Abstract
Study Objectives:
Developed the Cleveland Adolescent Sleepiness Questionnaire (CASQ), a brief, self-completed instrument to measure excessive daytime sleepiness in adolescents.
Design:
Cross-sectional analysis.
Participants:
A subsample of 411 adolescents 11–17 years of age recruited from area schools, churches, and “control” participants in a sleep disordered breathing cohort study; a second subsample of 62 adolescents with diagnosed sleep disordered breathing also participating in the sleep disordered breathing study.
Measurements:
Participants completed the CASQ along with two other available measures of daytime sleepiness and other sleep parameters (sleep duration on school nights, sleep duration on non-school nights, and sleep debt, defined as non-school night sleep duration minus school-night sleep duration). Demographic information was obtained from a caregiver-completed questionnaire. The CASQ was developed using exploratory factor analysis, followed by confirmatory factor analysis using structural equation modeling techniques.
Results:
Goodness-of-fit measures for the final 16-item scale structure ranged from good to excellent. The CASQ's internal consistency was good (α = 0.89). Correlations between the CASQ, two other measures of daytime sleepiness, and sleep parameters gave preliminary evidence of the CASQ's construct validity.
Conclusion:
The CASQ shows promise as a valid measure of daytime sleepiness in adolescents.
Citation:
Spilsbury JC; Drotar D; Rosen CL et al. The cleveland adolescent sleepiness questionnaire: a new measure to assess excessive daytime sleepiness in adolescents.
Keywords: Daytime sleepiness, adolescents, measurement
Alarming numbers of U.S. adolescents experience excessive daytime sleepiness. Research of adolescent sleep habits indicates that anywhere between 54%–87% of adolescents are not getting enough sleep.1–4 Similar trends have also been observed among adolescents in other nations.5–7 Excessive daytime sleepiness has been linked to several problems in adolescents: increased aggression and other behavior problems; negative moods and difficulty controlling emotions, poorer academic performance; increased risk of injury, including accidents at work or behind the wheel; and increased use of caffeine, nicotine, and other stimulants.4,8–10 Reliable, easy-to-use questionnaires that assess sleepiness in adolescents may facilitate identification of clinically meaningful levels of sleepiness in pediatric practice, as well as provide research tools to gauge this important, prevalent symptom in the population.
Measuring excessive daytime sleepiness among adults has been greatly facilitated by the development of valid, simple, self-administered, and inexpensive measures such as the Epworth Sleepiness Scale (ESS).11 The ESS is brief, easily comprehensible, and has found widespread use in both clinical and research settings worldwide.
In contrast to adult measures, equally versatile assessment tools that are valid, practical (i.e., expense and time demands on staff, facilities, and patients/participants), and appropriate for use with adolescents have been less forthcoming. The laboratory-based multiple sleep latency test (MSLT) can be used for adults and adolescents alike.12–14 However, the MSLT involves a significant time demand and requires adequate testing facilities. The Pediatric Sleep Questionnaire–Sleepiness Subscale (PSQ-SS)15,16 contains a 4-item sleepiness subscale showing good psychometric properties, but the PSQ-SS is completed by a parent, which may not be possible or suitable in some clinical or research settings involving adolescents.
Concerning available, less costly self-report instruments for adolescents, one popular instrument, the School Sleep Habits Survey (SSHS),4 has a 15-item sleepiness subscale, in which adolescents rate the degree of “struggling to stay awake” in 10 situations, ranging from face-to-face conversations with others to driving a car. The SSHS has shown acceptable internal consistency as measured by Cronbach's alpha.17 Another instrument, The Pediatric Daytime Sleepiness Scale (PDSS)18 is a simple, 8-item instrument designed for use with children of middle-school age (11–15 years). Each item assesses the frequency of a sleep related behavior (e.g., how often do you fall asleep or get drowsy during class periods; are you usually alert most of the day; how often do you think you need more sleep) using a 5-point Likert type scale (0 = never, 4 = always). The PDSS has shown both acceptable internal consistency as well as expected associations with outcomes linked to sleepiness (e.g., decreased sleep time, poor grades, negative moods).
However, the PDSS and SSHS may have some potential limitations. The SSHS was not constructed using exploratory and confirmatory factor analytic techniques, which are generally recommended to develop psychometrically sound instruments.19 Moreover, although the SSHS has been used among adolescents 13–17 years of age, one of the items in the instrument – perceived sleepiness while driving a car – is not applicable to younger adolescents who are unable to drive. The PDSS is somewhat limited by its target age range (11–15 years of age). Also, although the instrument has been used with samples of adolescents who are overweight20 or epileptic,21 it has not been specifically tested with adolescents having known sleep problems. Moreover, some of the individual PDSS items actually contain 2 separate behaviors (e.g., fall asleep or get drowsy), which may, in fact, occur at very different rates and thereby create difficulties for some children to complete.
The purpose of the present study was to develop and validate a brief, easily comprehensible instrument – the Cleveland Adolescent Sleepiness Questionnaire (CASQ) – to measure daytime sleepiness in adolescents of a broader age range (11–17 years) than either the PDSS (11–15 years) or SSHS (13–17 years). Also, our approach to validation was designed to avoid some of the potential limitations of other available measures by (1) limiting each item in the instrument to one behavior/situation; (2) limiting questionnaire items to those that can be answered by children throughout the age range; (3) utilizing exploratory and confirmatory factor analyses to develop a scale with sound, verified structure; and (4) conducting the confirmatory factor analysis using structural equation modeling (SEM) techniques. SEM is a particularly effective method for evaluating the underlying structure of a measure because it allows investigators to specify causal relationships among observed and latent variables while simultaneously accounting for measurement error.22
We hypothesized that scores on the CASQ, ordered such that higher scores would indicate greater sleepiness, would: (1) positively correlate with child age; (2) negatively correlate with sleep duration; (3) positively correlate with sleep debt (defined as weekend sleep minus weekday sleep); and (4) positively correlate with existing sleepiness measures. Furthermore, we hypothesized that CASQ scores of adolescents with a diagnosed sleep disorder would be significantly greater than CASQ scores of adolescents without a diagnosed sleep disorder.
METHODS
Participants
Normative Sample
Adolescents were recruited from 3 different sources in order to obtain a broad representation of normative sleep behavior among adolescents from mixed socioeconomic backgrounds. First, families with adolescents attending 10 churches in the northeast Ohio region were invited to participate in the study during information meetings held at the churches. The second source of adolescents consisted of all students attending a public middle school and high school in a Cuyahoga County, Ohio community. The third source of adolescents for the normative sample consisted of participants in a community-based cohort study (Cleveland Sleep and Health Study; CSHS) who did not have evidence of sleep disordered breathing by objective overnight polysomnographic monitoring or reported snoring (see below). Construction of the study cohort has been described elsewhere.23
Sleep Disordered Breathing Sample
Adolescent participants in the CSHS who were classified with sleep disordered breathing —i.e., either obstructive sleep apnea (OSA) or primary snoring—constituted the sleep disorders sample. CSHS participants underwent full-channel overnight polysomnography, and procedures for scoring polysomnographic data have been described previously.24 Measures included the apnea-hypopnea index, or AHI, (total number of obstructive apneas plus hypopneas associated with ≥3% desaturation per hour of sleep) and sleep efficiency (percentage of sleep period spent asleep). OSA was defined as an AHI ≥5 events per hour and/or an obstructive apnea index ≥1 event per hour. Adolescents without OSA were categorized as having primary snoring if the caregiver answered “yes” to the statement that the adolescent had “loud snoring the past month” at least 1 to 2 times per week.
Procedure
Following informational meetings at the churches and schools (targeting parents of potentially participating adolescents at adult Sunday school classes and school PTA meetings, respectively), study packets containing letters explaining the study to parents and adolescents, study information forms, questionnaires, and stamped return envelopes were distributed to (a) all church families with an adolescent in the age range 11–17 years of age; and (b) all students attending the middle school and high school. Adolescents participating in the CSHS completed study instruments as part of the cohort study protocol, and one of their parents completed the demographic questionnaire.
All adolescents completed 3 questionnaires: the CASQ, the PDSS, and the SSHS. In the case of the SSHS sleepiness subscale, one item that involved sleepiness while driving a car was not included in computing an overall sleepiness score because many of the participants were below the legal age of driving. The SSHS collects information about usual bedtime, waketime, and “time it takes to fall asleep” for both school nights and weekends (no school the next day), thereby permitting calculation of usual nightly sleep duration for weekdays and weekends (length of time between bedtime and waketime, minus the time it takes to fall asleep). Sleep debt was calculated as weekend sleep duration minus weekday sleep duration.
Overview of CASQ Construction
The CASQ was constructed based upon recommended procedures for creating a psychosocial instrument19: (1) initial selection of items based on empirical evidence and theory; (2) pretesting of items and response format for readability and comprehension, with scale modification as needed; (3) administration of the questionnaire to a normative sample of adolescents; (4) using a split sample approach, exploratory factor analysis (EFA) to identify the underlying scale structure on one-half of the normative sample; (4) confirmatory factor analysis (CFA) using SEM to test the scale structure established by the EFA on the remaining half of the sample, with scale modification as needed; (5) internal consistency and validity analyses utilizing the modified scale.
Initial Selection & Pretesting of CASQ Items
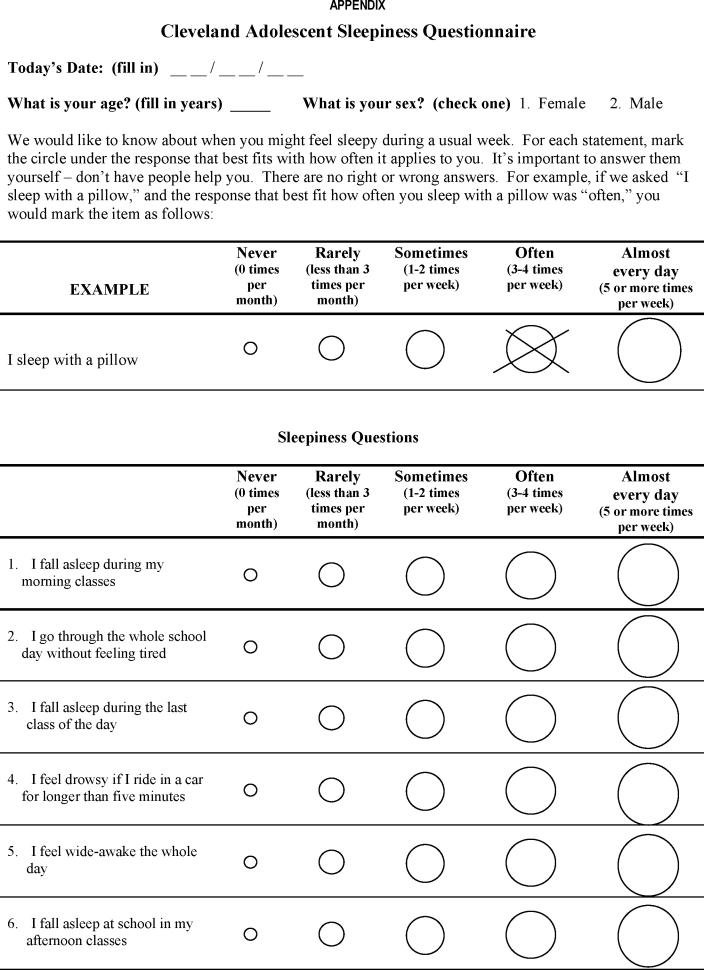
Forty-six potential items were generated based on theory and research findings on sleepiness as well as review of other sleepiness instruments. Items consisted of a range of situations when an adolescent might feel sleepy or fall asleep (e.g., I fall asleep during the last class of the day). In complementary fashion, several items were worded to assess feeling “wide awake” or “alert” (e.g., I feel wide awake the last class of the day). A Likert-type response format was designed to indicate the frequency of each behavior occurring during a usual week: never (0 times per month); rarely (<3 times per month); sometimes (1–2 times per week); often (3–4 times per week); almost every day (5 or more times per week). CASQ responses were assigned a numerical value (1 = never, 5 = almost every day) and then summed to produce an overall score. Items involving alertness or feeling “wide awake” were reverse coded before summing. Higher scores on the CASQ reflect greater sleepiness.
Four experts in adolescent sleep medicine reviewed the list and rated items according to their relevance in measuring the sleepiness construct. A tentative list of 40 items was then individually pre-tested on a convenience sample of 23 children, focusing on comprehension and readability of items and the response format. Based on their recommendations, the questionnaire was reduced to 35 items.
Analysis
The normative sample was split approximately in half, and an EFA using a principal axis extraction and varimax rotation was conducted to identify the underlying factor structure of adolescents' responses to the CASQ items. The critical eigenvalues were set at 1. PEDS items were removed if they failed to load on any factor (loading < 0.40) or had unacceptably high secondary loadings (>0.30). Based on examination of the factor loadings, the least acceptable item was removed, and the analysis was re-run with the remaining items. The EFA continued in this manner until all remaining items had a primary factor loading > 0.40 and secondary loadings < 0.30. In each re-analysis, alternative factor solutions (up to 2 factors above and below the number of factors extracted when critical eigenvalues were set to 1) were also examined. EFA analyses were repeated using a direct oblimin rotation in order to compare final factor structures when factors were allowed to be correlated. The EFA was conducted using SPSS 13.0. (SPSS, Inc, Chicago, IL).
Next, we conducted a CFA on the remaining half of the normative sample using a structural equation modeling (SEM) software program AMOS 5.0 (Analysis of Moment Structures Version 5, Smallwaters Corporation). Model fit was assessed by 3 standard measures: the Tucker-Lewis Index (TLI), the Comparative Fit Index (CFI), and the Root Mean Square Error of Approximation (RMSEA). For the first 2 measures, values close to 1 indicate a well-fitting model, with >0.90 considered as the cut-off for an acceptable model and >0.95 an excellent model.25 For the RMSEA, a value as close to 0 as possible is desirable; <0.08 is considered reasonable and <0.05 excellent.26 To finalize the scale structure, modifications were made based on modification indices calculated by AMOS.
After finalization of the scale structure, a series of one-way ANOVAs were performed to test for CASQ score differences in the normative sample by child sex and ethnicity. Pearson correlation coefficients were calculated to determine the association between the scale scores and child age and family income. Cronbach alpha coefficients were calculated to assess the scale's internal consistency.
Three analyses were conducted to make preliminary assessments of the scale's validity. First, Pearson correlation coefficients were calculated to determine the association between CASQ scores and average reported sleep duration on schooldays and on weekends, sleep debt (difference in average sleep duration on weekends versus weekdays), child age, as well as scores on the PDSS and SSHS. Second, a series of one-way ANOVAs were conducted to compare the CASQ, PDSS, and SSHS scores of 3 groups of adolescent participants in the sleep apnea cohort study: OSA vs. primary snorers vs. “normal controls.” In cases where the overall ANOVA was statistically significant, post-hoc comparisons (Fisher's least-significant-difference tests) were conducted to identify significant differences among the 3 groups. We limited ANOVA analyses to participants in the cohort study because the presence or absence of a diagnosed sleep disorder was known among these adolescents, unlike study participants from churches or schools. Third, for adolescents participating in the sleep apnea cohort study, Spearman correlation coefficients were calculated to determine the association between CASQ scores and polysomnography-measured AHI and sleep efficiency. Spearman correlation coefficients were used instead of Pearson coefficients because of the skewed distributions of AHI and sleep efficiency. Correlations and ANOVA were conducted using SPSS 13.0.
RESULTS
Sample Characteristics
Normative Subsample
A total of 411 adolescents comprised the normative sample. Most (n=193, 47.0%) of the normative sample was recruited from the 2 public schools, followed by controls from the sleep disordered breathing cohort study (n=127, 30.9%) and churches (n=91, 22.1%). Participation rates for the schools and churches were 8% and 28%, respectively. It should be noted that the sample was not intended to be representative of specific schools or churches; rather, we hoped that by recruiting individuals from several sources, we would obtain a broad representation of children.
Characteristics of the normative sample are reported in Table 1. The average age of adolescent participants was 13.9 ± 1.6 years. Slightly less than half the sample (46.2%) was male. Most of the sample reported being either of White/European American ethnicity (72.4%) or African American (21.3%). Twenty-one percent of the sample reported an annual family income equal or less than $30,000, and 39% reported an annual income > $70,000. Nearly three-quarters of adolescents (71.4%) came from households with married spouses. Participating caregivers were mostly mothers (86.5%) with an average age of 43.5 ± 7.0 years. Nearly all caregivers had completed high school (92.7%), and nearly half (48.1%) had completed a college degree or more. Mean sleep duration for the normative subsample was 7.7 ± 1.2 hours on school nights and 9.4 ± 1.5 on weekends. Mean sleep debt for the subsample was 1.7 ± 1.7 hours.
Table 1.
Demographic and Sleep Characteristics of Participants
| Characteristic | Normative Subsamplea (n=411) | Cohort Study |
|||
|---|---|---|---|---|---|
| OSA (n=18) | Primary Snorers (n=44) | Control (n=127) | p | ||
| Demographic | |||||
| Adolescent age in years, mean (SD) | 13.9 (1.6) | 13.1 (0.8) | 13.8 (1.2) | 13.3 (0.8) | 0.007 |
| Caregiver age in years, mean (SD) | 43.5 (7.0) | 41.4 (4.8) | 42.7 (10.6) | 43.1 (7.6) | 0.71 |
| Adolescent male sex (%) | 46.2 | 88.2 | 53.7 | 54.7 | 0.027 |
| Adolescent African American ethnicity (%) | 21.3 | 64.7 | 68.4 | 65.8 | 0.95 |
| Caregiver completing high school (%) | 92.7 | 88.9 | 80.0 | 83.6 | 0.70 |
| Caregiver completing college (%) | 48.1 | 33.3 | 25.0 | 34.5 | 0.54 |
| Caregiver married (%) | 72.4 | 61.1 | 40.0 | 53.4 | 0.23 |
| Family median annual income range ($) | 50,001–60,000 | 30,001–40,000 | 30,001–40,000 | 30,001–40,000 | 0.67 |
| Adolescent Sleep | |||||
| Mean duration school nights in hours, mean (SD) | 7.7 (1.2) | 7.9 (1.2) | 7.9 (1.5) | 8.2 (1.2) | 0.51 |
| Mean duration non-school nights in hours, mean (SD) | 9.4 (1.5) | 8.6 (2.5) | 9.4 (1.8) | 9.5 (1.5) | 0.10 |
| Sleep debt in hours, mean (SD) | 1.7 (1.7) | 0.70 (1.9) | 1.4 (2.0) | 1.3 (1.8) | 0.41 |
| Sleep efficiency, median | ---------- | 89.5 | 91.4 | 91.2 | 0.89 |
| (IQR) | (86.5–95.2) | (85.1–95.0) | (85.6–94.5) | ||
| AHI, median | ---------- | 14.3 | 0.8 | 0.4 | < 0.001 |
| (IQR) | (6.7–24.6) | (0.3–1.2) | (0.1–1.2) | ||
AHI=Apnea-Hypopnea Index. IQR = Interquartile range.
The normative subsample consists of participants recruited from schools (n=193), churches (n=91), and cohort controls (n=127).
Sleep Disordered Breathing Subsample
Sixty-two adolescents with sleep disordered breathing who were participating in the cohort study were recruited into the sleep disorders subsample: 18 with OSA and 44 with primary snoring. Comparisons of the OSA, primary snorers, and control groups recruited from the CSHS (Table 1) revealed that these 3 groups did not significantly differ by child ethnicity, family income, caregiver age, caregiver education, caregiver marital status (married vs. nonmarried), or in weekday sleep duration, weekend sleep duration, sleep debt, or sleep efficiency. Primary snorers (average age = 13.8 years) were slightly older than either control-group adolescents (13.3 years) or adolescents with OSA (13.1 years), F=5.106, p = 0.007. Also, a larger percentage of adolescents with OSA were boys (88.2%) compared to primary snorers (53.7%) or controls (54.7%), χ2 (2 df) = 7.2, p = 0.027. As might be expected, the OSA group's median AHI (14.3) was greater than that of the primary snorers (0.8) or controls (0.4), Kruskal-Wallis χ2 (2 df) = 51.2, p <0.001.
Exploratory & Confirmatory Factor Analysis
The EFA using approximately half of the normative sample (n=181) revealed a final solution consisting of 4 factors that explained 55% of the variance. The 4 factors were labeled “sleep in school,” “alert in school,” “sleep in the evening,” and “sleep during transport.” Re-analysis allowing factors to be correlated (oblique rotation) produced virtually identical results (one additional item loading on the factor “alert in school”). Composition of the factors and item loadings are presented in Table 2. Only the psychometric properties of the CASQ total score are analyzed in this study.
Table 2.
Results of Exploratory Factor Analysis (n = 181): Factors and Factor loadings
| CASQ Item | Factor 1 Sleep in school | Factor 2 Alert in school | Factor 3 Sleep in evening | Factor 4 Sleep in transport |
|---|---|---|---|---|
| Sq17 Fall asleep in morning at school | 0.777 | 0.079 | .228 | 0.191 |
| Sq3 Fall asleep in afternoon classes | 0.722 | 0.179 | −0.069 | 0.044 |
| Sq25 During school day, realize just fell asleep | 0.719 | 0.134 | 0.194 | 0.226 |
| Sq5 Fall asleep morning classes | 0.719 | 0.057 | 0.248 | 0.151 |
| Sq2 Fall asleep last class | 0.543 | 0.207 | −0.017 | 0.050 |
| Sq29 When in class, wide awake | 0.257 | 0.746 | 0.275 | 0.142 |
| Sq4 Wide-awake whole day | 0.139 | 0.736 | 0.245 | 0.237 |
| Sq7 Wide awake last class of day | 0.102 | 0.707 | 0.062 | 0.080 |
| Sq12 Feel alert during classes | 0.125 | 0.519 | 0.298 | 0.004 |
| Sq1 Go through whole school day without feeling tired | 0.108 | 0.497 | 0.061 | 0.206 |
| Sq18 Feel sleepy doing homework in the evening | 0.041 | 0.267 | 0.790 | 0.096 |
| Sq31 Fall asleep during schoolwork at home in evening | 0.272 | 0.127 | 0.700 | 0.272 |
| Sq9 Sleepy in evening after school | 0.090 | 0.279 | 0.507 | 0.174 |
| Sq28 Fall asleep when ride bus, car, train | 0.235 | 0.175 | 0.102 | 0.748 |
| Sq13 Feel drowsy in car > 5 minutes | 0.042 | 0.103 | 0.224 | 0.725 |
| Sq14 Feel sleepy on bus trip for school event | 0.214 | 0.216 | 0.112 | 0.584 |
CFA using the remainder of the normative sample (n=230) and SEM revealed an unsatisfactory fit: χ2 = 9.7; df = 98; TLI = 0.877, CFI = 0.911; RMSEA = 0.077. Re-analysis of the CFA using only cases with complete CASQ data (n=218) provided virtually identical goodness of fit measures as the initial CFA and allowed for calculation of modification indices, which indicate relationships between variables that, if specified in the model, may result in a better overall fit. Modification of the model based on these indices resulted in a final model that is presented in Figure 1 (error terms not shown). The goodness of fit measures ranged from good (TLI = 0.939 and RMSEA = 0.059) to excellent (CFI = 0.951).
Figure 1.
Final Model based on SEM (standardized values, n=218)
Note: Error Terms not shown
SEM = Structural Equation Modeling, DF = Degrees of Freedom, TLI = Tucker-Lewis Index, CFI = Comparative Fit Index, RMSEA = Root Mean
Square Error of Approximation
CASQ's Psychometric Properties –Normative Subsample
The means, standard deviations, and Cronbach alpha coefficients of the CASQ total score, PDSS, and SSHS for the normative sample are presented in Table 3. The internal consistency of the CASQ total score was good: Cronbach's alpha = 0.89, and comparable or slightly higher than that for the PDSS or SSHS.
Table 3.
Means, Medians, and Alpha Coefficients for Sleepiness Measures (Normative Sample)
| Mean (SD) | Median (IQR) | Cronbach's α | |
|---|---|---|---|
| CASQ | 35.2 (11.0) | 34.0 (26.0–43.0) | 0.89 |
| PDSS | 15.3 (6.4) | 15.0 (10.0–20.0) | 0.81 |
| SSHS | 13.0 (3.6) | 12.0 (10.0–15.0) | 0.70 |
CASQ=Cleveland Adolescent Sleepiness Questionnaire, PDSS = Pediatric Daytime Sleepiness Scale, SHSS=Sleep Habits School Survey, SD = Standard Deviation, IQR = Interquartile Range
Per our hypothesis, CASQ scores were significantly correlated with age: r = 0.360, p < 0.001. Comparisons of total CASQ score by gender revealed that girls scored significantly higher than did boys: 36.5 ± 11.1 vs. 33.4 ± 10.8, t = 2.69, p = 0.008. Comparisons by child ethnicity revealed no significant difference in white vs. African American children's mean CASQ scores. The small number of children of other ethnic background precluded additional comparisons by ethnicity.
Correlations Between Sleepiness Measures and Sleep Characteristics
Per our hypotheses, CASQ total score was negatively correlated with sleep duration on school nights both in the normative and sleep disorders samples (Table 4). Our hypothesized relationship between CASQ and sleep debt was partially confirmed: CASQ was positively correlated with sleep debt in the normative sample. However, in the sleep disordered breathing sample, where factors other than sleep duration may impact sleepiness, no such relationship was observed.
Table 4.
Pearson Correlation Coefficients between Sleepiness Measures and Sleep Characteristics
| Sample | Measure | Sleep Duration School Night | Sleep Duration Non-School Night | Sleep Debt |
|---|---|---|---|---|
| Normative | ||||
| (n=411) | CASQ | −0.40*** | −0.05 | 0.24*** |
| PDSS | −0.33*** | −0.02 | 0.22*** | |
| SSHS | −0.37*** | −0.02 | 0.23*** | |
| Sleep | ||||
| Disorders | CASQ | −0.34** | −0.02 | 0.20 |
| (n=62) | PDSS | −0.24 | 0.14 | 0.29* |
| SSHS | −0.18 | −0.07 | 0.05 |
*p <0.05 **p <0.01 ***p <0.001
Similar to the CASQ, the PDSS and SSHS were also negatively correlated with sleep duration on school nights and positively correlated with sleep debt among the normative sample. However, in the sleep disordered breathing sample, neither the PDSS nor the SSHS significantly correlated with sleep duration on school nights, but the PDSS was significantly correlated with sleep debt. None of the 3 sleepiness measures correlated with adolescents' reported sleep duration on non-school nights.
Correlations Among Sleepiness Measures
As predicted, CASQ was highly positively correlated with scores of PDSS and SSHS in both the normative and sleep disorder samples (Table 5).
Table 5.
Pearson Correlation Coefficients Among Sleepiness Measures
| Sample | Measure | CASQ | PDSS |
|---|---|---|---|
| Normative Sample | CASQ | ||
| (n=411) | PDSS | 0.75*** | |
| SSHS | 0.72*** | 0.55*** | |
| Sleep Disorders Sample | CASQ | ||
| (n=62) | PDSS | 0.70*** | |
| SSHS | 0.66*** | 0.47*** |
*p <0.05 **p <0.01 ***p <0.001
Sleepiness and Sleep Measures in Adolescents With Vs. Without A Diagnosed Sleep Disorder
We compared CASQ, PDSS, and SSHS scores of adolescents with a known sleep disorder (cases of OSA or primary snoring in the cohort study) versus adolescent participants in the cohort study without a diagnosed sleep disorder. ANOVA results revealed that overall Fs for all 3 sleep measures were statistically significant (Table 6). In support of our hypothesis, post hoc comparisons revealed that CASQ scores for the adolescents with either primary snoring or OSA were significantly greater than those without these sleep disorders. Post hoc comparisons of PDSS scores revealed one significant difference: greater scores among primary snorers than the control adolescents. Post hoc comparison of SSHS scores revealed that the children with OSA had significantly greater scores than the primary snorers and the control adolescents, but scores between the control adolescents and primary snorers were not significantly different.
Table 6.
Comparison of Sleepiness Measure Scores: Controls (No Diagnosed Sleep Disorders) vs. Primary Snorers vs. Sleep Apnea.
| Measure | Subsample | N | M | SD | F | p value |
|---|---|---|---|---|---|---|
| Controls | 115 | 31.2a | 9.4 | |||
| CASQ | Primary snorers | 43 | 35.0 | 12.3 | 4.373 | 0.01 |
| Sleep apnea | 18 | 37.7 | 11.5 | |||
| Controls | 123 | 12.2b | 5.3 | |||
| PDSS | Primary snorers | 43 | 14.7 | 5.5 | 3.909 | 0.02 |
| Sleep apnea | 17 | 14.1 | 6.2 | |||
| Controls | 119 | 12.2c | 3.3 | |||
| SHSS | Primary snorers | 43 | 12.7 | 3.2 | 8.250 | < 0.001 |
| Sleep apnea | 17 | 16.1 | 6.9 |
Controls < primary snorers; controls < sleep apnea
Controls < primary snorers
Controls < sleep apnea; primary snorers < sleep apnea
Additional analyses of polysomnography-derived sleep measures among cohort study participants revealed that the CASQ was weakly, although significantly correlated with the AHI (Spearman's ρ = 0.16, p = 0.04) and marginally associated with sleep efficiency (ρ = −0.15, p = 0.06) (Table 7). The SSHS was marginally associated with the AHI (ρ = 0.13, p = 0.08) and not associated with sleep efficiency. The PDSS was not significantly associated with either of the polysomnographic measures.
Table 7.
Spearman Correlation Coefficients Between Sleepiness Measures and Polysomnographic Measures
| Sleepiness Measure | Polysomnographic Measure |
|||
|---|---|---|---|---|
| AHI |
Sleep Efficiency |
|||
| ρ | p value | ρ | p value | |
| CASQ | 0.16 | 0.04 | −0.15 | 0.06 |
| PDSS | 0.05 | 0.50 | −0.02 | 0.81 |
| SSHS | 0.13 | 0.08 | −0.05 | 0.55 |
AHI=Apnea-Hypopnea Index
DISCUSSION
The present study constructed the CASQ, a measure of daytime sleepiness for use with 11–17 year-old adolescents. The CASQ's internal consistency was good, and preliminary evidence indicated that the CASQ has construct validity. Per study hypotheses, greater CASQ scores, reflecting increased daytime sleepiness, were significantly associated with decreased sleep duration in both normative and sleep disorder samples, as well as with increased sleep debt in the normative sample. The reason for the lack of a significant association between CASQ scores and sleep debt among adolescents with a sleep disorder was not clear, though the small sample size may have been a factor.
As hypothesized, CASQ scores were also positively correlated with age, congruent with other reports of increased daytime sleepiness with increasing age across adolescence.4,18 Furthermore, the CASQ displayed convergent validity by its strong positive correlations with 2 other available measures of daytime sleepiness, the PDSS and SSHS.
Our hypothesis that adolescents with sleep disordered breathing, presumably a group with increased daytime sleepiness, would have higher CASQ scores than adolescents without sleep disordered breathing was also confirmed; the CASQ detected differences in daytime sleepiness between both normal controls and primary snorers, and between normal controls and adolescents with OSA. This finding is consistent with a previous report of greater behavioral morbidity in both primary snorers and children with OSA compared to controls in this cohort.27 In contrast to the CASQ, the PDSS did not detect significant differences in sleepiness between adolescent controls and those with OSA, while the SSHS did not detect differences between primary snorers and controls.
Furthermore, the CASQ was associated, albeit weakly, with objective measures derived from polysomnography (AHI and sleep efficiency). Although objective and subjective measures of sleep disturbances are often only weakly associated, the associations observed in this study were consistent with our hypotheses and are supportive of the CASQ's construct validity.
Study limitations should be noted. First, participation of adolescents recruited from schools and churches was low, resulting in a sample that may not have adequately represented the range of normative sleep behavior in this age group. Second, the study did not utilize an objective measure of excessive daytime sleepiness (e.g., the MSLT12), and use of an objective measure related to sleep duration (efficiency) was limited to CSHS participants. On the other hand, use of a subjective measure such as a self-completed questionnaire or diary has produced estimates of sleep duration consistent with an objective measure such as actigraphy.28
Nevertheless, future research should examine the association between the CASQ and additional objective measures of sleepiness and sleep duration. Additional studies should also include participants with greater social and ethnic diversity, which would permit more precise estimates of the CASQ's psychometric properties for various subpopulations of adolescents, including estimates of individual properties of the CASQ's 4 factors (subscales). Also, adolescents with a known sleep problem potentially leading to daytime sleepiness were limited to those with sleep disordered breathing.
Future CASQ research should include adolescents with other sleep disorders or problems (e.g., insomnia, narcolepsy), and the ability of the CASQ to discriminate among other sleep disorders should also be evaluated. Administering the CASQ to groups of adolescents with other known sleep disorders would provide additional information about clinically significant score cut-off points. Having a brief, valid, and inexpensive measure of daytime sleepiness at their disposal would enable clinicians to avoid the more costly and burdensome MSLT. Such an instrument could also be used as a simple, inexpensive way to monitor patient responses to treatment for sleep problems or disorders.
The CASQ is freely available (appendix), and we invite clinicians and researchers to use the measure and to share their findings with us so that the CASQ may be improved.
ACKNOWLEDGMENTS
This study was supported by grants RR02326402, 5T32HD041923, and HL070916 from the National Institutes of Health, Bethesda, MD. We gratefully acknowledge the assistance of Judy Owens, Tonya Palermo, and Kingman Strohl.
List of Abbreviations
- AHI
Apnea-Hypopnea Index
- CASQ
Cleveland Adolescent Sleepiness Questionnaire
- CFA
Confirmatory Factor Analysis
- CFI
Comparative Fit Index
- CSHS
Cleveland Sleep and Health Study
- EFA
Exploratory Factor Analysis
- IQR
Interquartile Range
- OSA
Obstructive Sleep Apnea
- PDSS
Pediatric Daytime Sleepiness Scale
- RMSEA
Root Mean Square Error of Approximation
- SD
Standard Deviation
- SEC
Structural Equation Modeling
- SSHS
School Sleep Habits Survey
- TLI
Tucker-Lewis Index
Appendix
Footnotes
Disclosure Statement
This was not an industry supported study. Dr. Rosen has received research support from Cephalon. The other authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Mercer PW, Merritt SL, Cowell JM. Differences in reported sleep need among adolescents. J Adolesc Health. 1998;23:259–63. doi: 10.1016/s1054-139x(98)00037-8. [DOI] [PubMed] [Google Scholar]
- 2.2006 Sleep in America Poll. Washington, DC: National Sleep Foundation; [Last accessed November 16, 2006]. Available at http://www.sleepfoundation.org/_content/hottopics/2006_summary_of_findings.pdf. [Google Scholar]
- 3.Strauch I, Meier B. Sleep needs in adolescents: a longitudinal approach. Sleep. 1988;11:378–86. doi: 10.1093/sleep/11.4.378. [DOI] [PubMed] [Google Scholar]
- 4.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–87. [PubMed] [Google Scholar]
- 5.Reid A, Maldonado CC, Baker FC. Sleep behavior of South African adolescents. Sleep. 2002;25:423–7. [PubMed] [Google Scholar]
- 6.Takaubu T, Kanbayashi T, Tutsui K, et al. Sleep habits of students attending elementary schools, and junior and senior high schools in Akita prefecture. Psychiatry Clin Neurosci. 2002;56:241–2. doi: 10.1046/j.1440-1819.2002.01013.x. [DOI] [PubMed] [Google Scholar]
- 7.Tynjala J, Kannas L, Valimaa R. How young Europeans sleep. Health Educ Res. 1993;8:69–80. doi: 10.1093/her/8.1.69. [DOI] [PubMed] [Google Scholar]
- 8.Carskadon MA. Patterns of sleep and sleepiness in adolescents. Pediatrician. 1990;17:5–12. [PubMed] [Google Scholar]
- 9.Dahl RE, Lewin DS. Pathways to adolescent health: sleep regulation and behavior. J Adolesc Health. 2002;31:S175–84. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 10.Mitru G, Millrood DL, Mateika JH. The impact of sleep on learning and behavior in adolescents. Teachers College Rec. 2002;104:704–26. [Google Scholar]
- 11.Johns MW. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–5. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 12.Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S. Guidelines for the Multiple Sleep Latency Test (MSLT): a standard measure of sleepiness. Sleep. 1986;9:519–24. doi: 10.1093/sleep/9.4.519. [DOI] [PubMed] [Google Scholar]
- 13.Thorpy MJ, Wesbrook P, Ferber R, et al. The clinical use of the Multiple Sleep Latency Test. Sleep. 1992;15:268–76. doi: 10.1093/sleep/15.3.268. [DOI] [PubMed] [Google Scholar]
- 14.Mysliwiec V, Henderson JH, Strollo PJ., Jr . Epidemiology, consequences, and evaluation of excessive daytime sleepiness. In: Lee-Chiong TL, Sateia MJ, Carskadon MA, editors. Sleep medicine. Philadelphia: Hanley & Belfus, Inc.; 2002. pp. 187–92. [Google Scholar]
- 15.Chervin RD, Hedger K, Dillon JE, Pituch KJ. Pediatric Sleep Questionnaire (PSQ): Validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med. 2000;1:21–32. doi: 10.1016/s1389-9457(99)00009-x. [DOI] [PubMed] [Google Scholar]
- 16.Chervin RD, Weatherly RA, Ruzicka DL, et al. Subjective sleepiness and polysomnographic correlates in children scheduled for adenotonsillectomy vs other surgical care. Sleep. 2006;29:495–503. [PMC free article] [PubMed] [Google Scholar]
- 17.Carskadon MA, Seifer R, Acebo C. Reliability of six scales in a sleep questionnaire for adolescents. Sleep Res. 1991;20:421A. [Google Scholar]
- 18.Drake C, Nickel C, Burduvali E, Roth T, Jefferson C, Badia P. The Pediatric Daytime Sleepiness Scale (PDSS): sleep habits and school outcomes in middle-school children. Sleep. 2003;26:455–8. [PubMed] [Google Scholar]
- 19.DeVellis RF. Newbury Park, CA: Sage; 1991. Scale Development: Theory and Applications. [Google Scholar]
- 20.Beebe DW, Lewin D, Zeller M, et al. Sleep in overweight adolescents: shorter sleep, poorer sleep quality, sleepiness, and sleep-disordered breathing. J Pediatr Psychol. 2007;32:69–79. doi: 10.1093/jpepsy/jsj104. [DOI] [PubMed] [Google Scholar]
- 21.Maganti R, Hausman N, Koehn M, Sandok E, Glurich I, Mukesh BN. Excessive daytime sleepiness and sleep complaints among children with epilepsy. Epilepsy Behav. 2006;8:272–7. doi: 10.1016/j.yebeh.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Byrne BM. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. Structural Equation Modeling with AMOS. [Google Scholar]
- 23.Rosen CL, Larkin EK, Kirchner HL, et al. Prevalence and risk factors for sleep-disordered breathing in 8- to 11-year-old children: association with race and prematurity. J Pediatr. 2003;142:383–9. doi: 10.1067/mpd.2003.28. [DOI] [PubMed] [Google Scholar]
- 24.Quan SF, Howard BV, Iber C, et al. The Sleep Heart Health Study: design, rationale, and methods. Sleep. 1997;20:1077–85. [PubMed] [Google Scholar]
- 25.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–606. [Google Scholar]
- 16.Brown MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 445–455. [Google Scholar]
- 27.Rosen CL, Storfer-Isser A, Taylor HG, Kirchner HL, Emancipator JL, Redline S. Increased behavioral morbidity in school-aged children with sleep-disordered breathing. Pediatrics. 2004;114:1640–8. doi: 10.1542/peds.2004-0103. [DOI] [PubMed] [Google Scholar]
- 28.Wolfson AR, Carskadon MA, Acebo C, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26:213–6. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]