Abstract
First-pass metabolism is a common cause of incomplete and variable absolute bioavailability for an orally dosed drug. The drug-metabolizing enzyme CYP3A4 is often implicated in this process, resulting, in some cases, in systemic exposures of less than 15% of the administered dose. By creating an elegant CYP3A4-transgenic mouse model, van Herwaarden et al. show in this issue of the JCI that first-pass metabolism of the anticancer agent docetaxel by the gut wall, and not the liver, is likely to be the major cause of its low oral bioavailability in humans (see the related article beginning on page 3583). This study helps explain interpatient differences in efficacy and safety following oral therapy with approved CYP3A4 substrates and provides a powerful new tool for preclinical predictions of first-pass metabolism for new drugs in development.
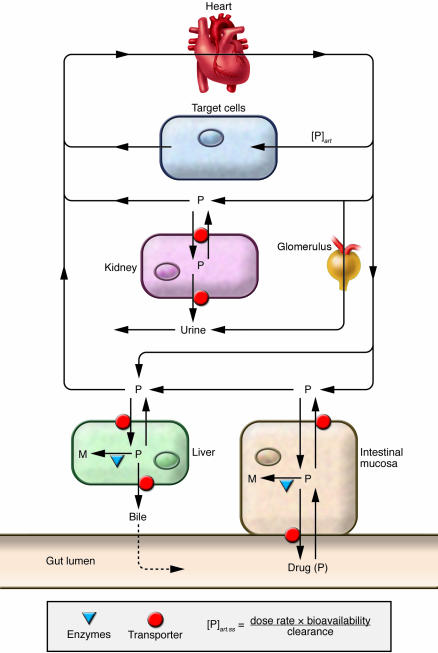
The concept of first-pass intestinal drug metabolism in humans is not new. Clinical investigators have known for decades that the metabolic fate of a drug dosed orally might differ substantially from that of an intravenous dose. As shown in Figure 1, drug is absorbed from the intestinal lumen into the mesenteric capillaries, and along the way it can be subjected to metabolic transformation by a battery of enzymes, particularly phase II conjugation enzymes such as the glucuronosyltransferases and sulfotransferases that are localized primarily in the mucosal enterocytes (1). A similar process can occur in hepatic parenchymal cells, as drug that is absorbed unchanged into the portal vein passes through the liver for the first time on its way to the heart and the rest of the body. Consequently, as in the case of the β2-receptor agonists isoproterenol and terbutaline (2), there can be sequential “first-pass” loss of a significant fraction of the oral dose by the actions of both hepatic and intestinal transferases before the drug ever reaches the systemic circulation, from where most often it exerts its pharmacological effects. When a drug is dosed intravenously, it avoids first-pass metabolism and is generally completely bioavailable to the different tissues of the body. Although both hepatic and intestinal enzymes, such as the glucuronosyl and sulfotransferases and those in the cytochrome P450 family, can catalyze first-pass drug metabolism, it was generally assumed that, with some exceptions, the liver exerted the dominant effect. However, discovery of the drug-metabolizing enzyme cytochrome P450 3A polypeptide 4 (CYP3A4) in the human intestinal mucosa as well as the liver by Watkins and coworkers (3, 4) and a demonstration that it contributes in a significant way to the first-pass metabolism of intestinally dosed cyclosporine (5) and midazolam (6), along with recognition that CYP3A4 metabolizes a large percentage of drugs currently available in the US (7), have led to renewed interest in the process of gut wall metabolism and its implications for drug therapy.
Figure 1. Pharmacokinetic model depicting the effect of intestinal and hepatic first-pass metabolism on steady-state systemic blood concentrations of an orally administered drug ([P]art.ss).
Sequential first-pass metabolism of the drug (P) to a metabolite (M) can occur in the enterocytes of the intestinal mucosa and in the hepatic parenchymal cells. This contributes, along with the fraction of the dose in the gut lumen that is absorbed into the enterocytes, to the absolute bioavailability of the oral dose. A reduction in oral bioavailability by first-pass metabolism has a proportional effect on the concentration of drug reaching the arterial blood circulation and, hence, the site of drug action. In this issue of the JCI, van Herwaarden et al. (1) show that selective intestinal expression of the human CYP3A4 gene in Cyp3a-knockout mice conferred high first-pass elimination of the anticancer agent docetaxel, in contrast to a more modest effect from selective hepatic CYP3A4 expression. art, arterial.
Quantitative differences in hepatic and intestinal CYP3A4 activity
In an elegant study of intestine- and liver-selective transgenic expression of CYP3A4 on a complete mouse Cyp3a gene knockout background, van Herwaarden et al. report in this issue of the JCI (8) unequivocal evidence of the profound impact that intestinal CYP3A4 activity has on systemic exposure to the anticancer drug docetaxel (Taxotere) following oral administration. Taking on the formidable task of removing all eight mouse Cyp3a genes, the investigators found that selective replacement of the major human CYP3A enzyme, CYP3A4, into the intestinal mucosa of these animals essentially restored the considerable first-pass metabolism of docetaxel that occurs normally in the wild-type animal and in humans. Moreover, selective hepatic expression of CYP3A4 conferred a near normal systemic clearance of the drug. Intriguingly, the authors also reported that the effect of intestinal CYP3A4 expression on systemic exposure to an oral docetaxel dose was much greater than that of the hepatically expressed CYP3A4 enzyme, even though both organs can exert a first-pass effect. The explanation for this observation is unclear, but it lends greater credence to the preeminence of intestinal enzymes in the first-pass metabolism process. The investigation was also remarkable for the subtle nuances that it confirmed about intestinal CYP3A4 function. For example, intestinal CYP3A4 expression also altered the disposition of an intravenous docetaxel dose, but to a much lesser extent than that of the oral dose, a phenomenon that has been observed in humans with midazolam (6) and attributed to segregated mucosal blood flow and the obligatory nature of first-pass elimination of transcellularly absorbed drugs (9).
Limited role for CYP3A enzymes in the regulation of endogenous hormones
In addition to many drugs, CYP3A4 catalyzes the metabolism of several different endogenous molecules, including androgens, estrogens, progestins, and vitamin D, and thus it was expected that a complete loss of this activity in the mouse (i.e., Cyp3a–/–) would lead to some physiological change and health consequences. However, the results of van Herwaarden et al. (8) revealed that a loss of all mouse Cyp3a enzymes had no apparent impact on the disposition of the steroidal substrates testosterone and estradiol, nor did it have an impact on the viability and fertility of the animals. This suggests that CYP3A4 may not be an important mediator of systemic and organ homeostasis in humans or that its role in regulating the function of different hormonal substrates is not as straightforward as previously thought. Admittedly, though, the analysis of endogenous CYP3A substrates by van Herwaarden et al. (8) was not exhaustive and, in their microarray analysis of total hepatic gene expression, significant increases and decreases in the mRNA levels for a number of genes were observed in the knockout animals. Thus, some systemic or local (e.g., intestinal) tissue effects from the complete loss of Cyp3a activity may eventually be revealed.
Revolutionary change in screening for intestinal first-pass metabolism
Regardless of the ultimate role of CYP3A4 in regulating the hormonal effects of molecules such as testosterone and estradiol, the results of van Herwaarden et al. (8) should refocus attention to the metabolic barrier function of CYP3A in preventing systemic exposure to naturally occurring and synthetic substrate molecules that are ingested orally. In this regard, the mouse models developed by these investigators (Cyp3a–/–V and Cyp3a–/–A, selective intestinal and hepatic CYP3A4 expression, respectively, on a Cyp3a-null mouse background) may revolutionize the way the drug industry screens new therapeutic molecules to evaluate the effects of CYP3A-dependent, first-pass metabolism. Extensive first-pass metabolism catalyzed by CYP3A4 is a considerable problem not only because it is commonly encountered in the development of new drugs, but also because of the high interpatient variability in both hepatic and intestinal CYP3A expression and function (10, 11) and the sensitivity of CYP3A4 to numerous inductive and inhibitory interactions with existing therapeutic agents (12). As pointed out by van Herwaarden et al. (8), it is the lack of predictability in systemic exposure to an orally dosed parent drug (and potentially active metabolites) and not necessarily the loss per se that creates a therapeutic dilemma and often precludes the use of the more convenient oral route of administration. The coadministration with docetaxel of a CYP3A inhibitor such as ritonavir could circumvent the problem of variable and extensive first-pass metabolism under short-term dosing conditions (e.g., certain chemotherapeutic regimens) and therefore result in high levels of docetaxel reaching the systemic circulation following oral administration. However, in the case of long-term therapies, it would likely create new clinical challenges and adverse consequences resulting from drug interactions with other therapeutic CYP3A substrates.
Broad applications of the CYP3A4 transgenic mouse model
The findings of van Herwaarden et al. (8) illustrate the important role that intestinal CYP3A4 expression can have in determining the biological response to an orally dosed substrate. However, they also turn the spotlight on our incomplete knowledge about intestinal CYP3A4 function and regulation. Indeed, it is remarkable that the authors observed such extensive first-pass metabolism of docetaxel given the relatively high dose (10 mg/kg) that was administered. Some investigators have suggested that this intestinal enzyme will be easily saturated when a substrate is dosed orally, and hence its impact on oral bioavailability may be greatly attenuated in the face of an unimpaired diffusional uptake clearance. Presumably, docetaxel did not accumulate within the mouse enterocytes after oral administration to levels that exceeded the 1- to 2-μM Km value that the authors reported for the dominant CYP3A4 metabolic pathway. Indeed, in comparing the tissue distribution of docetaxel in the CYP3A4-transgenic mouse (Cyp3a–/–V) to that of the Cyp3a-knockout mouse, the authors found much lower parent drug levels (and higher metabolite concentrations) in the intestine when CYP3A4 was expressed in situ. This also appears to be true for midazolam, a rapidly absorbed CYP3A probe drug that exhibits both high aqueous solubility and high membrane permeability (Biopharmaceutics Class System [BCS] class 1 drug; refs. 13, 14), as do other drugs thought to undergo significant intestinal first-pass metabolism, such as nifedipine, verapamil, and felodipine in humans.
Limited saturation of intestinal CYP3A4 in vivo may not be the rule for all of its substrates, particularly those that are given at relatively high doses and that exhibit low aqueous solubility and high membrane permeability (e.g., BCS class 2 drugs), such as cyclosporine and tacrolimus. For these and other drugs with similar physico-chemical properties, it has been suggested that a synergistic interaction between CYP3A4 and P-glycoprotein (also known as ABCB1) may enhance first-pass loss of a drug that might otherwise escape the intestine largely unchanged (15, 16). There is considerable controversy surrounding this mechanistically interesting hypothesis, and, as van Herwaarden et al. (8) point out, a modification of their CYP3A4-transgenic models to incorporate deletion and insertion of the mouse and human ABCB1 gene(s) may permit more rigorous testing of this concept. This and other pharmacokinetic aspects of intestinal first-pass metabolism, such as the impact of a basolateral membrane diffusional barrier, plasma protein binding, and mucosal blood flow on first-pass intestinal extraction, could be readily investigated with their animal model. The model should also be amenable to studies of CYP3A4 inhibition. Although an in vitro determination of inhibition potency reveals much about the potential of a new molecular entity (NME) to reduce CYP3A4-dependent drug clearance, the in vivo mouse models of van Herwaarden et al. (8) should provide unique quantitative information about the change in systemic drug exposure as a function of the NME dose, as well as a better understanding of time-dependent, mechanism-based inhibition and a clearer dissection of the potential sites (hepatic or intestinal) of a CYP3A4 drug substrate–NME interaction.
Future research needs and directions
One characteristic of the Cyp3a–/–V mouse model that limits its application for exploring CYP3A4 function is the fact that the human genetic insert lacks cis-regulatory elements that mediate constitutive enzyme expression and its modulation by trans-acting factors such as the human pregnane receptor (hPXR) and the vitamin D receptor (VDR). In this regard, the mouse model of Cheung and coworkers provides intestinal and hepatic expression of the entire gene, including known 5′regulatory elements (17), although currently not in an organ-selective way and not on a mouse Cyp3a-deficient background. However, such a system can still permit investigation of sources of interindividual variability in hepatic and intestinal CYP3A4 expression and function, which despite a substantial amount of effort remains incompletely understood. For example, we (18) and others (19) have been studying the regulation of intestinal CYP3A4 by a VDR signaling pathway. The endogenous activating ligand may be 1α,25-dihydroxyvitamin D3 itself or possibly one of the more lipophilic bile acids (20).
Elucidation of the mechanisms of intestinal (and hepatic) CYP3A4 regulation is critical to understanding and predicting interpatient variability in drug response. Much has been made of late about the potential for genetic testing (e.g., CYP3A4, -5, -7 testing) to permit more rational, individualized dosing of a drug, but it is likely that in the case of CYP3A4 substrates, nongenetic factors will exert an important influence on enzyme function. Application of a humanized transgenic mouse model such as that of Cheung et al. (17) may permit the identification and characterization of both endogenous and exogenous modulating factors. Combined use of this model with that of van Herwaarden et al. (8) or creation of a dually functional hybrid may open the door toward a new round of mechanistic discovery of intestinal CYP3A function and translational applications that ultimately will lead to improvements in drug safety and efficacy.
Acknowledgments
K.E. Thummel is supported in part by a grant from the NIH (GM63666).
Footnotes
Nonstandard abbreviations used: CYP3A4, cytochrome P450 3A polypeptide 4.
Conflict of interest: The author has declared that no conflict of interest exists.
Citation for this article: J. Clin. Invest. 117:3173–3176 (2007). doi:10.1172/JCI34007.
See the related article beginning on page 3583.
References
- 1.Thummel K.E., Kunze K.L., Shen D.D.1997Enzyme-catalyzed processes of first-pass hepatic and intestinal drug extraction . Adv. Drug Deliv. Rev. 2799–127. [DOI] [PubMed] [Google Scholar]
- 2.Morgan D.J. Clinical pharmacokinetics of beta-agonists. Clin. Pharmacokinet. . 1990;18:270–294. doi: 10.2165/00003088-199018040-00002. [DOI] [PubMed] [Google Scholar]
- 3.Watkins P.B., et al. Identification of glucocorticoid-inducible cytochromes P-450 in the intestinal mucosa of rats and man. J. Clin. Invest. 1987;80:1029–1036. doi: 10.1172/JCI113156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kolars J.C., et al. Identification of rifampin-inducible P450IIIA4 (CYP3A4) in human small bowel enterocytes. J. Clin. Invest. . 1992;90:1871–1878. doi: 10.1172/JCI116064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kolars J.C., et al. 1991First-pass metabolism of cyclosporin by the gut . Lancet 3381488–1490. [DOI] [PubMed] [Google Scholar]
- 6.Paine M.F., et al. First-pass metabolism of midazolam by the human intestine. Clin. Pharmacol. Ther. 1996;60:14–24. doi: 10.1016/S0009-9236(96)90162-9. [DOI] [PubMed] [Google Scholar]
- 7.Guengerich F.P. Cytochrome P-450 3A4: regulation and role in drug metabolism. Annu. Rev. Pharmacol. Toxicol. 1999;39:1–17. doi: 10.1146/annurev.pharmtox.39.1.1. [DOI] [PubMed] [Google Scholar]
- 8.van Herwaarden A.E., et al. Knockout of cytochrome P450 3A yields new mouse models for understanding xenobiotic metabolism. J. Clin. Invest. 2007;117:3583–3592. doi: 10.1172/JCI33435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cong D., Doherty M., Pang K.S. A new physiologically based, segregated-flow model to explain route-dependent intestinal metabolism. Drug Metab. Dispos. . 2000;28:224–235. [PubMed] [Google Scholar]
- 10.Paine M.F., et al. Characterization of inter- and intra-intestinal differences in human CYP3A-dependent metabolism. J. Pharmacol. Exp. Ther. 1997;283:1552–1562. [PubMed] [Google Scholar]
- 11.von Richter O., et al. Cytochrome P450 3A4 and P-glycoprotein expression in human small intestinal enterocytes and hepatocytes: a comparative analysis in paired tissue specimens. Clin. Pharmacol. Ther. 2004;75:172–183. doi: 10.1016/j.clpt.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Thummel K.E., Wilkinson G.R. In vitro and in vivo drug interactions involving human CYP3A. Annu. Rev. Pharmacol. Toxicol. 1998;38:389–430. doi: 10.1146/annurev.pharmtox.38.1.389. [DOI] [PubMed] [Google Scholar]
- 13.Amidon G.L., et al. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm. Res. 1995;12:413–420. doi: 10.1023/a:1016212804288. [DOI] [PubMed] [Google Scholar]
- 14.Wu C.Y., Benet L.Z. Predicting drug disposition via application of BCS: transport/absorption/ elimination interplay and development of a biopharmaceutics drug disposition classification system. Pharm. Res. 2005;22:11–23. doi: 10.1007/s11095-004-9004-4. [DOI] [PubMed] [Google Scholar]
- 15.Lown K.S., et al. 1997Role of intestinal P-glycoprotein (mdr1) in interpatient variation in the oral bioavailability of cyclosporine . Clin. Pharmacol. Ther. 62248–260. [DOI] [PubMed] [Google Scholar]
- 16.Wacher V.J., et al. Role of P-glycoprotein and cytochrome P450 3A in limiting oral absorption of peptides and peptidomimetics. J. Pharm. Sci. 1998;87:1322–1330. doi: 10.1021/js980082d. [DOI] [PubMed] [Google Scholar]
- 17.Cheung C., et al. Growth hormone determines sexual dimorphism of hepatic cytochrome P450 3A4 expression in transgenic mice. J. Pharmacol. Exp. Ther. 2006;316:1328–1334. doi: 10.1124/jpet.105.094367. [DOI] [PubMed] [Google Scholar]
- 18.Thummel K.E., et al. Transcriptional control of intestinal cytochrome P-4503A by 1α,25-Dihydroxy Vitamin D3. . Mol. Pharmacol. . 2001;60:1399–1406. doi: 10.1124/mol.60.6.1399. [DOI] [PubMed] [Google Scholar]
- 19.Jurutka P.W., et al. Molecular and functional comparison of 1,25-dihydroxyvitamin D3 and the novel vitamin D receptor ligand, lithocholic acid, in activating transcription of cytochrome P450 3A4. . J. Cell. Biochem. 2005;94:917–943. doi: 10.1002/jcb.20359. [DOI] [PubMed] [Google Scholar]
- 20.Makishima M., et al. Vitamin D receptor as an intestinal bile acid sensor. Science. 2002;296:1313–1316. doi: 10.1126/science.1070477. [DOI] [PubMed] [Google Scholar]