the efficacy of the OIA method for the direct screening of colony sweeps from conventionally plated stool cultures. Although not as rapid as direct fecal screening, the OIA is comparable to the broth enrichment technique and provides an additional method for screening cultures that have already been plated, perhaps at off-site satellite laboratory facilities. The colony sweep procedure would also be very useful for identification of isolates from a toxin-positive stool that produces Shiga toxins, particularly among those that ferment sorbitol. It should be emphasized that although Stx detection has immediate implications for patient care, this method does not obviate the need for the isolation and identification of Stx-producing organisms. The importance of reporting and profiling such isolates is to identify non-O157 STEC strains that may also be responsible for outbreaks of food- or waterborne disease among the general public (2).
Finally, the use of toxin detection methods expands our recognition of the scope of non-O157 STEC in diarrheal disease. Data from the past 10 years at IFH, where all diarrheal stools are screened with the Premier EHEC kit, revealed that 35% of STEC-positive patients had non-O157 serotypes and 30% had nonbloody samples (11; also unpublished data). In fact, screening for toxin production showed that STEC represented the second most frequently diagnosed enteric pathogen, behind Salmonella enterica, at IFH. Similarly, in this study, one third-of the STEC strains identified were non-O157 isolates. Routine screening for O157 and non-O157 STEC strains in patients regardless of age and without limitation to bloody stools may increase the detection of STEC infections overall and help to control the spread of these potentially life-threatening infections.
Acknowledgments
We gratefully acknowledge the technical support provided by Jonelle McKey, Deidre Jarrett, and Jennifer Twineham at Children's Healthcare of Atlanta, Atlanta, GA, and by E. Kent Korgenski at Primary Children's Medical Center, Salt Lake City, UT. Statistical analysis of the data was directed by Cara Olsen at the Uniformed Services University.
Thanks also to Inverness Medical Professional Diagnostics for providing the OIA and EIA kits and funding for the cytotoxicity assays. NIH grant 2 RO1 1 A120148-23 supported research and Shiga toxin purification at the Uniformed Services University.
Footnotes
Published ahead of print on 1 August 2007.
REFERENCES
- 1.Andreoli, S. P., H. Trachtman, D. W. Acheson, R. L. Siegler, and T. G. Obrig. 2002. Hemolytic uremic syndrome: epidemiology, pathophysiology, and therapy. Pediatr. Nephrol. 17:293-298. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. 2006. Importance of culture confirmation of shiga toxin-producing Escherichia coli infection as illustrated by outbreaks of gastroenteritis—New York and North Carolina, 2005. Morb. Mortal. Wkly. Rep. 55:1042-1045. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. 2006. Ongoing multistate outbreak of Escherichia coli serotype O157:H7 infections associated with consumption of fresh spinach—United States, September 2006. Morb. Mortal. Wkly. Rep. 55:1045-1046. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. 2007. Laboratory-confirmed non-O157 Shiga toxin-producing Escherichia coli—Connecticut, 2000-2005. Morb. Mortal. Wkly. Rep. 56:29-31. [PubMed] [Google Scholar]
- 5.Dowling, T. C., P. A. Chavaillaz, D. G. Young, A. Melton-Celsa, A. O'Brien, C. Thuning-Roberson, R. Edelman, and C. O. Tacket. 2005. Phase 1 safety and pharmacokinetic study of chimeric murine-human monoclonal antibody cαStx2 administered intravenously to healthy adult volunteers. Antimicrob. Agents Chemother. 49:1808-1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Farmer, J. J., III, and B. R. Davis. 1985. H7 antiserum-sorbitol fermentation medium: a single tube screening medium for detecting Escherichia coli O157:H7 associated with hemorrhagic colitis. J. Clin. Microbiol. 22:620-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gentry, M. K., and J. M. Dalrymple. 1980. Quantitative microtiter cytotoxicity assay for Shigella toxin. J. Clin. Microbiol. 12:361-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson, K. E., C. M. Thorpe, and C. L. Sears. 2006. The emerging clinical importance of non-O157 Shiga toxin-producing Escherichia coli. Clin. Infect. Dis. 43:1587-1595. [DOI] [PubMed] [Google Scholar]
- 9.Kehl, K. S., P. Havens, C. E. Behnke, and D. W. Acheson. 1997. Evaluation of the premier EHEC assay for detection of Shiga toxin-producing Escherichia coli. J. Clin. Microbiol. 35:2051-2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mead, P. S., L. Slutsker, V. Dietz, L. F. McCaig, J. S. Bresee, C. Shapiro, P. M. Griffin, and R. V. Tauxe. 1999. Food-related illness and death in the United States. Emerg. Infect. Dis. 5:607-625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park, C. H., K. M. Gates, N. M. Vandel, and D. L. Hixon. 1996. Isolation of Shiga-like toxin producing Escherichia coli (O157 and non-O157) in a community hospital. Diagn. Microbiol. Infect. Dis. 26:69-72. [DOI] [PubMed] [Google Scholar]
- 12.Rangel, J. M., P. H. Sparling, C. Crowe, P. M. Griffin, and D. L. Swerdlow. 2005. Epidemiology of Escherichia coli O157:H7 outbreaks, United States, 1982-2002. Emerg. Infect. Dis. 11:603-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sheoran, A. S., S. Chapman-Bonofiglio, B. R. Harvey, J. Mukherjee, G. Georgiou, A. Donohue-Rolfe, and S. Tzipori. 2005. Human antibody against shiga toxin 2 administered to piglets after the onset of diarrhea due to Escherichia coli O157:H7 prevents fatal systemic complications. Infect. Immun. 73:4607-4613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tarr, P. I., C. A. Gordon, and W. L. Chandler. 2005. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet 365:1073-1086. [DOI] [PubMed] [Google Scholar]
- 15.Teel, L. D., B. R. Steinberg, N. E. Aronson, and A. D. O'Brien. 2003. Shiga toxin-producing Escherichia coli-associated kidney failure in a 40-year-old patient and late diagnosis by novel bacteriologic and toxin detection methods. J. Clin. Microbiol. 41:3438-3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Voetsch, A. C., F. J. Angulo, T. Rabatsky-Ehr, S. Shallow, M. Cassidy, S. M. Thomas, E. Swanson, S. M. Zansky, M. A. Hawkins, T. F. Jones, P. J. Shillam, T. J. Van Gilder, J. G. Wells, and P. M. Griffin. 2004. Laboratory practices for stool-specimen culture for bacterial pathogens, including Escherichia coli O157:H7, in the FoodNet sites, 1995-2000. Clin. Infect. Dis. 38(Suppl. 3):S190-S197. [DOI] [PubMed] [Google Scholar]


