Abstract
Repeated use of opiate analgesic drugs such as morphine for the relief of chronic pain may result in the development of opiate tolerance and dependence, leading to a narrowing of the drug’s therapeutic index and increased side effects. Previous preclinical work has shown that interruption of a signaling cascade involving the N-methyl-D-aspartate receptor and NO prevents morphine tolerance. In this issue of the JCI, Muscoli and colleagues extend our understanding of the role of NO in tolerance by demonstrating that, in mice, tolerance to chronic morphine administration is associated with NO conversion to peroxynitrite, which accumulates and nitrates tyrosine moieties within various proteins in the spinal cord (see the related article beginning on page 3530). This and other data suggest that peroxynitrite plays a role in opiate tolerance and that regulation of peroxynitrite may be utilized for the management of opiate-induced tolerance.
With the recognition of the importance of pain control in recent years and its designation as the “fifth vital sign” has come a marked expansion in opiate use, including the use of high doses in patients with refractory malignant and nonmalignant pain. Since there is no ceiling effect to opioid analgesia, doses can be increased to overcome tolerance or the inherent insensitivity of some pain types to opiate analgesics. In clinical practice, doses are progressively increased until the pain is controlled, but dose escalation is often limited by side effects such as sedation, confusion, constipation, or respiratory depression. Although tolerance develops to these side effects, it may not develop as quickly or to as great an extent as it does to analgesia, leading to a narrowing of the therapeutic index. It has been suggested that preventing tolerance would enable the use of lower opiate doses and avoid or minimize these side effects.
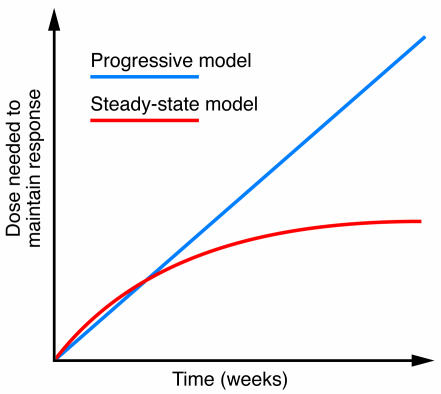
Opioid tolerance was considered an undesired and unavoidable result of chronic dosing until recent discoveries in animal models found that tolerance could be prevented without interfering with analgesia (1, 2). However, these same observations have not yet been fully confirmed clinically. Clinical pain is difficult to study due to inherent problems in the quantification of pain and pain relief, the influence of emotional and non-nociceptive factors in its perception, and the wide range of sensitivity of individuals to pain and to opiates. Tolerance has an additional disadvantage in that it is often difficult to dissociate disease progression from tolerance when assessing the need for dose escalation. In cancer patients on stable doses of opiates for extended periods, the need to escalate the dosage is more often due to disease progression than the sudden appearance of tolerance (3–5). Much of the clinical literature on tolerance is anecdotal, and there is some controversy about its significance. Critics of tolerance point out the ability to maintain patients with malignant (3, 4) and nonmalignant (6) pain on stable doses of opioids for extended periods of time. However, maintaining patients on stable doses for prolonged periods doses not necessarily indicate the absence of tolerance. Many of these patients take opiates at doses significantly higher than those used in naive patients, implying that they are indeed tolerant. Rather, these observations imply that tolerance may not necessarily be a continually escalating process and patients may achieve a steady state, or equilibrium level, of tolerance (Figure 1).
Figure 1. Hypothetical models of drug tolerance.
In drug tolerance, increased amounts of drug are needed to maintain an effect. In the clinical setting, many patients with malignant pain stabilize their dose over prolonged periods of time, with the need for further increases due to the progression of their underlying disease process. Tolerance is often considered as a progressive effect, in which drug doses need to be continually escalated. However, clinical observations suggest that in many situations tolerance can achieve a steady-state in which stable doses of drug are sufficient for extended periods of time.
Contributions to opioid tolerance
The first studies exploring tolerance at the molecular level focused upon transduction systems, with the proposal by Collier that chronic morphine treatment led to “hypertrophy”, or upregulation, of adenylyl cyclase activity to overcome its inhibition by opiates (7). He then suggested that withdrawal resulted from a rebound in adenylyl cyclase activity resulting from the loss of inhibition, following the discontinuation of the opioid or the administration of an antagonist. Unfortunately, tolerance has proven to be far more complex, involving factors at the level of the drug receptor, the cell, and the integrated nervous system (see “Sites of modulation of opioid tolerance”). Desensitization and trafficking of a drug’s receptor have been implicated in tolerance, as have a number of cellular factors such as G-protein regulation, regulator of G-protein signaling proteins, and both adenylyl and guanylyl cyclase. Perhaps the most complex aspect of tolerance involves its modulation by a number of neurotransmitter systems, including the enkephalins and the δ opioid receptor. Even drug disposition is important (8–10). Loss of P-glycoprotein impairs the blood-brain barrier and prevents the development of tolerance, while chronic morphine treatment upregulates P-glycoprotein levels in the brain, leading to lower morphine brain levels and a diminished response (9, 10). Although all these systems have been extensively studied, rarely have any taken into consideration the potential role of the others. Thus the study of opioid tolerance is like the adage of the three blind men trying to define an elephant. Each feels a different part of the animal, with one calling it a snake after feeling the trunk, another describes it as a wall after feeling its side, and yet another saying it is like a tree after feeling the leg. Ultimately, we need to step back and integrate all of these mechanisms into a unified model of tolerance in order to obtain the whole picture.
NMDA receptor/NO cascade and opioid tolerance
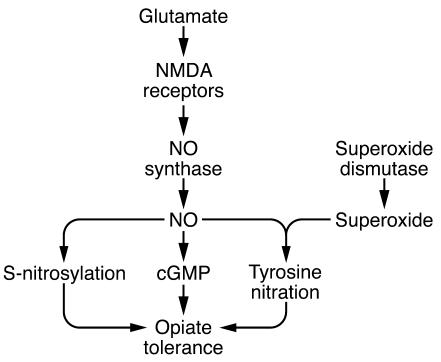
The modulatory neurotransmitter circuits offer particularly useful pharmacological targets. The most intensively studied system is the glutamate/NMDA/NO cascade (Figure 2). The importance of NMDA receptors in tolerance was first recognized over 15 years ago (11, 12) and was followed almost immediately by the discovery of a role for NO in morphine tolerance (13, 14) (see “Selected tolerance-related actions of NO”). Since these initial observations, many laboratories have confirmed the importance of the glutamate system and NO in opioid tolerance using a vast array of NMDA antagonists and neuronal NOS (nNOS) inhibitors (15, 16). There is even a mouse strain that does not develop tolerance to morphine due to a deficit at the level of the NMDA receptor (17), illustrating the potential importance of the genetic background of patients in the clinical development of tolerance.
Figure 2. Schematic of the NMDA receptor/NO cascade in opioid tolerance.
Activation of the NMDA receptor by glutamate induces the activation of NO synthase, which in turn synthesizes NO. As a gas, NO cannot be stored and immediately diffuses through membranes. NO will complex with heme-containing proteins such as guanylyl cyclase, which is then activated. It will also S-nitrosylate proteins, including subunit 1 and subunit 2 of the NMDA receptor. Finally, when exposed to superoxide, which is generated by superoxide dismutase, NO is converted to peroxynitrite, which will nitrate tyrosine residues within proteins, including the glutamate transporter GLT-1 and the enzyme glutamine synthase, as shown in the report in this issue from Muscoli et al. (20). Thus all three of these putative mechanisms of NO action may be involved in the development of opioid tolerance.
Despite the extensive literature over the past 15 years documenting the importance of NO in morphine tolerance, its molecular actions remain unclear. NO is an uncharged free radical gas, making it unique in the realm of neurotransmitters (18). It can readily diffuse through membranes and therefore can chemically attack many targets. It is synthesized upon demand since it cannot be stored, and its selectivity among targets is likely due to limiting its site of action by very localized stimulation of its synthetic enzyme NOS. One of the first NO actions identified was its ability to stimulate cGMP formation by binding to the heme moiety in the enzyme guanylyl cyclase, but it also will interact with other heme-containing proteins. NO is chemically reactive and S-nitrosylates a wide range of proteins under physiological conditions, including both subunit 1 and subunit 2 of the NMDA receptor (19) (see “Selected tolerance-related actions of NO”).
In their study in the current issue of the JCI (20), Muscoli and coworkers explore another mechanism of NO action in which exposure of NO to superoxide generates peroxynitrite, which then nitrates tyrosine residues. Using a murine model of chronic morphine administration, these authors confirmed the ability of the NO synthase inhibitor l-NAME to prevent morphine-induced tolerance and then demonstrated a similar effect with the superoxide scavenger MnTBAP3–, consistent with a role for peroxynitrite in the development of morphine tolerance. Evidence for this proposed role of peroxynitrite was strengthened by their observation of the accumulation of nitrotyrosine immunoreactivity in the dorsal horn of the spinal cord, a region important in opioid action. Immunoprecipitation followed by western blots revealed the presence of nitrotyrosine in mitochondrial superoxide dismutase, the glutamate transporter GLT-1, and the enzyme glutamine synthase following chronic morphine administration — proteins important in glutamate actions and in the regulation of superoxide formation. The same paradigms that blocked tolerance in vivo diminished the nitration of these proteins, as did inducing the decomposition of peroxynitrite.
These are interesting studies in that they provide a strong association between morphine tolerance and the nitration of tyrosine residues in a number of proteins associated with the glutamate/NMDA receptor/NO signaling cascade. However, establishing a causal relationship is not simple. Although blocking NO production prevents tolerance, not all NO is involved in tolerance. In fact, NO also enhances opioid analgesia (21). Neuronal NOS undergoes splicing. Although the predominant splice variant is involved in the development of morphine tolerance, a second splice variant, lacking exons 9 and 10, generates NO that has an opposite effect in vivo, facilitating analgesia, presumably through different targets (21). This may make it difficult to separate NO targets important in tolerance as opposed to those important to analgesia.
It also is important to integrate these findings with the prior observation that blockade of guanylyl cyclase also prevents morphine tolerance (22) and the demonstration that two different subunits of the NMDA receptor are endogenously S-nitrosylated in the brain (19). Any or all of these mechanisms of NO action may be important in opioid tolerance. The challenge in the future will be to establish causal relationships for these mechanisms. Muscoli and colleagues have provided strong evidence correlating the generation of nitrotyrosine proteins in morphine tolerance, and this needs to be examined further (18). The potential involvement of proinflammatory cytokines and the nuclear enzyme poly(ADP-ribose) polymerase, as suggested by these authors, seems more tenuous, but certainly deserving of additional investigation. The involvement of so many diverse components in the expression of morphine tolerance makes development of a comprehensive, integrated model difficult. However, this diversity also expands the number of potential pharmacological targets and will hopefully lead to new therapies to facilitate the use of opioids in the management of chronic pain.
Footnotes
Conflict of interest: The author is a consultant for Limmerick Neurosciences Inc. and EpiCept Corp. and receives research support from Sarentis Therapeutics.
Citation for this article: J. Clin. Invest. 117:3185–3187 (2007). doi:10.1172/JCI34035.
See the related article beginning on page 3530.
References
- 1.Inturrisi C.E. NMDA receptors, nitric oxide and opioid tolerance. Regul. Pept. 1994;54:129–130. [Google Scholar]
- 2.Pasternak G.W., Inturrisi C. Pharmacological modulation of opioid tolerance. Exp. Opin. Invest. Drugs. 1995;4:271–281. [Google Scholar]
- 3. Foley, K.M. 1996. Pain syndromes in patients with cancer. InPain management: theory and practice. R.K. Portenoy and R.M. Kanner, editors. F.A. Davis Company. Philadelphia, Pennsylvania, USA. 191–215. [Google Scholar]
- 4.Foley K.M. Controlling the pain of cancer. Sci. Am. 1996;275:164–165. doi: 10.1038/scientificamerican0996-164. [DOI] [PubMed] [Google Scholar]
- 5. Payne, R., and Pasternak, G.W. 1992. Pharmacology of pain treatment. InContemporary neurology series: scientific basis of neurologic drug therapy. M.V. Johnston, R. MacDonald, and A.B. Young, editors. Davis. Philadelphia, Pennsylvania, USA. 268–301. [Google Scholar]
- 6.Portenoy R.K. Current pharmacotherapy of chronic pain. J. Pain Symptom Manage. 2000;19:S16–S20. doi: 10.1016/s0885-3924(99)00124-4. [DOI] [PubMed] [Google Scholar]
- 7.Collier H.O. Cellular site of opiate dependence. Nature. 1980;283:625–629. doi: 10.1038/283625a0. [DOI] [PubMed] [Google Scholar]
- 8.Roerig S.C., O’Brien S.M., Fujimoto J.A., Wilcox G.L. Tolerance to morphine analgesia: decreased multiplicative interaction between spinal and supraspinal sites. Brain Res. 1984;308:360–363. doi: 10.1016/0006-8993(84)91078-3. [DOI] [PubMed] [Google Scholar]
- 9.Aquilante C.L., Letrent S.P., Pollack G.M., Brouwer K.L.R. Increased brain P-glycoprotein in morphine tolerant rats. Life Sci. 1999;66:PL47–PL51. doi: 10.1016/s0024-3205(99)00599-8. [DOI] [PubMed] [Google Scholar]
- 10.King M., Su W., Chang A., Zuckerman A., Pasternak G.W. Transport of opioids from the brain to the periphery by P-glycoprotein: peripheral actions of central drugs. Nat. Neurosci. 2001;4:268–274. doi: 10.1038/85115. [DOI] [PubMed] [Google Scholar]
- 11.Trujillo K.A., Akil H. Inhibition of morphine tolerance and dependence by the NMDA receptor anagonist MK-801. Science. 1991;251:85–87. doi: 10.1126/science.1824728. [DOI] [PubMed] [Google Scholar]
- 12.Ben-Eliyahu S., et al. The NMDA receptor antagonist MK-801 prevents long-lasting non-associative morphine tolerance in the rat. Brain Res. 1992;575:304–308. doi: 10.1016/0006-8993(92)90094-p. [DOI] [PubMed] [Google Scholar]
- 13.Kolesnikov Y.A., Pick C.G., Pasternak G.W. NG-Nitro-L-arginine prevents morphine tolerance. . Eur. J. Pharmacol. 1992;221:399–400. doi: 10.1016/0014-2999(92)90732-j. [DOI] [PubMed] [Google Scholar]
- 14.Kolesnikov Y.A., Pick C.G., Ciszewska G., Pasternak G.W. Blockade of tolerance to morphine but not to kappa opioids by a nitric oxide synthase inhibitor. Proc. Natl. Acad. Sci. U. S. A. 1993;90:5162–5166. doi: 10.1073/pnas.90.11.5162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Inturrisi C.E. Clinical pharmacology of opioids for pain. Clin. J. Pain. 2002;18:S3–S13. doi: 10.1097/00002508-200207001-00002. [DOI] [PubMed] [Google Scholar]
- 16. Pasternak, G.W., and Kolesnikov, Y. 2005. The NMDA/Nitric oxide synthase cascade in opioid analgesia and tolerance. InContemporary clinical neuroscience: glutamate and addiction. B.H. Herman, et al., editors. Humana Press. Totowa, New Jersey, USA. 409–416. [Google Scholar]
- 17.Kolesnikov Y., Jain S., Wilson R., Pasternak G.W. Lack of morphine and enkephalin tolerance in 129/SvEv mice: Evidence for a NMDA receptor defect. J. Pharmacol. Exp. Ther. 1998;284:455–459. [PubMed] [Google Scholar]
- 18.Bredt D.S., Snyder S.H. Nitric oxide: A physiologic messenger molecule. Ann. Rev. Biochem. 1994;63:175–195. doi: 10.1146/annurev.bi.63.070194.001135. [DOI] [PubMed] [Google Scholar]
- 19.Jaffrey S.R., Erdjument-Bromage H., Ferris C.D., Tempst P., Snyder S.H. Protein S-nitrosylation: a physiological signal for neuronal nitric oxide. Nat. Cell Biol. 2001;3:193–197. doi: 10.1038/35055104. [DOI] [PubMed] [Google Scholar]
- 20.Muscoli C., et al. Therapeutic manipulation of peroxynitrite attenuates the development of opiate-induced antinociceptive tolerance in mice. J. Clin. Invest. 2007;117:3530–3539. doi: 10.1172/JCI32420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kolesnikov Y.A., et al. Functionally differentiating two neuronal nitric oxide synthase isoforms through antisense mapping: Evidence for opposing NO actions on morphine analgesia and tolerance. Proc. Natl. Acad. Sci. U. S. A. 1997;94:8220–8225. doi: 10.1073/pnas.94.15.8220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Babey A.M., et al. Nitric oxide and opioid tolerance. Neuropharmacology. 1994;33:1463–1470. doi: 10.1016/0028-3908(94)90050-7. [DOI] [PubMed] [Google Scholar]