Abstract
Background
People with severe mental health problems receive less effective care for some physical conditions. There is concern that this could apply to rectal bleeding or postmenopausal bleeding. Published estimates of consultation rates and outcomes for these symptoms vary widely.
Aim
To estimate rates of first-ever consultation for rectal bleeding and postmenopausal bleeding in general practice, together with subsequent referrals and outcomes. To identify inequalities for patients with severe mental health problems.
Design of study
Cohort study.
Setting
Primary care.
Method
Patients with first-ever consultations for rectal or postmenopausal bleeding were identified among more than 3 million patients from 328 practices contributing routine data to the QRESEARCH database. Their records were followed for 2 years.
Results
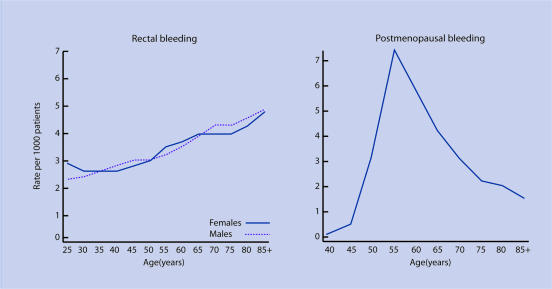
There were 30 175 first consultations for rectal bleeding (2.6 per thousand patients per year at age 25–29 years, rising to 4.8 over age 85 years) and 10 142 for postmenopausal bleeding (highest at 7.4 per thousand per year aged 55–59 years). Overall, 2.2% of those with rectal bleeding and 1.7% of those with postmenopausal bleeding went on to have a relevant cancer diagnosis within 2 years. Cancer risk was strongly related to age, and was higher for males with rectal bleeding than females with rectal bleeding. Recorded referrals were at similar rates among patients with and without severe mental health problems.
Conclusion
The rate of first consultations for rectal bleeding or postmenopausal bleeding is relatively low. Less than 2.5% overall have a relevant cancer diagnosis within 2 years. There is no evidence of inequality in referral for patients with severe mental health problems.
Keywords: mental health, neoplasms, postmenopause, primary health care, rectal diseases
INTRODUCTION
Abnormal bleeding can be a cardinal symptom of malignancy and will usually be first reported in the primary care setting.1 GPs need to identify patients requiring further investigation as soon as possible, but should avoid subjecting large numbers of patients to unnecessary investigations.
A study was undertaken to determine consultation rates and outcomes of rectal bleeding and postmenopausal bleeding in primary care. The initial focus was on possible inequalities for people with mental health problems who are known to receive less effective care for some physical conditions.2,3 Reasons for less effective care could include communication difficulties, patients with mental health problems giving lower priority to their own health,2 misunderstandings of patients with mental health problems in general medical settings,3 or a failure to reach mental health patients with health promotion information.4 There was concern that patients with rectal or postmenopausal bleeding and severe mental health problems could be managed less effectively. On reviewing the literature, there was little published information on consultation rates and outcomes for rectal or postmenopausal bleeding in general practice. Therefore, the current researchers decided to conduct a more general study of consultation for rectal and postmenopausal bleeding in primary care. Factors to consider are the extent of recorded referrals and the likelihood of a subsequent cancer diagnosis.
How this fits in
Estimated rates of rectal bleeding and postmenopausal bleeding in primary care vary widely. People with severe mental health problems receive less effective care for some physical conditions. This study provides robust age- and sex-specific rates of first consultations for rectal bleeding and postmenopausal bleeding, based on a total number of over 3 million patients' routine primary care records. Age- and sex-specific rates of relevant referrals and cancer diagnoses in the 2 years following first consultation are also given. There is no evidence of inequality for patients with severe mental health problems.
Existing studies of population rates for rectal or postmenopausal bleeding were mainly based on questionnaire surveys, which could be open to bias, (due to selection, non-response or poor recall) or had relatively small samples.5,6 While several studies reported the proportion of patients with rectal or postmenopausal bleeding who subsequently developed bowel or uterine cancer, many were based on patients already referred to secondary care.7,8 The current study aimed to identify patients with first-ever primary care consultations for rectal bleeding or postmenopausal bleeding and to follow them for 2 years, using routine electronic medical records held in the QRESEARCH database, which has a good coverage of the UK primary care system.9 The study aimed to compare patients with and without severe mental health problems in terms of referral rates and outcomes.
METHOD
Data
This cohort study was based on computerised patient records of general practices contributing to the QRESEARCH database, which currently contains the records of over 9 million patients who have ever been registered with 518 general practices throughout England, Wales, Scotland, and Northern Ireland. It has been validated by comparing birth, death, consultation, prevalence, and mortality rates with other data sources providing national general practice statistics. The age–sex structure of the population has been compared with the 2001 census.10 There was good correspondence for all of these measures, although in some instances QRESEARCH prevalence figures are marginally higher than less recent data.11 Practices taking part in regional research networks are similar to non-participating practices in their patient demographics, morbidity, mortality, and access to secondary care.12 Detailed analyses have shown good levels of completeness and consistency.13
For this study, practices were included if they had been using current EMIS computer systems (Egton Medical Information Systems) before 1 April 1998 and had complete data up to 1 April 2005. Patients were included if they were registered with an eligible practice at any time between 1 April 1998 and 31 March 2003, had been registered with the practice for at least 12 months, and had a first-ever consultation for rectal bleeding or postmenopausal bleeding between 1 April 1998 and 31 March 2003.
The following information was extracted for individual patients at the time of their first consultation for bleeding:
Personal and area demographics
Age, sex, and Townsend deprivation score for output area (quintile scores 1–5 based on national levels; 5 indicating high deprivation).
General characteristics
Most recent body mass index (BMI), smoking status, and blood pressure.
Severe mental health problems
Diagnosis of schizophrenia, bipolar disorder, or learning difficulties prior to first consultation for bleeding; depression diagnosed at least 5 years prior to first consultation for bleeding.
Comorbid physical conditions
Prior diagnosis of coronary heart disease, stroke, diabetes, chronic obstructive pulmonary disease, asthma, or cancer.
Medications
For patients with postmenopausal bleeding only, any prior recorded hormone replacement therapy (HRT) or tamoxifen; for patients with diagnosis of depression, any prior recorded antidepressant prescriptions.
Outcomes
Relevant referrals, investigations, cancer diagnoses, surgery, or death within the 2-year follow-up period. For rectal bleeding, relevant referrals were general surgery, gastroenterology, and radiooncology; relevant cancer was colorectal. For postmenopausal bleeding, relevant referrals and investigations were gynaecology, hysteroscopy and radio-oncology; relevant cancer was endometrial.
Statistical methods
Consultation rates were based on patients aged at least 25 years for rectal bleeding or at least 40 years for postmenopausal bleeding with a first-ever consultation for these symptoms in their medical record during the study period. For the analyses of relevant referrals, cancer diagnoses, and surgery, patients were excluded if they had a previous record of relevant cancer, as the expected management and outcomes of the bleeding would be different in these patients. Patients were classified as having a severe mental health problem if they had a pre-existing diagnosis of schizophrenia, bipolar disorder, or learning difficulties, or if they had long-standing depression (depression diagnosis and prescription for antidepressant medication at least 5 years before, excluding individuals who had discontinued antidepressants more than 6 months before the consultation). Patients with and without severe mental health problems were described by age group and compared for rates of referral, relevant cancer diagnosis, and relevant surgery in the following 2 years. Multivariate analyses by Cox proportional hazards model were used to estimate relationships between patient characteristics and diagnosis of relevant cancer, adjusting for all other characteristics (age, sex, area deprivation, BMI, smoking status, blood pressure, comorbidities, and HRT use for postmenopausal bleeding). Analyses were conducted using STATA (version 9.1).
RESULTS
The study population consisted of 3 867 132 patients registered with 328 general practices and meeting the inclusion criteria. Between 1 April 1998 and 31 March 2003 there were 30 175 patients aged 25 years or over with a first consultation for rectal bleeding, and 10 142 patients aged 40 years or over with a first consultation for postmenopausal bleeding, arising from 9 341 636 person-years of observation.
Figure 1 (see Supplementary Table 1 for data) shows the rate of first consultations for each type of bleeding by sex and age group. The rate of rectal bleeding increased with age: for females it ranged from 2.9 per thousand per year among those aged 25–29 years to 4.8 among those aged 85 years or over; for males from 2.3 to 4.9 per thousand per year for the same age groups. Postmenopausal bleeding consultations had their highest rate of 7.4 per thousand per year in females aged from 55–59 years, decreasing to 1.5 in the oldest age group. After excluding patients who had a prior diagnosis of a relevant cancer, there were 29 007 cases of rectal bleeding and 10 122 cases of postmenopausal bleeding for analysis.
Figure 1.
First consultations for rectal bleeding (n = 30 175) and postmenopausal bleeding (n = 10 142) by age and sex (all patients).
Table 1 (see Supplementary Table 2 for full data) shows the characteristics of the two patient groups. The rectal bleeding sample had similar proportions of males and females, and in both samples the proportion living in the most deprived areas (Townsend quintile 5) was lower than in the general population. Among the group with postmenopausal bleeding, 20% were recorded as obese, 30% were taking HRT, and 4% used tamoxifen. The prevalence of severe mental health problems (schizophrenia, bipolar disorder, learning difficulty, or long-standing depression) was around 2% in each group.
Table 1.
Characteristics of patients.
| Characteristic | Patients with rectal bleeding n = 29 007 (%) | Patients with postmenopausal bleeding n = 10 122 (%) |
|---|---|---|
| Female | 15 076 (52.0) | 10 122 (100.0) |
| Age, median (interquartile range) | 54 (40 to 69) | 58 (54 to 67) |
| Living in most deprived areas (quintile 5) | 5244 (18.1) | 1444 (14.3) |
| Obesea | 4196 (14.5) | 2006 (19.8) |
| Current smoker | 5435 (18.7) | 1445 (14.3) |
| Used HRT in last 12 months | – | 3,017 (29.8) |
| Used tamoxifen in last 12 months | – | 413 (4.1) |
| Severe mental health problems | ||
| Schizophrenia | 126 (0.4) | 59 (0.6) |
| Bipolar disorder | 72 (0.2) | 36 (0.4) |
| Learning difficulties | 189 (0.7) | 38 (0.4) |
| Long-standing depression | 257 (0.9) | 113 (1.1) |
| Any of these mental health problems | 606 (2.1) | 229 (2.3) |
Body mass index ≥30kg/m2. HRT = hormone replacement therapy.
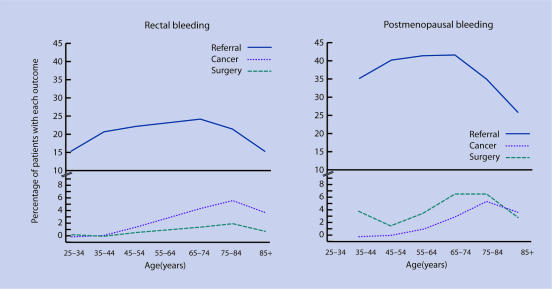
Relevant events in the 2 years following the first consultation for bleeding are summarised in Figure 2 (see Supplementary Table 3 for data). For patients with rectal bleeding, 21% had a relevant referral in their medical records, around 2% had a relevant cancer diagnosis, and less than 1% had relevant surgery. The rate of recorded referral was somewhat lower among the youngest and oldest patients, and the proportion with a cancer diagnosis increased substantially with age until the age of 85 years. For postmenopausal bleeding, 40% had a relevant referral or investigation in their record, under 2% had a relevant cancer diagnosis, and less than 4% underwent surgery. The proportion with a recorded referral was fairly constant up to 74 years of age and then diminished, and again there was a strong age-related rise in the proportion with a cancer diagnosis until the age of 85 years.
Figure 2.
Events in the 2 years following first consultation for rectal bleeding (n = 29 007) and postmenopausal bleeding (n = 10 122) (all patients).
For the comparison between patients with and without severe mental health problems, the characteristics and recorded events of patients in each group are shown in Table 2 (see Supplementary Table 4 for full data). Patients with mental health problems were more likely to live in an area of high deprivation, to be current smokers, and to be obese. In each sample, the proportion with recorded referrals was marginally higher in patients with mental health problems than in those without. The subgroup with depression accounted for much of this difference: 24.5% were referred for rectal bleeding compared with 21.4% in the other three mental health groups combined, and 47.8% with depression were referred for postmenopausal bleeding compared with 42.3% in the other three groups. The proportions of patients with cancer or surgery were difficult to compare, as in each sample fewer than ten patients with mental health problems experienced these events.
Table 2.
Characteristics and events for patients with and without mental health problems.
| Rectal bleeding | Postmenopausal bleeding | |||
|---|---|---|---|---|
| Characteristic/event | Mental health problems n = 606 (%) | No mental health problems n = 28 401(%) | Mental health problems n = 229 (%) | No mental health problems n = 9893 (%) |
| Female | 340 (56.1) | 14 736 (51.9) | 229 (100.0) | 9893 (100.0) |
| Age, median (interquartile range) | 55 (42 to 69) | 54 (40 to 69) | 57 (53 to 65) | 58 (54 to 67) |
| Living in most deprived area (quintile 5) | 152 (25.1) | 5092 (17.9) | 56 (24.5) | 1388 (14.0) |
| Obesea | 110 (18.2) | 4086 (14.4) | 70 (30.6) | 1936 (19.6) |
| Current smoker | 173 (28.5) | 5262 (18.5) | 51 (22.3) | 1394 (14.1) |
| Used HRT in last 12 months | – | – | 71 (31.0) | 2946 (29.8) |
| Used tamoxifen in last 12 months | – | – | 9 (3.9) | 404 (4.1) |
| Events in following 2 years | ||||
| Relevant referral/investigation | 137 (22.6) | 5928 (20.9) | 102 (44.5) | 3953 (40.0) |
| Relevant cancer | 9 (1.5) | 636 (2.2) | 3 (1.3) | 167 (1.7) |
| Relevant surgery | 2 (0.3) | 250 (0.9) | 6 (2.6) | 369 (3.7) |
Body mass index ≥30kg/m2. HRT = hormone replacement therapy.
The estimated relationships between patient characteristics and diagnosis of relevant cancer, derived from multivariate analysis by Cox proportional hazards models and adjusted for all other characteristics, are shown in Table 3 (see Supplementary Table 5). Mental health status was not included in the models in view of the very small numbers with cancer among those with mental health problems. For patients with rectal bleeding, males had a 72% higher cancer risk than females and there was a strong age association, with patients aged 75 years and over having an estimated risk 9.1 times higher than those aged under 55 years. There was a lower rate of colorectal cancer among patients with rectal bleeding recorded as current smokers. For postmenopausal bleeding there was a stronger age association, with patients aged 75 years and over having an estimated cancer risk 13 times higher than those aged under 55 years. Patients recorded as obese had double the risk of endometrial cancer and those taking HRT had a 69% lower risk.
Table 3.
Risk of relevant cancer within 2 years of first consultation for bleeding (all patients).
| Rectal bleeding n = 29 007 | Postmenopausal bleeding n = 10 122 | |||
|---|---|---|---|---|
| Characteristic | Hazard ratioa | 95% CI | Hazard ratioa | 95% CI |
| Sex | ||||
| Female | 1.00 | – | – | – |
| Male | 1.72 | 1.46 to 2.01 | – | – |
| Age group (years) | ||||
| 54 or lessb | 1.00 | – | 1.00 | – |
| 55–64 | 4.54 | 3.48 to 5.92 | 3.80 | 1.92 to 7.52 |
| 65–74 | 7.14 | 5.52 to 9.22 | 8.91 | 4.51 to 17.63 |
| 75 and over | 9.14 | 7.05 to 11.85 | 12.98 | 6.47 to 26.04 |
| Body mass index (BMI) | ||||
| Normal (<25) | 1.00 | – | 1.00 | – |
| Overweight (25–29.9) | 1.04 | 0.85 to 1.28 | 1.39 | 0.89 to 2.17 |
| Obese (≥30) | 1.13 | 0.88 to 1.44 | 2.00 | 1.26 to 3.10 |
| No valid BMI recorded | 1.00 | 0.77 to 1.31 | 1.58 | 0.92 to 2.73 |
| Smoking status | ||||
| Non–smoker | 1.00 | – | 1.00 | – |
| Smoker | 0.72 | 0.56 to 0.93 | 1.13 | 0.68 to 1.88 |
| Not recorded | 0.86 | 0.65 to 1.15 | 1.1 | 0.64 to 1.90 |
| HRT medication | ||||
| Previous user/none recorded | – | – | 1.00 | – |
| User in last 12 months | – | – | 0.31 | 0.18 to 0.55 |
Adjusted for all other variables in table plus deprivation, blood pressure, and comorbidities.
Minimum age 25 years for rectal bleeding, 40 years for postmenopausal bleeding. HRT = hormone replacement therapy.
DISCUSSION
Summary of main findings
First consultations for rectal bleeding increased steadily with age, from 2.9 per thousand patients per year at age 25–29 years to 4.8 over the age of 85 years. For postmenopausal bleeding the highest rate for first consultation of 7.4 per thousand per year was in women aged 55–59 years. Overall, 2.2% of those with rectal bleeding and 1.7% of those with postmenopausal bleeding went on to have a relevant cancer diagnosis within 2 years. The risk of cancer increased substantially with age; men with rectal bleeding were 72% more likely than women to have colorectal cancer. No evidence was found of a shortfall in referrals or investigations for rectal or postmenopausal bleeding among those with severe mental health problems.
Strengths and limitations of the study
This study, based on the electronic medical records of more than 3 million patients over 5 years, provides new information on primary care consultations and outcomes for rectal bleeding and postmenopausal bleeding. In contrast to previous questionnaire studies on these symptoms, the current results provide robust rates based on routinely collected medical data, avoiding bias due to selection, non-response, or poor recall. First-ever consultations are a useful reference point for practitioners making decisions on management and referral for patients reporting the symptom for the first time.
The overall rate of referrals was lower than expected. It may be that not all practices routinely record this information, but there is no reason to suspect that the level of recording would differ between mental health groups. Even in a dataset of this size, a comparison of cancer risk between mental health groups was not possible in view of the small numbers of patients with mental health problems and cancer within 2 years. Routine medical records provided patients' most recent recorded blood pressure, BMI, and smoking status, but the relatively high rates of missing data on these variables, and the likelihood that those with missing data were different from other patients, make any associations difficult to interpret.
Comparison with existing literature
Comparison of consultation rates with previous studies is difficult in view of the variety of methodologies that have been employed. Questionnaire surveys have reported prevalence rates among selected populations, or converted the occurrence of bleeding to incidence rates based on estimated population numbers. Studies have variously reported the number stating whether they have ever had bleeding, had first-ever bleeding, consulted a doctor for bleeding, and/or made a first consultation for bleeding. Surveys have found that up to 20% of all patients experienced rectal bleeding in one year, but only a minority sought medical advice.14–16 In a general practice of 2000 patients, an estimated 280–380 people reported that they had rectal bleeding in the previous year, 44 experienced it for the first time, and 14–30 people consulted their doctor about it.1 A study based on GPs' recordings of consultations for rectal bleeding reported 15 per thousand per year.6 This included all consultations rather than first-ever consultations as reported in the present study. For postmenopausal bleeding, studies with varying methodologies have found prevalence rates up to 11% and incidence up to 134 per thousand per year.5,17,18
Rectal bleeding and postmenopausal bleeding can be important signs of cancer, but for both symptoms the cause is non-malignant in the vast majority of cases.6,8 A substantial age gradient in cancer diagnosis within 2 years of follow-up was found in the current sample of patients reporting bleeding for the first time. The proportion of patients with rectal bleeding who went on to have colorectal cancer rose from 0.1% in those aged 25–34 years to 5.5% in those aged 75–84 years; a comparable age gradient has previously been found among patients with any consultation for rectal bleeding.19
For postmenopausal bleeding the proportion with endometrial cancer was 0.3% in women aged 45–54 years and 5.4% in those aged 75–84 years. Males with rectal bleeding had a higher rate of cancer than women, reflecting the differential sex risk in the general population.20 As with previous research, this study found that postmenopausal bleeding in women taking HRT was less likely to indicate endometrial cancer.18 Women recorded as obese had a higher probability that their postmenopausal bleeding was associated with endometrial cancer, reflecting the higher risk in the general population.21 There was a lower rate of colorectal cancer among patients with rectal bleeding who were recorded as current smokers.
There was no previous study of inequality in referral for these symptoms to compare the current findings with. People with severe mental health problems are known to have higher mortality from many cancers. Later detection and less effective delivery of treatment have been suggested as possible contributing factors,22 but this study found no evidence of differential referral patterns for these symptoms in UK primary care.
Implications for future research or clinical practice
First consultations for postmenopausal bleeding and rectal bleeding, together with subsequent referrals and diagnoses of cancer, have not been previously documented in detail for a large sample based on medical records rather than questionnaires which are more open to bias. The findings presented here provide useful reference material for clinicians and researchers. There is no evidence that clinicians are less likely to refer people with severe mental health problems who present with these symptoms.
Supplementary Material
Acknowledgments
We thank EMIS practices contributing to QRESEARCH, David Stables (EMIS Computing) for his help and expertise in establishing QRESEARCH, and Gavin Langford for carrying out the data extraction.
Supplementary information
Additional information accompanies this paper at: http://www.rcgp.org.uk/bjgp-suppinfo
Funding body
The study was supported by funding from the Disability Rights Commission. Chris Parker received NHS research and development support funding.
Ethics committee
Approval was granted by Trent Medical Research Ethics Committee (05/MRE04/47)
Competing interests
The authors have stated that there are none
REFERENCES
- 1.Hamilton W, Sharp D. Diagnosis of colorectal cancer in primary care: the evidence base for guidelines. Fam Pract. 2004;21(1):99–106. doi: 10.1093/fampra/cmh121. [DOI] [PubMed] [Google Scholar]
- 2.Jeste DV, Gladsjo JA, Lindamer LA, Lacro JP. Medical comorbidity in schizophrenia. Schizophr Bull. 1996;22(3):413–430. doi: 10.1093/schbul/22.3.413. [DOI] [PubMed] [Google Scholar]
- 3.Kendrick A. The shift to community mental health care: the impact on general practitioners. In: Jenkins R, Field V, Young R, editors. The primary care of schizophrenia. London: HMSO; 1992. [Google Scholar]
- 4.Cohen A, Phelan M. The physical health of patients with mental illness: a neglected area. Mental Health Promotion Update. 2001;2:15–16. [Google Scholar]
- 5.Astrup K, Olivarius NdF. Frequency of spontaneously occurring postmenopausal bleeding in the general population. Acta Obstet Gynecol Scand. 2004;83(2):203–207. doi: 10.1111/j.0001-6349.2004.00400.x. [DOI] [PubMed] [Google Scholar]
- 6.Ellis BG, Thompson MR. Factors identifying higher risk rectal bleeding in general practice. Br J Gen Pract. 2005;55(521):949–955. [PMC free article] [PubMed] [Google Scholar]
- 7.Douek M, Wickramasinghe M, Clifton MA. Does isolated rectal bleeding suggest colorectal cancer? Lancet. 1999;354(9176):393. doi: 10.1016/s0140-6736(99)02296-5. [DOI] [PubMed] [Google Scholar]
- 8.Bachmann LM, ter Riet G, Clark TJ, et al. Probability analysis for diagnosis of endometrial hyperplasia and cancer in postmenopausal bleeding: an approach for a rational diagnostic workup. Acta Obstet Gynecol Scand. 2003;82(6):564–569. doi: 10.1034/j.1600-0412.2003.00176.x. [DOI] [PubMed] [Google Scholar]
- 9.Hippisley-Cox J, Stables D, Pringle M. QRESEARCH—a new general practice database for research. Inform Prim Care. 2004;12(1):49–50. doi: 10.14236/jhi.v12i1.108. [DOI] [PubMed] [Google Scholar]
- 10.Office for National Statistics. Census 2001: national report for England and Wales. Part 1. London: The Stationery Office; 2003. [Google Scholar]
- 11.Hippisley-Cox J, Pringle M. Prevalence, care and outcomes for patients with diet controlled diabetes in general practice: cross sectional survey. Lancet. 2004;364(9432):423–428. doi: 10.1016/S0140-6736(04)16765-2. [DOI] [PubMed] [Google Scholar]
- 12.Hammersley V, Hippisley-Cox J, Wilson A, Pringle MA. Comparison of research general practices and their patients with other practices—cross sectional survey in Trent. Br J Gen Pract. 2002;52(479):463–468. [PMC free article] [PubMed] [Google Scholar]
- 13.Hippisley-Cox J, Hammersley V, Pringle M, et al. How useful are general practice databases for research? Analysis of their accuracy and completeness in one research network. Health Informatics J. 2004;10:91–109. [Google Scholar]
- 14.Crosland A, Jones R. Rectal bleeding: prevalence and consultation behaviour. BMJ. 1995;311(7003):486–488. doi: 10.1136/bmj.311.7003.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fijten GH, Blijham GH, Knottnerus JA. Occurrence and clinical significance of overt blood loss per rectum in the general population and in medical practice. Br J Gen Pract. 1994;44(384):320–325. [PMC free article] [PubMed] [Google Scholar]
- 16.Talley NJ, Jones M. Self-reported rectal bleeding in a United States community: prevalence, risk factors, and health care seeking. Am J Gastroenterol. 1998;93(11):2179–2183. doi: 10.1111/j.1572-0241.1998.00530.x. [DOI] [PubMed] [Google Scholar]
- 17.Viikki M, Pukkala E, Hakama M. Bleeding symptoms and subsequent risk of gynecological and other cancers. Acta Obstet Gynecol Scand. 1998;77(5):564–569. [PubMed] [Google Scholar]
- 18.Gredmark T, Kvint S, Havel G, Mattsson LA. Histopathological findings in women with postmenopausal bleeding. Br J Obstet Gynaecol. 1995;102(2):133–136. doi: 10.1111/j.1471-0528.1995.tb09066.x. [DOI] [PubMed] [Google Scholar]
- 19.Wauters H, Van Casteren V, Buntinx F. Rectal bleeding and colorectal cancer in general practice: diagnostic study. BMJ. 2000;321(7267):998–999. doi: 10.1136/bmj.321.7267.998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wei EK, Giovannucci E, Wu K, et al. Comparison of risk factors for colon and rectal cancer. Int J Cancer. 2004;108(3):433–442. doi: 10.1002/ijc.11540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weber AM, Belinson JL, Piedmonte MR. Risk factors for endometrial hyperplasia and cancer among women with abnormal bleeding. Obstet Gynecol. 1999;93(4):594–598. doi: 10.1016/s0029-7844(98)00469-4. [DOI] [PubMed] [Google Scholar]
- 22.Lawrence D, Holman CD, Jablensky AV, et al. Excess cancer mortality in Western Australian psychiatric patients due to higher case fatality rates. Acta Psychiatr Scand. 2000;101(5):382–388. doi: 10.1034/j.1600-0447.2000.101005382.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.