Abstract
The rescue of influenza viruses by reverse genetics has been described only for the influenza A and B viruses. Based on a similar approach, we developed a reverse-genetics system that allows the production of influenza C viruses entirely from cloned cDNA. The complete sequences of the 3′ and 5′ noncoding regions of type C influenza virus C/Johannesburg/1/66 necessary for the cloning of the cDNA were determined for the seven genomic segments. Human embryonic kidney cells (293T) were transfected simultaneously with seven plasmids that direct the synthesis of each of the seven viral RNA segments of the C/JHB/1/66 virus under the control of the human RNA polymerase I promoter and with four plasmids encoding the viral nucleoprotein and the PB2, PB1, and P3 proteins of the viral polymerase complex. This strategy yielded between 103 and 104 PFU of virus per ml of supernatant at 8 to 10 days posttransfection. Additional viruses with substitutions introduced in the hemagglutinin-esterase-fusion protein were successfully produced by this method, and their growth phenotype was evaluated. This efficient system, which does not require helper virus infection, should be useful in viral mutagenesis studies and for generation of expression vectors from type C influenza virus.
The influenza C virus, a member of the Orthomyxoviridae family, was first isolated in 1947 and is a common cause of mild upper respiratory tract illness. Seroepidemiology studies indicate that this virus is widely distributed around the world and that the majority of humans acquire antibodies against the virus early in life (30). The disease caused by it tends to take an unapparent or very mild course, so that the virus is only exceptionally isolated (29). Furthermore, analysis of the genome sequence of type C influenza viruses isolated over time suggested that reassortment between two different type C influenza viruses occurs frequently in nature (4, 31).
It has long been believed that unlike the case for influenza A virus, humans are the only natural host for influenza C viruses (1). Guo et al. (13) succeeded in isolating a number of influenza C viruses from abattoir pigs in Beijing, China, and demonstrated pig-to-pig transmission of the virus upon experimental infection. The presence of specific antibodies was also demonstrated in the serum of pigs in Japan and Great Britain (3, 55). Furthermore, human influenza C virus isolates were found to be closely related to pig isolates, suggesting that interspecies transmission of influenza C virus between humans and pigs has occurred in nature (24). Influenza C virus-specific antibodies were also detected in dogs (26, 27, 39), but detection or isolation of the virus from this animal species has not been documented, although experimental infection resulted in clinical symptoms and viral replication (38). Consequently, influenza C viruses are not restricted to humans, but the potential role of pigs or dogs as an animal reservoir for human influenza C virus remains to be elucidated.
In contrast with those of type A and B influenza viruses, the type C influenza virus genome consists of only seven segments of single-stranded RNA of negative polarity, which are numbered based on decreasing lengths, i.e., the PB2, PB1, P3, HEF, NP, M, and NS segments, respectively (reviewed in reference 42). As for type A and B influenza viruses, each viral RNA (vRNA) molecule is associated with the nucleoprotein (NP) and a heterotrimeric polymerase complex (P) that consists of the three polymerase subunits, PB2, PB1, and P3, thus forming the ribonucleoproteins (RNP). Because the minimal replication unit is formed by the RNPs, the generation of virus from cloned cDNAs requires the presence of the seven vRNAs, as well as that of the four viral proteins, PB2, PB1, P3, and NP, involved in the transcription and replication of the viral RNA (6). Reverse-genetics systems that allow the production of infectious virus from cloned cDNA have already been developed for the type A (11, 35) and B (20, 23) influenza viruses and for the Thogoto virus, a tick-transmitted orthomyxovirus (54). Several strategies have been designed. The primary method was based on the transfection of 12 plasmids: the 8 full-length cDNAs derived from the viral genome were cloned into a vRNA expression plasmid between the human RNA polymerase I promoter and the mouse RNA polymerase I terminator, and the coding regions of the nucleoprotein and of the PB2, PB1, and PA viral polymerase proteins were cloned into a protein expression plasmid to provide the four viral proteins required for transcription/replication of the vRNAs (11, 23, 35). The second strategy was based on the use of bidirectional RNA polymerase I/II plasmids to clone the full-length cDNAs derived from each of the viral genomic segments to drive, after transfection, both the expression of the proteins and the synthesis of each of the negative-sense vRNAs (20, 21). More recently, Neumann et al. (34) reduced the number of plasmids required for virus generation to six, five, three, and even one plasmid. Finally, a third recently published strategy is based on the use of the T7 RNA polymerase promoter, thus allowing the use of a variety of cell lines (9).
To date, no plasmid-based system for the rescue of influenza C virus has been reported. Here we describe a reverse-genetics system for influenza C virus based on the C/Johannesburg/1/66 (C/JHB/1/66) virus strain. Having completed the sequence of the 3′ and 5′ noncoding (NC) regions of the seven genomic segments of this strain, we chose to base our type C influenza virus reverse-genetics system on the primary method described above for influenza virus types A and B. Plasmids that direct expression of the seven vRNAs under the control of the human RNA polymerase I promoter were thus generated and used together with the four plasmids that direct the expression of the NP, PB2, PB1, and P3 proteins previously described (6).
Having set up an efficient reverse-genetics system to rescue wild-type influenza C virus, we tested its usefulness by engineering influenza C viruses mutated in the hemagglutinin-esterase-fusion protein (HEF). The spike glycoproteins of the lipid-enveloped orthomyxoviruses have three functions: to recognize the receptor on the cell surface, to mediate viral fusion, and to destroy the receptor. In type A and B influenza viruses, the first two activities are mediated by the hemagglutinin (HA) and the third by a second glycoprotein, the neuraminidase (42). In the case of type C influenza virus, a single glycoprotein, the HEF protein, possesses all three functions (16). The receptor recognized by HEF differs from that used by the type A and B influenza virus HA by the addition of an acetyl group at the 9-O position of the glycerol side chain of the sialic acid. More precisely, the influenza C virus utilizes the 9-O-acetyl-N-acetylneuraminic acid (Neu5,9Ac2) for attachment to the cell surface (19, 46). Because of the lack of Neu5,9Ac2 in the cell surface receptors, Madin-Darby canine kidney II cells (MDCK II cells), which are commonly used for type A and B influenza viruses, are resistant to infection by type C influenza virus. However, their resistance can be overcome by coating the cells with bovine brain gangliosides (BBG), which naturally contain Neu5,9Ac2 (17). The fusion activity of HEF is dependent on the proteolytic cleavage of a precursor (HEF0) into HEF1 and HEF2, the largest and smallest proteolytic cleavage products, respectively (15, 37), and requires activation at a low pH upon internalization of the viral particle through the endosome pathway. Finally, the acetylesterase activity of HEF inactivates the virus receptor by releasing the O-acetyl residues from C-9 of Neu5,9Ac2 (18).
Based on published data on residues that could be critical in HEF processing or function (14, 44, 45, 50), we chose to focus on positions 284 and 465 of the HEF protein (amino acid numbering). Indeed, it has been suggested that position 284 of HEF could be involved in receptor binding activity (50), whereas position 465 is located in the peptide fusion domain of HEF (12). Single and double mutants could be rescued, and their phenotype was further analyzed and compared to that of the wild-type virus.
MATERIALS AND METHODS
Cells and viruses.
293T human embryonic kidney cells and MDCK II cells were maintained in Dulbecco's modified Eagle medium (DMEM) supplemented with 10% and 5% fetal calf serum (FCS), respectively. The MDCK cell line was isolated in 1958, and two sublines have been described: MDCK I cells, which derived from an early passage and are susceptible to type C influenza virus, and MDCK II cells, which predominated in later passages and are resistant to type C influenza virus because they lack Neu5,9Ac2 (56).
Human skin melanoma cells (SK 93/2) were kindly provided by Frade (Saint Antoine Hospital, Paris, France) and were maintained in RPMI supplemented with 5% FCS (40, 43).
All cells were maintained at 37°C in 5% CO2 before transfection or infection.
Influenza C virus C/JHB/1/66, considered the reference strain, was propagated in 10-day-old embryonated eggs.
Determination of 3′ and 5′end NC sequences of genomic RNA segments.
Viral genomic RNA was extracted from C/JHB/1/66 using the Trizol reagent (Gibco-BRL). The 3′ and 5′ NC sequence were determined as previously described (7) using an anchored (dT)14 oligonucleotide and primers specific for the coding sequences of each of the seven type C vRNA segments for reverse transcription and amplification. After purification, the PCR products were sequenced with internal oligonucleotides. The exact sequences of the primers used for amplification and sequencing of the 3′ and 5′ NC sequences of each segment are available from the authors upon request.
Cloning of plasmids.
Plasmids pHMG-PB2, -PB1, -P3, and -NP, which direct expression of the PB2, PB1, P3, and NP proteins of the influenza C virus under the control of the mouse hydroxymethylglutaryl-coenzyme A reductase promoter, have been described previously (6).
To generate plasmids that direct the synthesis of the seven vRNA segments from C/JHB/1/66 virus, PCR products corresponding to each of the full-length segments were cloned in plasmid vector pPR, in which BbsI restriction sites are flanked by the promoter of the human RNA polymerase I and the hepatitis delta ribozyme sequence (6). For cloning of the cDNA corresponding to the PB2, P3, and NP segments, sequences were amplified from the pHMG-PB2, -P3, and -NP plasmids, respectively, using High Fidelity Enzyme Taq polymerase (Roche) and primers containing the total 3′ and the far-end 5′ NC sequences for PB2 and P3 and primers containing the total 3′ and partial 5′ NC sequences for NP. For the cloning of cDNA corresponding to the four other segments, C/JHB/1/66 RNA was reverse transcribed with 300 nM of the C/uni1 primer, 5′-AGC AGA AGC AG, in the presence of 0.4 U/μl of avian myeloblastosis virus reverse transcriptase (Promega) at 37°C. The cDNAs were then amplified by PCR using the High Fidelity Enzyme Taq polymerase for the HEF, M, and NS segments or with the pfx platinium Taq polymerase (Invitrogen) for the PB1 segment. Specifics primers containing the 3′ and 5′ NC sequences were used. For PB1 and HEF, a two-step strategy was necessary. For both segments, two overlapping PCR products corresponding to both halves of the segment were produced. These were then used as templates for a second PCR using the outer primers to generate the full-length cDNA. The 5′ end sequences of all primers contained BsmBI sites. The purified PCR products were then digested with BsmBI and cloned into the BbsI sites of the pPR vector. The sequences of the primers will be provided upon request. The resulting vRNA expression plasmids were named pC/PR/X/JHB, where X corresponds to the name of each segment. To ensure that the genes were free of nonsilent mutations, several plasmids were sequenced for each constructions.
Mutations in the HEF gene sequence around nucleotides (nt) 872 and 1414, resulting in Thr-to-Ile and Thr-to-Ala substitutions at residues 284 and 465, respectively, were introduced into the pC/PR/HEF/JHB plasmid using the Quikchange II site-directed mutagenesis kit (Stratagene) according to the manufacturer's instructions and verified by sequencing. The double mutant was obtained by subcloning. All plasmids were sequenced using a Big Dye terminator sequencing kit and an automated sequencer (Perkin-Elmer).
Transfection and rescue of viruses.
293T cells (6 × 105) seeded on 35 mm poly-d-lysine plates (Greiner bio-one) in DMEM supplemented with 10% FCS were transfected with the four protein expression plasmids, allowing the expression of the NP and the polymerase proteins, and the seven vRNA expression plasmids, allowing the synthesis of the seven vRNA templates, using 0.5 μg of each plasmid and 10 μl of FUGENE 6 (Roche) according to the manufacturer's instructions. Briefly, the DNA and the transfection reagent were mixed, incubated at room temperature for 15 min, and then added to the cells and incubated at 33°C. Sixteen hours later, the DNA transfection reagent was removed and the cells were washed twice in DMEM and, after addition of 4 ml of DMEM containing 0.25 μg/ml l-1-tosylamido-2-phenyl chloromethyl ketone (TPCK)-trypsin (Worthington), incubated at 33°C. Eight to 10 days after transfection, supernatants were collected and the viruses were titrated by plaque assay on MDCK II cells.
Plaque assay.
MDCK II cells were seeded in six-well tissue culture plates (106 cells per well). At 100% confluence, cells were washed twice with phosphate-buffered saline (PBS) and incubated for at least 45 min at 37°C with 0.4 ml of a solution of BBG (Sigma) at 0.2 mg/ml in PBS. Then, cells were washed twice in PBS and incubated with 0.4 ml of each serial dilution of the virus for 30 min at room temperature. Finally, each well was covered with 4 ml of a 1× agar overlay mixture (final concentration, 1% SeaKem GTG agarose [Tebu], 1× DMEM [Eurobio], 1 μg/ml TPCK-trypsin). Plates were then incubated at 33°C with 5% CO2 for 4 to 5 days: once the plaques were clearly visible, the agar overlay was carefully removed and the cells stained with 0.3% crystal violet solution and 10% formaldehyde. Titers were expressed as PFU/ml.
Virus amplification and growth kinetics.
SK 93/2 cells were infected with the transfection supernatant at a multiplicity of infection (MOI) of 10−3 in RPMI containing 0.25 μg/ml of TPCK-trypsin at 33°C with 5% CO2. Five days after incubation, the supernatant was titrated by plaque assay on MDCK II cells. Growth kinetics and analysis of the virus phenotype were performed in duplicate and triplicate, respectively, with viruses amplified once on SK 93/2 cells. MDCK II cells incubated with or without BBG were infected at an MOI of 10−3 in DMEM containing 0.25 or 5 μg/ml of TPCK-trypsin and incubated at 33°C with 5% CO2. The supernatants were collected each day for determining the kinetics or 4 days after infection for virus phenotype analysis. The virus titers were determined by plaque assay as described above.
RNA isolation and RT-PCR.
To analyze mutations on the HEF protein, viral RNA was extracted from infectious culture supernatants (140 μl) by using the QIAamp viral RNA kit (QIAGEN, Inc., Valencia, CA) according to the manufacturer's instructions. The RNA was eluted in 60 μl of buffer and stored at −80°C. The rescued influenza C viruses were characterized by reverse transcription-PCR (RT-PCR). For synthesis of cDNA, viral RNA (5 μl) was reverse transcribed with avian myeloblastosis virus reverse transcriptase in the presence of primer C/uni1 (0.5 μM). A nested PCR was performed to amplify an 875-nt amplicon in the HEF gene using specific primers (sequences of the four primers are available upon request). The purified PCR products were analyzed by 1% agarose gel electrophoresis before and after digestion with EcoRV or NgoMIV.
Nucleotide sequence accession numbers.
The GenBank/EMBL/DDJ accession numbers are AF170573, AF170574, AF170575, and AF170576 for the NP, P3, PB1, and PB2 segments, respectively, and AM410041, AM410042, and AM410043 for the HEF, M, and NS segments, respectively.
RESULTS
Complete sequences of 3′ and 5′ NC regions of genomic RNA segments from influenza virus C/Johannesburg/1/66.
As a first step in generating a reverse-genetics system for influenza C virus, we determined the complete sequences of the 3′ and 5′ NC regions of the seven segments of the virus C/JHB/1/66/. Indeed, very few complete 3′ and 5′ NC sequences are available in the GenBank database and not for all segments of the same virus. In the early 1980s, only partial nucleotide sequences of the 3′ and 5′ NC regions were determined for the seven genomic segments of C/JHB/1/66 virus by Desselberger et al. (8). The only complete NC sequences of C/JHB/1/66 in the databases were those of the HEF segment (accession numbers M17868 and AY880247) (14). In 1984, Clern-van Haaster and Meier-Ewert (5) also published partial 3′ NC sequences for two other type C virus isolates. Our sequences showed that at the 3′ end, the first 11 nt as well as nt 14 were conserved for the seven segments of C/JHB/1/66. Similarly, at the 5′ end, the first 12 nt and nt 15 were found to be conserved among the seven segments except for the NS segment, for which the U residue at nt 6 was replaced by a G. This was already described for the 5′ end of the NS segment of the C/California/78 virus (accession number M10087).
Cloning of cDNAs of the seven vRNA segments of C/JHB/1/66 influenza virus.
To generate the vRNA expression plasmids, the cDNAs corresponding to the seven full-length genomic segments of influenza C virus C/JHB/1/66 were cloned as described in Materials and Methods.
The sequences of the different clones were then compared with those available in the GenBank database, including our own previous sequences (6). No difference in the nucleotide sequence was found for the PB2, PB1, P3, and NP segments. One nucleotide difference was found for the M segment compared with the sequence available in the database (accession number AB000604), but this mutation was silent.
Out of the five nucleotide differences found between our sequence and previously published sequences of HEF of C/JHB/1/66 (14), only position 1414 resulted in a Thr-to-Ala substitution at position 465.
For the NS segment, we confirmed the observation made by Marschall et al. (28) and Alamgir et al. (2): i.e., the presence of an additional G residue at position 701 compared with the sequence of C/JHB/1/66 published in 1986 (accession number D00031). Eleven other differences were found with that 1986 sequence, most of them silent (data not shown). When comparing our C/JHB/1/66 NS sequence with that of C/JHB/4/67 published more recently by Alamgir (2), six nucleotide differences were found, three of which were nonsilent mutations that resulted in four amino acid substitutions, two in NS1 (amino acids [aa] 74 and 228) and two in NS2 (aa 124 and 144).
Rescue of infectious influenza C virus from cloned cDNAs.
The 293T cell line is very easily transfectable but lowly adherent and extremely sensitive to the concentration of trypsin which is required for the cleavage of the HEF glycoprotein (14). We therefore cultured 293T cells on poly-lysine plates to improve the adhesion of the cells and limit their sensitivity to trypsin. A concentration of TPCK-trypsin of 0.25 μg/ml was found to be optimal to maintain the 293T cell adherence and to obtain viral titers up to 105 to 106 PFU/ml after an infection at an MOI of 10−3 with influenza C virus (data not shown). Furthermore, we observed that the 293T cells had to be 70 to 80% confluent before transfection, and thus, we decided to use all of these conditions to build our reverse-genetics system for influenza C virus.
To produce infectious influenza C virus entirely from cloned cDNAs, the seven plasmids that direct the synthesis of each of the full-length viral RNAs were transfected into 293T cells along with the expression plasmids that encode the three polymerase subunits and NP protein.
For three representative experiments, we could detect between 103 and 104 PFU/ml of rescued virus in the supernatant of the transfected cells at 8 or 10 days after transfection (Table 1). Upon amplification on the permissive cell line SK 93/2, titers of 105 to 106 PFU/ml were reached. Similarly, the virus was readily amplified on embryonated eggs to titers of 109 PFU/ml. Furthermore, the virus was successfully recovered for five consecutive passages on SK 93/2 cells (data not shown).
TABLE 1.
Generation of type C influenza viruses following plasmid transfection of 293T cells
| Virusa | Titer of virusb (PFU/ml)
|
||
|---|---|---|---|
| Expt 1 | Expt 2 | Expt 3 | |
| wt | 1.3 × 103 | 2.5 × 104 | 1.2 × 104 |
| 284 | 2.5 × 105 | 6 × 104 | |
| 465 | 1.5 × 103 | 2.25 × 104 | 1 × 104 |
| 284+465 | 7.5 × 104 | 105 | |
Rescued viruses: wt, wild-type-like; 284, 284 Ile mutant; 465, 465 Ala mutant; 284+465, 284 Ile and 465 Ala double mutant.
Titers from transfection supernatants as determined by plaque assay with MDCK II cells. For 284 and 284+465 viruses, only two experiments were performed.
For each transfection, an attempt without the HEF vRNA expression plasmid was performed as a negative control and no virus could be rescued (data not shown).
Generation of infectious influenza C viruses harboring mutations in the HEF gene.
To further validate our reverse-genetics procedure, we explored the possibility of engineering C/JHB/1/66 viruses with mutations in the HEF gene. In 1989, Szepanski et al. (51) obtained a mutant of C/JHB/1/66 able to grow on MDCK II cells in the presence of a high concentration of trypsin. A single mutation at nt 872 of the HEF segment, resulting in a Thr-to-Ile substitution at aa 284 of HEF, was thought to be responsible for this phenotype (50).
Based on Szepanski's work, we decided to generate a HEF 284 Ile mutant of C/JHB/1/66 (referred to as 284 virus) by reverse genetics and to test its phenotype. Along with the introduction into plasmid pC/PR/HEF/JHB of the desired nonsilent mutation at nt 872 of the HEF sequence, we also introduced a silent mutation at nt 870 to generate an EcoRV restriction site (Table 2).
TABLE 2.
Substitutions introduced into the HEF protein of C/JHB/1/66 and enzyme restriction strategy used to analyze the stability of the rescued mutants
| Virus description | Amino acid position | Amino acid | Nucleotide sequenceb | Restriction site | After digestionc |
|---|---|---|---|---|---|
| wta | 284 | Thr | GAC ACC | None | 875 |
| 465 | Thr | ACA GGA | None | 875 | |
| Mutants | 284 | Ile | GAT ATC | EcoRV | 694 + 181 |
| 465 | Ala | GCC GGC | NgoMIV | 727 + 148 |
Wild type.
Underlined, nucleotide codons coding for the indicated amino acid; in bold, nonsilent mutations; in italics, silent mutations introduced in the neighboring codons to design a restriction enzyme site.
Expected length(s) (nt) of fragment(s) produced after digestion of amplicons with the indicated restriction enzymes.
Based on the observation of a single difference at aa 465 between our sequence and the previously published (14) sequences of the C/JHB/1/66 HEF protein, we replaced the Thr codon found in our sequence with an Ala codon as described by Hanika et al. (14) (465 mutant) and also introduced a new restriction site at that position. For this purpose, two nonsilent (nt 1414 and 1416) nucleotide mutations and one silent (nt 1419) nucleotide mutation were introduced into the cDNA of plasmid pC/PR/HEF/JHB, resulting in the desired amino acid substitution and the creation of a NgoMIV restriction site (Table 2). Finally, a double mutant (284+465 mutant) was also constructed by subcloning to study whether these mutations have independent effects or not.
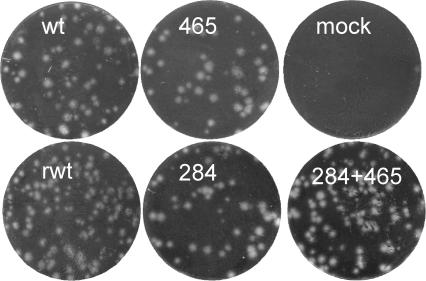
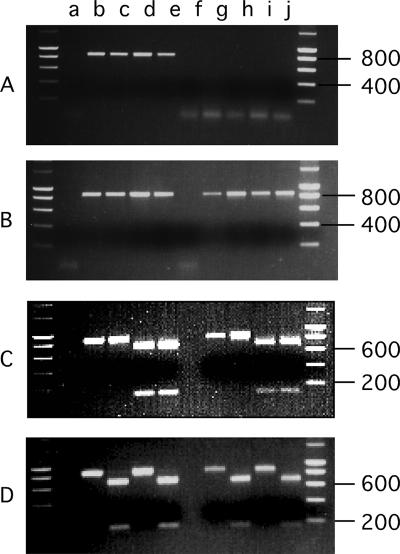
As for the rescued wild-type influenza C virus, the rescued mutant viruses were detected in the supernatant of transfected cells at 9 or 10 days posttransfection. They could easily be titrated by plaque assay, either directly (data not shown) or upon amplification in embryonated eggs and exhibited a plaque phenotype similar to that of the C/JHB/1/66 reference virus (Fig. 1). The titers obtained varied for each mutant but were in a range close to that of the rescued wild-type virus (Table 1). The rescued mutant viruses were then amplified on SK 93/2 cells at an MOI of 10−3 to reach titers between 105 and 107 PFU/ml at 5 days postinfection (data not shown). After five consecutive passages on SK 93/2 cells, the stability of the rescued mutant viruses was analyzed by RT-PCR followed by restriction enzyme digestion as described in Material and Methods. No amplification was observed for water and mock-infected cells supernatant used as negative controls (Fig. 2, lanes a and f, respectively). The expected 875-nt-long amplicon was observed when the vRNA expression plasmids for HEF and its mutants were used as templates for PCR (Fig. 2A, lanes b to e). With RNA from cells infected with rescued viruses, no amplification was observed without reverse transcription, thus ensuring the absence of plasmids carried over from transfected/infected cells (Fig. 2A, lanes g to j). After RT-PCR, the expected 875-nt-long amplicon was obtained (Fig. 2B, lanes g to j). Only the PCR products of the 284 and the 284+465 mutants were cleaved by EcoRV (Fig. 2C, lanes d, e, i, and j), as were those of the 465 and 284+465 mutants by NgoMIV (Fig. 2D, lanes c, e, h, and j). This confirmed that the rescued mutant viruses were stable after five passages on SK 93/2 cells. Furthermore, the nucleotide sequences were confirmed around amino acid positions 284 and 465 for the four rescued viruses (data not shown).
FIG. 1.
Plaque phenotype of the C/JHB/1/66 wild type (wt), rescued wild type (rwt), and mutant (465, 284, and 284+465) viruses. Viruses amplified on embryonated eggs were titrated by plaque assay on MDCK II cells pretreated with BBG as described in Materials and Methods.
FIG. 2.
Genetic stability of rescued HEF mutants. The HEF mutants of C/JHB/1/66 were engineered to carry genetic markers. For each rescued virus, vRNA was extracted from virus particles after five passages on SK 93/2 cells at a MOI of 10−3 (lanes g to j). Amplification by RT-PCR was performed with primers specific for the HEF sequences flanking the mutated region (B). Amplification was performed in parallel on water (lane a) and with samples derived from the mock-transfected cell supernatant (lane f) as negative controls and on the counterpart vRNA expression plasmids (lanes b to e) as positive controls. After purification, PCR products were digested with EcoRV (C) or NgoMIV (D). A control reaction was carried out in the absence of reverse transcriptase (A) in order to ensure that the amplification product was derived from vRNA and not from plasmid carried over from transfected cells. Lanes b and g, wt virus; lanes c and h, 465 Ala mutant; lanes d and i, 284 Ile mutant; lanes e and j, 284 Ile and 465 Ala double mutant.
Effect of the Thr 465 Ala and Thr 284 Ile mutations in the HEF protein.
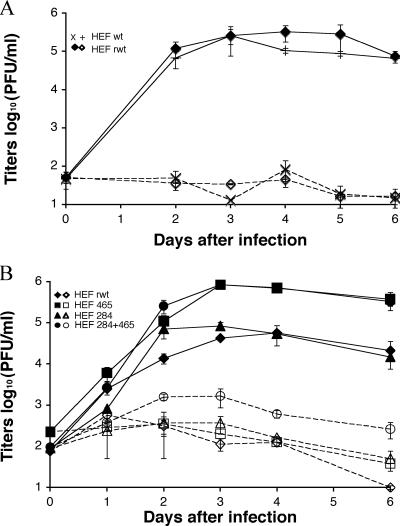
To analyze the effect of the substitutions at aa 284 and 465 in the HEF protein, determination of growth kinetics was performed with MDCK II cells treated or not with BBG in the presence of a low concentration of TPCK-trypsin (0.25 μg/ml).
As expected, treatment of the cells with BBG was found to be essential for infection by the wild type as well as rescued wild-type or mutant viruses (Fig. 3). On cells pretreated with BBG, the wild-type C/JHB/1/66 reference and rescued viruses showed similar growth (Fig. 3A). Furthermore, rescued wild-type and mutant viruses grew with essentially the same kinetics up to 2 days postinfection (Fig. 3B). Interestingly, for both viruses harboring an Ala at position 465 in HEF (465 and 284+465 viruses), the titers were 10-fold higher than those obtained for both viruses with a Thr 465 (rescued wild-type and 284 viruses) once the plateau phase was reached (after 3 days postinfection).
FIG. 3.
Growth kinetics of the wild type (A), rescued wild type (rwt) (A and B), or HEF mutant (B) virus. Confluent monolayers of BBG-treated (solid lines) or untreated (dotted lines) MDCK II cells were infected in duplicate in the presence of 0.25 μg/ml of TPCK-trypsin at an MOI of 10−3 with viruses amplified on embryonated eggs (A) or SK 93/2 cells (B). At the indicated time points, the supernatants were collected and virus titers were determined by plaque assay as described in Materials and Methods. Viruses: x, wild type; diamonds, rescued wild type; triangles, 284 Ile mutant; squares, 465 Ala mutant; circles, double mutant. Each result is expressed as the mean of the two infections and is representative of two independent experiments.
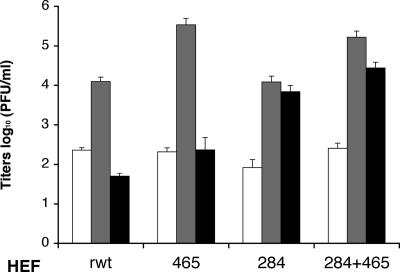
Since Szepanski et al. (50, 51) had shown that the Thr 284 Ile mutation enabled the growth of influenza C virus on untreated MDCK II cells in the presence of a high concentration of trypsin, we compared the ability of each of the four rescued viruses to grow on MDCK II cells without pretreatment with BBG and in the presence of a low (0.25 μg/ml) or high (5 μg/ml) concentration of TPCK-trypsin (51). As already mentioned, in the presence of a low concentration of TPCK-trypsin, pretreatment with BBG was necessary to allow infection by the four rescued viruses (Fig. 4). For the wild-type reference and rescued viruses no significant difference in titer was observed when using a low or high concentration of TPCK-trypsin (data not shown). In contrast, in the presence of a high concentration of TPCK-trypsin, titers obtained for both viruses harboring an Ile at position 284 in HEF (284 and 284+465 viruses) were 100-fold higher than those for their respective counterparts with a Thr at position 284 (rescued wild-type and 465 viruses) (Fig. 4). These results thus further demonstrated that the Thr 284 Ile substitution in the HEF is necessary and sufficient to enable influenza C virus to grow on MDCK II cells in the absence of BBG if a high concentration of trypsin is used. Furthermore, it could be noted that the two mutations introduced in the HEF proteins have independent effects on the growth of influenza C virus. On the whole, our results showed that the reverse-genetics system described provides an efficient means to perform site-directed mutagenesis of the HEF sequence of influenza C virus.
FIG. 4.
Trypsin phenotype of the rescued wild-type or HEF mutant virus. MDCK II cells were infected in triplicate at an MOI. of 10−3, with each of the four rescued viruses as indicated in three different conditions. MDCK II cells were either treated (gray bars) or not (open and black bars) by BBG before infection and, after infection, further incubated in the presence of 0.25 μg/ml (open and gray bars) or 5 μg/ml (black bars) of TPCK-trypsin. Four days after infection, the supernatants were harvested and virus titers were determined by plaque assay as described in Materials and Methods. Each result us expressed as the mean for the three infections and is representative of two independent experiments.
DISCUSSION
Reverse-genetics systems have been previously described only for the type A and B influenza viruses but not for type C. This may be due at least in part to the fact that the complete NC sequences for a given influenza C virus had not been determined and to difficulties related to the type of cells to use, the method of detecting and titrating the type C virus, and the delay before the appearance of rescued virions.
The first influenza virus reverse-genetics system described consisted in the rescue of a vRNA segment produced from recombinant plasmid DNA in the presence of a helper virus (10, 25). These experiments paved the way for the rescue of type A influenza virus entirely from cloned cDNA. This was first successful with the trypsin-independent A/WSN/33 strain, for which the authors could use the very efficiently transfectable 293T (11, 35) or Vero cells (41). The system was later improved by making use of a coculture of 293T cells with the highly infectible MDCK cells (21), also allowing the engineering of trypsin-dependent type A influenza viruses. For the type B influenza virus, the system was developed using a coculture of the trypsin-resistant, efficiently transfectable COS7 cells with MDCK cells (20). To set up our reverse-genetics system for the type C influenza virus, we first thought of using cells that are sensitive to type C influenza virus infection. The SK 93/2 cell line, which is highly infectible by type C influenza virus (data not shown), proved to be poorly transfectable by a green fluorescent protein control plasmid, whatever the transfectant agent (FUGENE 6 [Roche], Lipofectamine 2000 [Invitrogen], or Jet PEI [Ozyme]) used (data not shown). Therefore, conditions were developed that allowed efficient growth of influenza C virus on the highly transfectable 293T cells.
The second technical problem was related to the detection and titration of the influenza C virus produced by reverse genetics. Usually authors use a red-blood-cell hemagglutination test (17), which detects both virion particles and HEF released in the supernatant. We developed a plaque assay based on the method used for influenza A virus (52). It was not possible to use the SK 93/2 cells, because they are not adherent enough, and only MDCK II cell monolayers remained intact when the agarose overlay was removed before staining with crystal violet (data not shown). Their resistance to infection with type C influenza virus was successfully overcome by coating the cells with BBG, which naturally contain Neu5,9Ac2 (17) and allowed the development of a reproducible plaque assay for influenza C virus on MDCK II cells (Fig. 1).
It is well known that at the optimal temperature of 33°C, the type C influenza virus grows on susceptible cells more slowly than type A at 35°C or type B at 33°C. Because of this slow virus growth, contrary to the case with type A and B influenza viruses, for which viruses rescued by reverse genetics were detected as soon as 24 or 36 h posttransfection (20, 35), the wild-type type C influenza virus rescued by our reverse-genetics system was first detectable in the supernatant of transfected cells only at 6 days posttransfection (data not shown), and the maximum yield was obtained only at day nine or ten. Also, for the titration by plaque assay, plaques of type A or B influenza virus usually appeared after 3 days, whereas for type C, plaques were clearly detected only after 4 or 5 days.
The reverse-genetics system we developed for influenza C virus is efficient and might be further improved. Indeed, coculture of highly transfectable cells, such as 293T, COS (20), or Vero (11) cells, with highly infectible cells, such as SK 93/2, might help to rescue viruses more efficiently. No improvement was observed when using 293T and SK 93/2 cells cocultured at a 1/1 ratio (data not shown), but different ratios need to be tested, as well as coculture with other cells permissive for influenza C virus. Alternatively, one could try to directly transfect the SK 93/2 cells by a more efficient method, such as electroporation or nucleofection (Amaxa Biosystems). Finally, as was done for type A and B influenza virus systems (20, 22, 34), one could wish to reduce the number of plasmids. However, to study mutations that affect the polymerase complex (structure or activity), a system that separates the vRNA and protein expression plasmids should be preferred for the rescue of mutant viruses. Indeed, if the mutation introduced in the vRNA affects the activity of the polymerase complex protein, a system based on bidirectional plasmids might not allow the reconstruction of functional RNPs and hence the rescue of the mutant virus.
Using our reverse-genetics system, based entirely on plasmids, we successfully generated influenza C viruses with mutations in the HEF protein. The Thr 465 Ala substitution resulted in an increase of virus growth capabilities (Fig. 3 and 4). Residue 465 is located in the peptide fusion domain of the HEF2 subunit, which is involved in the fusion of the virus envelope and cell membranes (42). The work of Formanowski et al. (12) indicated that amino acid substitutions involving a change of charge in HEF2 might be responsible for the variation of the pH optimum for fusion among influenza C virus strains. Since the Thr-to-Ala substitution replaced a polar residue with a nonpolar residue, the global hydrophobicity of the fusion peptide might be increased and the fusion capabilities of the virus enhanced, thus explaining the difference in growth properties. Interestingly, we also noticed that recovery of the 465 Ala viruses by reverse genetics seemed to be easier, since the virus yields in the supernatant of the transfected cells repeatedly reached about 104 PFU/ml at 6 days after transfection, i.e., 10- to 100-fold more than for the wild-type-like virus at that time (data not shown). This could prove useful for studying the positive or negative effects of mutations in any of the seven segments on the growth and replication of influenza C virus.
Using our reverse-genetics system, we confirmed that the Thr 284 Ile mutation in HEF described by Szepanski et al. (50) was associated with the capability of influenza C virus to grow on MDCK II cells in the presence of a high concentration of trypsin. Thr 284 in the HEF was found to be conserved in all sequences available in the GenBank database for influenza C virus strains isolated between 1950 and 2000. For the hemagglutinin of influenza A virus, it was shown that a single point mutation can have a drastic effect on the receptor-binding activity (47, 49). For instance, for the H1 and H3 subtypes, position 226 in the HA was shown to determine the receptor specificity by the recognition of α2,3-linked or α2,6-linked sialic acids (36, 47, 53). Similarly, Suzuki et al. (49) showed that position 205 in H1 can on its own influence the binding specificity. The substitution at residue 193 of H3 altered the binding of the hemagglutinin from human or equine influenza A viruses (32). The Thr 284 Ile substitution in the HEF protein of influenza C virus was described by Szepanski et al. for a mutant virus obtained by passaging C/JHB/1/66 on MDCK II cells in the presence of a high concentration of trypsin (50, 51). Our results further demonstrated that the Thr 284 Ile substitution is necessary and sufficient to enable influenza C virus to grow on MDCK II cells at a high concentration of trypsin in the absence of BBG. Based on adhesion assays on ganglioside-treated red blood cells (50), it was suggested that an Ile at position 284 would enhance the affinity of HEF for the Neu5,9Ac2 sialic acid receptor. Since position 285 of HEF was found to be directly involved in receptor binding (48), it is possible that an Ile at position 284 induces a conformational change in the structure of the receptor-binding pocket. However, how and where the trypsin acts in this process is not clear at present. It seems rather unlikely that a high concentration of trypsin could improve the cleavage of HEF, since similar effects would be expected irrespective of the nature of the residue at position 284. It is then possible that another low-affinity cleavage site, which would be recognized by trypsin, could be revealed by a change of conformation of the HEF protein of 284 Ile viruses. This would in turn lead to changes in the HEF properties that could be involved in the observed growth phenotype. Alternatively, trypsin at a high concentration could act on the MDCK II cells and unmask Neu5,9Ac2 sialic acids that would be present in very small amounts on the MDCK II cells. This could explain why only the 284 Ile viruses, with their enhanced HEF affinity for the receptor, would grow in these conditions.
Our system for influenza C virus completes the series of reverse-genetics systems for the different genera of the Orthomyxoviridae family. While this paper was under review, a similar system was described for type C influenza virus C/Ann Arbor/1/50 by Muraki et al. (33). These will prove extremely helpful for addressing a number of questions in the field of influenza virus research, with a particular interest for the type specificity requirements. Having the technology to introduce any viable mutation into the influenza C virus genome will enable us to study the viral life cycle and its regulation, the structure-function relationships of the different viral proteins, or the molecular mechanisms of viral pathogenicity (notably the limited pathogenicity recorded for influenza C virus). Finally, one could try to engineer influenza C viruses to generate expression vectors, which could then be used as live vaccines.
Acknowledgments
We thank Patricia Jeannin for production of influenza C viruses on eggs, and we are greatly indebted to Cyril Barbezange for helpful discussion and for critical reading of the manuscript.
Footnotes
Published ahead of print on 8 August 2007.
REFERENCES
- 1.Air, G. M., and R. W. Compans. 1983. Influenza B and influenza C viruses, p. 280-304. In P. Palese and D. W. Kingsbury (ed.), Genetics of influenza viruses. Springer-Verlag, Vienna, Austria.
- 2.Alamgir, A. S., Y. Matsuzaki, S. Hongo, E. Tsuchiya, K. Sugawara, Y. Muraki, and K. Nakamura. 2000. Phylogenetic analysis of influenza C virus nonstructural (NS) protein genes and identification of the NS2 protein. J. Gen. Virol. 81:1933-1940. [DOI] [PubMed] [Google Scholar]
- 3.Brown, I. H., P. A. Harris, and D. J. Alexander. 1995. Serological studies of influenza viruses in pigs in Great Britain 1991-2. Epidemiol. Infect. 114:511-520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Buonagurio, D. A., S. Nakada, W. M. Fitch, and P. Palese. 1986. Epidemiology of influenza C virus in man: multiple evolutionary lineages and low rate of change. Virology 153:12-21. [DOI] [PubMed] [Google Scholar]
- 5.Clern-van Haaster, C. M., and H. Meier-Ewert. 1984. 3′-Terminal sequences of influenza C virion RNA. Arch. Virol. 80:239-246. [DOI] [PubMed] [Google Scholar]
- 6.Crescenzo-Chaigne, B., N. Naffakh, and S. van der Werf. 1999. Comparative analysis of the ability of the polymerase complexes of influenza viruses type A, B and C to assemble into functional RNPs that allow expression and replication of heterotypic model RNA templates in vivo. Virology 265:342-353. [DOI] [PubMed] [Google Scholar]
- 7.Crescenzo-Chaigne, B., S. van der Werf, and N. Naffakh. 2002. Differential effect of nucleotide substitutions in the 3′ arm of the influenza A virus vRNA promoter on transcription/replication by avian and human polymerase complexes is related to the nature of PB2 amino acid 627. Virology 303:240-252. [DOI] [PubMed] [Google Scholar]
- 8.Desselberger, U., V. R. Racaniello, J. J. Zazra, and P. Palese. 1980. The 3′ and 5′-terminal sequences of influenza A, B and C virus RNA segments are highly conserved and show partial inverted complementarity. Gene 8:315-328. [DOI] [PubMed] [Google Scholar]
- 9.de Wit, E., M. I. Spronken, G. Vervaet, G. F. Rimmelzwaan, A. D. Osterhaus, and R. A. Fouchier. 2007. A reverse-genetics system for influenza A virus using T7 RNA polymerase. J. Gen. Virol. 88:1281-1287. [DOI] [PubMed] [Google Scholar]
- 10.Enami, M., W. Luytjes, M. Krystal, and P. Palese. 1990. Introduction of site-specific mutations into the genome of influenza virus. Proc. Natl. Acad. Sci. USA 87:3802-3805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fodor, E., L. Devenish, O. G. Engelhardt, P. Palese, G. G. Brownlee, and A. Garcia-Sastre. 1999. Rescue of influenza A virus from recombinant DNA. J. Virol. 73:9679-9682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Formanowski, F., S. A. Wharton, L. J. Calder, C. Hofbauer, and H. Meier-Ewert. 1990. Fusion characteristics of influenza C viruses. J. Gen. Virol. 71:1181-1188. [DOI] [PubMed] [Google Scholar]
- 13.Guo, Y. J., F. G. Jin, P. Wang, M. Wang, and J. M. Zhu. 1983. Isolation of influenza C virus from pigs and experimental infection of pigs with influenza C virus. J. Gen. Virol. 64:177-182. [DOI] [PubMed] [Google Scholar]
- 14.Hanika, A., B. Larisch, E. Steinmann, C. Schwegmann-Wessels, G. Herrler, and G. Zimmer. 2005. Use of influenza C virus glycoprotein HEF for generation of vesicular stomatitis virus pseudotypes. J. Gen. Virol. 86:1455-1465. [DOI] [PubMed] [Google Scholar]
- 15.Herrler, G., I. Durkop, H. Becht, and H. D. Klenk. 1988. The glycoprotein of influenza C virus is the hemagglutinin, esterase and fusion factor. J. Gen. Virol. 69:839-846. [DOI] [PubMed] [Google Scholar]
- 16.Herrler, G., and H. D. Klenk. 1991. Structure and function of the HEF glycoprotein of influenza C virus. Adv. Virus Res. 40:213-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Herrler, G., and H. D. Klenk. 1987. The surface receptor is a major determinant of the cell tropism of influenza C virus. Virology 159:102-108. [DOI] [PubMed] [Google Scholar]
- 18.Herrler, G., G. Multhaup, K. Beyreuther, and H. D. Klenk. 1988. Serine 71 of the glycoprotein HEF is located at the active site of the acetylesterase of influenza C virus. Arch. Virol. 102:269-274. [DOI] [PubMed] [Google Scholar]
- 19.Herrler, G., R. Rott, H. D. Klenk, H. P. Muller, A. K. Shukla, and R. Schauer. 1985. The receptor-destroying enzyme of influenza C virus is neuraminate-O-acetylesterase. EMBO J. 4:1503-1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoffmann, E., K. Mahmood, C. F. Yang, R. G. Webster, H. B. Greenberg, and G. Kemble. 2002. Rescue of influenza B virus from eight plasmids. Proc. Natl. Acad. Sci. USA 99:11411-11416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoffmann, E., G. Neumann, Y. Kawaoka, G. Hobom, and R. G. Webster. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. USA 97:6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoffmann, E., and R. G. Webster. 2000. Unidirectional RNA polymerase I-polymerase II transcription system for the generation of influenza A virus from eight plasmids. J. Gen. Virol. 81:2843-2847. [DOI] [PubMed] [Google Scholar]
- 23.Jackson, D., A. Cadman, T. Zurcher, and W. S. Barclay. 2002. A reverse genetics approach for recovery of recombinant influenza B viruses entirely from cDNA. J. Virol. 76:11744-11747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kimura, H., C. Abiko, G. Peng, Y. Muraki, K. Sugawara, S. Hongo, F. Kitame, K. Mizuta, Y. Numazaki, H. Suzuki, and K. Nakamura. 1997. Interspecies transmission of influenza C virus between humans and pigs. Virus Res. 48:71-79. [DOI] [PubMed] [Google Scholar]
- 25.Luytjes, W., M. Krystal, M. Enami, J. D. Parvin, and P. Palese. 1989. Amplification, expression, and packaging of a foreign gene by influenza virus. Cell 59:1107-1113. [DOI] [PubMed] [Google Scholar]
- 26.Manuguerra, J. C., and C. Hannoun. 1992. Natural infection of dogs by influenza C virus. Res. Virol. 143:199-204. [DOI] [PubMed] [Google Scholar]
- 27.Manuguerra, J. C., C. Hannoun, F. Simon, E. Villar, and J. A. Cabezas. 1993. Natural infection of dogs by influenza C virus: a serological survey in Spain. New Microbiol. 16:367-371. [PubMed] [Google Scholar]
- 28.Marschall, M., A. Helten, A. Hechtfischer, A. Zach, C. Banaschewski, W. Hell, and H. Meier-Ewert. 1999. The ORF, regulated synthesis, and persistence-specific variation of influenza C viral NS1 protein. Virology 253:208-218. [DOI] [PubMed] [Google Scholar]
- 29.Matsuzaki, Y., C. Abiko, K. Mizuta, K. Sugawara, E. Takashita, Y. Muraki, H. Suzuki, M. Mikawa, S. Shimada, K. Sato, M. Kuzuya, S. Takao, K. Wakatsuki, T. Itagaki, S. Hongo, and H. Nishimura. 2007. A nationwide epidemic of influenza C virus infection in Japan in 2004. J. Clin. Microbiol. 45:783-788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Matsuzaki, Y., N. Katsushima, Y. Nagai, M. Shoji, T. Itagaki, M. Sakamoto, S. Kitaoka, K. Mizuta, and H. Nishimura. 2006. Clinical features of influenza C virus infection in children. J. Infect. Dis. 193:1229-1235. [DOI] [PubMed] [Google Scholar]
- 31.Matsuzaki, Y., K. Mizuta, K. Sugawara, E. Tsuchiya, Y. Muraki, S. Hongo, H. Suzuki, and H. Nishimura. 2003. Frequent reassortment among influenza C viruses. J. Virol. 77:871-881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Medeiros, R., N. Naffakh, J. C. Manuguerra, and S. van der Werf. 2004. Binding of the hemagglutinin from human or equine influenza H3 viruses to the receptor is altered by substitutions at residue 193. Arch. Virol. 149:1663-1671. [DOI] [PubMed] [Google Scholar]
- 33.Muraki, Y., T. Murata, E. Takashita, Y. Matsuzaki, K. Sugawara, and S. Hongo. 2007. A mutation on influenza C virus M1 protein affects virion morphology by altering the membrane affinity of the protein. J. Virol. 81:8766-8773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Neumann, G., K. Fujii, Y. Kino, and Y. Kawaoka. 2005. An improved reverse genetics system for influenza A virus generation and its implications for vaccine production. Proc. Natl. Acad. Sci. USA 102:16825-16829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neumann, G., T. Watanabe, H. Ito, S. Watanabe, H. Goto, P. Gao, M. Hughes, D. R. Perez, R. Donis, E. Hoffmann, G. Hobom, and Y. Kawaoka. 1999. Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl. Acad. Sci. USA 96:9345-9350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nobusawa, E., and K. Nakajima. 1988. Amino acid substitution at position 226 of the hemagglutinin molecule of influenza (H1N1) virus affects receptor binding activity but not fusion activity. Virology 167:8-14. [DOI] [PubMed] [Google Scholar]
- 37.Ohuchi, M., R. Ohuchi, and K. Mifune. 1982. Demonstration of hemolytic and fusion activities of influenza C virus. J. Virol. 42:1076-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ohwada, K., F. Kitame, and M. Homma. 1986. Experimental infections of dogs with type C influenza virus. Microbiol. Immunol. 30:451-460. [DOI] [PubMed] [Google Scholar]
- 39.Ohwada, K., F. Kitame, K. Sugawara, H. Nishimura, M. Homma, and K. Nakamura. 1987. Distribution of the antibody to influenza C virus in dogs and pigs in Yamagata Prefecture, Japan. Microbiol. Immunol. 31:1173-1180. [DOI] [PubMed] [Google Scholar]
- 40.Ollert, M. W., R. Frade, A. Fiandino, M. Panneerselvam, E. C. Petrella, M. Barel, M. K. Pangburn, R. Bredehorst, and C. W. Vogel. 1990. C3-cleaving membrane proteinase. A new complement regulatory protein of human melanoma cells. J. Immunol. 144:3862-3867. [PubMed] [Google Scholar]
- 41.Ozaki, H., E. A. Govorkova, C. Li, X. Xiong, R. G. Webster, and R. J. Webby. 2004. Generation of high-yielding influenza A viruses in African green monkey kidney (Vero) cells by reverse genetics. J. Virol. 78:1851-1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Palese, P., and M. L. Shaw. 2007. Orthomyxoviridae: the viruses and their replication, p. 1647-1689. In D. M. Knipe and P. M. Howley (ed.), Fields virology. Lippincott Williams & Wilkins, Philadelphia, PA.
- 43.Panneerselvam, M., S. Welt, L. J. Old, and C. W. Vogel. 1986. A molecular mechanism of complement resistance of human melanoma cells. J. Immunol. 136:2534-2541. [PubMed] [Google Scholar]
- 44.Pfeifer, J. B., and R. W. Compans. 1985. Structure and variation of the influenza C glycoprotein. Vaccine 3:189-194. [DOI] [PubMed] [Google Scholar]
- 45.Pfeifer, J. B., and R. W. Compans. 1984. Structure of the influenza C glycoprotein gene as determined from cloned DNA. Virus Res. 1:281-296. [DOI] [PubMed] [Google Scholar]
- 46.Rogers, G. N., G. Herrler, J. C. Paulson, and H. D. Klenk. 1986. Influenza C virus uses 9-O-acetyl-N-acetylneuraminic acid as a high affinity receptor determinant for attachment to cells. J. Biol. Chem. 261:5947-5951. [PubMed] [Google Scholar]
- 47.Rogers, G. N., J. C. Paulson, R. S. Daniels, J. J. Skehel, I. A. Wilson, and D. C. Wiley. 1983. Single amino acid substitutions in influenza hemagglutinin change receptor binding specificity. Nature 304:76-78. [DOI] [PubMed] [Google Scholar]
- 48.Rosenthal, P. B., X. Zhang, F. Formanowski, W. Fitz, C. H. Wong, H. Meier-Ewert, J. J. Skehel, and D. C. Wiley. 1998. Structure of the hemagglutinin-esterase-fusion glycoprotein of influenza C virus. Nature 396:92-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Suzuki, Y., H. Kato, C. W. Naeve, and R. G. Webster. 1989. Single-amino-acid substitution in an antigenic site of influenza virus hemagglutinin can alter the specificity of binding to cell membrane-associated gangliosides. J. Virol. 63:4298-4302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Szepanski, S., H. J. Gross, R. Brossmer, H. D. Klenk, and G. Herrler. 1992. A single point mutation of the influenza C virus glycoprotein (HEF) changes the viral receptor-binding activity. Virology 188:85-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Szepanski, S., H.-D. Klenk, and G. Herrler. 1989. Analysis of a mutant of influenza C virus with a change in the receptor specificity, p. 125-134. In R. W. Compans, A. Helenius, and M. B. A. Oldstone (ed.), Cell biology of virus entry, replication, and pathogenesis. A. R. Liss, New York, NY.
- 52.Tobita, K., A. Sugiura, C. Enomote, and M. Furuyama. 1975. Plaque assay and primary isolation of influenza A viruses in an established line of canine kidney cells (MDCK) in the presence of trypsin. Med. Microbiol. Immunol. (Berlin) 162:9-14. [DOI] [PubMed] [Google Scholar]
- 53.Vines, A., K. Wells, M. Matrosovich, M. R. Castrucci, T. Ito, and Y. Kawaoka. 1998. The role of influenza A virus hemagglutinin residues 226 and 228 in receptor specificity and host range restriction. J. Virol. 72:7626-7631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wagner, E., O. G. Engelhardt, S. Gruber, O. Haller, and G. Kochs. 2001. Rescue of recombinant Thogoto virus from cloned cDNA. J. Virol. 75:9282-9286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yamaoka, M., H. Hotta, M. Itoh, and M. Homma. 1991. Prevalence of antibody to influenza C virus among pigs in Hyogo Prefecture, Japan. J. Gen. Virol. 72:711-714. [DOI] [PubMed] [Google Scholar]
- 56.Zimmer, G., F. Lottspeich, A. Maisner, H. D. Klenk, and G. Herrler. 1997. Molecular characterization of gp40, a mucin-type glycoprotein from the apical plasma membrane of Madin-Darby canine kidney cells (type I). Biochem. J. 326:99-108. [DOI] [PMC free article] [PubMed] [Google Scholar]